ICHS (Florida International College of Health Sciences) Med Surg 1
Total Questions : 53
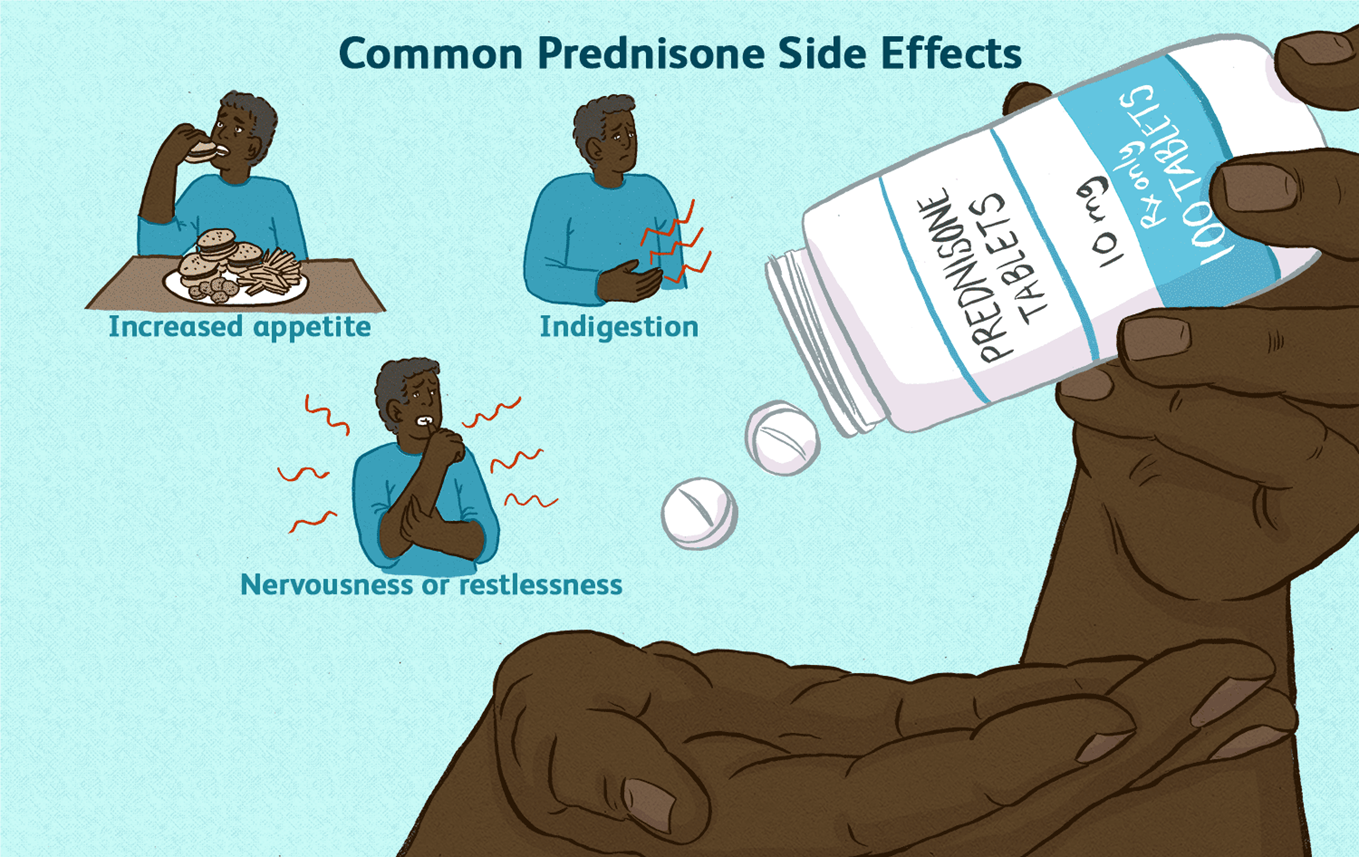
Showing 25 questions, Sign in for moreA nurse is educating a client with systemic lupus erythematosus about the use of prednisone. Which piece of information should be prioritized?
Explanation
Choice A rationale:
Prednisone is a corticosteroid that suppresses the body's natural production of cortisol. Cortisol is a hormone that is essential for life, and it plays a role in many important bodily functions, including:
Regulating blood sugar levels Maintaining blood pressure Reducing inflammation Responding to stress
When a person takes prednisone for a long period of time, their body begins to rely on the medication to provide cortisol. If the medication is stopped suddenly, the body cannot produce enough cortisol on its own, which can lead to a life-threatening condition called adrenal insufficiency.
Adrenal insufficiency can cause a variety of symptoms, including: Extreme fatigue
Weakness Dizziness Nausea Vomiting Abdominal pain Confusion
Loss of consciousness
To prevent adrenal insufficiency, it is important to taper off prednisone slowly over a period of time. This allows the body to gradually adjust to producing cortisol on its own.
Here are some additional details about why prednisone should never be discontinued abruptly: The risk of adrenal insufficiency is highest when prednisone has been taken for more than 3 weeks. The longer a person has been taking prednisone, the slower the taper should be.
It is important to follow the tapering instructions provided by the healthcare provider.
If a person experiences any symptoms of adrenal insufficiency, they should seek medical attention immediately.
A nurse has conducted an educational session for a community group on Lyme disease. Which statement by a participant indicates a need for further review of the material?
Explanation
Choice A rationale:
This statement is accurate. Early Lyme disease (Stage I) is typically treated with oral antibiotics for 14 to 21 days. This is often effective in clearing the infection and preventing further complications.
Choice B rationale:
This statement is also accurate. A red rash that may resemble a bull's eye is a common early symptom of Lyme disease. It often appears at the site of the tick bite, typically within 3 to 30 days after the bite.
Choice C rationale:
This statement is incorrect. While Lyme disease can be serious if not treated, it is rarely fatal. Most people who are treated for Lyme disease recover fully. However, if left untreated, it can lead to chronic health problems, such as arthritis, neurological problems, and heart issues.
Choice D rationale:
This statement is accurate. Taking precautions against tick bites is essential for preventing Lyme disease. Ticks are most active during the warmer months, so it's crucial to be vigilant about tick prevention during the spring, summer, and fall.
A nursing manager is worried about the number of infections in the hospital unit. What action by the manager would be most effective in preventing these infections?
Explanation
Choice A rationale:
While promptly removing urinary catheters can reduce the risk of catheter-associated urinary tract infections (CAUTIs), it addresses only one specific type of infection. It doesn't comprehensively address other common healthcare-associated infections (HAIs) like central line-associated bloodstream infections (CLABSIs), surgical site infections (SSIs), ventilator-associated pneumonia (VAP), and Clostridium difficile infections (CDI).
Education about infection control methods, however, encompasses a broader range of preventive measures that can be applied to various HAIs, making it a more effective strategy for overall infection prevention.
Choice C rationale:
Placing patients in appropriate isolation can prevent the spread of infections, but it's a reactive measure that's implemented after an infection has already occurred. It doesn't address the root causes of infections or prevent their occurrence in the first place.
Education about infection control methods, on the other hand, is a proactive approach that aims to prevent infections from happening in the first place by teaching staff about proper hygiene practices, aseptic techniques, and other infection prevention strategies.
Choice D rationale:
Monitoring hand hygiene practices is crucial for infection prevention, but it's only one aspect of a comprehensive infection control program. Education about infection control methods goes beyond hand hygiene and covers various other preventive measures, such as:
Proper use of personal protective equipment (PPE) Aseptic technique during invasive procedures
Proper cleaning and disinfection of equipment and surfaces Proper handling of patient waste
Recognition of signs and symptoms of infection Prompt reporting of potential outbreaks
Therefore, educating staff members about infection control methods is the most effective action the nursing manager can take to prevent infections in the hospital unit because it provides a comprehensive approach to infection prevention, addressing various aspects of HAI prevention and promoting a culture of safety among healthcare staff.
A nurse is caring for an older patient admitted with mild dehydration. What advice should the nurse give to best address this issue?
Explanation
Choice A rationale:
While it's true that dehydration can lead to incontinence, simply stating this fact to the patient doesn't directly address the issue of dehydration. It doesn't provide actionable steps to correct the dehydration.
Incontinence can be a result of dehydration, but addressing the dehydration is the primary concern to prevent further complications.
Providing information about incontinence might be helpful in other contexts, but it's not the most effective advice to address mild dehydration in this specific scenario.
Choice B rationale:
Diuretics promote fluid loss through urination, which can worsen dehydration.
Advising the patient to take a diuretic in the morning would be counterproductive in this case. The goal is to increase fluid intake, not further deplete fluid levels.
It's important to consider the patient's medications and potential interactions before suggesting any changes to their medication regimen.
Choice C rationale:
Regular fluid intake is essential for maintaining hydration and replenishing lost fluids.
This advice directly addresses the issue of dehydration by encouraging the patient to consume fluids consistently. Drinking fluids every 1 to 2 hours can help restore fluid balance and prevent further complications.
It's a simple, actionable, and effective measure to address mild dehydration.
Choice D rationale:
While reducing sodium intake can be beneficial for some individuals with hypertension or other conditions, it's not the most relevant advice for addressing mild dehydration.
Sodium restriction might be appropriate in certain cases, but it doesn't directly address the immediate need to increase fluid intake.
The primary focus in this situation should be on replenishing fluids, not restricting sodium.
A patient is scheduled to receive 2000 ml of Normal Saline over 24 hours. How much fluid should be administered per hour?
Explanation
Rationale:
Step 1: Divide the total volume of fluid (2000 ml) by the total time in hours (24 hours). Step 2: Perform the calculation: 2000 ml ÷ 24 hours = 83.33 ml/hour.
Step 3: Round the answer to the nearest whole number, as fluid administration is typically measured in whole milliliters.
The correct answer is 83 ml/hour.
A nurse is discussing with a colleague who is relocating to a new state and needs to find a new job there. What is the best advice the nurse can give?
Explanation
Choice A rationale:
While working in a facility affiliated with a medical or nursing school can offer opportunities for professional development and collaboration, it is not the most important factor to consider when choosing a new job.
Affiliation with a school does not guarantee a positive work environment, strong nursing leadership, or a commitment to quality patient care, which are all hallmarks of Magnet hospitals.
It's essential to consider other factors that directly impact job satisfaction, patient outcomes, and overall nursing excellence.
Choice B rationale:
Having the latest technology can be beneficial, but it does not ensure a supportive work environment or a high standard of nursing care.
Technology is only one aspect of a hospital's operations, and it should not be the primary focus when making a career decision. It's crucial to prioritize factors that directly influence the quality of nursing practice and patient outcomes.
Choice C rationale:
Inquiring about nurse-client ratios is important, as it can provide insight into the workload and staffing levels at a hospital. However, it's not the most comprehensive indicator of a hospital's commitment to nursing excellence.
Magnet status, in contrast, signifies a broader commitment to quality nursing care, professional development, and positive work environments.
Choice D rationale:
Magnet status is a prestigious designation awarded by the American Nurses Credentialing Center (ANCC) to hospitals that demonstrate excellence in nursing care, leadership, and innovation.
Magnet hospitals are known for:
Attracting and retaining highly qualified nurses Fostering a culture of collaboration and teamwork Investing in professional development and growth
Promoting evidence-based practice and quality improvement Demonstrating outstanding patient outcomes
Seeking employment at a Magnet hospital is strongly recommended for nurses who prioritize professional growth, job satisfaction, and the delivery of exceptional patient care.
A patient diagnosed with HIV-II is admitted to the hospital presenting symptoms of fever, night sweats, and a severe cough.
The laboratory results show a CD4+ cell count of 180/mm and a negative tuberculosis (TB) skin test conducted 4 days prior.
What is the first action the nurse should take?
Explanation
Rationale for Choice A:
While it's important for the primary healthcare provider to be informed about the CD4+ results, it's not the first action the nurse should take. The priority is to implement appropriate infection control measures to protect the patient, other patients, and healthcare staff.
CD4+ cell count is a crucial indicator of the patient's immune status. A count of 180/mm is significantly low, suggesting a weakened immune system and increased vulnerability to infections. However, informing the provider alone doesn't directly address the immediate need for infection control.
Rationale for Choice B:
Airborne Precautions are specifically used for patients with known or suspected airborne infections, such as tuberculosis, measles, or varicella. These precautions involve the use of negative pressure rooms and N95 respirators.
In this case, the patient's TB skin test was negative, indicating no evidence of active tuberculosis infection. Implementing Airborne Precautions unnecessarily could lead to excessive resource utilization and potential stigmatization of the patient.
Rationale for Choice C:
Droplet Precautions are used for patients with infections that can be spread through large respiratory droplets, such as influenza, pertussis, or meningococcal meningitis. These precautions involve the use of masks and eye protection.
While the patient's symptoms of fever, night sweats, and severe cough could be consistent with a droplet-spread infection, there's no definitive evidence to support this at the present time. Initiating Droplet Precautions without a clear indication could also lead to unnecessary resource use and potential anxiety for the patient.
Rationale for Choice D:
Standard Precautions are the foundation of infection control and should be used for all patients, regardless of their known or suspected infection status. These precautions include hand hygiene, use of personal protective equipment (PPE) when indicated, and safe handling of sharps and bodily fluids.
By implementing Standard Precautions, the nurse can effectively minimize the risk of transmission of pathogens, protecting both the patient and other individuals in the healthcare setting. This is the most appropriate first action to ensure a safe and appropriate level of care.
A nurse is providing care for a patient who has a methicillin-resistant Staphylococcus aureus (MRSA) infection, which was cultured from the urine. What is the most appropriate action for the nurse to take?
Explanation
Choice A rationale:
Utilizing a respirator when handling urine output is not the most appropriate action for a nurse caring for a patient with MRSA.
MRSA is not typically transmitted through the air, but rather through direct contact with infected wounds or contaminated surfaces.
While a respirator may offer some protection against airborne particles, it is not necessary for routine care of a patient with MRSA.
It is more important to focus on hand hygiene and other infection control measures.
Choice B rationale:
Restricting visitors strictly to immediate family members only is not necessary for a patient with MRSA.
While it is important to limit the number of visitors to reduce the risk of spreading infection, there is no need to restrict visitors to immediate family members only.
Visitors should be instructed on proper hand hygiene and other infection control measures, and they should avoid contact with the patient's wounds or dressings.
Choice C rationale:
Washing hands only after removing gloves post-care is not sufficient for preventing the spread of MRSA. It is important to wash hands before and after any contact with the patient, even when wearing gloves.
This is because gloves can become contaminated with bacteria, and hand washing helps to remove any bacteria that may have gotten on the hands.
Choice D rationale:
Preparing to administer vancomycin is the most appropriate action for a nurse caring for a patient with MRSA. Vancomycin is an antibiotic that is effective against MRSA.
It is often used to treat MRSA infections, and it can help to prevent the infection from spreading.
An elderly patient, who is ambulatory and independent, is admitted to the hospital. What intervention by the nurse would be most effective in preventing falls for this patient?
Explanation
Rationale for Choice A:
Arranging for a bedside commode can be helpful for patients who have difficulty ambulating to the bathroom. However, it is not the most effective intervention for preventing falls in an ambulatory and independent patient. In fact, it could potentially increase the risk of falls if the patient attempts to use the commode without assistance or if they become disoriented in the dark.
Research has shown that bedside commodes are associated with an increased risk of falls in hospitalized patients. This is because patients may try to get out of bed to use the commode without assistance, or they may become disoriented in the dark and fall.
Additionally, bedside commodes can be a tripping hazard, especially for patients with impaired mobility.
Rationale for Choice B:
Ensuring the bathroom light is kept on during the night can help to reduce the risk of falls by making it easier for the patient to see. However, it is not the most effective intervention for preventing falls.
Patients may still fall even if the bathroom light is on, especially if they are weak, unsteady, or have impaired vision. Additionally, keeping the bathroom light on all night can disrupt the patient's sleep, which can also increase the risk of falls.
Rationale for Choice C:
Using side rails to keep the patient in bed is not an effective intervention for preventing falls. In fact, it can actually increase the risk of falls by making it more difficult for the patient to get out of bed safely.
Patients may try to climb over the side rails, which can lead to falls.
Additionally, side rails can restrict the patient's movement and make them feel trapped, which can lead to agitation and an increased risk of falls.
Rationale for Choice D:
Implementing a toileting schedule is the most effective intervention for preventing falls in an ambulatory and independent patient. This is because it helps to reduce the patient's need to get out of bed at night to use the bathroom.
When a patient has a scheduled time to toilet, they are less likely to try to get out of bed on their own and risk a fall. Additionally, a toileting schedule can help to prevent incontinence, which can also lead to falls.
The primary healthcare provider prescribes Hydroxychloroquine for a patient. What information should the nurse include when discussing this medication with the patient?
Explanation
Rationale for Choice A:
Hydroxychloroquine does not typically cause hair loss as a significant side effect. While some anecdotal reports have suggested hair thinning as a possibility, it's not a well-established or common occurrence in clinical studies.
If a patient experiences hair loss while on hydroxychloroquine, it's essential to rule out other potential causes, such as underlying medical conditions, stress, or nutritional deficiencies.
It's also important to note that some individuals may have a personal predisposition to hair loss, and medications can sometimes trigger or exacerbate this issue.
Rationale for Choice B:
Hydroxychloroquine is not known to cause a burst of energy. In fact, some patients may experience fatigue or drowsiness as a side effect.
It's crucial to inform patients about potential side effects to manage expectations and promote adherence to treatment.
If a patient experiences unexpected energy changes while taking hydroxychloroquine, it's essential to report this to their healthcare provider for further evaluation.
Rationale for Choice C:
Hydroxychloroquine is generally recommended to be taken with food or milk to reduce potential gastrointestinal side effects such as nausea and vomiting.
Taking it on an empty stomach could increase the risk of these side effects, which could impact medication adherence and effectiveness.
Rationale for Choice D:
Retinal damage is the most serious adverse effect of hydroxychloroquine. It can lead to irreversible vision loss if not detected and managed early.
Patients taking hydroxychloroquine must undergo regular eye examinations to monitor for any signs of retinal toxicity.
Early detection and prompt discontinuation of the medication can often prevent permanent vision loss.
It's crucial for nurses to educate patients about this potential risk and emphasize the importance of regular eye exams.
A patient diagnosed with HIV-II and wasting syndrome is suffering from inadequate nutrition. What assessment finding by the nurse would best indicate that the goals have been met for this patient’s problem?
Explanation
Choice A rationale:
Weight gain is the most objective and reliable indicator of improved nutritional status in patients with HIV-II and wasting syndrome. It directly reflects an increase in lean body mass, which is essential for restoring physical strength, immune function, and overall health.
A weight gain of 2 lb (1 kg) in a month is considered a clinically significant improvement for this patient population. It demonstrates that the patient is consuming more calories than they are expending, leading to a positive energy balance and tissue growth.
Other assessment findings, such as food intake, food choices, and oral discomfort, can be subjective and influenced by various factors, such as appetite, taste changes, nausea, fatigue, and psychosocial issues. While they provide valuable information about the patient's nutritional status, they do not directly measure the actual improvement in body composition.
Choice B rationale:
Consuming 90% of meals and snacks is a positive sign that the patient is adhering to their dietary recommendations. However, it does not guarantee that they are consuming enough calories to promote weight gain. The patient's individual energy needs and the nutritional content of the meals and snacks must be considered.
Choice C rationale:
Choosing high-protein foods is important for building and repairing tissues, but it does not ensure adequate overall caloric intake. The patient may still be experiencing a calorie deficit if they are not consuming enough total calories, even if they are focusing on protein-rich foods.
Choice D rationale:
Decreased oral discomfort can facilitate better food intake, but it does not directly reflect weight gain or improved nutritional status. The patient may still have challenges with appetite, nausea, or other factors that hinder their ability to consume enough calories.
You are instructed to administer 40 mg of methadone (Dolophine) subcutaneously for opioid detoxification. Given that you have a concentration of 30 mg/mL on hand, how much should you draw into the syringe?
Explanation
Step 1: Divide the prescribed dose (40 mg) by the concentration on hand (30 mg/mL).
Step 2: Perform the calculation: 40 mg ÷ 30 mg/mL = 1.3333 mL.
Step 3: Round the answer to the nearest tenth: 1.3333 mL rounds to 1.3 mL.
A nurse is contacting the on-call healthcare provider about a patient who underwent a hysterectomy two days ago and is experiencing pain that is not alleviated by the prescribed opioid pain medication. Which statement constitutes the “Background” portion of the SBAR format for communication?
Explanation
Choice A rationale:
This statement belongs to the "Request" portion of the SBAR format. It articulates a specific action the nurse wants the healthcare provider to take.
It's not part of the Background because it doesn't provide any historical or contextual information about the patient's condition.
Choice B rationale:
This statement is the correct choice for the "Background" portion of the SBAR format.
It provides essential background information about the patient's recent medical history, specifically the recent hysterectomy.
This information is crucial for the healthcare provider to understand the context of the current situation and make informed decisions about pain management.
Choice C rationale:
This statement provides additional patient information, but it's not the most relevant for the Background section in this context.
The patient's aversion to NSAIDs might be important for medication choices, but it doesn't directly address the current issue of pain management after a hysterectomy.
Choice D rationale:
This statement provides important information about the patient's allergies, but it's not the most relevant for the Background section in this context.
Allergies are crucial for medication safety, but they don't directly address the current issue of pain management or provide context about the patient's recent surgery.
A patient with HIV-1 has experienced a sudden decline in health status accompanied by a significant increase in viral load. What is the first action the nurse should take?
Explanation
Choice A rationale:
Assessing the patient's adherence to the drug regimen is the most crucial first step in this situation. Here's a comprehensive explanation:
1. Significance of Adherence in HIV Treatment:
Viral Suppression and Disease Progression: Adherence to antiretroviral therapy (ART) is paramount in HIV management. It directly impacts viral suppression, preventing disease progression, and reducing the risk of opportunistic infections and complications. Non-adherence can lead to viral rebound, increased viral load, and potential disease advancement.
Primary Cause of Treatment Failure: Suboptimal adherence is the leading cause of treatment failure in HIV patients. It can result in:
Reduced effectiveness of ART Development of drug resistance Increased healthcare costs Increased risk of transmission
2. Rationale for Prioritizing Adherence Assessment:
Direct Link to Viral Load and Health Status: A sudden decline in health status and a significant increase in viral load strongly suggest potential non-adherence. Assessing adherence early on can:
Identify the root cause of the clinical deterioration
Inform timely interventions to address adherence barriers Prevent further complications
3. Assessing Adherence Thoroughly:
Non-Judgmental Approach: Creating a supportive and non-judgmental environment is essential for honest and accurate assessment.
Open-Ended Questions: Utilize open-ended questions to explore potential challenges and barriers to adherence, such as: Difficulties with medication schedules
Side effects Financial constraints Forgetfulness
Mental health concerns Substance abuse
Lack of social support
Objective Measures: Complement patient reports with objective measures like:
Pill counts
Pharmacy refill records
Medication Event Monitoring Systems (MEMS)
4. Addressing Adherence Barriers:
Tailored Interventions: Based on the assessment findings, develop individualized strategies to enhance adherence, such as: Simplifying medication regimens
Addressing side effects
Providing medication reminders
Offering counseling and support services
Connecting patients with resources
5. Reassessing and Monitoring:
Continuous Evaluation: Regularly reassess adherence and viral load to ensure treatment effectiveness and make adjustments as needed.
Conclusion:
While other options (B, C, D) may provide valuable information, prioritizing adherence assessment is critical to promptly identify and address potential adherence issues, optimize treatment outcomes, and prevent further health decline in HIV patients experiencing viral rebound.
A nurse is caring for a patient who has a methicillin-resistant Staphylococcus aureus (MRSA) infection that was cultured from the urine. What is the most appropriate action for the nurse to take?
Explanation
Choice A rationale:
Wearing a respirator when handling urine output is not routinely recommended for MRSA infections. While airborne transmission of MRSA is possible, it is primarily spread through direct contact with infected skin or surfaces. Respirators are typically reserved for situations where there is a high risk of aerosolization, such as during certain medical procedures.
The use of a respirator can be cumbersome and uncomfortable, and it may not provide significant additional protection in this context.
It's important to prioritize hand hygiene and contact precautions over respirator use for routine care of patients with MRSA infections.
Choice B rationale:
Limiting visitors strictly to immediate family members only is not necessary for MRSA infection control. Visitors can be educated on proper hand hygiene and contact precautions to minimize the risk of transmission.
Restricting visitors can have negative psychosocial impacts on the patient, such as isolation and decreased social support. It's important to balance infection control measures with the patient's overall well-being.
Choice C rationale:
Washing hands only after removing gloves post-care is inadequate for MRSA infection control. Hands should be washed thoroughly with soap and water or an alcohol-based hand sanitizer:
Before and after entering the patient's room
Before and after any contact with the patient or their surroundings After removing gloves
After using the toilet Before eating or drinking.
Choice D rationale:
Vancomycin is an antibiotic that is effective against MRSA infections. It is often the first-line treatment for these infections.
Preparing to administer vancomycin as prescribed by the healthcare provider is the most appropriate action to take to address the patient's MRSA infection.
Prompt initiation of appropriate antibiotic therapy is essential to controlling the infection and preventing complications.
A 40-year-old patient with polycystic kidney disease is scheduled to receive a kidney transplant.
When the nurse begins to administer 2 units of leukocyte-poor packed red blood cells to treat a low hemoglobin level, the patient asks why this has been prescribed.
What is the appropriate response from the nurse?
Explanation
Choice A rationale:
Leukocyte-poor packed red blood cells (LP-PRBCs) have a significantly reduced number of white blood cells (WBCs), also known as leukocytes. This is crucial for pre-transplant patients like the one in the question for several reasons:
Prevention of Alloimmunization: WBCs in blood transfusions carry human leukocyte antigens (HLAs), which are proteins on the surface of cells that play a role in the immune system. Exposure to foreign HLAs can cause the recipient's immune system to develop antibodies against them, a process called alloimmunization. These antibodies can then attack and damage the transplanted kidney, leading to rejection. By reducing the number of WBCs in the transfusion, LP-PRBCs significantly lower the risk of alloimmunization.
Reduced Incidence of Febrile Non-Hemolytic Transfusion Reactions (FNHTRs): FNHTRs are the most common type of transfusion reaction, characterized by fever, chills, and occasionally other symptoms like nausea and vomiting. They are thought to be caused by cytokines released from WBCs in the transfused blood. LP-PRBCs, with their reduced WBC content, have been shown to lower the incidence of FNHTRs.
Potential Benefits for Graft Survival: Some studies have suggested that the use of LP-PRBCs for transfusions may improve long-term graft survival rates in kidney transplant patients, although more research is needed to confirm these findings.
Choice B rationale:
This statement is incorrect. While LP-PRBCs may have some advantages in terms of absorption or utilization, this is not the primary reason for their use in pre-transplant patients. The main goal is to reduce the risk of alloimmunization and other transfusion-related complications.
Choice C rationale:
This statement is partially correct. LP-PRBCs do tend to cause fewer blood reactions, particularly FNHTRs, as explained in the rationale for Choice A. However, this is not the most comprehensive or accurate explanation for their use in pre-transplant patients.
Choice D rationale:
This statement is not directly relevant to the use of LP-PRBCs in pre-transplant patients. While LP-PRBCs may have a lower risk of hemolysis, this is not the primary reason for their use in this specific context.
A nurse learns that which of the following is the single biggest risk factor for developing cancer?
Explanation
Choice A rationale:
While advancing age is a significant risk factor for cancer, it is not considered the single biggest risk factor. The risk of developing cancer does increase with age, primarily due to the accumulation of DNA damage over time. This damage can arise from various sources, including exposure to carcinogens, errors in DNA replication, and oxidative stress. With age, the body's ability to repair DNA damage also declines, making cells more susceptible to cancerous changes.
However, it's important to note that cancer can develop at any age, and even younger individuals can be affected if exposed to other significant risk factors.
Choice B rationale:
Exposure to tobacco is widely recognized as the single biggest risk factor for developing cancer. It is estimated to be responsible for about 25-30% of all cancer deaths worldwide.
Tobacco smoke contains over 70 known carcinogens, which are substances that can damage DNA and lead to cancer. These carcinogens can affect various organs in the body, including the lungs, mouth, throat, esophagus, stomach, pancreas, liver, bladder, kidney, cervix, and colon.
The risk of cancer increases with the amount and duration of tobacco use. Even exposure to secondhand smoke can increase the risk of cancer.
Quitting tobacco use is the most effective way to reduce the risk of cancer.
Choice C rationale:
Exposure to occupational chemicals is a known risk factor for certain types of cancer, such as lung cancer, bladder cancer, and leukemia. However, it is not considered the single biggest risk factor for developing cancer overall.
The risk of cancer from occupational chemicals depends on the specific chemical, the level of exposure, and the duration of exposure.
Workplace safety measures, such as using protective equipment and limiting exposure to hazardous chemicals, can help reduce the risk of cancer.
Choice D rationale:
Infection with certain viruses, known as oncoviruses, can increase the risk of developing certain types of cancer. For example, infection with human papillomavirus (HPV) can increase the risk of cervical cancer, and infection with hepatitis B virus (HBV) can increase the risk of liver cancer.
However, oncoviruses are not considered the single biggest risk factor for developing cancer overall. Vaccines are available to protect against some oncoviruses, such as HPV and HBV.
A patient with HIV-1 is curious as to why gabapentin is included in their medication regimen, despite not having a history of seizures. What would be the most appropriate response from the nurse?
Explanation
Choice A rationale:
It is not accurate to state that the patient is at risk for seizures due to fungal infections. While fungal infections can occur in individuals with HIV-1, they are not a primary cause of seizures in this population.
Linking fungal infections directly to seizure risk without clear evidence could cause unnecessary anxiety in the patient. It's important to provide accurate and relevant information to patients.
Choice B rationale:
Responding with "I have no idea why you would be taking this drug" is unprofessional and unhelpful.
Nurses are expected to have a basic understanding of the medications their patients are taking and to be able to provide education and support.
It's essential to demonstrate knowledge and confidence when interacting with patients.
Choice C rationale:
While gabapentin can have mood-elevating effects in some individuals, it is not primarily used as an antidepressant. Mentioning this potential side effect without clarifying the primary purpose of the medication could mislead the patient. It's crucial to prioritize the main indication for the medication to avoid confusion.
Choice D rationale:
This is the most appropriate response because it accurately explains the primary reason for prescribing gabapentin to this patient.
Gabapentin is commonly used to treat neuropathic pain, which is pain caused by nerve damage.
HIV-1 can often lead to neuropathic pain, making gabapentin a valuable treatment option in this population.
Providing clear and accurate information about medication purpose builds trust and understanding between the nurse and the patient.
A patient has been put on Contact Precautions. The patient’s family is extremely apprehensive about visiting due to fear of being “contaminated” by the patient. What is the best course of action for the nurse?
Explanation
Choice A: Clarify that these precautions are mandated by law.
While it's important to acknowledge the legal requirements for Contact Precautions, this approach alone may not adequately address the family's emotional concerns and fears. It could potentially increase their anxiety if they feel forced to visit without understanding the reasons behind the precautions.
Choice B: Emphasize the importance of their visit to the patient.
While family support is crucial for the patient's well-being, emphasizing the importance of their visit without addressing their fears could inadvertently pressure them to visit without feeling comfortable or confident in their ability to protect themselves.
Choice C: Assure the family that they will not contract the infection.
It's not always possible to guarantee that the family won't contract the infection. Making such assurances could create a false sense of security and potentially lead to lapses in infection control practices.
Choice D: Demonstrate to the family how to prevent the spread of the disease.
Empowering the family through education and demonstration is the most effective approach. It addresses their concerns directly, promotes understanding, and instills confidence in their ability to protect themselves while visiting.
Key elements of this demonstration include:
Proper hand hygiene techniques
Use of personal protective equipment (PPE) such as gloves and gowns Safe handling of potentially contaminated items
Maintaining a safe distance from the patient when appropriate Understanding the modes of transmission for the specific disease
By providing clear guidance and allowing for practice, the nurse can help the family feel more comfortable and confident in their ability to visit safely.
Additional considerations:
Addressing the family's emotional concerns: Acknowledge their fears and provide reassurance in a compassionate and understanding manner.
Tailoring education to the family's level of understanding: Use simple language and visual aids as needed.
Encouraging questions and open communication: Create a supportive environment where the family feels comfortable asking questions and expressing their concerns.
Collaborating with other healthcare professionals: Involve infection control specialists or other relevant team members to provide additional support and expertise.
A nurse is conversing with a colleague who is relocating to another state and is in search of a new job. What advice from the nurse would be most beneficial?
Explanation
Choice A rationale:
Affiliation with a medical or nursing school can offer some benefits, but it's not the most crucial factor to consider when seeking a new job.
Nurses in these facilities may have opportunities for professional development and involvement in research, but these benefits might not be available to all nurses.
The quality of the work environment, staffing levels, and support for nurses can vary significantly in facilities affiliated with schools.
Prioritizing Magnet status ensures a focus on nursing excellence and a commitment to providing a supportive work environment.
Choice B rationale:
Having the latest technology can be appealing, but it doesn't guarantee a positive work experience for nurses.
The most important factors for job satisfaction and quality patient care are often related to the work environment, staffing levels, and leadership support.
Magnet hospitals prioritize these factors, leading to better outcomes for both nurses and patients.
Choice C rationale:
Inquiring about nurse-patient ratios is essential, but it's not the only indicator of a positive work environment.
Magnet hospitals typically have favorable nurse-patient ratios, but they also excel in other areas that contribute to job satisfaction and quality care.
These areas include: shared governance, leadership support, professional development opportunities, and a focus on evidence-based practice.
Choice D rationale:
Magnet status is the highest recognition a hospital can achieve for nursing excellence.
It signifies a commitment to: quality patient care, positive work environments for nurses, professional development, and shared governance.
Research consistently demonstrates that Magnet hospitals have: lower nurse turnover rates, higher patient satisfaction scores, and better patient outcomes.
Seeking employment in a Magnet hospital is the most beneficial advice for a nurse looking for a job that prioritizes nursing excellence, job satisfaction, and quality patient care.
A patient has recently been diagnosed with systemic lupus erythematosus and is discussing self-care strategies with the nurse. Which statement from the patient suggests a need for further review of the material?
Explanation
Choice A rationale:
Planning activities to prevent fatigue is a valid self-care strategy for SLE patients. Fatigue is a common symptom of SLE, and it can be exacerbated by overexertion. By planning activities and pacing themselves, patients can help to manage their fatigue and conserve energy.
Fatigue management strategies include:
Prioritizing tasks and delegating when possible.
Breaking down large tasks into smaller, more manageable ones. Taking frequent rest breaks throughout the day.
Maintaining a regular sleep schedule. Engaging in moderate exercise, as tolerated.
Avoiding caffeine and alcohol, which can interfere with sleep.
Addressing any underlying health conditions that may be contributing to fatigue, such as anemia or depression.
Choice B rationale:
Prioritizing rest is another essential self-care strategy for SLE patients. Rest allows the body to conserve energy and repair itself. Patients with SLE may need more rest than healthy individuals, especially during flares.
Resting strategies include:
Getting enough sleep at night. Napping during the day, as needed.
Taking breaks from activities throughout the day.
Practicing relaxation techniques, such as deep breathing or meditation.
Choice C rationale:
Sunbathing is not recommended for SLE patients, as it can trigger flares. Ultraviolet (UV) radiation from the sun can damage skin cells and exacerbate inflammation in SLE patients. This can lead to a flare-up of symptoms, such as skin rash, joint pain, and fatigue.
Sun protection strategies include:
Avoiding direct sunlight, especially during the middle of the day when UV rays are strongest. Wearing protective clothing, such as long-sleeved shirts, pants, and wide-brimmed hats.
Using sunscreen with an SPF of 30 or higher on a daily basis.
Applying sunscreen liberally and reapplying it every two hours, or more often if sweating or swimming.
Choice D rationale:
Avoiding direct sunlight is a correct self-care strategy for SLE patients.
A nurse is studying the differences between normal cells and benign tumor cells. What information is included in this?
Explanation
Choice B rationale:
Benign tumors typically grow in the wrong place or at the wrong time. This is a key distinguishing feature of benign tumors compared to normal cells. Normal cells have precise mechanisms that control their growth, ensuring they divide and multiply only when and where they are needed. Benign tumors, however, have disruptions in these regulatory mechanisms, leading to abnormal growth patterns. This means they may grow in locations where they don't belong or continue to grow even when they are no longer needed.
Here's a detailed explanation of why the other choices are incorrect:
Choice A:
Benign tumors have not lost their cellular regulation from contact inhibition. Contact inhibition is a process that stops normal cells from growing when they come into contact with other cells. Benign tumors still maintain this ability, which helps to limit their growth and prevent them from spreading to other tissues.
Choice C:
Benign tumors do not grow through invasion of other tissue. Invasion is a hallmark feature of malignant tumors (cancers). Benign tumors, on the other hand, typically grow as encapsulated masses, meaning they are surrounded by a well-defined border that separates them from surrounding tissues. They do not infiltrate or invade surrounding structures.
Choice D:
Anaplasia refers to the loss of differentiation and resemblance to the parent cells, which is a characteristic of malignant tumors, not benign tumors. Benign tumors still maintain a degree of differentiation, meaning they retain some of the characteristics of the normal cells from which they originated.
A nurse studying infection control learns that which factor is the most effective and crucial barrier to infection?
Explanation
Choice A rationale:
Skin and mucous membranes are the most effective and crucial barriers to infection. They provide a continuous physical barrier that prevents pathogens from entering the body. Here's a detailed explanation of their protective mechanisms:
1. Physical Barrier:
Skin: The outermost layer of skin, the epidermis, is composed of tightly packed cells that are difficult for pathogens to penetrate. It's also covered in a layer of sebum, an oily substance that helps to repel water and microorganisms.
Mucous membranes: These moist linings cover the openings of the body, such as the nose, mouth, eyes, and digestive, respiratory, and urogenital tracts. They produce mucus, a sticky substance that traps pathogens and prevents them from entering the body. Mucus also contains enzymes and antibodies that can kill certain pathogens.
2. Chemical Barrier:
Skin and mucous membranes secrete a variety of substances that have antimicrobial properties. These include: Sebum: Contains fatty acids that can kill bacteria and fungi.
Sweat: Contains salt and lysozyme, an enzyme that can break down bacterial cell walls. Saliva: Contains enzymes that can break down food and kill bacteria.
Gastric acid: The highly acidic environment of the stomach kills most pathogens that are ingested.
3. Immune Barrier:
Skin and mucous membranes are home to a diverse community of microbes, known as the microbiome. These microbes play an important role in protecting against infection by competing with pathogens for resources and space.
Mucous membranes contain specialized immune cells, such as M cells and dendritic cells, that can recognize pathogens and initiate an immune response.
In contrast, the other choices are less effective barriers to infection:
Choice B: Gastrointestinal secretions, such as gastric acid, do play a role in preventing infection, but they are not as effective as skin and mucous membranes. Pathogens can still enter the body through the digestive tract, even in the presence of gastric acid.
Choice C: Colonization by host bacteria can actually help to protect against infection by competing with pathogens. However, it is not a primary barrier to infection.
Choice D: Inflammatory processes are a response to infection, not a barrier to it. They occur after pathogens have already entered the body.
A nurse is providing care for four patients. Which patient should the nurse evaluate first for cognitive impairment?
Explanation
Choice A rationale:
A serum sodium level of 134 mEq/L (134 mmol/L) is mildly low, but this level of hyponatremia is not typically associated with significant cognitive impairment.
Symptoms of hyponatremia, such as confusion, lethargy, and seizures, usually occur when sodium levels are 125 mEq/L or lower.
However, it's important to monitor this patient for any changes in cognitive status as hyponatremia can worsen and lead to more severe symptoms.
Choice C rationale:
A patient who underwent an open cholecystectomy two days ago may experience some cognitive impairment due to the effects of anesthesia and pain medications.
However, this type of impairment is usually temporary and resolves within a few days.
It's important to assess for cognitive impairment in this patient, but it is not the most urgent priority.
Choice D rationale:
A 32-year-old patient with a 20-pack-year history of smoking is at risk for cognitive impairment due to the long-term effects of smoking on the brain.
However, this risk is typically not as immediate as the risk of cognitive impairment following a stroke.
It's important to educate this patient about the risks of smoking and encourage smoking cessation, but it is not the most urgent priority in terms of cognitive assessment.
Choice B rationale:
An 88-year-old patient who had a hemorrhagic stroke three days ago is at the highest risk for cognitive impairment among the given options.
Hemorrhagic stroke involves bleeding in the brain, which can damage brain tissue and lead to cognitive deficits.
The risk of cognitive impairment is particularly high in older adults, as they may have less cognitive reserve to compensate for the damage caused by the stroke.
Early assessment and intervention for cognitive impairment are crucial for optimizing recovery and quality of life in stroke patients.
Prompt evaluation for cognitive impairment is essential to identify any deficits and initiate appropriate interventions to support the patient's cognitive function and recovery.
A 25-year-old patient is admitted to the ambulatory surgery unit to receive two units of whole blood.
The patient has anemia, systemic lupus erythematosus, hypertension, schizophrenia, and primary hypothyroidism.
The patient’s vital signs are BP 100/68, P 110, R 24, T 99.1 °F, O2-97%. The patient reports experiencing shortness of breath with exertion, fatigue, dizziness when standing, and an intolerance to cold temperatures.
Initial labs indicate an Hgb of 6.8, an Hct of 21.2, a CRP of 38, an albumin of 14, and an iron level of 9. The patient’s current medications include hydroxychloroquine 200 mg one BID, amlodipine 10 mg one PO daily, Citalopram 20 mg one PO daily, Lisinopril 20 mg one PO daily, sertraline 50 mg one daily, levothyroxine 75 mg one PO daily, Ferrous sulfate 30 mg one PO TID, and quetiapine 100 mg one PO HS. Which patient assessment findings require immediate follow-up by the nurse at this time? (Select all that apply)
Explanation
Rationale for A: Hemoglobin and Hematocrit
Hemoglobin (Hgb) of 6.8 g/dL is significantly below the normal range of 12-16 g/dL for women and 14-18 g/dL for men. This indicates severe anemia, which can cause several of the patient's reported symptoms, including shortness of breath, fatigue, dizziness, and intolerance to cold. It's crucial to address this promptly as severe anemia can lead to tissue hypoxia and organ damage.
Hematocrit (Hct) of 21.2% is also below the normal range of 36-46% for women and 41-50% for men. Hct measures the percentage of red blood cells in the blood, and its low value further confirms the presence of anemia.
Rationale for B: Blood Pressure 100/68, Respirations 24
Blood pressure of 100/68 mmHg is considered low, especially in a patient with a history of hypertension. This could be due to the anemia, as low red blood cell count can decrease blood volume and subsequently lower blood pressure. It's essential to monitor the patient's blood pressure closely, as hypotension can lead to dizziness, fainting, and even shock.
Respirations of 24 breaths per minute are slightly elevated above the normal adult range of 12-20 breaths per minute. This could be a compensatory mechanism for the anemia, as the body tries to increase oxygen intake. However, it could also indicate other underlying respiratory issues that need to be investigated.
Rationale for F: Shortness of breath with exertion
Shortness of breath (dyspnea) is a common symptom of anemia, as the body struggles to deliver enough oxygen to tissues during physical activity. This symptom warrants immediate attention, as it can significantly impact the patient's quality of life and could potentially signal worsening anemia or other cardiopulmonary problems.
Rationale for G: Dizziness when standing
Dizziness upon standing (orthostatic hypotension) is a sign of low blood pressure, which can be exacerbated by anemia. This can increase the risk of falls and injuries, especially in a patient with other health conditions. It's crucial to address this symptom to prevent potential complications.
Sign Up or Login to view all the 53 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

