Fetal Non-Stress Test (NST) > Maternal & Newborn
Exam Review
Interpretation of results
Total Questions : 4
Showing 4 questions, Sign in for moreA nurse is performing a nonstress test (NST) on a pregnant client at 38 weeks of gestation.
The nurse observes that the fetal heart rate (FHR) increases by 20 beats per minute (bpm) for 20 seconds, twice in a 10-minute period.
How should the nurse interpret this result?
Explanation
This means that the fetal heart rate (FHR) increases by at least 15 beats per minute (bpm) for at least 15 seconds, twice in a 10-minute period.This indicates that the baby is healthy and getting enough oxygen.
Nonreactive.
This means that the FHR does not show the expected accelerations in response to movement.This may indicate that the baby is not well or needs further testing.
Indeterminate.
This means that the FHR shows some accelerations, but not enough to be considered reactive.This may indicate that the baby is asleep or needs more time to show reactivity.
Abnormal.
This means that the FHR shows decelerations, which are drops in the heart rate below the baseline.This may indicate that the baby is in distress or has a problem with the umbilical cord or placenta.
A nurse is reviewing the electronic fetal monitoring (EFM) tracing of a client in active labor.
The nurse notes that the baseline FHR is 150 bpm, with moderate variability and no decelerations.
The nurse also observes that the FHR increases by 25 bpm for 15 seconds, four times in a 20-minute period.
What term is used to describe these FHR changes?
Explanation
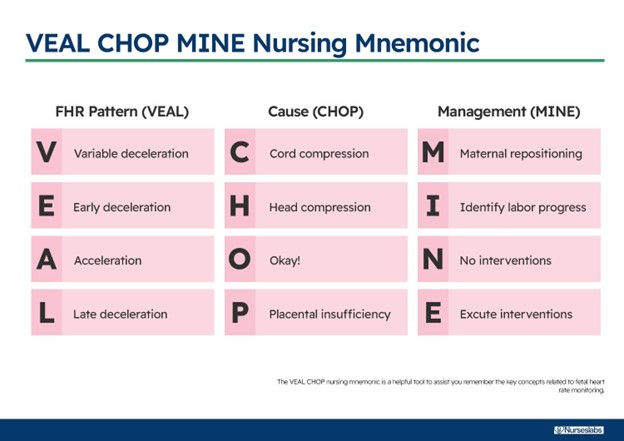
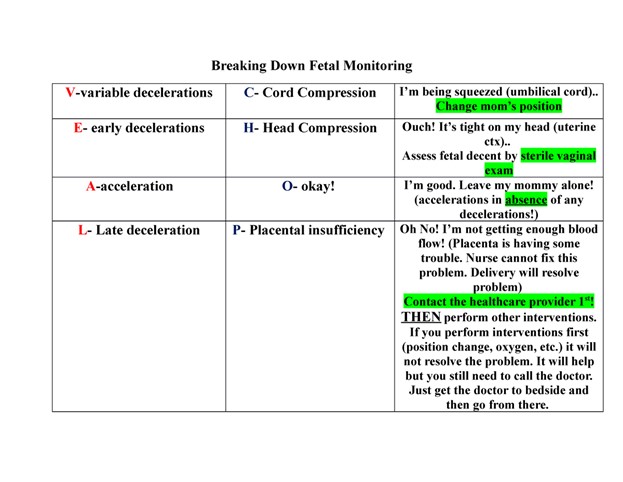
Accelerations.According to the National Institute of Child Health and Human Development (NICHD) terminology, accelerations are defined as transient increases in the FHR of at least 15 bpm above the baseline for at least 15 seconds.Accelerations are a reassuring sign of fetal well-being and oxygenation.
Early decelerations are decreases in the FHR that coincide with the onset and end of a uterine contraction.They are caused by fetal head compression and are usually benign.
Late decelerations are decreases in the FHR that begin after the peak of a uterine contraction and do not return to baseline until after the contraction ends.They are caused by uteroplacental insufficiency and are a sign of fetal hypoxia.
Variable decelerations are abrupt decreases in the FHR that vary in timing.
A nurse is caring for a client who is undergoing an oxytocin (pitocin) infusion for induction of labor.
The nurse notices that the FHR shows a pattern of late decelerations, which are decelerations that begin after the peak of the contraction and return to baseline after the contraction ends.
What is the most likely cause of these decelerations?
Explanation
Uteroplacental insufficiency.Late decelerations are decelerations that begin after the peak of the contraction and return to baseline after the contraction ends.They are caused by inadequate blood flow and oxygen delivery to the fetus through the placenta.This can be due to maternal hypotension, uterine hyperstimulation, placental abruption, or other factors.
Choice A is wrong because fetal head compression causes early decelerations, which are decelerations that begin and end with the contraction.
Choice B is wrong because umbilical cord compression causes variable decelerations, which are abrupt drops in the fetal heart rate that vary in shape and timing.
Choice D is wrong because maternal hypotension can cause uteroplacental insufficiency, but it is not the only cause.Also, maternal hypotension would affect the fetal heart rate baseline, not just the decelerations.
Normal ranges for fetal heart rate are 110 to 160 beats per minute for baseline and 15 beats per minute above or below baseline for variability.
A nurse is assessing a client who is in labor and has meconium-stained amniotic fluid.
The nurse observes variable decelerations on the EFM tracing, which are decelerations that have an abrupt onset and vary in shape, duration, and degree of fall below the baseline FHR.
What is the most appropriate nursing intervention for this situation?
Explanation
Prepare for an amnioinfusion to dilute the meconium and relieve cord compression.
An amnioinfusion is a procedure in which sterile fluid is infused into the uterus through a catheter to increase the volume of amniotic fluid and reduce the risk of fetal distress caused by meconium aspiration or cord compression.
Variable decelerations are a sign of cord compression and can be alleviated by an amnioinfusion.
Choice A is wrong because repositioning the client may not be enough to improve placental blood flow and prevent fetal hypoxia.
Choice B is wrong because administering oxygen to the client may not be sufficient to increase fetal oxygenation if the cord is compressed.
Choice D is wrong because an emergency cesarean delivery may not be necessary if an amnioinfusion can resolve the variable decelerations and improve fetal well-being.
Sign Up or Login to view all the 4 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

