Interprofessional Care of the Client and Family Across the Lifespan II
Total Questions : 119
Showing 25 questions, Sign in for moreWhich statement would be correct for a patient with type 2 diabetes who was admitted to the hospital with pneumonia?
Explanation
Choice A rationale: The patient with type 2 diabetes admitted with pneumonia might not necessarily need insulin therapy to prevent ketoacidosis.
Choice B rationale: Type 2 diabetes doesn't typically involve islet cell antibodies destroying the pancreas's ability to produce insulin.
Choice C rationale: In this scenario, the patient might have enough endogenous insulin to prevent ketosis but could be at risk for hyperosmolar hyperglycemic syndrome due to illness-induced stress.
Choice D rationale: Type 2 diabetes often involves some degree of endogenous insulin secretion, and not all patients require daily insulin injections.
The nurse completes visual inspection of a client's abdomen. What technique should the nurse perform next in the abdominal examination?
Explanation
Choice A rationale: After visual inspection, the next step typically involves auscultation, which allows the nurse to listen for bowel sounds and gather information about
gastrointestinal function.
Choice B rationale: Percussion involves tapping the abdomen to assess density or abnormal masses but usually follows auscultation.
Choice C rationale: Palpation, both light and deep, follows percussion in the sequence of an abdominal examination.
Choice D rationale: Similar to light palpation, deep palpation follows auscultation and percussion in the sequence of an abdominal examination.
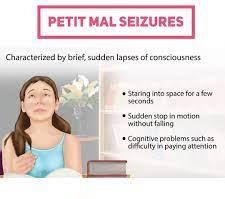
Which type of epileptic seizure is characterized by a sudden lapse of consciousness for 5 to 30 seconds?
Explanation
Choice A rationale: Petit mal seizures, also known as absence seizures, involve a sudden lapse in consciousness for a brief duration, typically 5 to 30 seconds.
Choice B rationale: Clonic seizures involve rhythmic jerking movements.
Choice C rationale: Tonic-clonic seizures involve both tonic (muscle stiffness) and clonic (rhythmic jerking) phases.
Choice D rationale: Tonic seizures involve muscle stiffness but don't usually present as sudden lapses of consciousness in a short duration.
 |
17-year-old male arrives at the emergency department following playing baseball. He slid into a base, felt a 'pop', and had pain in his right ankle.
The client reports pain of 7 out of 10 in his right ankle, which is described as throbbing. Right pedal pulse was 2+, and the sensation was intact.
The client had a limited and painful range of motion in his ankle. Significant swelling and bruising in the ankle were observed.
The emergency department nurse cares for a client with right ankle pain.
Complete the statement below:
While teaching the client how to use crutches, the nurse should instruct the client to ambulate using the _________________ and based on the client ____________ ?
Explanation
Choice A rationale: A three-point gait is used when one leg is weaker or injured and cannot bear weight. The client should place the crutches about 12 inches in front of the feet and lean forward on the crutches. Then, the client should lift the injured leg and
swing the body forward between the crutches, landing on the uninjured leg. The client should not put any weight on the injured ankle, as ordered by the physician.
Choice B rationale: A four-point gait is used when both legs can bear some weight, but one is weaker than the other.
Choice C rationale: A swing-through gait is used when both legs can bear weight, but need assistance with balance and coordination.
Choice D rationale: A two-point gait is used when both legs have equal strength and can bear full weight.
Which of the following patients is most likely experiencing Hyperglycemic Hyperosmolar Nonketotic Syndrome based on their symptoms?
Explanation
Choice A rationale: This may indicate a different condition such as gastroenteritis rather than Hyperglycemic Hyperosmolar Nonketotic Syndrome (HHNS).
Choice B rationale: This is more indicative of diabetic ketoacidosis (DKA) rather than HHNS.
Choice C rationale: A 72-year-old with a history of diabetes, elevated blood glucose, and complaints of thirst and frequent urination might have uncontrolled diabetes, but the absence of severe hyperglycemia and other symptoms specific to HHNS makes this choice less likely.
Choice D rationale: This fits the criteria for HHNS. The infection, missed medication, and extremely high blood glucose levels suggest the possibility of Hyperglycemic Hyperosmolar Nonketotic Syndrome.
The nurse observes a novice nurse caring for a client experiencing status epilepticus. It will require immediate intervention if the novice nurse does which of the following?
Explanation
Choice A rationale: Activates the rapid response team (RRT) - Status epilepticus is a medical emergency requiring immediate intervention. Activating the rapid response team would ensure a prompt response to the situation.
Choice B rationale: Loosens any restrictive clothing - While important for patient safety and comfort, it may not necessarily require immediate intervention in the context of managing status epilepticus.
Choice C rationale: Places the client in a lateral position - This is a recommended positioning to prevent aspiration during a seizure but might not constitute immediate intervention.
Choice D rationale: Prepares to administer intravenous valproate acid - While administering medication might be necessary, activating the rapid response team takes precedence for immediate intervention in status epilepticus.
A client arrives at the clinic with his daughter, reporting memory impairments:
Which of the following clinical feature are consistent with delirium? Select all that apply?
Explanation
Choice A rationale: Altered consciousness is a hallmark feature of delirium, where individuals may experience fluctuations in awareness.
Choice B rationale: Delirium typically has an acute onset rather than symptoms developing over months to years.
Choice C rationale: Delirium often has a fluctuating course, rather than a consistent progressive decline.
Choice D rationale: Delirium can result from various factors including fluid/electrolyte imbalances or infections.
Choice E rationale: While these conditions might contribute to cognitive impairments, they are not typically associated with delirium.
Choice F rationale: Delirium can affect judgment, but it's not a defining feature.
Choice G rationale: While memory impairments can be seen in delirium, they're often accompanied by altered consciousness and fluctuations in awareness.
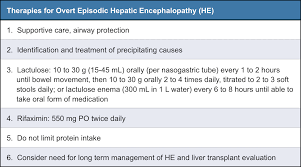
The nurse is caring for a client who has ascites and hepatic encephalopathy. Which of the following prescriptions should the nurse clarify with the primary healthcare provider (PHCP)?
Explanation
Choice A rationale: Used in the management of hepatic encephalopathy by reducing the production of ammonia in the gut.
Choice B rationale: Often prescribed to reduce ammonia levels in hepatic encephalopathy by promoting bowel movements and aiding ammonia excretion. Choice C rationale: Typically used in managing ascites by reducing fluid retention and treating edema.
Choice D rationale: This medication can potentially worsen hepatic encephalopathy due to its sedative effects and impact on mental function. It's crucial to clarify its use in a patient with hepatic encephalopathy.
A nurse is caring for a client with a new diagnosis of Paget's disease. The nurse anticipates the provider will prescribe which of the following medications for this client?
Explanation
Choice A rationale: Used primarily for gout and familial Mediterranean fever, not for Paget's disease.
Choice B rationale: Alendronate is a bisphosphonate commonly used to manage Paget's disease by slowing down bone breakdown and reducing the risk of complications.
Choice C rationale: Prednisone is a corticosteroid used for various inflammatory conditions but not typically prescribed for Paget's disease.
Choice D rationale: Used to lower uric acid levels and prevent gout attacks, not a primary medication for Paget's disease.
A nurse notes that a client's serum potassium level is 5.9 mEq/L. The nurse interprets this as an expected finding in the client with:
Explanation
Choice A rationale: Typically associated with potassium depletion rather than elevated levels.
Choice B rationale: Furosemide, a loop diuretic, can cause potassium depletion leading to hypokalemia, but it might also cause transient elevations in potassium levels initially. Choice C rationale: Addison disease can cause hyperkalemia, or high potassium, due to decreased renal excretion of potassium and increased retention of sodium and water.
Choice D rationale: Cushing disease can cause hypokalemia, or low potassium, due to increased renal excretion of potassium and decreased reabsorption of sodium and water.
A 25-year-old female presents with amenorrhea and hirsutism and is diagnosed with polycystic ovary syndrome (PCOS). Lab testing will most likely reveal:
Explanation
Choice A rationale: PCOS is not typically associated with genetic cancerous mutations.
Choice B rationale: Insulin resistance and hyperinsulinemia are commonly associated with PCOS, contributing to its pathophysiology.
Choice C rationale: While cortisol abnormalities can cause similar symptoms, it's not a primary finding in PCOS.
Choice D rationale: PCOS often involves hormonal imbalances, but it's not characterized by an estrogen deficit.
A female client has just been diagnosed with condylomata acuminata (genital warts).
What information is appropriate to tell this client?
Explanation
Choice A rationale: Metronidazole is not typically used to treat genital warts caused by HPV.
Choice B rationale: HPV can be transmitted through various forms of sexual contact, including oral sex.
Choice C rationale: Condoms reduce but do not eliminate the risk of HPV transmission. Choice D rationale: Genital warts caused by HPV increase the risk of cervical cancer,
necessitating regular Pap smears for monitoring and early detection.
Nurse Lily is assessing a male client diagnosed with gonorrhea. Which symptom most likely prompted the client to seek medical attention?
Explanation
Choice A rationale: This symptom typically indicates secondary syphilis, not gonorrhea.
Choice B rationale: Warts on the genitals suggest a different sexually transmitted infection caused by HPV, not gonorrhea.
Choice C rationale: A discharge from the penis is a common symptom of gonorrhea and often prompts individuals to seek medical attention.
Choice D rationale: While discomfort can be associated with gonorrhea, the primary presenting symptom often involves discharge rather than specific lesions.

The RN is serving as preceptor to a new graduate nurse who has recently passed the RN licensure (NCLEX®) examination. The new nurse has only been on the unit for 2 days. Which patient should be assigned to the new graduate nurse?
Explanation
Choice A rationale: Cellulitis management typically involves wound care, antibiotics, and monitoring. It's a suitable assignment for a new graduate nurse to begin learning about wound management and diabetic care.
Choice B rationale: Post-operative care for an amputation requires experience in assessing and managing post-surgical complications, which might not be suitable for a new graduate nurse.
Choice C rationale: Diabetic ketoacidosis management involves complex insulin therapy and critical care, which might be overwhelming for a new graduate nurse.
Choice D rationale: While hyperglycemia requires monitoring and intervention, the cause and severity need to be determined before assigning this patient to a new
graduate nurse.
The client is brought to the ER after falling off a roof and landing on his back. A T4 spinal fracture is diagnosed. The client's blood pressure is 74/40 mmHg, pulse is 55/min, and skin is pink and dry. What of the following nursing actions is a priority?
Explanation
Choice A rationale: Although important to assess for potential kidney injury, addressing hypotension due to potential spinal shock takes priority.
Choice B rationale: Important for determining any neurological deficits, but addressing hypotension is the initial priority.
Choice C rationale: Hypotension indicates potential spinal shock or hemorrhagic shock, and fluid resuscitation is the immediate priority to stabilize the client's blood pressure.
Choice D rationale: While important for assessing cardiac status, addressing hypotension takes precedence to stabilize the client's condition.
The nurse is reviewing the record of a female client with Crohn's disease. Which stool characteristics should the nurse expect to note documented in the client's record?
Explanation
Choice A rationale: Not a typical characteristic of Crohn's disease; more associated with conditions like rectal fistulas.
Choice B rationale: Crohn's disease commonly involves diarrhea rather than chronic constipation.
Choice C rationale: A common symptom of Crohn's disease due to inflammation and malabsorption in the intestines.
Choice D rationale: Crohn's disease typically presents with diarrhea but not necessarily alternating with constipation. Constipation alternating with diarrhea may also occur in irritable bowel syndrome.
After reviewing the laboratory reports of a client, a nurse finds that the client has chronic pelvic inflammatory disorder (PID). Which condition should the nurse anticipate in the client?
Explanation
Choice A rationale: PID is not associated with meningitis, which is an infection or inflammation of the meninges.
Choice B rationale: Chronic PID typically involves long-term inflammation of the pelvic organs, including the fallopian tubes and ovaries.
Choice C rationale: This condition refers to genital warts caused by HPV, not directly related to PID.
Choice D rationale: Dysplasia refers to abnormal cell growth or development and isn't directly associated with PID.
Which antidiabetic medication is a sulfonylurea?
Explanation
Choice A rationale: Metformin belongs to the biguanide class of antidiabetic medications.
Choice B rationale: Pioglitazone is a thiazolidinedione used to treat diabetes, not a sulfonylurea.
Choice C rationale: Glipizide is a sulfonylurea used to stimulate insulin secretion in type 2 diabetes.
Choice D rationale: Repaglinide is a meglitinide, another class of drugs that stimulates insulin release.
 |
While reviewing the clinical history of a client with brain injury, the nurse finds that there is a periorbital ecchymosis, which is referred to as raccoon eyes. The client also has leakage of cerebrospinal fluid (CSF) from the nose. Which fracture should the nurse suspect in the client?
Explanation
Choice A rationale: Often results from direct trauma to the skull, but not typically associated with CSF leakage or raccoon eyes.
Choice B rationale: Basilar skull fractures, particularly involving the anterior or middle fossa, can lead to CSF leakage from the nose (rhinorrhea) and periorbital ecchymosis (raccoon eyes).
Choice C rationale: A simple fracture line without displacement, less likely to cause CSF leakage and raccoon eyes.
Choice D rationale: Less commonly associated with CSF leakage and periorbital ecchymosis compared to basilar skull fractures.
A client is brought to the hospital because of severe abdominal pain, nausea, and vomiting. The client reports increased pain in the abdomen and in the epigastric region radiating to the back when lying supine. Upon physical assessment, the nurse finds that the client has fever and hypotension.
What should the nurse infer from these findings?
Explanation
Choice A rationale: Symptoms and findings described align more with an acute, severe condition rather than a chronic one.
Choice B rationale: While cholecystitis can present with similar symptoms, the radiation of pain to the back is more indicative of a different condition.
Choice C rationale: Cholelithiasis (gallstones) might cause abdominal pain but typically doesn’t lead to fever and hypotension.
Choice D rationale: Symptoms including severe abdominal pain, radiation to the back, fever, and hypotension suggest acute pancreatitis, a potentially serious condition requiring urgent medical attention.
Jane, a 20-year old college student is admitted to the hospital with a tentative diagnosis of myasthenia gravis. She is scheduled to have a series of diagnostic studies for myasthenia gravis, including a Tensilon test. In preparing her for this procedure, the nurse explains that her response to the medication will confirm the diagnosis if Tensilon produces:
Explanation
Choice A rationale: The Tensilon test involves injecting edrophonium, and in myasthenia gravis, temporary improvement in muscle strength confirms the diagnosis by demonstrating increased acetylcholine activity at the neuromuscular junction.
Choice B rationale: This describes the pathophysiology of myasthenia gravis but doesn’t directly confirm the diagnosis via the Tensilon test.
Choice C rationale: While this may be seen in myasthenia gravis, the Tensilon test specifically aims to observe improved muscle strength after administration.
Choice D rationale: While the presence of these antibodies is a characteristic of myasthenia gravis, the Tensilon test is used to assess the immediate response to the medication for diagnostic confirmation.
A patient with gonorrhea is treated with a single IM dose of ceftriaxone and is given a prescription for azithromycin (Zithromax) 1000 mg 1 dose. What rationale should the nurse provide to the patient for this combination?
Explanation
Choice A rationale: The combination treats gonorrhea and chlamydia but not trichomonas.
Choice B rationale: While important, this combination aims to treat multiple potential infections, not solely prevent reinfection.
Choice C rationale: The dual therapy doesn’t cover syphilis; it's specifically targeted for gonorrhea and chlamydia.
Choice D rationale: Azithromycin covers both gonorrhea and chlamydia, so the combination ensures coverage for both possible infections.
A 21-year-old college student has come to see the nurse practitioner for treatment of a vaginal infection. Physical assessment reveals inflammation of the vagina and vulva, and vaginal discharge has a cottage cheese appearance. These findings are consistent with:
Explanation
Choice A rationale: candidiasis - The described symptoms of inflammation, cottage
cheese-like discharge, and vaginal/vulvar inflammation are indicative of a yeast infection or candidiasis.
Choice B rationale: Chlamydia - Chlamydia often presents with different symptoms such as discharge, but it's not typically associated with a cottage cheese-like appearance.
Choice C rationale: bacterial vaginosis - Bacterial vaginosis typically presents with a different type of discharge, often described as "fishy" smelling, rather than a cottage cheese appearance.
Choice D rationale: trichomoniasis - Symptoms of trichomoniasis usually include frothy, malodorous discharge, not consistent with the described cottage cheese-like discharge.
The nurse is preparing a teaching plan for a client who is newly diagnosed with Type 1 diabetes mellitus. Which signs and symptoms should the nurse describe when teaching the client about hypoglycemia?
Explanation
Choice A rationale: These symptoms are more indicative of diabetic ketoacidosis, not hypoglycemia.
Choice B rationale: Symptoms of increased urination, thirst, and hunger are more associated with hyperglycemia, not hypoglycemia.
Choice C rationale: These are classic signs of hypoglycemia and should be described to the client for early recognition and intervention.
Choice D rationale: These symptoms can occur in hypoglycemia but are less specific compared to sweating, cold, trembling, and tachycardia.
A nurse in a clinic is assessing a client. Which of the following findings should the nurse identify as a risk factor for osteoporosis?
Explanation
Choice A rationale: Smoking is a risk factor for osteoporosis as it can interfere with calcium absorption and decrease bone density.
Choice B rationale: Moderate alcohol consumption isn't a significant risk factor for osteoporosis.
Choice C rationale: Generally, having a larger body stature is not considered a significant risk factor for osteoporosis.
Choice D rationale: While fractures during childhood can affect bone health, they might not necessarily predict osteoporosis risk in adulthood.
Sign Up or Login to view all the 119 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

