Anti-inflammatory and Immunosuppressive Drugs > Pharmacology
Exam Review
Introduction
Total Questions : 5
Showing 5 questions, Sign in for moreA nurse is caring for a client who has rheumatoid arthritis and is prescribed prednisone, a glucocorticoid. What is the primary mechanism of action of prednisone in this condition?
Explanation
A. It inhibits the synthesis of inflammatory mediators and suppresses the activation and proliferation of immune cells.
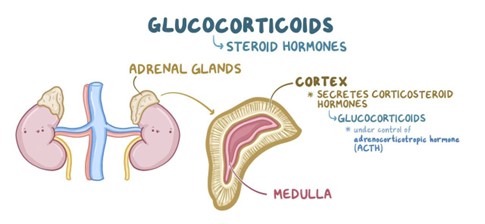
Prednisone is a synthetic glucocorticoid that mimics the natural hormone cortisol, which is produced by the adrenal cortex. Cortisol has potent anti-inflammatory and immunosuppressive effects by inhibiting the synthesis of inflammatory mediators such as prostaglandins, leukotrienes, histamine, cytokines, and adhesion molecules, and by suppressing the activation and proliferation of lymphocytes, macrophages, eosinophils, and mast cells. These effects reduce the immune-mediated damage to the self-tissues in autoimmune diseases such as rheumatoid arthritis.
The other options are wrong because:
B. It blocks the activation of T cells by inhibiting the enzyme calcineurin, which is required for the transcription of interleukin-2.
This option is wrong because it describes the mechanism of action of calcineurin inhibitors, not glucocorticoids. Calcineurin inhibitors are a type of immunosuppressant that target T cells specifically, while glucocorticoids have a broader effect on various immune cells and inflammatory mediators.
C. It interferes with the synthesis of nucleic acids, which are essential for the replication and function of immune cells.
This option is wrong because it describes the mechanism of action of antimetabolites, not glucocorticoids. Antimetabolites are a type of immunosuppressant that interfere with the synthesis of nucleic acids, which are the building blocks of DNA and RNA. This affects the replication and function of immune cells, as well as other rapidly dividing cells such as cancer cells.
D. It binds to specific antigens or receptors on the surface of immune cells and either neutralizes them or induces their destruction.
This option is wrong because it describes the mechanism of action of monoclonal antibodies, not glucocorticoids. Monoclonal antibodies are a type of immunosuppressant that bind to specific antigens or receptors on the surface of immune cells and either neutralize them or induce their destruction. This can prevent the activation or function of immune cells that are involved in transplant rejection or autoimmune diseases.
A nurse is administering ibuprofen, a nonselective COX inhibitor, to a client who has osteoarthritis. What are the expected pharmacologic effects of ibuprofen in this condition?
Explanation
This is because ibuprofen is a nonselective COX inhibitor, which means it blocks both COX-1 and COX-2 enzymes². COX-1 is responsible for producing prostaglandins that protect the gastric mucosa, regulate platelet aggregation, and maintain renal function². COX-2 is responsible for producing prostaglandins that mediate inflammation, pain, and fever². Therefore, by inhibiting both COX-1 and COX-2, ibuprofen reduces inflammation, pain, fever, and gastric mucosal protection by blocking the production of prostaglandins.
The other options are incorrect because:
A. It reduces inflammation, pain, fever, and platelet aggregation by blocking the production of prostaglandins.
This is incorrect because ibuprofen also blocks the production of prostaglandins that regulate platelet aggregation. Therefore, ibuprofen can increase the risk of bleeding by inhibiting platelet function².
C. It reduces inflammation, pain, fever, and sodium retention by blocking the production of prostaglandins.
This is incorrect because ibuprofen also blocks the production of prostaglandins that maintain renal function. Therefore, ibuprofen can cause sodium and water retention by impairing renal perfusion and glomerular filtration².
D. It reduces inflammation, pain, fever, and bronchoconstriction by blocking the production of prostaglandins.
This is incorrect because ibuprofen also blocks the production of prostaglandins that mediate bronchodilation. Therefore, ibuprofen can cause bronchoconstriction by shifting the balance between prostanoids and leukotrienes in favor of leukotrienes².
A nurse is teaching a client who has Crohn's disease and is prescribed azathioprine, an antimetabolite. What should the nurse include in the teaching?
Explanation
This is because azathioprine can affect the production of blood cells in your bone marrow, which are essential for fighting infections and clotting blood². Therefore, you may have a higher chance of getting infections or bleeding more easily while taking this drug. You should monitor your blood counts regularly and report any signs of infection (such as fever, sore throat, cough) or bleeding (such as bruising, nosebleeds, blood in urine or stool) to your doctor².
The other options are incorrect because:
B. The drug may cause nephrotoxicity and increase the risk of renal impairment and electrolyte imbalances.
This is incorrect because azathioprine is not known to cause nephrotoxicity or damage to the kidneys². However, some other drugs that are used to treat IBD, such as mesalazine or sulfasalazine, may have this effect³. Therefore, you should have your kidney function checked before starting these drugs and periodically during treatment³.
C. The drug may cause neurotoxicity and increase the risk of tremor, headache, and seizures.
This is incorrect because azathioprine is not known to cause neurotoxicity or damage to the nervous system². However, some other drugs that are used to treat IBD, such as metronidazole or ciprofloxacin, may have this effect³. Therefore, you should report any signs of neurological problems (such as numbness, tingling, weakness, vision changes, confusion) to your doctor³.
D. The drug may cause hepatotoxicity and increase the risk of liver impairment and jaundice.
This is incorrect because azathioprine is not known to cause hepatotoxicity or damage to the liver². However, some other drugs that are used to treat IBD, such as methotrexate or 6-mercaptopurine, may have this effect³. Therefore, you should have your liver function checked before starting these drugs and periodically during treatment³.
A nurse is monitoring a client who has asthma and is receiving fluticasone, a corticosteroid, by inhalation. What are some of the adverse effects that the nurse should watch for?
Explanation
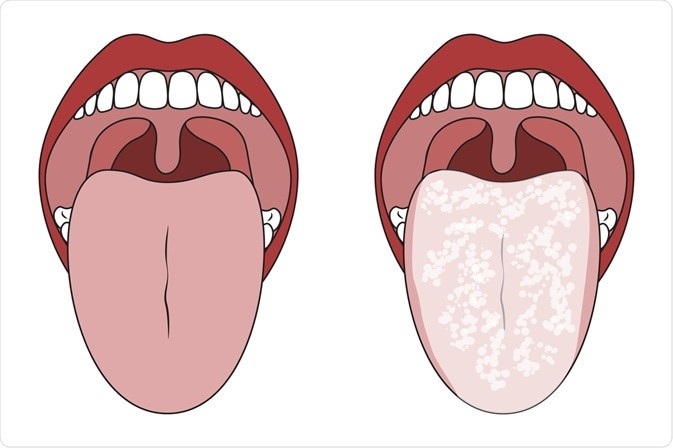
This is because fluticasone inhalation can cause local side effects in the mouth and throat, such as oral candidiasis (thrush), hoarseness, cough, and dysphonia (voice changes)²³. These side effects are more likely to occur if the dose is high, the duration of treatment is long, or the inhaler technique is poor². To prevent or reduce these side effects, the nurse should instruct the client to rinse the mouth with water after each use of the inhaler, use a spacer device if possible, and check the inhaler technique regularly². Fluticasone is a corticosteroid that is used to treat asthma and other respiratory conditions by reducing inflammation and swelling in the airways¹. It can be administered by inhalation using an aerosol or a powder device.
The other options are incorrect because:
A. Hyperglycemia, osteoporosis, glaucoma, and cataracts
This is incorrect because these are systemic side effects of corticosteroids that are more likely to occur with oral or injectable forms of the drug². Fluticasone inhalation has a low systemic absorption and a high first-pass metabolism, which means that only a small amount of the drug reaches the bloodstream and most of it is broken down in the liver before it can cause systemic effects¹. Therefore, these side effects are rare with fluticasone inhalation².
B. Hypoglycemia, osteomalacia, myopia, and dry eyes
This is incorrect because these are not known side effects of fluticasone inhalation or corticosteroids in general². Hypoglycemia (low blood sugar) is more likely to occur with drugs that lower blood glucose levels, such as insulin or oral antidiabetic agents⁴. Osteomalacia (softening of the bones) is more likely to occur with drugs that affect vitamin D metabolism, such as anticonvulsants or antiretrovirals⁵. Myopia (nearsightedness) and dry eyes are more likely to occur with drugs that affect the eye muscles or tear production, such as antihistamines or anticholinergics⁶.
D. Oral ulcers, dysphagia, wheeze, and dyspnea
This is incorrect because these are not common side effects of fluticasone inhalation or corticosteroids in general². Oral ulcers (sores in the mouth) are more likely to occur with drugs that irritate the mucous membranes, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or chemotherapy agents. Dysphagia (difficulty swallowing) is more likely to occur with drugs that affect the esophageal motility or sphincter function, such as calcium channel blockers or antipsychotics. Wheeze (a high-pitched sound when breathing) and dyspnea (shortness of breath) are more likely to occur with drugs that cause bronchoconstriction or respiratory depression, such as beta blockers or opioids.
A nurse is evaluating a client who has ulcerative colitis and is receiving infliximab, a monoclonal antibody. What are some of the outcomes that indicate the effectiveness of the therapy?
Explanation
Infliximab is a monoclonal antibody that is used to treat ulcerative colitis and other inflammatory conditions by blocking the action of tumor necrosis factor-alpha (TNF-α), a cytokine that causes inflammation and tissue damage in the gut¹. It can be given intravenously every 8 weeks as a maintenance therapy for moderate to severe ulcerative colitis¹. However, it can also have some potential benefits and risks that the nurse should monitor.
The correct answer to your question is:
D. All of the above
This is because infliximab can improve the clinical outcomes of ulcerative colitis in several ways, such as:
A. Decreased frequency and severity of diarrhea, abdominal pain, and rectal bleeding:
These are the main symptoms of ulcerative colitis that affect the quality of life of patients. Infliximab can reduce these symptoms by healing the inflammation and ulcers in the colon and rectum. Several studies have shown that infliximab can induce and maintain clinical remission, response, and mucosal healing in patients with moderate to severe ulcerative colitis who are refractory to conventional therapies²³⁴.
B. Increased appetite, weight gain, energy level, and quality of life:
These are the secondary outcomes of ulcerative colitis that reflect the nutritional status and well-being of patients. Infliximab can improve these outcomes by reducing the systemic effects of inflammation, such as malabsorption, anemia, fatigue, and fever. Several studies have shown that infliximab can improve the health-related quality of life, nutritional status, and functional status of patients with moderate to severe ulcerative colitis²³⁴.
C. Normalized stool culture, blood count, electrolytes, and liver function tests:
These are the laboratory tests that indicate the severity and complications of ulcerative colitis. Infliximab can normalize these tests by reducing the bacterial translocation, blood loss, dehydration, and liver involvement that may occur in ulcerative colitis. Several studies have shown that infliximab can improve the stool culture, hemoglobin, albumin, C-reactive protein, and liver enzymes of patients with moderate to severe ulcerative colitis²³⁴.
Sign Up or Login to view all the 5 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

