Ivytech Community college Lawrence campus paediatric exam
Total Questions : 38
Showing 25 questions, Sign in for moreThe nurse is caring for a 16-year-old child with a diagnosis of acquired immunodeficiency syndrome (AIDS). What treatment goal has the highest priority for this child?
Explanation
A. Preventing spread of infection:
This is a priority because individuals with acquired immunodeficiency syndrome (AIDS) have a compromised immune system. Preventing the spread of infections is crucial to avoid additional complications and safeguard the individual's health.
B. Maintaining skin integrity:
Skin integrity is important for overall health, but in the context of AIDS, preventing infections and promoting immune function take precedence over maintaining skin integrity. Skin issues might be secondary to the immune system's compromised state.
C. Improving nutrition:
Good nutrition is important for overall health, including supporting the immune system. However, preventing the spread of infection is more immediate and critical in the case of someone with AIDS. Addressing nutritional needs can be part of the overall care plan but might be secondary to preventing infections.
D. Promoting comfort:
While promoting comfort is essential in nursing care, the priority in the case of a child with AIDS would be preventing the spread of infection due to the immunocompromised state. Comfort measures may be incorporated into the care plan, but they would not take precedence over preventing further health complications.
A 6-month-old boy weighed 8 lbs. 2 oz. at birth. Understanding developmental milestones, what should the nurse caring for the child calculate his current weight as?
Explanation
A. Approximately 18 lbs. 6 oz.:
This option represents an overestimation of the expected weight. Doubling the birth weight of 8 lbs. 2 oz. would be 16 lbs. 4 oz., so this choice is higher than the expected weight.
B. Approximately 14 lbs. 8 oz.:
This option represents an underestimation of the expected weight. Doubling the birth weight of 8 lbs. 2 oz. would be 16 lbs. 4 oz., so this choice is lower than the expected weight.
C. Approximately 24 lbs. 4 oz.:
This option represents a significant overestimation of the expected weight. Doubling the birth weight of 8 lbs. 2 oz. would be 16 lbs. 4 oz., so this choice is much higher than the expected weight.
D. Approximately 16 lbs. 4 oz.:
This option is the correct estimate based on doubling the birth weight of 8 lbs. 2 oz. It accurately reflects the expected weight of a 6-month-old child according to developmental milestones.
A nurse is assisting with a parenting class and is approached by a parent of a 2-year-old toddler who asks what to do when the toddler throws a tantrum. Which of the following instructions should the nurse give?
Explanation
A. Calmly tell the child to stop:
While remaining calm is important, simply telling the child to stop might not be effective during a tantrum. Toddlers experiencing a meltdown might not respond immediately to verbal commands.
B. Distract the child by buying a toy:
Using material objects to distract a child during a tantrum might reinforce the behavior by rewarding it with something desired. It's also not always feasible to buy a toy instantly.
C. Appear to ignore them:
This strategy might involve not engaging directly with the tantrum, which could sometimes help to de-escalate the situation. However, it's crucial to ensure the child is in a safe environment and to offer support if necessary.
D. Place the child in time-out for 3 min:
Time-out can be a useful method for calming down a child. However, its effectiveness depends on the child's age, temperament, and the consistency of applying this method. Time-out might not be suitable for all children, especially for a 2-year-old who might not fully understand the concept.
The nurse is caring for a toddler with acute laryngotracheobronchitis. Which action aids in bronchodilation to improve breathing for this child?
Explanation
A. Teaching the child to take long, slow breaths:
While teaching slow breathing techniques can be helpful in managing anxiety and promoting a sense of calm, it may not directly address the underlying airway inflammation and bronchodilation needed in acute laryngotracheobronchitis.
B. Assisting with racemic epinephrine nebulizer therapy:
Racemic epinephrine is a medication that contains epinephrine, a bronchodilator. Nebulizer therapy with racemic epinephrine helps reduce airway inflammation, allowing for bronchodilation and improved breathing. This is a common intervention for managing acute respiratory distress in conditions like croup.
C. Administering an oral analgesic:
Oral analgesics, such as pain medications, can provide relief from discomfort or pain, but they do not directly address the bronchodilation needed for conditions like acute laryngotracheobronchitis.
D. Administering a corticosteroid:
Corticosteroids have anti-inflammatory properties and can help reduce swelling and inflammation in the airways. By doing so, they contribute to bronchodilation and improved breathing in conditions like croup. Corticosteroids are often used as part of the treatment plan for acute laryngotracheobronchitis.
A mother brings a 15-month-old child to the clinic for a routine health maintenance visit. Which immunization should the nurse prepare to administer to this child?
Explanation
A. Measles, Mumps, and Rubella (MMR):
The first dose of the MMR vaccine is usually administered around 12-15 months of age. Therefore, this vaccine is appropriate for a 15-month-old child's routine health visit.
B. Pneumococcal:
The pneumococcal vaccine is typically given in several doses, with one of the doses recommended around 12-15 months. It's part of the routine immunization schedule for this age range.
C. Meningococcal:
Meningococcal vaccines are not usually part of the routine schedule at 15 months of age unless there are specific risk factors or circumstances that necessitate this vaccination.
D. Rotavirus (RV):
The rotavirus vaccine is administered in multiple doses, usually starting at around 2 months and completing before 8 months of age. By 15 months, the child should have completed the recommended doses.
The nurse is meeting with a group of caregivers of adolescents and discussing sex and sexuality, including how to discuss these issues with their children. Which comment should the nurse prioritize with this group of caregivers?
Explanation
A. Internet resources, movies, and television have the most accurate and current information for your adolescent to learn about sexuality issues:
This statement may not be accurate, as the internet, movies, and television can sometimes provide misinformation or biased perspectives. It's crucial to emphasize the importance of reliable and evidence-based sources when adolescents seek information about sexuality.
B. Being honest and straightforward with teenagers will encourage them to ask about subjects like sexuality:
This statement is valuable as it emphasizes open communication. Being honest and straightforward creates an environment where adolescents feel comfortable approaching their caregivers with questions or concerns about sexuality. It promotes trust and a supportive relationship.
C. Most schools have excellent programs to teach adolescents about sex and sexuality:
While some schools do have comprehensive sex education programs, the quality of these programs can vary. Additionally, the involvement of parents and caregivers in discussions about sex and sexuality is essential. Relying solely on school programs may not cover all aspects, and caregivers play a crucial role in reinforcing positive attitudes and values.
D. Teenagers spend so much time with their peers, and that is usually how they find out about sex:
While it's true that peers can influence adolescents, relying solely on peer influence for information about sex may not provide accurate or comprehensive knowledge. Caregivers should aim to create an open and honest dialogue to supplement information from peers and address any misconceptions.
A breast-feeding mother asks the nurse about when she can begin feeding her 5-month-old infant some solids and vitamins. Which information provided by the nurse would most accurately address this mother’s concerns?
Explanation
A. At 6 months, you need to quit breast-feeding because he is not getting enough iron or Vitamin C and D and that should help him transition to solids better:
This statement is incorrect. Breastfeeding is recommended for the first six months, and then complementary foods can be introduced while continuing breastfeeding. Breast milk is a primary source of nutrition, and iron and vitamins are typically supplemented as needed.
B. The first food offered to an infant is iron-enriched rice cereal and can be started now. Additionally, the infant needs to receive Vitamin D and iron:
This statement is accurate. Iron-enriched rice cereal is often recommended as a first solid food for infants, and vitamin D supplementation is commonly advised, especially for breastfed infants, as breast milk may not provide enough vitamin D.
C. If you give him one or two bottles of juice each day, he should get all the vitamins he needs. You can begin fruits and cereal in 1 month:
This statement is not recommended. Juice is not recommended for infants, especially in large quantities, as it can interfere with proper nutrition and contribute to dental issues. Also, introducing fruits and cereals should be done gradually, following appropriate guidelines.
D. You can begin feeding the infant fruits and vegetables now followed by iron-enriched cereal to ensure that he gets enough iron:
While introducing fruits and vegetables is a part of introducing solids, iron-enriched cereal is often recommended earlier as a source of iron. The recommendation for iron-enriched rice cereal aligns more with the typical guidance for introducing solids to infants.
The student nurse is collecting data on a child diagnosed with cystic fibrosis and notes the child has a barrel chest and clubbing of the fingers. In explaining this manifestation of the disease, the staff nurse explains the cause of this symptom to be:
Explanation
A. High sodium chloride concentration in the sweat:
Cystic fibrosis is characterized by abnormally thick and sticky mucus in various organs, including the respiratory and digestive systems. However, high sodium chloride concentration in the sweat is a diagnostic feature of cystic fibrosis. This doesn't directly explain the barrel chest and clubbing of the fingers.
B. Chronic lack of oxygen:
Chronic lack of oxygen (chronic hypoxia) is more directly related to the development of clubbing of the fingers and certain respiratory symptoms. In conditions like cystic fibrosis, impaired lung function can lead to inadequate oxygenation, contributing to this manifestation.
C. Decreased respiratory capacity:
This is the correct explanation. Decreased respiratory capacity, often due to the chronic respiratory issues associated with cystic fibrosis, can result in a barrel chest (increased chest diameter due to air trapping) and clubbing of the fingers (a sign of chronic hypoxia).
D. Impaired digestive activity:
While impaired digestive activity is another characteristic of cystic fibrosis, it is not directly linked to the barrel chest or clubbing of the fingers. Digestive issues in cystic fibrosis are primarily related to the thickening of mucus in the pancreas, leading to difficulties in digesting and absorbing nutrients.
The nurse has brought a group of preschoolers to the playroom to play. Which activity would the nurse predict the children to become involved in?
Explanation
A. Painting pictures in the art corner of the room:
Painting pictures in the art corner can be a fun and creative activity for preschoolers. It allows them to express themselves through art and develop fine motor skills. However, it might not be a group activity unless they are sharing materials and ideas.
B. Watching a movie with other children their age:
Watching a movie can be an enjoyable activity for preschoolers, especially if the content is age-appropriate. However, it is a passive activity, and group interactions might be limited during the movie.
C. Playing a board game:
Playing a board game can be a good group activity that involves turn-taking, following rules, and social interaction. However, some board games may be more suitable for older children who have developed certain cognitive and social skills.
D. Pretending to be mommies and daddies in the playhouse:
Pretend play, such as pretending to be mommies and daddies in a playhouse, is a developmentally appropriate and common activity for preschoolers. It encourages imaginative play, role-playing, and social interaction, helping with emotional and social development.
A child comes to the clinic for evaluation of skin lesions and is diagnosed with impetigo. Which of the following medications would the nurse anticipate the physician might prescribe?
Explanation
A. Tetracycline:
Tetracycline antibiotics, such as doxycycline or minocycline, can be effective against the bacteria that cause impetigo. However, their use in children, especially younger ones, might be limited due to concerns about potential effects on developing teeth and bones. Therefore, they are not the first-line choice for pediatric impetigo.
B. Penicillin:
Penicillin or other antibiotics in the penicillin family, such as dicloxacillin or amoxicillin, are commonly used to treat impetigo caused by Streptococcus pyogenes. Penicillin-based antibiotics are effective against certain strains of the bacteria responsible for impetigo. They are often a preferred choice for pediatric impetigo.
C. Metronidazole:
Metronidazole is an antibiotic with activity against anaerobic bacteria and certain parasites. However, it is not typically used to treat impetigo caused by Staphylococcus aureus or Streptococcus pyogenes.
D. Lindane:
Lindane is an anti-parasitic medication used for conditions like scabies or lice. It is not effective against the bacteria that cause impetigo. Lindane is not an appropriate treatment for impetigo, and its use is limited due to potential neurotoxicity.
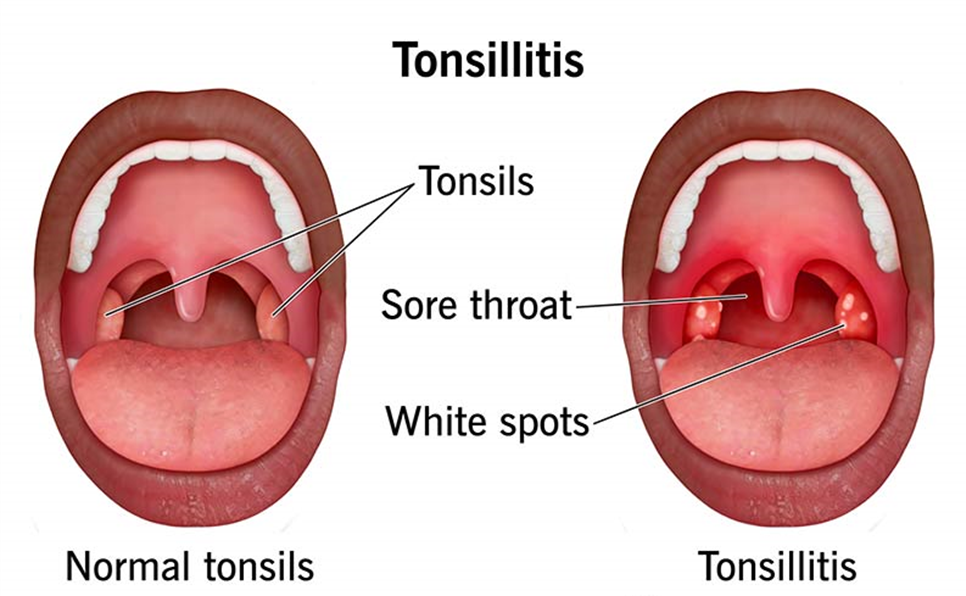
The nurse is collecting data on a child with a diagnosis of tonsillitis. Which clinical manifestation would likely have been noted in the child with this diagnosis?
Explanation
A. Inability to make audible voice sounds:
This symptom is more indicative of conditions affecting the vocal cords or larynx, such as laryngitis. Tonsillitis primarily involves inflammation of the tonsils and may not directly impact the ability to make audible voice sounds.
B. Erythema of the pharynx:
Erythema (redness) of the pharynx is a common manifestation of tonsillitis. Inflammation of the tonsils and surrounding areas can lead to redness and swelling in the throat.
C. Bark-like cough:
A bark-like cough is often associated with croup, which involves inflammation of the larynx and trachea, not the tonsils. It is a distinct condition from tonsillitis.
D. Hoarseness:
Hoarseness can be a symptom of various conditions affecting the vocal cords or larynx, but it is not a typical manifestation of tonsillitis. Tonsillitis is more commonly associated with sore throat, difficulty swallowing, and erythema of the pharynx.
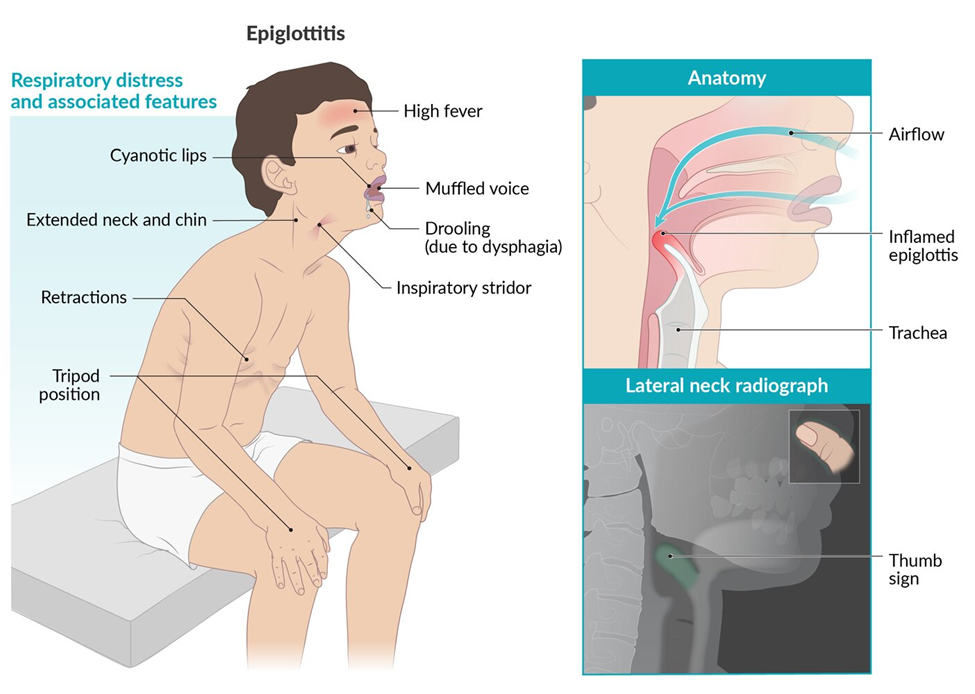
The nurse is assessing a child with acute epiglottitis. Examining the child’s throat by using a tongue depressor might precipitate which symptom or condition?
Explanation
A. Sore throat:
A sore throat is a common symptom of various respiratory tract infections, including acute epiglottitis. However, examining the throat with a tongue depressor is unlikely to directly precipitate a sore throat in this context.
B. Complete obstruction:
Examining the child's throat with a tongue depressor in acute epiglottitis can potentially trigger spasm or swelling of the already inflamed epiglottis, leading to a rapid and complete obstruction of the airway. This is a critical concern and is why healthcare providers approach suspected cases of epiglottitis with great caution.
C. Inspiratory stridor:
Inspiratory stridor (high-pitched sound during inhalation) is a common symptom of upper airway obstruction, including in conditions like acute epiglottitis. It may be present without manipulation, but using a tongue depressor in the throat could exacerbate this symptom.
D. Respiratory tract infection:
Acute epiglottitis is indeed a type of respiratory tract infection. However, examining the throat with a tongue depressor is not likely to directly precipitate a respiratory tract infection.
When providing anticipatory guidance to a group of parents with school-aged children, what would the nurse describe as the most important aspect of social interaction?
Explanation
A. Temperament:
Temperament refers to a child's innate traits and behavioral style. While temperament influences how a child responds to social situations, during the school-aged years, the focus often shifts towards developing social skills through interactions with peers.
B. School:
School is a crucial aspect of a child's life, providing opportunities for social interaction, learning, and development. However, within the context of social interaction, the emphasis on school might encompass friendships, group activities, and the overall social environment that the child experiences within the school setting.
C. Peer relationships:
During the school-aged years, peer relationships become particularly important for social development. Children start to form friendships, learn to navigate social situations, and develop a sense of belonging. Peer interactions contribute significantly to emotional and social growth during this stage.
D. Family:
Family plays a fundamental role in a child's development, including social development. However, during the school-aged years, children often begin to explore relationships outside the family circle, and peer relationships become increasingly influential.
A nurse is preparing a presentation for a group of nurses about human immunodeficiency virus infection. Which of the following would the nurse include as the major means of transmission responsible for almost all new HIV infections in the infant population?
Explanation
A. Exposure to contaminated body fluid:
HIV can be transmitted through exposure to contaminated body fluids such as blood, semen, vaginal fluids, and breast milk. However, in the context of infants, mother-to-child transmission is the primary mode of concern.
B. Mother-to-child transmission:
Mother-to-child transmission, also known as perinatal or vertical transmission, is the major means of HIV transmission in infants. It can occur during pregnancy, childbirth, or breastfeeding when the virus is passed from an HIV-positive mother to her child.
C. Blood transfusions:
While HIV transmission through blood transfusions was a concern in the past, current blood screening and testing procedures have significantly reduced this risk. It is not a major means of transmission in the infant population.
D. Sharing of infected needles:
The sharing of infected needles is a risk factor for HIV transmission among individuals who use injection drugs. However, this mode of transmission is not relevant to infants, as they are not typically exposed to such risk factors.
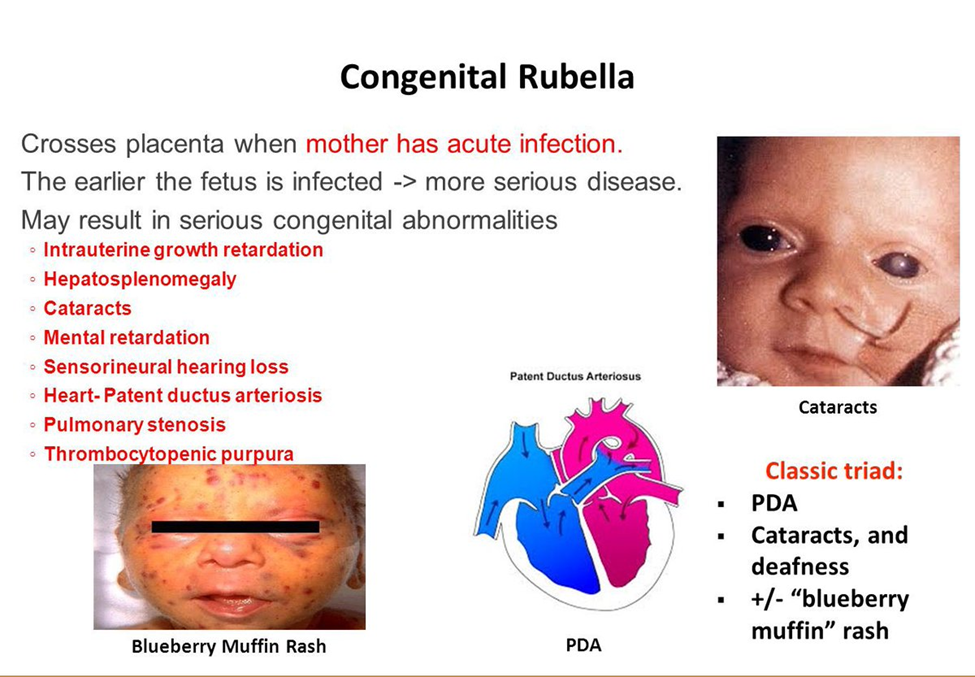
Which common childhood communicable disease may cause severe defects in the fetus when it occurs in its congenital form?
Explanation
A. Rubella:
Rubella is a viral infection that, when contracted by a pregnant woman during the first trimester, can lead to congenital rubella syndrome (CRS) in the developing fetus. CRS can result in severe birth defects, including heart abnormalities, hearing impairments, and vision problems.
B. Varicella-zoster:
Varicella-zoster virus causes chickenpox. While chickenpox can cause complications in certain populations, it is not specifically associated with severe defects in the fetus when the mother is infected during pregnancy.
C. Rubeola:
Rubeola, commonly known as measles, can lead to complications, but it is not as strongly associated with severe defects in the fetus if the mother is infected during pregnancy compared to rubella.
D. Mumps:
Mumps is generally not associated with severe defects in the fetus when the mother is infected during pregnancy. However, mumps infection during pregnancy can pose risks to the mother's health.
An adolescent patient is to receive 50 mL of Cefazolin IV over 40 minutes. With a tubing drop factor of 20 gtt/mL, how many drops per minute (gtt/min) should be given?
Explanation
To calculate the drops per minute for an IV infusion, we need to use the following formula:
gtt/min = (volume x drop factor) / time
In this case, the volume is 50 mL, the drop factor is 20 gtt/mL, and the time is 40 minutes. Plugging these values into the formula, we get:
gtt/min = (50 x 20) / 40
gtt/min = 1000 / 40
gtt/min = 25
Therefore, the adolescent patient should receive 25 drops per minute of Cefazolin IV.
Which statement by the mother of an 18-month-old would lead the nurse to believe that the child should be referred for further evaluation for developmental delay?
Explanation
A. “My child has a vocabulary of approximately 20 words.”
This statement indicates language development, and an 18-month-old with a vocabulary of approximately 20 words is within the expected range. It's a positive indicator of language acquisition.
B. “My child is still thumb sucking.”
Thumb sucking is a common self-soothing behavior in infants and toddlers. While it's a normal behavior, it typically decreases with age. Thumb sucking alone may not necessarily be a cause for concern unless it persists significantly and interferes with other aspects of development.
C. “My child seems to be quite wary of strangers.”
Stranger anxiety is a normal developmental stage, and many children exhibit wariness or fear of unfamiliar people around the age of 18 months. It is considered a typical response and not necessarily indicative of developmental delay.
D. “My child is able to stand but is not yet taking steps independently.”
At 18 months, most children are expected to be walking independently. The inability to take independent steps might be a concern for gross motor skill development. While some variation is normal, a delay in achieving this milestone might prompt further evaluation to rule out any underlying developmental issues.
The nurse is presenting an in-service training to a group of pediatric nurses on the topic of play. The nurse determines the session is successful when the group correctly chooses which example as best displaying toddlers playing?
Explanation
A. Playing in an organized group with each other:
Toddlers typically engage in parallel play rather than organized group play. They may play near each other, but their interactions are often individual rather than coordinated in an organized group.
B. Playing independently and are side by side:
This is an accurate description of parallel play. Toddlers often play independently but are aware of and interested in what their peers are doing. They may play side by side without direct interaction.
C. Playing apart from others without being part of a group:
This option describes solitary play, where a child plays alone and does not actively engage with others. While solitary play is also common, parallel play is more characteristic of toddlers.
D. Playing together in an activity without organization:
This may describe a form of cooperative play, where children engage in an activity together. However, for toddlers, the organized aspect of play is less typical. Parallel play, where they play side by side but independently, is more common.
The nurse is evaluating teaching provided to a school-age child and parents about the use of pancreatic enzymes for cystic fibrosis. Which observation indicates that teaching has been effective?
Explanation
A. The mother opens the capsule and some medication spills on the fingers:
Pancreatic enzymes are usually taken intact, and their contents are meant to be sprinkled on soft food, not opened and spilled. This observation suggests a misunderstanding of the proper administration.
B. The child takes a dose before having an afternoon snack.
In cystic fibrosis, pancreatic enzyme replacement therapy is commonly used to help digest and absorb nutrients. The enzymes are typically taken with meals and snacks to aid in the digestion of food.
C. The child chews an enteric form of the medication:
Pancreatic enzymes are usually enteric-coated to protect them from stomach acid, and they are not meant to be chewed. Chewing can reduce their effectiveness. This observation indicates a need for clarification on administration.
D. The father tells the child that diarrhea is expected with this medication:
While gastrointestinal side effects can occur with pancreatic enzyme use, persistent diarrhea may indicate a dosage issue or other problems. It's important to address this with the healthcare provider. The statement suggests a potential misunderstanding or need for clarification.
The nursing instructor is leading a class discussion on the various aspects of adolescents. The instructors determines the class is successful after the students correctly choose which milestone as the beginning of adolescence?
Explanation
A. The deciduous teeth falling out:
The falling out of deciduous (baby) teeth is a natural part of early childhood development and is not specifically indicative of adolescence. The loss of deciduous teeth usually occurs before the age of 12.
B. The beginning of puberty:
Puberty is the period of physical and sexual development that marks the transition from childhood to adolescence. It involves the development of secondary sexual characteristics, such as breast development in girls and facial hair growth in boys, along with other physical changes.
C. The child becoming self-supported:
Becoming self-supported is a broad concept that can occur at various stages of development and is not a specific marker of the beginning of adolescence. Adolescents may gain increasing independence, but this is a gradual process.
D. The fine motor skills fully developed:
Fine motor skills typically develop during early childhood, and the full development of these skills is not a specific marker for the beginning of adolescence. Fine motor skills involve the coordination of small muscle movements and are important for tasks like writing and drawing.
The caregivers of a 2-year-old who has had a common cold for 4 days calls the nurse in the emergency department at 2 AM on a cold winter night to say that the child has awakened with a barking cough and an elevated temperature. The caregiver reports she has taken the child into the bathroom and ran hot water for 15 minutes and now the child seems blue around her mouth The nurse would most appropriately recommend what action to the caregiver?
Explanation
A. “Bring the child to the emergency room immediately.”
This is the most appropriate recommendation given the symptoms described, including the barking cough, elevated temperature, and blueness around the mouth. These signs may indicate respiratory distress, and immediate medical attention is needed.
B. “Bundle the child up and take her out into the cold for a few minutes. Call back if the exposure to the cold air does not provide relief.”
Taking a child out into the cold is not a recommended intervention for respiratory distress. This action may exacerbate the child's breathing difficulties. The symptoms described require urgent evaluation in a healthcare setting.
C. “Take the child into the steam-filled room for an additional 15 minutes. If there is no relief, bring the child to the emergency room.”
While steam may provide temporary relief for mild respiratory symptoms, the presence of blueness around the mouth suggests a more severe condition. Delaying care by waiting for an additional 15 minutes may not be appropriate in this situation.
D. “Put a cool mist humidifier or vaporizer in the room to see if that relieves the cough. Call back if there’s no relief in an hour.”
Using a cool mist humidifier may be helpful for mild respiratory symptoms, but the severity of the symptoms described, especially blueness around the mouth, indicates a need for immediate medical attention. Waiting for an hour could lead to worsening of the child's condition.
The nurse instructs a mother on actions to prevent sibling rivalry between a toddler and a newborn. Which observation indicates that instruction has been effective?
Explanation
A. Mother sets aside afternoon time for the toddler while the baby naps.
Setting aside dedicated time for the older sibling when the newborn is napping demonstrates a proactive approach to ensuring the older child receives attention and feels valued, reducing the likelihood of resentment or rivalry.
B. Mother sleeps while newborn is sleeping:
While rest is important for the mother, this doesn't directly address the dynamics of sibling rivalry. It's essential to focus on positive interactions and attention for the toddler when the newborn is not requiring immediate care.
C. Mother asks if the toddler likes the new baby:
While communication is important, simply asking if the toddler likes the new baby may not be sufficient to prevent sibling rivalry. Actions and dedicated time are often more impactful.
D. Mother suggests family not bring gifts to the toddler until behavior changes:
Delaying gifts based on behavior may create an association between gifts and behavior change, which might not be the most effective approach. Positive reinforcement and attention are often more beneficial in preventing rivalry.
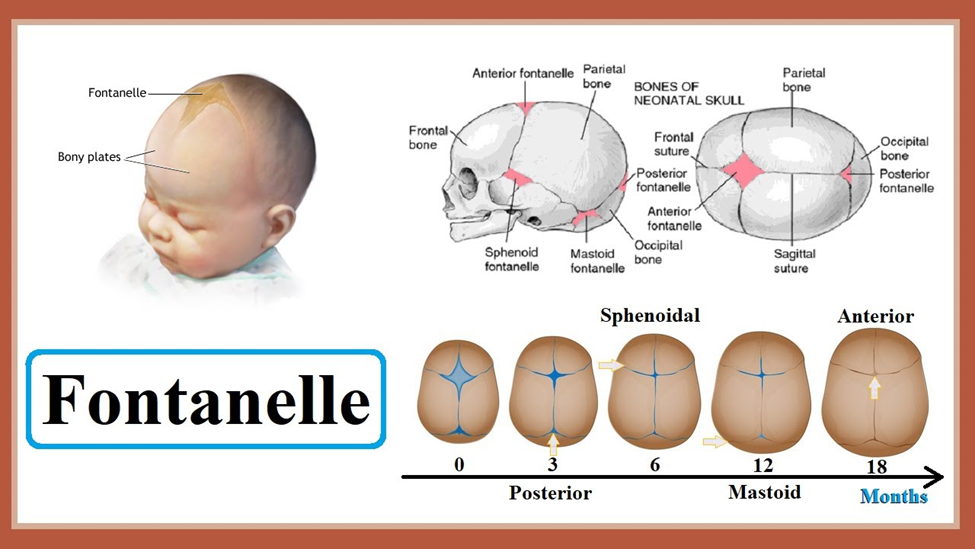
The nurse is performing a physical assessment on a 6-month-old baby. Which finding should the nurse understand as abnormal for this child?
Explanation
A. The child has the beginning signs of tooth eruption:
Teething usually begins around 4-7 months of age, so the beginning signs of tooth eruption (teething) are typical at six months.
B. The child is able to track and follow objects:
By six months, most infants can track and follow objects with their eyes, which is a normal developmental milestone for this age.
C. The child’s anterior fontanel is open:
The anterior fontanelle, the soft spot at the top of the baby's head, remains open until around 18-24 months of age, so its presence at six months is expected and considered normal.
D. The child’s posterior fontanel is open.
By six months of age, the posterior fontanelle, the soft spot located at the back of the baby's head, typically closes or is significantly smaller than it was at birth. The posterior fontanelle usually closes between 2 to 4 months of age in most infants. If it remains noticeably open by six months, it might warrant further evaluation as it could be indicative of a developmental or medical issue.
The nurse is caring for an infant who has impetigo and is hospitalized. Which nursing intervention is the highest priority for this child?
Explanation
A. The nurse applies elbow restraints to the infant:
The use of elbow restraints is not a standard intervention for impetigo. Restraints are typically used for specific medical reasons, such as preventing the infant from interfering with medical equipment or procedures. It is not the highest priority in managing impetigo.
B. The nurse soaks the skin with warm water:
Soaking the skin with warm water can help in keeping the affected areas clean and promoting healing, but it is not the highest priority when considering the prevention of the spread of impetigo.
C. The nurse follows contact precautions:
Following contact precautions is the highest priority when dealing with impetigo. Since impetigo is highly contagious, implementing contact precautions, such as wearing appropriate PPE, is crucial to prevent the spread of the infection within the hospital setting.
D. The nurse applies topical antibiotics to the lesions:
Applying topical antibiotics is an important part of the treatment for impetigo. It helps to eliminate the bacterial infection and promote healing. However, while important, it is not the highest priority compared to preventing the spread of the infection through contact precautions.
The nurse is caring for a school-age child with varicella. What should the nurse observe about the rash that is associated with this infection?
Explanation
A. Dark red, macular lesions, and very pruritic:
Varicella lesions are typically pink or red and start as macules (flat, red spots) that develop into papules (raised bumps) and then vesicles (fluid-filled blisters). Dark red macular lesions are not commonly associated with varicella.
B. Various stages of lesions present at the same time, appear in successive crops, and very pruritic:
The presence of various stages of lesions (papules, vesicles, crusts) simultaneously, occurring in successive crops, and being intensely itchy are typical features of varicella.
C. Yellowish, scaly patches present on the scalp:
Yellowish, scaly patches on the scalp are not typical of varicella. This description is more indicative of conditions like seborrheic dermatitis rather than the rash associated with chickenpox.
D. A pink maculopapular rash starts at the hairline and spreads down the body.
Varicella rash usually begins as pink or red spots that develop into small, itchy, fluid-filled blisters (vesicles). These vesicles can then progress to form crusts and scabs. The rash often starts on the face, scalp, or trunk and then spreads to other parts of the body, gradually covering the entire body.
Sign Up or Login to view all the 38 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

