Ivytech community College Nursing Fundamentals exam 1
Total Questions : 25
Showing 25 questions, Sign in for moreA nurse is repositioning a client who has physical limitations due to recent back surgery. How often would the nurse turn the client in bed?
Explanation
A. Every four hours:
Turning a client every four hours may not be frequent enough to prevent pressure ulcers, especially in individuals with physical limitations or recent surgical procedures.
B. Every hour:
Turning a client every hour might be too frequent for some patients, and it may disrupt their rest and sleep. The optimal frequency depends on the client's condition.
C. Every shift:
Turning a client every shift (which typically spans 8-12 hours) may not provide adequate prevention for pressure ulcers, especially if the client has limited mobility.
D. Every two hours:
Turning a client every two hours is a common practice to prevent pressure ulcers. This interval helps redistribute pressure on vulnerable areas, improving blood circulation and reducing the risk of skin breakdown.
During a physical assessment a nurse inspects a patient’s abdomen. What assessment technique would the nurse perform next?
Explanation
A. Palpation:
Palpation involves using the hands to feel for tenderness, masses, or abnormalities in the abdomen. It is typically performed after auscultation. This helps prevent stimulating bowel activity before listening to bowel sounds.
B. The order does not matter:
In the context of abdominal assessment, the order does matter. Following a specific sequence, such as inspection, auscultation, palpation, and then percussion, is recommended to ensure a comprehensive and accurate assessment.
C. Auscultation:
Auscultation involves listening to bowel sounds using a stethoscope. It is the next step after inspection. Listening to bowel sounds before palpation helps avoid artificially stimulating bowel activity.
D. Percussion:
Percussion involves tapping the abdomen to assess for the presence of fluid or air. While less commonly performed in routine abdominal assessments, it is usually the last technique after inspection, auscultation, and palpation.
A nurse is administering enoxaparin 40mg subcutaneous to a client for prevention of blood clots when the client suddenly moves causing the needle to exit the client’s tissue and stick the nurse’s finger. What is the nurse’s first priority action?
Explanation
A. Report the injury to a nurse manager:
While reporting the incident is important, the immediate action to take is cleaning the affected area to minimize the risk of infection.
B. Wash the affected area with soap and water:
This is the immediate priority to reduce the risk of potential infection or transmission of any contaminants from the needlestick injury.
C. Report the needle stick to the infection control department:
Reporting the incident is essential, but it should follow the immediate step of cleaning the affected area to prevent infection.
D. Scrub the area with hand sanitizer for a full 2 minutes:
Hand sanitizer may not be as effective as soap and water in removing contaminants from a needlestick injury site. Washing with soap and water is more appropriate for cleaning the area.
Nursing in the United States is regulated by the state nurse practice act. What is a common element of each state’s nurse practice act?
Explanation
A. Defining the legal scope of nursing practice:
The nurse practice act in each state defines the scope of practice for nurses, outlining what nurses can and cannot do within the legal boundaries of their profession. It specifies the duties, responsibilities, and limitations of nursing practice within that particular state.
B. Lobbying federal lawmakers to advance professional nursing:
While nursing organizations and associations may engage in lobbying efforts at the federal level, it's not a direct component of the state's nurse practice act.
C. Providing continuing education programs:
While states might require nurses to participate in continuing education for license renewal, the provision of continuing education programs itself is not a direct element of the nurse practice act.
D. Creating institutional policies for health care practices:
Institutional policies are typically developed by healthcare institutions or organizations and are separate from the state's nurse practice act.
The nursing process guides nurses in delivery of care and includes sequential steps. Which step does the registered nurse (RN) perform within the nursing process that is not part of the standard of practice for the licensed practical nurse (LPN)?
Explanation
A. Evaluation:
Both RNs and LPNs engage in the evaluation step of the nursing process. It involves assessing the effectiveness of the care plan and determining whether the desired outcomes have been achieved.
B. Analysis:
The analysis step involves a deeper level of critical thinking and problem-solving. It often includes a more comprehensive examination and interpretation of assessment data to develop the nursing diagnosis, a step that typically falls within the scope of practice for RNs.
C. Implementation:
Both RNs and LPNs are involved in implementing the care plan, which includes carrying out nursing interventions according to the established plan of care.
D. Planning:
Both RNs and LPNs participate in the planning phase, which involves setting goals, establishing priorities, and creating a care plan tailored to the patient's needs.
The nurse is admitting a patient with a suspected tuberculosis infection. Which type of isolation should the nurse institute for this client?
Explanation
A. Droplet isolation:
Droplet isolation is used for diseases spread by respiratory droplets that are larger than those in airborne transmission. Examples include influenza and bacterial meningitis.
B. Enhanced contact isolation:
Enhanced contact precautions are implemented for patients known or suspected to be infected with pathogens that require additional control measures beyond standard precautions. This may include multi-drug resistant organisms.
C. Airborne isolation:
Airborne isolation is specifically used for diseases that are transmitted through small airborne particles that can remain suspended in the air for an extended period. Tuberculosis is one such example. The use of N95 respirators and negative pressure rooms is common for airborne precautions.
D. Neutropenic isolation:
Neutropenic precautions are implemented for patients with compromised immune systems, particularly those with low neutrophil counts. It involves measures to protect the patient from potential infections.
The nurse is performing a respiration assessment on her client. The nurse begins counting the respirations when the second hand on the clock is at 12. When the nurse looks at the chest of the client he is exhaling. The client then continues to inhale and exhale 9 times. When the second hand on the clock is just past 5 the patient begins to inhale. When the second hand reaches the 6 the client has not exhaled. What would the nurse record in the chart as this client’s respiratory rate?
Explanation
A. 20 bpm: This is twice the calculated rate, so it's significantly higher than observed.
B. 10 bpm: This matches closely with the calculated rate of approximately 10.23 breaths per minute.
The scenario describes the nurse counting the client's breaths starting from when the second hand of the clock was at 12 and ending just past 5, and the client completed 9 breaths during this time frame.
Counting Period:
From just past 12 to just past 5 on the clock, the time span is approximately 53 seconds.
Number of Breaths:
The client completed 9 breaths within this time frame.
Now, to calculate the respiratory rate:
Respiratory rate = (Number of breaths / Time in minutes)
Respiratory rate = (9 breaths / 0.88 minutes) (53 seconds converted to minutes)
After calculation, the respiratory rate is approximately 10.23 breaths per minute.
C. 09 bpm: This is a lower value than observed and doesn't align with the counted breaths.
D. 18 bpm: This is close to double the observed rate, which doesn't match with the counted breaths within the time frame.
The nurse is providing oral care for a client who is weak, drowsy, and unable to take anything by mouth (NPO). Which of the following would the nurse implement when performing appropriate oral care for this client?
Explanation
A. Perform oral hygiene at least every 2 hours:
Regular oral care is essential to maintain oral health, prevent infections, and provide comfort. When a client is NPO, and especially if they are weak or drowsy, the nurse should perform oral care at least every 2 hours to keep the oral cavity moist, reduce the risk of infection, and provide comfort.
B. Client must be supine with the head of the bed below 30 degrees:
Keeping the head of the bed elevated to at least 30 degrees is important for preventing aspiration and promoting respiratory function. This position is not specific to oral care but is a general guideline for managing clients at risk for aspiration.
C. Use alcohol-based mouth rinse with oral swab:
Alcohol-based mouth rinses can be drying and may not be suitable for a client who is NPO, as they might contribute to further dryness of the oral mucosa. Non-alcohol-based mouth rinses or moistened oral swabs are often preferred.
D. Assist the client with oral care by brushing their teeth twice daily:
While regular oral care is important, the frequency of twice daily brushing may not be sufficient for a weak, drowsy client, especially if they are NPO. Oral care should be performed more frequently to maintain oral hygiene.
A nurse is providing oral care to a client with dentures. What action would the nurse do first?
Explanation
A. Wash the client’s face:
While washing the client's face might be part of general care, when specifically providing oral care for a client with dentures, the first step should be to don gloves to ensure infection control and safety.
B. Remove dentures:
Removing dentures may be a step in the oral care process, but it should come after donning gloves to maintain proper infection control measures.
C. Apply lubricant:
Applying lubricant might be necessary, especially if the client experiences dryness or discomfort, but it should follow the step of donning gloves.
D. Don gloves:
This is the first action because it is crucial to wear gloves before handling a client's dentures or engaging in any oral care procedures. Gloves protect both the nurse and the client from potential infections and ensure proper hygiene during care.
A nurse is caring for a patient who has a low platelet count and is at risk for bleeding. Which of the following is a critical factor or priority that the nurse should apply when considering how to obtain the patient’s vital signs?
Explanation
A. Do not let the patient know you are counting their respirations:
This is not directly related to obtaining vital signs and is not a critical factor for a patient with a low platelet count.
B. Let the patient rest for 5 minutes before you measure their blood pressure:
Allowing the patient to rest for a few minutes before measuring blood pressure is a good practice but may not be as critical as other considerations in a patient with a low platelet count.
C. Do not measure the patient’s temperature rectally:
Patients with low platelet counts are at an increased risk of bleeding. Rectal temperatures can be invasive and carry a risk of mucosal injury, making them less advisable in patients with bleeding risks.
D. Count the patient’s radial pulse for 30 seconds and multiply it by 2:
Counting the radial pulse is a suitable method for assessing heart rate in a patient at risk for bleeding. However, rectal temperature measurement should be avoided due to the risk of mucosal injury.
The nurse would recognize which of the following patients would be at highest risk for developing an infection?
Explanation
A. 74-year-old female with malnutrition and a foley catheter in place:
Malnutrition can weaken the immune system, making the individual more susceptible to infections. Additionally, the presence of a foley catheter increases the risk of urinary tract infections.
B. 54-year-old female admitted for chest pain observation:
Chest pain observation does not inherently increase the risk of infection.
C. 34-year-old male admitted for seizure observation:
Seizure observation does not inherently increase the risk of infection.
D. 78-year-old male with right-sided hemiplegia following a stroke:
While the hemiplegia following a stroke may pose mobility challenges, the presence of malnutrition and a foley catheter in option A puts the patient at a higher risk for infection.
A nurse is ambulating a client who catches her foot on the bed frame and begins to fall. Which of the following is an accurate step to prevent or minimize damage from this fall?
Explanation
A. Placing the nurse's feet close together side by side to have a good center of gravity:
While maintaining a good center of gravity is important, in a falling situation, it's crucial to prioritize the client's safety over the nurse's stability. This option doesn’t address the prevention of the client’s fall.
B. Rocking the nurse's pelvis out and trying to hold the patient up to prevent falling:
Attempting to hold the patient up during a fall may put both the nurse and the client at risk of injury.
C. Grasping the gait belt and pushing the client’s body backward away from the nurse's body:
Pushing the client backward could cause the client to lose balance and fall in an uncontrolled manner.
D. Using the patient's gait belt to gently slide the client down the nurse's body to the floor:
This is the recommended action as it allows for a controlled descent to the floor, minimizing the impact of the fall and reducing the risk of injury to both the client and the nurse.
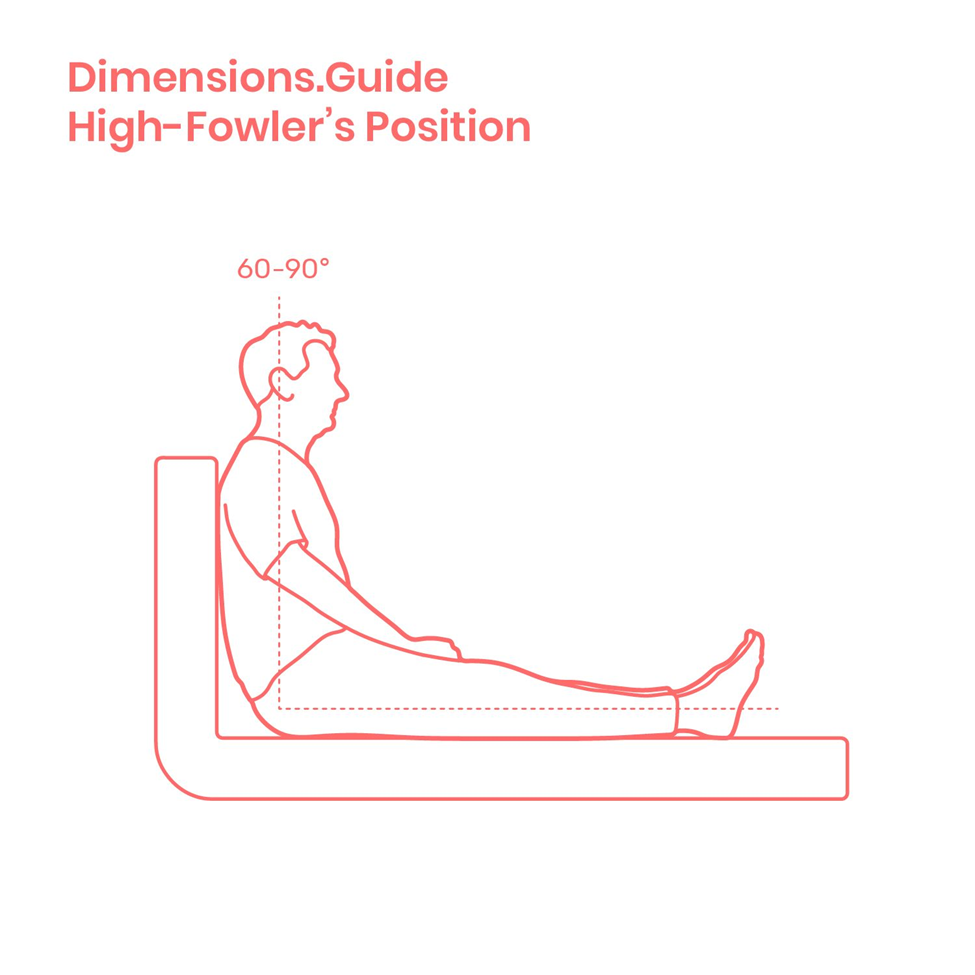
The physician’s admitting orders indicate that the client is to be placed in a High Fowler’s position. Upon positioning this client, how much will the nurse elevate the head of the bed?
Explanation
A. 30 degrees:
This angle does not meet the criteria for a High Fowler's position, which requires a more upright position.
B. 15 to 20 degrees:
This angle is lower than what is generally considered as High Fowler's position. High Fowler's is a more upright position.
C. 90 degrees:
High Fowler's position involves elevating the head of the bed to 90 degrees. This position is often used for better lung expansion and respiratory function.
D. 45-60 degrees:
While this range is higher than a semi-Fowler's position, it is not as upright as the 90-degree elevation in a High Fowler's position.
Various sounds are heard when assessing a blood pressure. What does the second sound heard through the stethoscope represent?
Explanation
A. Systolic pressure:
The first sound heard during blood pressure measurement corresponds to the systolic pressure, the pressure in the arteries when the heart is contracting.
B. Pulse pressure:
Pulse pressure is the numerical difference between the systolic and diastolic pressures but is not specifically represented by a sound in blood pressure measurement.
C. Auscultatory gap:
An auscultatory gap is a temporary disappearance of sounds during blood pressure measurement, typically occurring between the systolic and diastolic pressures. It is not directly associated with the second sound.
D. Diastolic pressure:
The second sound heard corresponds to the closure of the aortic valve, marking the beginning of diastole. This sound represents the diastolic pressure, which is the pressure in the arteries when the heart is at rest.
A nurse is assessing the level of consciousness of a patient who has sustained a head injury in a motor vehicle accident. The nurse notes that the patient appears drowsy but the nurse is able to wake the patient by gently shaking and calling the patient by name. What level of consciousness would the nurse document?
Explanation
A. Comatose:
A comatose state is characterized by an unarousable and unresponsive condition. Individuals in a coma do not respond to external stimuli, including shaking or calling their name.
B. Stuporous:
Stupor is a state of near-unconsciousness or insensibility. A stuporous patient may require more intense stimulation to achieve a response than someone who is lethargic.
C. Lethargic:
Lethargy is a state of drowsiness or fatigue. Lethargic patients may appear drowsy but can be awakened by gentle stimulation, such as shaking and calling their name.
D. Awake and Alert:
An awake and alert state implies full responsiveness, awareness, and orientation to the environment. The patient in the scenario does not fit this description.
The unlicensed assistive personnel reports vital signs for a patient to the nurse: Oral Temperature of 99.2 degrees Fahrenheit. Radial pulse of 88 bpm and regular, Respirations of 18 bpm and regular, blood pressure supine in left arm of 178/112 mm Hg. and oxygen saturation of 95% on room air. Which vital sign should the nurse be most concerned about?
Explanation
A. Pulse:
A pulse rate of 88 bpm is within the normal range. While it's important to monitor the pulse for changes, the reported pulse rate does not raise immediate concerns.
B. Temperature:
An oral temperature of 99.2 degrees Fahrenheit is within the normal range. While it's slightly elevated, it might be influenced by various factors, and isolated temperature readings are not as urgent as other vital signs.
C. Blood Pressure:
A blood pressure reading of 178/112 mm Hg is significantly elevated. High blood pressure is a major concern due to the potential risks it poses to the cardiovascular system, kidneys, and other organs. Immediate attention and further assessment are needed.
D. Respirations:
Respiratory rate of 18 bpm is within the normal range. While it's important to monitor respiratory rate, the reported rate does not raise immediate concerns.
A new patient is visiting a health clinic for the first time for a physical examination. The nurse obtains the patient’s medical history and the patient reports no history of chronic illness or disease and has been very healthy. The patient reports that they have not been seen by a physician for a physical examination in 2 years. The patient states “I am fearful of doctors and I am nervous about being here”. The nurse begins their assessment by collecting vital signs and notes the patient’s blood pressure reading is 130/90 mm Hg in the patient’s right arm while sitting. What would be the priority for the nurse to do next?
Explanation
A. Allow the patient to relax and then recheck the patient’s B/P in 5 minutes:
The initial elevated blood pressure reading could be influenced by the patient's anxiety about visiting the doctor. Allowing the patient to relax and rechecking the blood pressure after a few minutes may provide a more accurate reading.
B. Document the elevated blood pressure and notify the physician immediately:
It is premature to immediately notify the physician based on a single elevated blood pressure reading. Reassessing after the patient has had time to relax is a reasonable approach before taking further action.
C. Begin education related to hypertension (high blood pressure):
While patient education is important, addressing the patient's anxiety and obtaining accurate blood pressure readings should be the initial focus.
D. Schedule the patient for follow-up visits for measurement and monitoring of the patient’s blood pressure:
Scheduling follow-up visits may be necessary based on subsequent assessments, but the immediate concern is to recheck the blood pressure after allowing the patient to relax.
The nurse on the progressive care unit is preparing to perform a sterile wet to dry dressing change on a client with a sacral pressure ulcer. The nurse notes that the sterile saline at the bedside is marked as opened 48 hours ago. What is the nurse’s priority action?
Explanation
A. Discard the bottle of saline and obtain a new bottle:
Sterility is crucial when performing a sterile procedure. If the saline solution has been opened for 48 hours, it may no longer be considered sterile. The nurse's priority is to use a fresh, sterile bottle of saline to ensure aseptic technique during the dressing change.
B. Lip the bottle of saline over the trash before pouring into the field:
Lipping the bottle over the trash is not a recommended practice. Pouring the saline over a sterile field is the appropriate way to maintain the sterility of the solution.
C. Pour the saline at least 6 inches above the sterile field:
While pouring from a height can help generate a flow without contamination, the priority in this situation is to address the sterility of the saline. It's crucial to start with a new, unopened bottle.
D. Be sure the label is facing the palm before pouring:
The orientation of the label is not the primary concern in this scenario. The primary concern is the sterility of the saline solution.
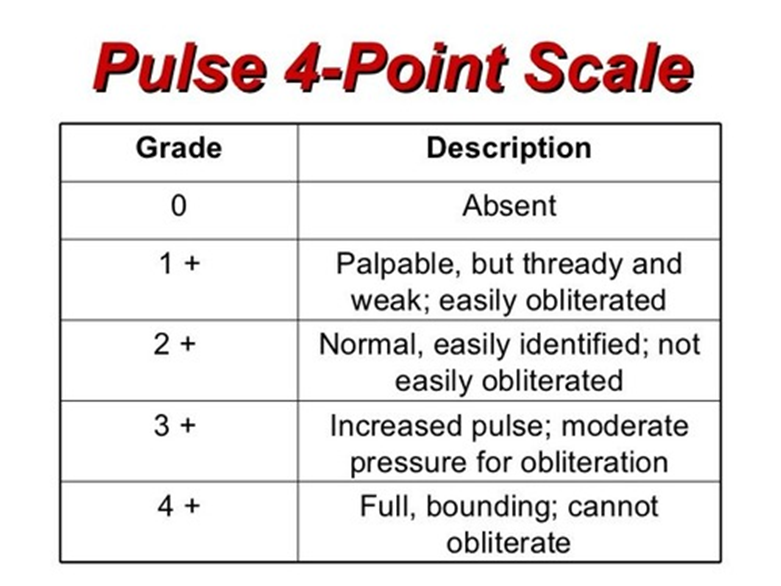
The nurse is taking a radial pulse and assessing the pulse amplitude for a patient. Documentation by the nurse states. “Pulses are +3 in the upper extremities.” What amplitude is the nurse assessing?
Explanation
A. Increased, strong:
A pulse amplitude of +3 indicates an increased or strong pulse. This suggests a forceful and palpable pulse, potentially associated with conditions like fever, anemia, or increased cardiac output.
B. Diminished, weaker than expected:
This would typically be associated with a lower than normal pulse amplitude. It might suggest poor peripheral perfusion or decreased cardiac output.
C. Absent, unable to palpate:
If the pulse is absent or unable to be palpated, it could indicate severe conditions such as vascular occlusion or cardiac arrest.
D. Bounding:
A bounding pulse is one with a forceful and strong amplitude. It suggests a powerful expansion of the arterial wall, and it can be associated with conditions like fever, anemia, or increased cardiac output.
The nurse is applying a wrist restraint on a client who has pulled out his IV multiple times. How should the nurse secure this device?
Explanation
A. Tie it to the bed frame with a quick release knot:
Tying the restraint directly to the bed frame is not recommended as it could limit the client's movement and potentially cause injury. Additionally, a quick release knot may not be ideal in this situation.
B. Strap the restraint with a square knot to the head of the bed:
Securing the restraint to the head of the bed with a square knot could restrict the client's movement and may not allow for quick release in case of emergency or need for rapid removal.
C. Use a quick release knot to tie the restraint to the side rail:
This is the correct approach. Using a quick release knot to tie the restraint to the side rail allows for restraint of movement while still enabling quick release if necessary for the client's safety or in case of emergency.
D. Assist with range of motion at least every 3 hours:
While assisting with range of motion is important for clients in restraints, this option does not address the primary question regarding how to secure the wrist restraint.
A nurse is caring for a comatose patient and applies a hand and wrist roll in each hand of the patient to keep the thumb slightly adducted and correct position to the fingers. What is the primary purpose of this action?
Explanation
A. To prevent contractions in the hand:
The use of hand and wrist rolls helps prevent contractures, which are permanent shortening of muscles or joints. This is particularly important in comatose patients or those with limited mobility to maintain proper hand positioning and prevent deformities.
B. To prevent skin breakdown:
While proper positioning can contribute to preventing skin breakdown, the primary purpose of hand and wrist rolls, in this context, is to address the risk of contractures rather than skin breakdown.
C. To prevent decreased perfusion in the lower extremities:
The action described is specifically related to the hands and wrists, not the lower extremities. It is not designed to prevent decreased perfusion in the lower extremities.
D. To prevent pooling of blood in the hand:
While maintaining proper hand positioning may contribute to optimal circulation, the primary purpose is to prevent contractures rather than addressing blood pooling.
The nurse assists the client back to bed from the bedside commode. What is the most important action the nurse can take to assure client safety prior to leaving the room?
Explanation
A. Make sure the bed is low, locked, and the call light is in reach of the patient:
This action is crucial for preventing falls. A low bed reduces the risk of injury if the client were to accidentally fall. Locking the bed prevents unintended movement, and ensuring the call light is within reach allows the client to call for assistance if needed.
B. Ask the client if they have ordered their dinner:
While nutrition is important, it is not the immediate priority after assisting the client back to bed. Safety measures should be addressed first.
C. Educate the client on the surgical procedure they are scheduled for in the morning:
While pre-operative education is important, it is not the immediate concern after assisting the client back to bed. Safety measures for the current situation take precedence.
D. Check that the client is wearing non-skid socks while in bed:
While wearing non-skid socks is a safety measure, ensuring the bed is low, locked, and the call light is accessible is a more immediate and critical action after assisting the client back to bed.
Which of the following interventions would best assist the nurse in breaking the chain of infection for all clients?
Explanation
A. Use standard precautions in caring for all clients:
Standard precautions involve applying infection prevention practices to all clients, regardless of their known or suspected infectious status. This includes hand hygiene, use of personal protective equipment (PPE), and safe injection practices. Standard precautions are designed to prevent the transmission of microorganisms and break the chain of infection.
B. Place all post-surgical clients in contact isolation:
Contact isolation is typically used for clients with known or suspected infections that can be spread through direct or indirect contact. Placing all post-surgical clients in contact isolation may not be necessary unless there is evidence of a specific infectious condition.
C. Order IV antibiotics for all clients with sacral pressure wounds:
Ordering antibiotics is a specific treatment for bacterial infections but does not address the broader approach of breaking the chain of infection for all clients.
D. Limit visitations to 2 people a day for each client:
While limiting visitations can reduce the risk of introducing infections, it does not address the nurse's direct care practices and adherence to infection prevention measures.
The nurse is caring for a client who has been on bed rest. The primary care provider has just written a new order for the client to sit in the chair three times a day. Which of the following is the best action to transfer the client, for the first time, safely into the chair?
Explanation
A. Infusing an intravenous fluid bolus 15 minutes before transferring the client into the chair:
Administering an IV fluid bolus before transferring the client to a chair is not necessary and not directly related to the safe transfer from bed to chair. It doesn't directly assist with the physical transfer process.
B. Obtaining a quad cane for the client to use as a transfer aid:
While a quad cane can be helpful for some individuals with mobility issues, it might not be necessary for the initial transfer from bed to chair and may not be appropriate for everyone.
C. Positioning a friction-reducing sheet under the client:
While a friction-reducing sheet can assist with moving a client, it may not be necessary for the initial transfer from bed to chair, especially if the client can bear weight and perform the transfer safely.
D. Having the client sit on the side of the bed for several minutes before moving to the chair:
This is the best action. Allowing the client to sit on the side of the bed for a few minutes helps the body adjust to being in a sitting position after an extended period of lying down. It allows for gradual adaptation and reduces the risk of dizziness or orthostatic hypotension when moving from lying down to sitting up.
The nurse understands that sequential compression devices and compression stockings are used for which of the following?
Explanation
A. Protect the muscles of the lower extremities from atrophy:
This statement is not the primary purpose of sequential compression devices (SCDs) and compression stockings. While these devices can help maintain muscle tone by promoting blood circulation, their primary function is to prevent blood pooling and reduce the risk of deep vein thrombosis (DVT).
B. Keep the blood from pooling in lower extremities to avoid clots:
This is the correct purpose of sequential compression devices and compression stockings. They are designed to promote venous return and prevent blood from pooling in the lower extremities, thereby reducing the risk of blood clots, especially in individuals at risk for deep vein thrombosis (DVT).
C. Keep the patient from getting sores on the skin:
Preventing sores on the skin is not the primary purpose of these devices. While improved circulation may contribute to skin health, preventing skin sores is not the primary therapeutic goal of SCDs and compression stockings.
D. Keep the patient’s joints in working order:
Maintaining joint function is not the primary purpose of sequential compression devices and compression stockings. These devices primarily focus on promoting venous circulation and preventing complications related to blood pooling and clot formation.

Sign Up or Login to view all the 25 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

