IvyTech Community College Obstetrics and Pediatrics
Total Questions : 37
Showing 25 questions, Sign in for moreA nurse is planning home care for a 9-year-old child following an acute exacerbation of asthma. Which of the following of Erikson’s developmental stages should the nurse consider in the planning?
Explanation
A. Industry vs. inferiority is relevant to the age range of 6 to 12 years, focusing on the development of competence and mastery in skills. However, it may not be as directly related to the immediate care following an asthma exacerbation.
B. Initiative vs. guilt is the stage where a child starts to take more initiative and responsibility for their own actions. Planning home care involves encouraging the child to take initiative in
managing their asthma, promoting a sense of control over their health.
C. Identity vs. role confusion is more applicable to adolescence and focuses on the formation of a stable self-identity.
D. Autonomy vs. shame and doubt is relevant to the toddler age range, emphasizing the development of independence. While independence is important, the immediate concern in the given scenario aligns more with the initiative and responsibility associated with the school-age child.
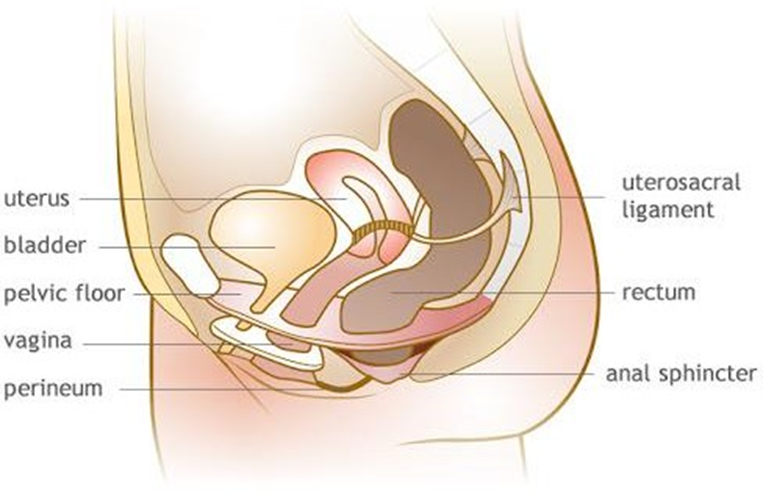
The nurse palpates a postpartum client's fundus two hours after birth and finds it located to the right of midline and somewhat soft. What does the nurse understand about this information?
Explanation
A. The uterine placement is not normal if it's to the right of midline. The fundus should be at the midline immediately after birth.
B. The urinary bladder is distended. A full bladder can displace the uterus and cause it to be off- center.
C. The uterus being filled with blood is not the primary reason for the displacement described.
It's more likely due to a distended bladder.
D. Infection inside the uterus is not the primary reason for the displacement described. A distended bladder is a more common cause.
The nurse is caring for a client in labor. Which process will the nurse use to determine the duration of contractions?
Explanation
A. The interval from the end of one contraction to the beginning of the next one is the frequency, not the duration.
B. Counting the interval from the beginning to the end of one contraction provides the duration of that contraction.
C. Counting the number of contractions in 10 minutes gives the frequency, not the duration.
D. Counting the interval between the acmes (peaks) of two consecutive contractions is not a standard method for determining the duration of contractions. The duration is usually measured from the beginning to the end of a single contraction.
The nurse is completing a fundal assessment for her postpartum clients today. What will the nurse determine when assessing the fundus?
Explanation
A. While shape and height are important aspects, tone is also a key component in assessing the fundus after childbirth.
B. Position is part of the assessment, but the shape and tone are equally crucial components.
C. This choice correctly includes all the essential aspects of a fundal assessment: tone, shape, and position.
D. While shape and height are important, tone and position are equally vital components in assessing the fundus.
The nurse is caring for a client in labor and discovers late decelerations of the fetal heart rate.
What does the nurse know as the reason for this type of deceleration?
Explanation
A. Late decelerations are associated with uteroplacental insufficiency, indicating that the baby is not getting enough oxygen during contractions.
B. Maternal hypotension can lead to decreased perfusion but is more likely associated with variable decelerations.
C. Cord compression is often associated with variable decelerations, not late decelerations.
D. Head compression typically does not cause late decelerations; it may be associated with early decelerations.
The nurse is caring for a client during a vaginal exam by the provider. The provider informs the client that he will use the most common mechanical method to ripen her cervix prior to induction of labor. What is the method being used by the provider?
Explanation
A. Artificial rupture of membranes involves breaking the amniotic sac to induce or augment labor but is not a method for cervical ripening.
B. Laminaria is a common mechanical method used to ripen the cervix before labor induction.
Laminaria tents are placed in the cervix to gradually dilate and soften it.
C. A catheter filled with sterile saline may be used for cervical ripening, but it is not the most common mechanical method.
D. Membrane stripping involves separating the amniotic membrane from the cervix, not a mechanical method for cervical ripening.
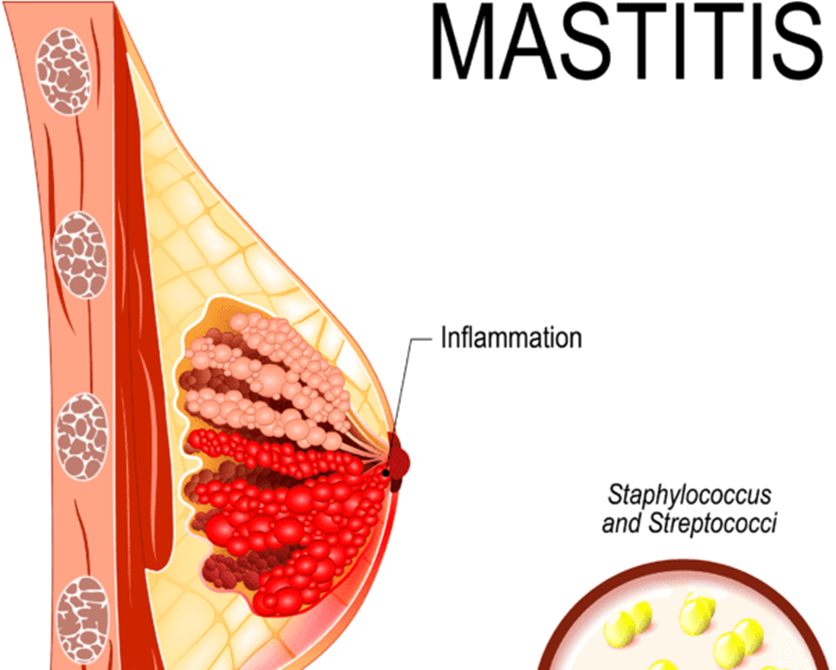
The nurse takes a phone call from a client at two weeks postpartum. The client states, "My left breast hurts." What other question will the nurse ask her to determine if it is mastitis?
Explanation
A. An inverted nipple is not indicative of mastitis.
B. Presence of breast milk is expected postpartum and does not specifically indicate mastitis.
C. A bruised area is not a common sign of mastitis.
D. Mastitis often presents with localized pain, redness, swelling, and a hardening of the affected area of the breast. Asking about the presence of a hardening will help assess for mastitis.
The nurse assesses the postpartum client's fundal height and tone in the first 24 hours. Which action will the nurse take to correctly assess the uterine fundus?
Explanation
A. Placing fingers across the uterus is not a standard technique for assessing the uterine fundus postpartum. Palpation is typically performed on the abdomen.
B. Placing a gloved hand just above the symphysis pubis is more related to assessing descent and engagement of the fetal head during labor, not uterine fundal height.
C. Palpating the abdomen while feeling the uterine fundus allows the nurse to assess the fundal height, tone, and position.
D. Massaging the fundus vigorously to expel blood clots is not a recommended practice; gentle massage is performed to assess tone and firmness.
The nurse is caring for a client during a vaginal exam by the provider. The provider informs the client that he will use the most common mechanical method to ripen her cervix prior to induction of labor. What is the method being used by the provider?
Explanation
A. Artificial rupture of membranes involves breaking the amniotic sac to induce or augment labor but is not a method for cervical ripening.
B. Laminaria is a common mechanical method used to ripen the cervix before labor induction.
Laminaria tents are placed in the cervix to gradually dilate and soften it.
C. A catheter filled with sterile saline may be used for cervical ripening, but it is not the most common mechanical method.
D. Membrane stripping involves separating the amniotic membrane from the cervix, not a mechanical method for cervical ripening.
The nurse is caring for a client at 42 weeks' gestation arriving for an induction of labor. The provider is planning to use dinoprostone (Cervidil) vaginal insert for cervical ripening. What is the nurse's priority prior to insertion?
Explanation
A. Initiating oxytocin infusion is not the priority before the insertion of dinoprostone. Fetal monitoring is a more immediate concern.
B. Ensuring the client eats a light meal and drinks fluids is important for general well-being but is not the priority before dinoprostone insertion.
C. Placing the catheter and sterile saline at the bedside may be done later but is not the priority before insertion.
D. Continuous monitoring of the fetal heart rate and uterine activity is essential to assess the response to cervical ripening agents, as they can cause uterine hyperstimulation and fetal distress.
A postpartum client has continuous seepage of bright red blood from the vagina. The nurse completes an assessment and finds a firm uterus, 1 cm below the umbilicus, and midline. What does the nurse suspect is the reason for the bleeding?
Explanation
A. Uterine atony is characterized by a boggy and enlarged uterus, not a firm one.
B. A cervical laceration would typically present with bleeding and possibly a deviation of the uterus from the midline, but the firm uterus suggests a different cause.
C. Continuous seepage of bright red blood, along with a firm uterus, 1 cm below the umbilicus, and midline, is indicative of retained placental fragments.
D. A urinary tract infection would not typically cause continuous bright red blood seepage from the vagina.
The nurse is discussing birth options with a pregnant client. The client previously had a cesarean birth with a classical incision at 26 weeks' gestation but desires a vaginal birth with this pregnancy. What is the best response by the nurse?
Explanation
A. A classical incision increases the risk of uterine rupture during labor, and a vaginal birth is not typically recommended due to this risk.
B. The type of incision, not the term of the subsequent birth, is the primary consideration for deciding on a mode of delivery.
C. A classical incision is associated with an increased risk of complications, not a decreased risk.
D. The recommendation for a vaginal birth after cesarean (VBAC) depends on factors such as the type of uterine incision and other clinical considerations, not just the time interval.
The nurse is caring for a client in labor. Assessment reveals that the fetus is in a vertex presentation and at -4 station. What does the nurse determine as the position of the fetal head?
Explanation
A. Horizontal does not describe the position of the fetal head in relation to the pelvic station.
B. Engagement typically occurs when the presenting part of the fetus reaches 0 station or is at the level of the ischial spines.
C. At -4 station, the fetal head is considered to be floating, indicating that it has not yet entered the pelvic inlet.
D. Crowning occurs when the fetal head is visible at the vaginal opening during the second stage of labor.
The nurse is caring for a laboring client. The nurse observes that there are variable decelerations. What is the nurse's priority action?
Explanation
A. Changing the client's position, especially if there's a cord compression causing variable decelerations, is a priority intervention to alleviate the decelerations.
B. Informing the primary care provider is important, but immediate action to address the decelerations should be taken first.
C. Vaginal examination is not the immediate priority when variable decelerations are observed; interventions to improve fetal oxygenation are more critical.
D. Continuous monitoring is essential, but addressing the cause of the variable decelerations by changing the client's position is the immediate action.
The nurse is caring for a client with contractions every 2-3 minutes, moderate to palpation, with a duration of 45-60 seconds. The client is having a difficult time breathing through contractions and is requesting something for pain. The client is 5 cm dilated, 80% effaced, and at a -1 station.
Which pain relief measure would be most effective for this client?
Explanation
A. An epidural provides comprehensive pain relief by blocking sensation from the waist down, making it an effective option for clients experiencing intense pain during labor.
B. Effleurage (massage or light stroking) may provide some comfort but may not be sufficient for the described level of pain.
C. Opioids can provide pain relief but may not be as effective in managing the intense pain of contractions in active labor.
D. Sedatives may not be the best choice during active labor as they can have a sedating effect on both the mother and the baby, potentially affecting the progress of labor.
The nurse is assisting a pregnant patient into bed after the patient reports a gush of fluid from the vagina. Which action will the nurse take first?
Explanation
A. Placing the client on her left side is important for optimizing fetal oxygenation but is not the first action when there is a report of a gush of fluid.
B. Notifying the registered nurse (RN) immediately is the first action to ensure prompt assessment and appropriate interventions for possible ruptured membranes.
C. Documenting the time and color of the fluid is important, but immediate notification of the RN takes precedence.
D. Checking fetal heart tones is important but should be done in conjunction with notifying the RN to assess the overall situation and determine the appropriate course of action.
The nurse is caring for a client in labor receiving oxytocin. The client asks the nurse, "What is this medication for?" What is the best response by the nurse?
Explanation
A. Oxytocin is administered to enhance contractions, not to slow them down.
B. While increased blood flow through the placenta is important for fetal well-being, oxytocin is primarily used to stimulate uterine contractions.
C. Increased urinary output is not the primary effect of oxytocin; its main action is to stimulate uterine contractions.
D. Oxytocin is commonly used to induce or augment labor by stimulating contractions of the uterus.
The nurse is caring for a client in labor. Assessment findings: The fetal heart rate (FHR) baseline is 120 bpm The FHR begins slowing as the contraction starts, and is back to baseline at the end of the contraction There is moderate variability of the FHR Which periodic change will the nurse document in the electronic health record?
Explanation
A. Late decelerations typically start after the contraction has reached its peak and return to baseline after the contraction ends, not during the contraction.
B. Early decelerations coincide with the contraction and return to baseline by the end of the contraction. They are typically considered benign and related to head compression.
C. Accelerations are brief increases in the FHR above the baseline and are usually associated with fetal movement.
D. Variable decelerations are abrupt decreases in the FHR, often unrelated to contractions, and have an erratic pattern.
The nurse is caring for a laboring client with early decelerations and a fetal heart rate baseline of 130 with moderate variability. What will the nurse do for this client?
Explanation
A. Early decelerations are generally considered benign and not an indication for a vaginal exam unless other concerning factors are present.
B. Promptly informing the primary care provider may not be necessary for early decelerations, which are often a normal response to head compression.
C. Continuous monitoring and observation of the client and fetal heart rate are appropriate for early decelerations, especially when the baseline is reassuring and there is moderate variability.
D. Repositioning the client to the left side is a general measure for optimizing fetal oxygenation, but it may not be the priority in the case of early decelerations, which are usually benign and
related to head compression.
The nurse is assessing four clients on the postpartum unit. Each client's uterine assessment is below. 1. The client is three days postpartum and her fundus is 3 cm below the umbilicus 2. The client is two days postpartum and her fundus is 2 cm above the umbilicus 3. The client is one day postpartum and her fundus is 1 cm below the umbilicus 4. The client delivered 8 hours ago and her fundus is at the umbilicus
Which client is experiencing uterine subinvolution?
Explanation
A. Client 4, who delivered 8 hours ago, having a fundus at the umbilicus is within the expected range for a client at this stage postpartum.
B. Client 2, two days postpartum with a fundus 2 cm above the umbilicus, is suggestive of uterine subinvolution, as the fundus should be descending, not rising, after delivery.
C. Client 1, three days postpartum with a fundus 3 cm below the umbilicus, is within the expected range for the postpartum period.
D. Client 3, one day postpartum with a fundus 1 cm below the umbilicus, is within the expected range for the postpartum period.
The nurse is admitting a client in the first stage of labor with active genital herpes. Which type of birth will the nurse anticipate for this client?
Explanation
A. Low forceps and mid-forceps deliveries are not typically chosen for clients with active genital herpes due to the risk of exposing the baby to the virus during passage through the birth canal.
B. While vaginal birth is the preferred mode of delivery in many cases, active genital herpes may increase the risk of neonatal transmission, and a cesarean section may be recommended to reduce this risk.
C. Cesarean section is often recommended for clients with active genital herpes to minimize the risk of neonatal transmission, especially if lesions are present at the time of delivery.
D. Mid-forceps delivery is not typically chosen for clients with active genital herpes due to the risk of exposing the baby to the virus during passage through the birth canal.
The nurse is caring for a client on the postpartum unit who had a vaginal delivery with epidural anesthesia 2 hours ago. 1. The client presses the call light and tells the nurse she needs to use the bathroom 2. The nurse arrives in the client's room 5 minutes later 3.
The client is getting out of bed alone What is the best response by the nurse?
Explanation
A. Catheterization may not be necessary at this time and can be uncomfortable for the client.
B. Using a bedpan may not be the most comfortable option for the client, who likely wants to ambulate.
C. Assisting the client to the bathroom is the best response to ensure her safety and prevent falls.
D. Dangling the legs over the side of the bed is not necessary in this situation and may not address the client's need to use the bathroom.
The nurse is caring for a multiparous client who has been in labor for 12 hours. The client had a spontaneous vaginal delivery 2 years ago. This was an unplanned pregnancy with someone she only knew briefly. Since finding out she was pregnant, she has been alone. Her pain is now 8/10 and she is becoming fearful that something is wrong since she has been in labor so long.
Contractions assessment:
- Contractions every 3-4 minutes
- Palpating moderate in intensity
- Lasting 45-60 seconds Cervical exam: .3 cm
- 90% effaced . -2 station
- Fetus is in a cephalic presentation.
Which component of labor is keeping the client from advancing in labor?
Explanation
A. Powers refer to uterine contractions and maternal pushing efforts, which seem appropriate based on the given information.
B. Passage refers to the birth canal, and there is no indication that the birth canal is obstructing the progress.
C. Passenger refers to the fetus, and the cephalic presentation is favorable for a vaginal delivery.
D. The client's psychological state, including fear and anxiety, can impact labor progress. The client's emotional and psychological well-being can influence the progression of labor.
The nurse is caring for a client in labor. Which assessment finding will the nurse report to the charge nurse immediately?
Explanation
A. A FHR baseline of 125 is within the normal range for a fetal heart rate.
B. A temperature of 99.9°F is a mild elevation and may not be an immediate concern.
C. Blood pressure of 142/90 may be elevated but may not require immediate action unless associated with other concerning symptoms.
D. Contractions lasting 45-60 seconds are prolonged and may lead to decreased fetal oxygenation. This finding should be reported immediately to the charge nurse.
The nurse has received shift report for five clients admitted in labor. Which clients will the nurse anticipate delivering by a cesarean section? Select all that apply.
Explanation
A. A previous low transverse uterine incision is a factor that may allow for a trial of labor after cesarean (TOLAC) or a vaginal birth after cesarean (VBAC), rather than an automatic cesarean section.
B. Placenta previa, where the placenta partially or completely covers the cervix, often requires a cesarean section to avoid complications such as bleeding during labor.
C. A previous classical uterine incision, especially if it extends into the upper part of the uterus, is a contraindication for a trial of labor or vaginal birth, usually requiring a repeat cesarean
section.
D. Prolapsed umbilical cord, where the cord precedes the presenting part, can lead to cord compression during contractions, necessitating a prompt cesarean section.
E. Breast cancer is not a direct indication for a cesarean section; it does not impact the mode of delivery in the absence of other obstetric indications.
Sign Up or Login to view all the 37 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

