Med Surg
Total Questions : 87
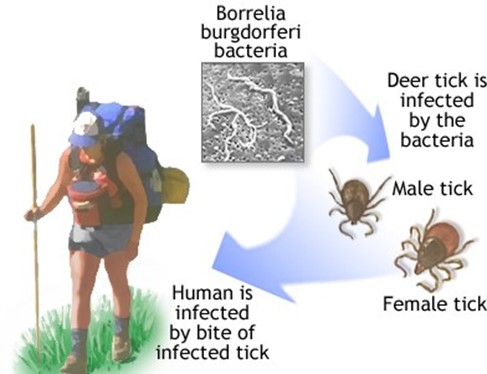
Showing 25 questions, Sign in for moreA client calls the clinic and tells the nurse that he was bitten by a tick and is afraid he has Lyme disease. How long does the nurse understand that the tick must be attached to Lyme disease?
Explanation
36 to 48 hours. Lyme disease is caused by the bacterium Borrelia burgdorferi, which is transmitted to humans through the bite of infected black-legged ticks. The tick must be attached to the skin for at least 36 to 48 hours for the bacterium to be transmitted. The nurse should advise the client to seek medical attention promptly.
Choice B is incorrect because the tick must be attached for a longer duration of time for the bacterium to be transmitted.
Choice C is incorrect because the tick must be attached for a longer duration of time for the bacterium to be transmitted.
Choice D is incorrect because the tick must be attached for a longer duration of time for the bacterium to be transmitted.
Which of the following interventions would be appropriate for a client who has undergone surgery for a disorder and has started shivering?
Explanation
Provide the client with warm fluids. Shivering is the body's natural response to try to warm itself up. Providing warm fluids to the client can help to increase the client's core temperature and decrease shivering.
Choice A is incorrect because a hypothermia blanket is used to reduce the client's core temperature, which is not appropriate for a client who is shivering.
Choice C is incorrect because a light blanket may not provide enough warmth for the client who is shivering.
Choice D is incorrect because the room temperature should be kept warm to prevent the client from getting colder and shivering more.
The nurse is talking with a group of clients that are older than age 50 years about the recognition of colon cancer to access early intervention. What should the nurse inform the clients to report immediately to their primary care provider?
Explanation
Change in bowel habits. Change in bowel habits, such as diarrhea, constipation, or a change in stool consistency, is a common early symptom of colon cancer. The nurse should advise clients over age 50 to report any changes in bowel habits to their primary care provider for early intervention.
Choice B is incorrect because abdominal cramping is a common symptom of irritable bowel syndrome and not necessarily an early symptom of colon cancer.
Choice C is incorrect because daily bowel movements are considered normal for some individuals and are not necessarily indicative of colon cancer.
Choice D is incorrect because excess gas is not an early symptom of colon cancer.
The nurse is caring for a client with a deteriorating neurological condition. The nurse is performing an assessment at the beginning of the shift and notes a falling blood pressure and heart rate. The client is lying flat with arms and legs that are extended, stiff, and rigid, and the feet are plantar flexed. What would be the correct documentation of this posturing?
Explanation
Decorticate posturing is characterized by flexion of the arms, wrists, and fingers, extension, internal rotation, and adduction of the legs, with plantar flexion of the feet. This is caused by damage to the cerebral cortex and is indicative of a neurological problem.
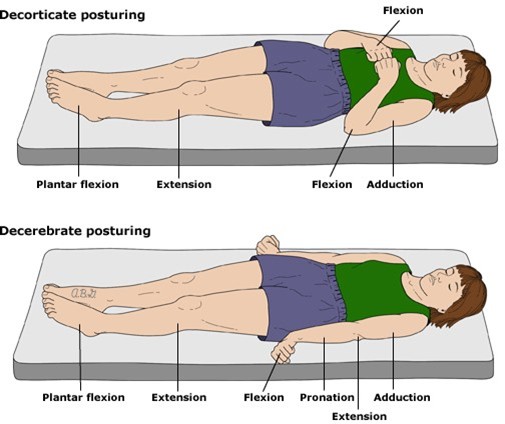
Choice A is incorrect because stuporous is a state of reduced consciousness, and does not describe the posturing observed in the client.
Choice B is incorrect because decerebrate posturing is characterized by extension of the arms, wrists, and fingers, and extension and internal rotation of the legs, with plantar flexion of the feet.
Choice D is incorrect because flaccidity is a state of complete lack of muscle tone, and does not describe the posturing observed in the client.
A client is taking large amounts of salicylates for the treatment of bursitis of the left shoulder. The client should be aware to report which symptoms of salicylate toxicity (salicylism)?
Explanation
Ringing in the ears. Salicylate toxicity or salicylism is a condition that occurs when a client is taking large amounts of salicylates, which can result in symptoms such as tinnitus or ringing in the ears, nausea, vomiting, and diarrhea. Clients should report these symptoms to their healthcare provider immediately to prevent further complications.

Choice A, diarrhea, is not a symptom of salicylate toxicity, but rather a potential side effect of the medication in normal doses.
Choice C, dry eyes, and choice D, dry hacking cough, are not symptoms of salicylate toxicity.
On initial nursing rounds, the diabetic client reports "not feeling well." Later, the nurse finds the client to be diaphoretic and in a stuporous state. What is the immediate action taken by the nurse?
Explanation
choice A, Obtain a glucometer reading. The immediate action taken by the nurse is to obtain a glucometer reading to determine the client's blood glucose level. The client's symptoms are suggestive of hypoglycemia, a condition that can lead to coma and seizures if left untreated. Administering fruit juice or starting an IV of dextrose without first checking the client's blood glucose level can worsen the condition if the client's blood glucose is high. The physician should be notified if the client's blood glucose level is critically low or high and if the client's condition does not improve after treatment.
B. Administering fruit juice can worsen the condition if the client's blood glucose is high.
C. Starting an IV of dextrose can worsen the condition if the client's blood glucose is high.
D. Calling the physician is not the immediate action, as the client needs urgent treatment.
Following a serious thermal burn, which complication will the nurse take action to prevent first?
Explanation
Hypovolemia. Following a serious thermal burn, the nurse takes action to prevent hypovolemia, which can result from fluid loss due to the burn. Hypovolemia can lead to hypoperfusion of vital organs, including the kidneys, and can cause acute renal failure. Preventing hypovolemia is critical to preventing other complications such as tissue hypoxia, cardiac failure, and infection.
A. Tissue hypoxia and cardiac failure are consequences of hypovolemia due to decreased blood flow to organs.
D. Infection is not the immediate complication to prevent but is a potential complication following burn injury.
The nurse is caring for a postoperative client who had surgery to decrease intracranial pressure after suffering a head injury. Which assessment finding is promptly reported to the physician?
Explanation
The client's vital signs are temperature, 101.9 F; heart rate, 88 beats/minute; respiratory rate, 18 breaths/minute, and blood pressure, 138/80 mm Hg. An elevated temperature is a significant finding that may indicate the presence of an infection, which can cause further neurological damage in a client with an intracranial injury. The physician should be notified promptly, as the client may require antibiotic therapy to prevent the spread of infection.
B. Periorbital edema and ecchymosis are normal findings following head injury and should be monitored but do not require immediate intervention.
C. Resting in semi-Fowler's position is an appropriate position to maintain after intracranial pressure-reducing surgery.
D. Improved level of consciousness is a positive finding and indicates that the client is responding well to treatment.
The nursing student is taking an anatomy and physiology class. What anatomical structure equalizes air pressure in the middle ear?
Explanation
Eustachian tube. The Eustachian tube is a narrow tube that connects the middle ear to the back of the nose and equalizes air pressure in the middle ear.
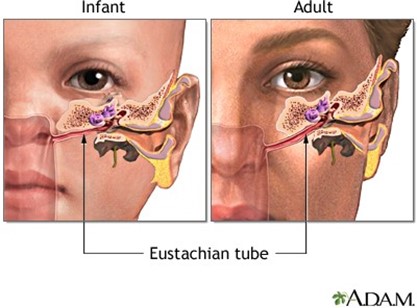
B. The malleus is a bone in the middle ear that transmits sound vibrations.
C. The pinna is the visible part of the ear that collects and directs sound waves.
D. The meatus is a passage or opening leading to the ear or nose.
The nurse is planning care for a client admitted to the neurologic rehabilitation unit following a cerebrovascular accident. Which nursing intervention would be of the highest priority?
Explanation
Assess the client for the ability to ambulate independently. The highest priority nursing intervention for a client admitted to a neurologic rehabilitation unit following a cerebrovascular accident is to assess the client's ability to ambulate independently. This assessment will help the nurse determine the level of assistance required and develop an appropriate care plan.
Option A. Providing instruction on blood-thinning medication is not the highest priority as it can be done later when the client's ambulation status is stable.
Option C. Including the client in the planning of care and setting of goals is important but not the highest priority in this situation as it can be done after assessing the client's ambulation status.
Option D. Praise the client when using adaptive equipment, is not the highest priority as the client's ambulation status is more important at this point.
A client comes to the emergency department complaining of localized pain and swelling of his lower leg. Ecchymotic areas are noted. History reveals that the client got bit in the leg with a baseball bat. Which of the following would the nurse suspect as most likely?
Explanation
Contusion. The nurse would suspect a contusion as the client was hit by a baseball bat and has localized pain and swelling with ecchymosis (bruising).
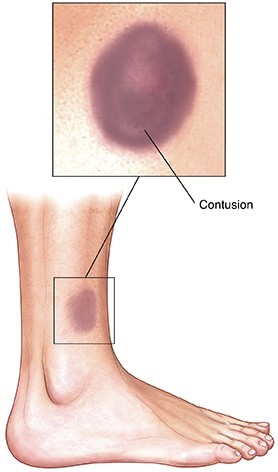
Option A, Strain, is unlikely as a strain is a stretching or tearing of a muscle or tendon, and it is not usually caused by blunt force trauma.
Option B, Sprain, is unlikely as a sprain is a stretching or tearing of a ligament, and it is not usually caused by blunt force trauma.
Option D, Fracture, is unlikely as a fracture is a break in the bone and usually involves more severe pain and may be accompanied by deformity.
A client, who is recovering from bariatric surgery, is returning from the post-anesthesia care unit. Which nursing assessment is of greatest concern in the immediate postoperative period for this client?
Explanation
Impaired Gas Exchange. Impaired gas exchange is the greatest concern in the immediate postoperative period for a client recovering from bariatric surgery, as the client may have difficulty breathing due to anesthesia, pain medication, or obesity-related respiratory problems.
Option A, Impaired Mobility, is a concern but not the greatest concern in the immediate postoperative period.
Option C, Self-Care Deficit, may be an issue but is not the greatest concern in the immediate postoperative period.
Option D, Diarrhea, may occur after bariatric surgery but is not the greatest concern in the immediate postoperative period.
The nurse is instructing the client on frequent sensations experienced when a contrast agent is injected into the body during diagnostic studies. Which sensation is most common?
Explanation
A warm sensation. The most common sensation experienced when a contrast agent is injected into the body during diagnostic studies is a warm sensation, as the contrast agent causes a temporary increase in blood flow to the injected area.
Option B, Light-headedness, is not the most common sensation experienced during diagnostic studies with contrast agents.
Option C, Heart palpitations, are not common sensations experienced during diagnostic studies with contrast agents.
Option D, Chills, are not common sensations experienced during diagnostic studies with contrast agents.
Which zone consists of the area where the injury is most severe and deepest?
Explanation
Necrosis. Necrosis is the death of cells or tissue due to disease, injury, or lack of blood supply. In the process of tissue injury, necrosis occurs in the deepest and most severe area of injury.

Choice A, Hyperemia is an increase in blood flow to an area, causing redness and warmth.
Choice B, Coagulation is the process of blood clotting.
Choice C, Stasis is a reduction in blood flow to an area, causing blood to pool and resulting in tissue hypoxia.
A client has a decreased secretion of erythropoietin from the kidneys due to end-stage kidney disease. What outcome will the decrease in erythropoietin have?
Explanation
Anemia from the decrease in the maturation of red blood cells. Erythropoietin, a hormone secreted by the kidneys, stimulates the production of red blood cells in the bone marrow. A decrease in erythropoietin secretion from the kidneys will result in a decrease in the maturation of red blood cells, leading to anemia.
Choice A, an increase in blood sugar levels due to alteration in insulin levels, and Choice C, Decrease in blood sugar levels due to alteration in insulin levels are not associated with decreased secretion of erythropoietin.
Choice D, Development of male sex characteristics is not related to the function of erythropoietin.
Which of the following is a true statement regarding psoriasis?
Explanation
It is characterized by patches of redness covered with silvery scales. Psoriasis is a chronic autoimmune disorder that causes patches of red, inflamed skin covered with silvery scales.

Choice A, It is a chronic, infectious inflammatory disease is incorrect as psoriasis is not caused by an infection.
Choice C, A cure is possible with prompt treatment is incorrect as there is no cure for psoriasis, but symptoms can be managed with treatment.
Choice D, The onset typically occurs in young children is incorrect as psoriasis can occur at any age.
The client is undergoing a tuning fork test to assess for hearing conduction. The nurse performs a Rinne test. How will this test be performed?
Explanation
In the Rinne test, the nurse first places a tuning fork on the mastoid process behind the ear, and when the client states that the sound is no longer heard, the tuning fork is placed beside the ear. This test is done to compare bone conduction with air conduction. When sound is no longer heard via bone conduction, the sound will still be heard via air conduction.
Choice A is incorrect because it describes the Weber test, not the Rinne test.
Choice C is incorrect because it is not a standard hearing test.
Choice D is incorrect because it describes the Whisper test, which is also used to test for hearing loss.
The nurse is caring for a young woman who is struggling with weight loss issues without apparent physical cause. Which is the most likely nursing assessment for this nutritional disorder in which normal body weight is not maintained?
Explanation
Anorexia nervosa is a nutritional disorder characterized by a distorted body image and fear of weight gain, leading to an abnormally low body weight. Clients with anorexia nervosa may also engage in binge eating and purging behaviors.
Choice A is incorrect because Kwashiorkor is a type of protein-energy malnutrition caused by a severe protein deficiency.
Choice C is incorrect because Crohn's disease is a chronic inflammatory bowel disease.
Choice D is incorrect because Bulimia nervosa is a nutritional disorder characterized by binge eating and purging behaviors.
The nurse is caring for a client experiencing autonomic dysreflexia. Which of the following does the nurse recognize as the source of symptoms?
Explanation
Autonomic dysreflexia is a medical emergency characterized by a sudden onset of excessively high blood pressure, sweating, and headache. It is caused by an overactivity of the autonomic nervous system in response to a noxious stimulus below the level of a spinal cord injury.
Choice B is incorrect because the central nervous system includes the brain and spinal cord, while autonomic dysreflexia is caused by a spinal cord injury.
Choice C is incorrect because the sympathetic nervous system is part of the autonomic nervous system and is involved in the response to autonomic dysreflexia.
Choice D is incorrect because the peripheral nervous system includes the nerves that extend from the brain and spinal cord to the rest of the body.
While performing a physical examination on a client with cirrhosis, which of the following interventions should the nurse report immediately to the physician?
Explanation
Giving non-prescription laxatives to a client with cirrhosis can cause severe dehydration and electrolyte imbalances, which can be life-threatening. The nurse should report this intervention immediately to the physician.
Choice B is incorrect because measuring abdominal girth is a standard nursing intervention for clients with cirrhosis to assess for ascites.
Choice C is incorrect because asking the client about food intake is a standard nursing intervention for assessing nutritional status.
Choice D is incorrect because checking for signs of hepatic encephalopathy is a standard nursing intervention for clients with cirrhosis.
A client with diabetes insipidus is extremely dehydrated and is unable to take oral fluids. Fluid therapy is prescribed. Which intervention would be most important for the client?
Explanation
Monitoring the rate of IV infusions. In clients with diabetes insipidus, fluid therapy is essential to restore hydration levels. It is important to monitor the rate of IV infusion to avoid rapid administration of fluids, which can lead to fluid overload and pulmonary edema. Therefore, monitoring the rate of IV infusions is the most important intervention for this client.
Choice B, weighing the client daily, is incorrect because it is not the most important intervention for this client. While daily weighing is important for monitoring fluid balance, monitoring the rate of IV infusion is more critical.
Choice C, measuring the urine output every 30 minutes, is incorrect because although it is important to monitor urine output in clients with diabetes insipidus, it is not the most important intervention. Monitoring the rate of IV infusion is more critical to prevent fluid overload.
Choice D, measuring the fluid intake, is incorrect because although it is important to monitor fluid intake in clients with diabetes insipidus, it is not the most important intervention. Monitoring the rate of IV infusion is more critical to prevent fluid overload.
The nurse is reviewing a client's history which reveals that the client has had an oversecretion of growth hormone (GH) that occurred before puberty. The nurse interprets this as which of the following?
Explanation
Gigantism. Oversecretion of growth hormone before puberty leads to gigantism, which is characterized by excessive growth in height and length of bones. The growth hormone stimulates the growth of cartilage and bone, resulting in an increased height. When oversecretion occurs after puberty, it results in acromegaly, which is characterized by the enlargement of bones in the face, hands, and feet.
Choice A, Acromegaly, is incorrect because acromegaly results from oversecretion of growth hormone after puberty, and not before puberty.
Choice C, Dwarfism, is incorrect because dwarfism is caused by insufficient growth hormone secretion or poor response to the hormone, and not oversecretion.
Choice D, Simmonds disease, is incorrect because Simmonds disease is a rare disorder characterized by the atrophy of the pituitary gland, which results in decreased secretion of several hormones, including growth hormone.
The nurse is assisting the physician in completing a lumbar puncture. Which would the nurse note as a concern?
Explanation
Cerebrospinal fluid is cloudy in nature. Cloudy cerebrospinal fluid is a sign of infection or inflammation in the central nervous system, and lumbar puncture can be used to obtain cerebrospinal fluid for diagnostic purposes. The nurse should report this finding immediately to the physician for further evaluation and management.
Choice A, client states a piercing feeling, is incorrect because a piercing feeling is common during the procedure due to the insertion of the needle into the subarachnoid space.
Choice B, physician maintains aseptic procedure, is incorrect because maintaining aseptic technique during the procedure is standard protocol to prevent infection.
Choice C, client states a pressure relief in the head, is incorrect because this is not a concerning finding during the procedure.
Which assessment finding is most important in determining which client has a higher risk for developing testicular cancer?
Explanation
cryptorchidism as an infant. Cryptorchidism, or undescended testicles, is a known risk factor for testicular cancer. During fetal development, the testicles form in the abdomen and descend into the scrotum before birth. Failure of one or both testicles to descend into the scrotum can increase the risk of testicular cancer later in life. Therefore, a history of cryptorchidism as an infant is the most important assessment finding to identify clients at higher risk of developing testicular cancer.
Choice A, previous sexually transmitted infection (STI), is incorrect because although STIs can increase the risk of certain types of cancer, they are not a significant risk factor for testicular cancer.
Choice C, low sperm count, is incorrect because although low sperm count can be associated with testicular cancer, it is not a reliable indicator for determining a higher risk for testicular cancer. Low sperm count may also be caused by various other factors, such as hormonal imbalances, infections, varicocele, and genetic abnormalities. While it is important to monitor and treat low sperm count, it is not a definitive indicator of testicular cancer risk.
A client is suspected of having acromegaly. What definitive diagnostic testing is the most reliable for confirming acromegaly?
Explanation
Glucose tolerance test in combination with a Growth hormone measurement. Acromegaly is a condition in which there is an excess of growth hormone (GH) production by the anterior pituitary gland, resulting in abnormal growth of bones and tissues in the body. The definitive diagnostic test for acromegaly involves a glucose tolerance test combined with a measurement of GH levels. During the test, the client will be given a dose of glucose, and the GH levels will be measured before and after the glucose is given. In acromegaly, the GH levels remain elevated even after glucose administration.
Choice A, bone radiographs, may show the enlarged bones associated with acromegaly, but it is not the definitive diagnostic test for the condition.
Choice C, growth hormone levels, is not specific enough for diagnosing acromegaly, as elevated GH levels can occur in other conditions as well.
Choice D, a serum glucose level, is not specific for acromegaly, as the glucose level may be normal in clients with the condition.
Sign Up or Login to view all the 87 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

