Med Surg Exam 3
Total Questions : 41
Showing 25 questions, Sign in for moreWhich of the following medications are used to treat and prevent strokes?
Explanation
Choice A: Antihypertensive medication lowers blood pressure, which reduces the risk of stroke caused by high blood pressure or hypertension.
Choice B: Anti-cholesterol medication lowers the level of cholesterol in the blood, which reduces the risk of stroke caused by atherosclerosis or plaque buildup in the arteries.
Choice C: Antiplatelet medication prevents blood clots from forming, which reduces the risk of stroke caused by ischemia or blockage of blood flow to the brain.
Choice D: All of the above medications are used to treat and prevent strokes, as they address different risk factors and causes of stroke.
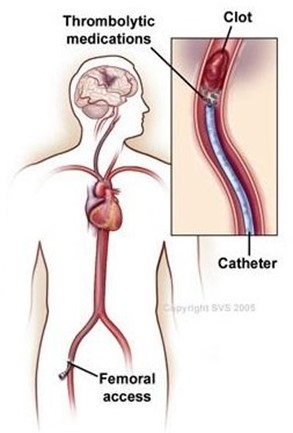
What is the main side effect of IV Thrombolytic therapy TPA?
Explanation
Choice A: High blood pressure is not a side effect of IV Thrombolytic therapy TPA, but rather a contraindication or a reason not to use it. TPA can increase the risk of bleeding in patients with high blood pressure.
Choice B: Bleeding is the main side effect of IV Thrombolytic therapy TPA, as it dissolves blood clots and can cause bleeding in the brain or other parts of the body.
Choice C: Confusion is not a side effect of IV Thrombolytic therapy TPA, but rather a symptom of stroke. TPA can improve confusion by restoring blood flow to the brain.
Choice D: All of the above is not correct, as only bleeding is a side effect of IV Thrombolytic therapy TPA.
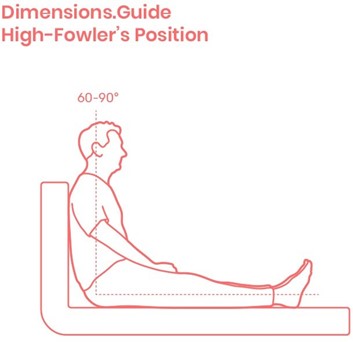
Assisting a stroke patient with feeding would include:
Explanation
Choice A: Head of bed 45 degrees is not enough to prevent aspiration or choking, as the patient may still have difficulty swallowing and clearing their airway.
Choice B: Patient should be on a regular diet to rebuild their swallowing ability is not correct, as the patient may need a modified diet depending on their level of dysphagia or swallowing impairment. A regular diet may pose a risk of aspiration or choking.
Choice C: Have patient sit upright 90 degrees in bed or chair is correct, as this position helps the patient align their head and neck and use gravity to facilitate swallowing and prevent aspiration.
Choice D: All of the above is not correct, as only choice C is appropriate for assisting a stroke patient with feeding.
Which health care discipline would the nurse consult to help a stroke patient with nutrition?
Explanation
Choice A: Speech therapist is correct, as they can assess and treat the patient's swallowing function and recommend appropriate diets and feeding strategies.
Choice B: Respiratory therapist is not correct, as they can help the patient with breathing problems and oxygen therapy, but not with nutrition.
Choice C: Physical therapist is not correct, as they can help the patient with mobility and exercise, but not with nutrition.
Choice D: Social worker is not correct, as they can help the patient with psychosocial and financial issues, but not with nutrition.
Nursing management of headache would include:
Explanation
Choice A: Dark quiet room is correct, as it can reduce the sensory stimulation and help the patient relax and rest.
Choice B: Massage is correct, as it can relieve muscle tension and improve blood circulation in the head and neck.
Choice C: Pain medication is correct, as it can reduce inflammation and block pain signals in the brain.
Choice D: All of the above is correct, as all of these interventions can help manage headache.
Which of the following is a modifiable risk factor of strokes?
Explanation
Choice A: Ethnicity is not a modifiable risk factor of strokes, as it is determined by genetic and cultural factors that cannot be changed.
Choice B: Gender is not a modifiable risk factor of strokes, as it is determined by biological and hormonal factors that cannot be changed.
Choice C: Age is not a modifiable risk factor of strokes, as it is determined by chronological factors that cannot be changed.
Choice D: Obesity is a modifiable risk factor of strokes, as it can be reduced by lifestyle changes such as diet and exercise. Obesity can increase the risk of strokes by causing high blood pressure, diabetes, and heart disease.
Which of the following medications may be used to reduce cerebral edema?
Explanation
Choice A: Corticosteroids is correct, as they can reduce inflammation and swelling in the brain by suppressing the immune system and decreasing the permeability of blood vessels.
Choice B: Antibiotics is not correct, as they are used to treat bacterial infections, not cerebral edema.
Choice C: Tylenol is not correct, as it is a pain reliever and fever reducer, not an anti-inflammatory agent.
Choice D: All of the above is not correct, as only corticosteroids can be used to reduce cerebral edema.
What sign/symptom of a patient would cause the nurse to suspect cerebral spinal fluid leakage?
Explanation
Choice A: Altered level of consciousness is not a sign/symptom of cerebral spinal fluid leakage, but rather a sign/symptom of increased intracranial pressure or brain injury.
Choice B: Painful headache is not a sign/symptom of cerebral spinal fluid leakage, but rather a sign/symptom of meningitis or sinusitis.
Choice C: Salty taste in their mouth, postnasal drip or clear fluid draining from the nose is a sign/symptom of cerebral spinal fluid leakage, as it indicates that the fluid is escaping from the brain or spinal cord through a tear or hole in the meninges or skull.
Choice D: All of the above is not correct, as only choice C is a sign/symptom of cerebral spinal fluid leakage.
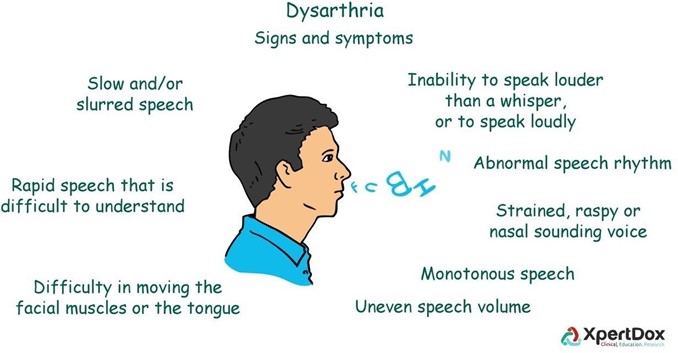
What best describes Dysarthria?
Explanation
Choice A: Paralysis of the joints is not a description of dysarthria, but rather a possible complication of stroke or other neurological disorders.
Choice B: Blindness over half the field of vision is not a description of dysarthria, but rather a sign/symptom of hemianopia or visual field loss.
Choice C: Difficult or unclear articulation of speech is a description of dysarthria, as it is a motor speech disorder caused by weakness or paralysis of the muscles involved in speech production.
Choice D: Paralysis of one side of the body is not a description of dysarthria, but rather a sign/symptom of hemiplegia or unilateral weakness.
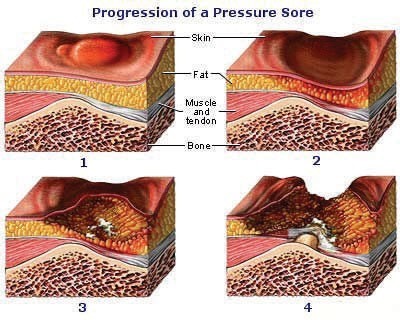
Maintaining skin integrity would include:
Explanation
Choice A: Nutrition supplements is not a direct intervention for maintaining skin integrity, but rather a general measure to support the patient's overall health and healing.
Choice B: Consulting speech therapy is not relevant for maintaining skin integrity, but rather for addressing the patient's communication and swallowing needs.
Choice C: Assessing the skin and frequent repositioning is a correct intervention for maintaining skin integrity, as it can prevent pressure ulcers or bedsores by reducing friction, shear, and moisture on the skin.
Choice D: Ambulating the patient as much as possible is not a specific intervention for maintaining skin integrity, but rather a general measure to promote the patient's mobility and circulation.
Which of the following causes skin breakdown?
Explanation
Choice A: Incontinence is a cause of skin breakdown, as it can expose the skin to moisture, bacteria, and chemicals that can irritate and damage the skin.
Choice B: Altered level of consciousness is a cause of skin breakdown, as it can impair the patient's ability to sense and report pain, discomfort, or pressure on the skin.
Choice C: Immobility is a cause of skin breakdown, as it can reduce the blood flow and oxygen to the skin and increase the pressure on bony prominences.
Choice D: All of the above is correct, as all of these factors can contribute to skin breakdown.
Which of the following is an early sign of intracranial pressure?
Explanation
Choice A: Flaccidity is not an early sign of intracranial pressure, but rather a late sign of brainstem compression or damage.
Choice B: Projectile vomiting is not an early sign of intracranial pressure, but rather a sign of increased pressure in the posterior fossa or cerebellum.
Choice C: Stupor is not an early sign of intracranial pressure, but rather a sign of severe impairment of consciousness or coma.
Choice D: Changes in level of consciousness is an early sign of intracranial pressure, as it reflects the brain's response to decreased oxygen and increased pressure.
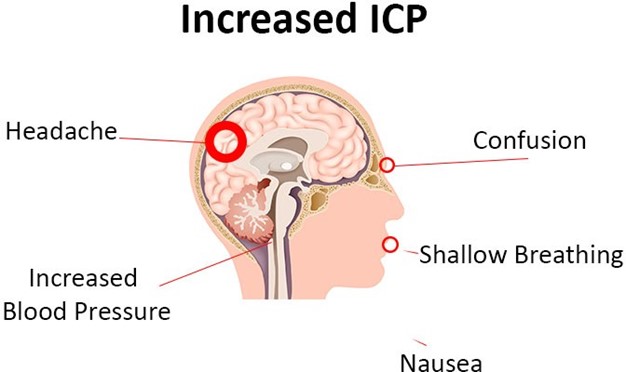
Which of the following is a late sign of intracranial pressure?
Explanation
Choice A: Headache is not a late sign of intracranial pressure, but rather an early sign of increased pressure or irritation of the meninges.
Choice B: Confusion is not a late sign of intracranial pressure, but rather an early sign of impaired cognition or orientation.
Choice C: Stupor to coma is a late sign of intracranial pressure, as it indicates a severe deterioration of consciousness or brain function.
Choice D: Weakness is not a late sign of intracranial pressure, but rather a sign of focal neurological deficit or hemiparesis.

Which Nursing Intervention for the Patient with Increased Intracranial Pressure would be first priority?
Explanation
Choice A: Frequent monitoring of respiratory status and lung sounds and measures to maintain a patent airway is the first priority, as it can prevent hypoxia, hypercapnia, and increased ICP that can lead to brain herniation and death.
Choice B: Maintain a calm, quiet atmosphere and protect patient from stress is not the first priority, but rather a supportive measure to reduce stimuli and agitation that can increase ICP.
Choice C: Use strict aseptic technique for management of ICP monitoring system is not the first priority, but rather a preventive measure to avoid infection and meningitis that can worsen ICP.
Choice D: Position with head in neutral position and elevation of HOB 0 to 60 degrees to promote venous drainage is not the first priority, but rather a therapeutic measure to facilitate blood flow and reduce ICP.
Which of the following describes Akinetic mutism?
Explanation
Choice A: Unresponsiveness to the environment, makes no movement or sound but sometimes opens eyes is a description of akinetic mutism, as it is a state of severe apathy and reduced motor activity caused by damage to the frontal lobes or basal ganglia.
Choice B: Devoid of cognitive function but has sleep-wake cycles is not a description of akinetic mutism, but rather a description of persistent vegetative state, as it is a state of minimal awareness and responsiveness caused by widespread brain damage.
Choice C: Unconsciousness, unarousable unresponsiveness is not a description of akinetic mutism, but rather a description of coma, as it is a state of complete loss of consciousness and reflexes caused by severe brain injury.
Choice D: Inability to move or respond except for eye movements due to a lesion affecting the pons is not a description of akinetic mutism, but rather a description of locked-in syndrome, as it is a state of complete paralysis and preserved consciousness caused by damage to the brainstem.
Which of the following describes a Persistent vegetative state?
Explanation
Choice A: Unconsciousness, unarousable unresponsiveness is not a description of persistent vegetative state, but rather a description of coma, as it is a state of complete loss of consciousness and reflexes caused by severe brain injury.
Choice B: Devoid of cognitive function but has sleep-wake cycles is a description of persistent vegetative state, as it is a state of minimal awareness and responsiveness caused by widespread brain damage.
Choice C: Inability to move or respond except for eye movements due to a lesion affecting the pons is not a description of persistent vegetative state, but rather a description of locked-in syndrome, as it is a state of complete paralysis and preserved consciousness caused by damage to the brainstem.
Choice D: Unresponsiveness to the environment, makes no movement or sound but sometimes opens eyes is not a description of persistent vegetative state, but rather a description of akinetic mutism, as it is a state of severe apathy and reduced motor activity caused by damage to the frontal lobes or basal ganglia.
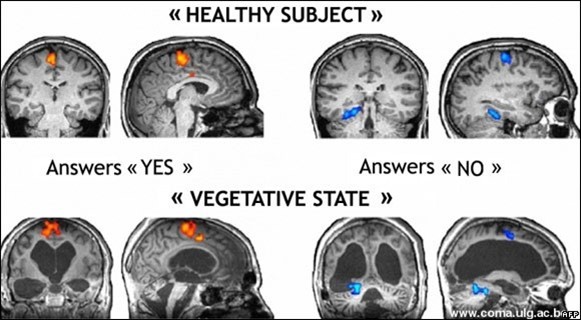
Which of the following describes Locked-in Syndrome?
Explanation
Choice A: Inability to move or respond except for eye movements due to a lesion affecting the pons is a description of locked-in syndrome, as it is a state of complete paralysis and preserved consciousness caused by damage to the brainstem.
Choice B: Unconsciousness, unarousable unresponsiveness is not a description of locked-in syndrome, but rather a description of coma, as it is a state of complete loss of consciousness and reflexes caused by severe brain injury.
Choice C: Unresponsiveness to the environment, makes no movement or sound but sometimes opens eyes is not a description of locked-in syndrome, but rather a description of akinetic mutism, as it is a state of severe apathy and reduced motor activity caused by damage to the frontal lobes or basal ganglia.
Choice D: Devoid of cognitive function but has sleep-wake cycles is not a description of locked-in syndrome, but rather a description of persistent vegetative state, as it is a state of minimal awareness and responsiveness caused by widespread brain damage.
When assessing a patient with altered level of consciousness, which of the following would the nurse assess first?
Explanation
Choice A: Respiratory status is the first priority, as it can affect the oxygenation and perfusion of the brain and other vital organs. The nurse should assess the rate, rhythm, depth, and quality of breathing, as well as the use of accessory muscles, chest expansion, and lung sounds.
Choice B: Alertness is not the first priority, but rather a component of the level of consciousness. The nurse should assess the patient's ability to open their eyes spontaneously or in response to stimuli, as well as their orientation to person, place, time, and situation.
Choice C: Motor response is not the first priority, but rather a component of the level of consciousness. The nurse should assess the patient's ability to move their limbs voluntarily or in response to stimuli, as well as their muscle strength, tone, and coordination.
Choice D: Verbal response is not the first priority, but rather a component of the level of consciousness. The nurse should assess the patient's ability to speak clearly and coherently, as well as their content and appropriateness of speech.
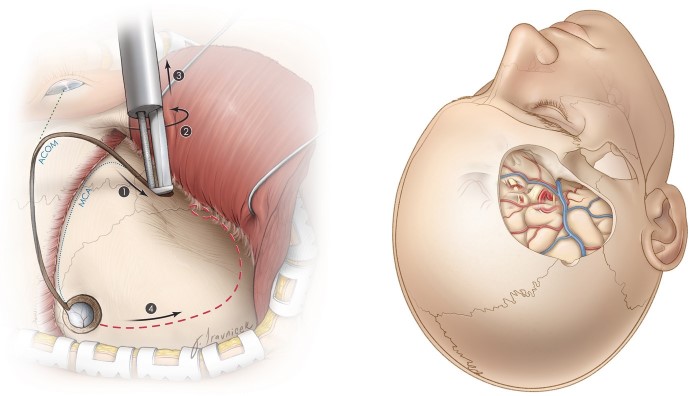
Assessment of the Patient Undergoing Intracranial Surgery would include:
Explanation
Choice A: Careful, frequent monitoring of respiratory function, including blood gases is correct, as it can detect and prevent hypoxia, hypercapnia, and acid-base imbalance that can affect the brain and other organs.
Choice B: Monitor for signs and symptoms of complications is correct, as it can identify and treat potential problems such as hemorrhage, infection, seizures, or increased intracranial pressure.
Choice C: Monitor fluid status and laboratory data is correct, as it can maintain fluid and electrolyte balance and prevent dehydration, overhydration, or cerebral edema.
Choice D: All of the above is correct, as all of these assessments are important for the patient undergoing intracranial surgery.
Planning and goals for a patient with altered level of consciousness would include:
Explanation
Choice A: Maintenance of clear airway is a goal for a patient with altered level of consciousness, as it can prevent aspiration, hypoxia, and respiratory failure.
Choice B: Maintenance of skin integrity is a goal for a patient with altered level of consciousness, as it can prevent pressure ulcers, infection, and sepsis.
Choice C: Protection from injury is a goal for a patient with altered level of consciousness, as it can prevent falls, fractures, and trauma.
Choice D: All of the above is correct, as all of these goals are relevant for a patient with altered level of consciousness.
Maintaining an airway would include:
Explanation
Choice A: Frequent vital sign monitoring including accurate blood sugars is not a direct intervention for maintaining an airway, but rather a general measure to monitor the patient's condition and prevent complications.
Choice B: Accurate intake and output records is not a direct intervention for maintaining an airway, but rather a general measure to monitor the patient's fluid and electrolyte balance and prevent dehydration or overhydration.
Choice C: Updating the patient's family on status is not a direct intervention for maintaining an airway, but rather a supportive measure to provide information and emotional support to the patient's family.
Choice D: Head of bed 30 degrees, suctioning, oral hygiene and monitoring of respiratory status is a correct intervention for maintaining an airway, as it can reduce the risk of aspiration, infection, and obstruction of the airway.
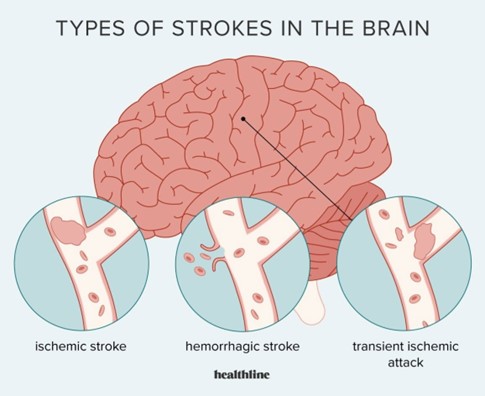
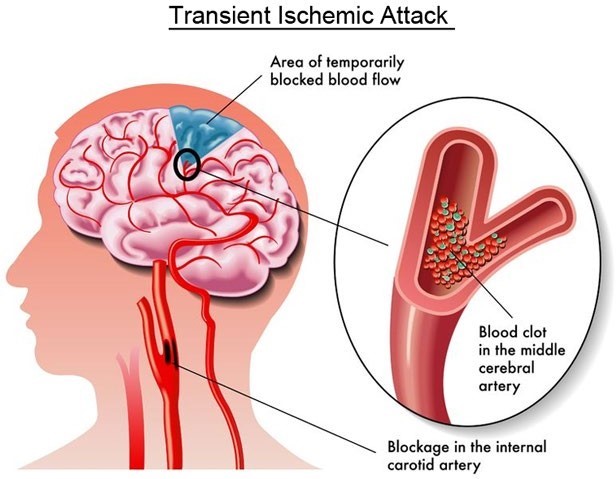
What is the difference between a CVA (Stroke) and TIA (Transient Ischemic Atack)?
Explanation
Choice A: CVA is a temporary neurologic deficit and a TIA is more long-term deficit is not correct, as it reverses the definitions of CVA and TIA.
Choice B: There is no difference is not correct, as there are significant differences between CVA and TIA in terms of duration, severity, and prognosis.
Choice C: TIA is a temporary neurologic deficit and a CVA is more long-term deficit is correct, as it accurately describes the difference between CVA and TIA. A TIA is a brief episode of neurologic dysfunction caused by focal brain ischemia that resolves within 24 hours, while a CVA is a permanent or lasting damage to brain tissue caused by ischemia or hemorrhage.
Choice D: CVA results from temporary impairment of blood flow and TIA is long-term impairment is not correct, as it reverses the causes of CVA and TIA.
Which of the following is the most serious complication of a patient with altered level of consciousness?
Explanation
Choice A: Pressure ulcer is not the most serious complication of a patient with altered level of consciousness, but rather a common and preventable complication that can cause skin breakdown, infection, and pain.
Choice B: Aspiration is the most serious complication of a patient with altered level of consciousness, as it can cause pneumonia, respiratory failure, and death.
Choice C: Contractures is not the most serious complication of a patient with altered level of consciousness, but rather a potential and reversible complication that can cause muscle stiffness, joint deformity, and reduced mobility.
Choice D: Deep vein thrombosis is not the most serious complication of a patient with altered level of consciousness, but rather a possible and treatable complication that can cause blood clots, swelling, and pain in the legs.
What best defines Amyotrophic Lateral Sclerosis ALS "Lou Gehrig Disease?"
Explanation
Choice A: Loss of motor neurons in the brain is not a complete definition of ALS, as it does not include the loss of motor neurons in the spinal cord and brainstem.
Choice B: Loss of sensory neurons in the anterior horn of the spinal cord is not a correct definition of ALS, as it involves sensory neurons, not motor neurons.
Choice C: Loss of motor neurons in the anterior horn of the spinal cord and loss of motor nuclei of the lower brainstem is a correct definition of ALS, as it describes the progressive degeneration and death of both upper and lower motor neurons that control voluntary muscle movements²⁴.
Choice D: All of the above is not correct, as only choice C is a correct definition of ALS.
Manifestations of Amyotrophic Lateral Sclerosis would include:
Explanation
Choice A: Progressive weakness and atrophy of muscle is a manifestation of ALS, as it results from the loss of motor
neurons that control voluntary muscle movements²³.
Choice B: Cramps, twitching, and lack of coordination is a manifestation of ALS, as it results from the abnormal activity of motor neurons that are still functioning²³.
Choice C: Spasticity, deep tendon reflexes brisk, and overactive is a manifestation of ALS, as it results from the damage to the upper motor neurons that regulate muscle tone²³.
Choice D: Difficulty speaking, swallowing, breathing is a manifestation of ALS, as it results from the involvement of the muscles in the mouth, throat, and chest²³.
Choice E: All of the above is correct, as all of these manifestations are common in ALS.

Sign Up or Login to view all the 41 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

