MED SURG EXAM 5
Total Questions : 68
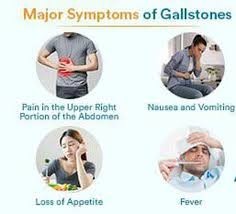
Showing 25 questions, Sign in for moreWhich assessment findings will the nurse anticipate in the client with cholelithiasis?
Explanation
Cholelithiasis refers to the presence of gallstones in the gallbladder or bile ducts. The most common symptom is right upper quadrant abdominal pain, which may be colicky or steady. Nausea and vomiting are also commonly associated with cholelithiasis.
Coffee ground emesis and constipation are not typical findings associated with cholelithiasis. Absent bowel sounds may be a sign of bowel obstruction but are not specific to cholelithiasis.
The nurse is caring for an adolescent diagnosed with scoliosis who just arrived to the floor from the recovery room after a Spinal fusion surgery. The nurse should question which physician order?
Explanation
After spinal fusion surgery, it is important to limit the patient's activity and movement to allow for proper healing and to prevent complications. The order to have the patient out of bed three times daily and ad lib (as desired) is not appropriate immediately after surgery.
The other orders listed are appropriate for the postoperative care of a patient who has undergone spinal fusion surgery:
- Assess neurological status every 4 hours: This is important to monitor for any changes in neurological function, which could indicate complications such as nerve damage or spinal cord compression.
- Logroll only to change position: Logrolling is a technique used to move patients with spinal fusion surgery while keeping their spine aligned and minimizing stress on the surgical site. This order is appropriate to ensure proper positioning and prevent injury to the surgical area.
- Monitor vital signs every 4 hours: Monitoring vital signs helps to assess the patient's overall condition and detect any signs of complications such as bleeding or infection.
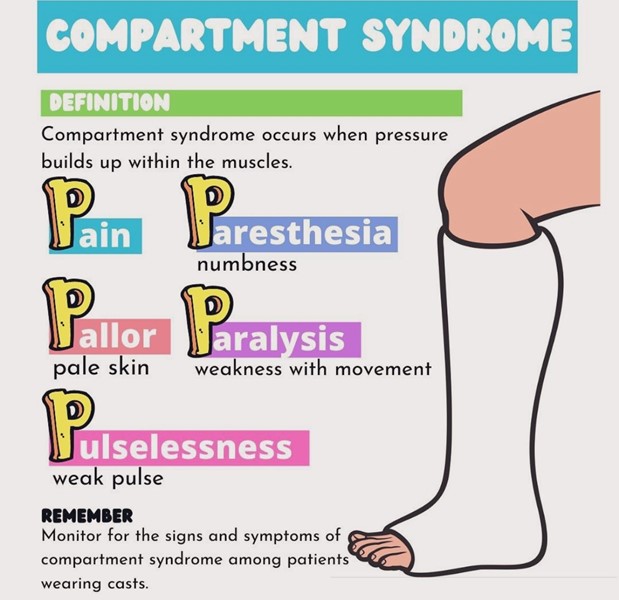
The nurse is caring for a preschool child with a cast applied recently for a fractured tibia. Which assessment finding indicates possible compartment syndrome?
Explanation
Compartment syndrome is a condition characterized by increased pressure within a muscle compartment, leading to impaired blood flow and potential tissue damage. It can occur when swelling or bleeding within a confined space, such as a cast, causes increased pressure on the surrounding tissues.
Tingling in the toes and decreased sensation can be indicative of nerve compression or damage due to increased pressure in the compartment. It is important to recognize these neurological changes as potential signs of compartment syndrome.
Signs and symptoms of compartment syndrome may include:
- Severe pain that is out of proportion to the injury or not relieved by pain medication.
- Swelling and tightness in the affected area.
- Numbness or tingling.
- Pale or cool skin over the affected area.
- Weakness or decreased sensation in the affected limb.
- In severe cases, paralysis or loss of pulse in the affected area.
The nurse will plan to teach a patient who has pernicious anemia about the need for:
Explanation
Pernicious anemia is a type of anemia that occurs due to a lack of intrinsic factor, a protein necessary for the absorption of vitamin B12 (cobalamin) in the digestive system. As a result, patients with pernicious anemia are unable to absorb sufficient amounts of vitamin B12 from dietary sources. The treatment for pernicious anemia involves regular administration of cobalamin (B12) injections to bypass the impaired absorption and provide the necessary vitamin B12 directly.
Oral ferrous sulfate tablets are not the appropriate treatment for pernicious anemia. Ferrous sulfate is a form of iron supplement used to treat iron deficiency anemia, which is different from pernicious anemia.
Iron dextran infusions are also not indicated for pernicious anemia. Iron dextran is used for iron replacement therapy in cases of iron deficiency anemia, but it does not address the underlying issue of vitamin B12 deficiency in pernicious anemia.
Routine blood transfusions may be necessary in some cases of pernicious anemia, especially if the patient is severely anemic. However, the primary treatment for pernicious anemia is cobalamin (B12) injections, which provide the necessary vitamin B12 that the patient is unable to absorb.
The nurse provides education to a female patient diagnosed with iron deficiency anemia. Which patient statements indicate a correct understanding of iron deficiency?
SELECT ALL THAT APPLY
Explanation
These statements reflect the appropriate knowledge related to iron deficiency anemia. Iron-rich foods such as meat and beans can help increase iron levels in the body. Vitamin C aids in the absorption of iron, so taking a Vitamin C supplement can enhance iron absorption. Iron deficiency anemia is more common during pregnancy or menstruation due to increased iron demands.
However, increasing intake of dairy products alone does not address the iron deficiency. The statement about oral supplements not being as effective as monthly subcutaneous injections is incorrect, as oral iron supplements are commonly used to treat iron deficiency anemia and are effective in most cases.
The nurse is preparing to witness the patient signing the operative consent form when the patient says, "I don't understand what the doctor said about the surgery." Which action should the nurse take next?
Explanation
It is important for patients to have a clear understanding of their surgical procedure before providing informed consent. The nurse should take the responsibility to ensure that the patient receives all the necessary information and has any questions or concerns addressed. By providing a thorough explanation of the planned surgical procedure, the nurse can help the patient make an informed decision and clarify any misunderstandings.
While notifying the surgeon or the operating room nurse may be appropriate in some situations, the initial response should be to address the patient's concerns directly and provide the necessary information. Administering preoperative antibiotics and withholding sedative medications is unrelated to the issue of the patient's understanding and informed consent. The primary focus should be on ensuring that the patient has a clear understanding of the surgical procedure and feels confident in giving informed consent.
What is one airway complication that can occur during surgery when the patient is receiving general anesthesia care?
Explanation
Aspiration refers to the inhalation of gastric contents or other substances into the respiratory tract. During surgery, when the patient is under general anesthesia, the protective airway reflexes may be suppressed, increasing the risk of aspiration. If stomach contents enter the lungs, it can lead to aspiration pneumonia, respiratory distress, and other complications.
While myocardial infarction (MI), hernia, and cerebral vascular accident (CVA) are possible complications that can occur during surgery, they are not specifically related to airway issues.
MI is a cardiac event involving the blood supply to the heart muscle, hernia refers to the protrusion of an organ or tissue through an abnormal opening, and CVA refers to a disruption of blood flow to the brain. These complications can have various causes but are not directly related to the airway during surgery.
A client is admitted with Diabetic Ketoacidosis (DKA). The client asks the nurse "Why did this happen? I have been taking my insulin as prescribed and following my diet carefully" The nurse reviews the client's chart and realizes that this emergency may be related to which common causes of DKA?
Explanation
Prednisone is a corticosteroid medication that can increase blood glucose levels by promoting gluconeogenesis (the production of glucose from non-carbohydrate sources) and reducing glucose utilization in the body. This can lead to elevated blood sugar levels, especially in individuals with diabetes. The client's history of urinary tract infection and the use of Prednisone suggest that the infection might have triggered the development of DKA.
It's important to note that DKA can occur even when a person is taking insulin as prescribed and following their diet carefully if other factors contribute to the development of DKA, such as an underlying infection or the use of certain medications like Prednisone. The nurse should further assess the client's condition and notify the healthcare provider to initiate appropriate management for DKA.
Aydan Miller is an 8-year-old with a history of Type 1 Diabetes. Current medications are: Glargine (Lantus; Insulin 5 units subcutaneous at bedtime Insulin lispro (Humalog) 1 unit per 50 grams of carbohydrates eaten. Aydan has just eaten 150 grams of carbs for lunch at school.
Which of the following medications will the nurse prepare to administer to Aydan?
Explanation
According to the given information, Aydan's insulin lispro (Humalog) dosage is 1 unit per 50 grams of carbohydrates eaten. As Aydan has just consumed 150 grams of carbs for lunch, we can calculate the insulin dose as follows:
Insulin dose = Carbohydrates eaten / Insulin-to-carbohydrate ratio Insulin dose = 150 grams / 50 grams/unit
Insulin dose = 3 units
Therefore, the nurse should prepare to administer 3 units of Aydan's prescribed rapid-acting insulin (Insulin lispro) to cover the carbohydrates he consumed for lunch. The long-acting insulin (Glargine) is typically given at bedtime to provide a basal insulin level and is not directly related to meal coverage.
A patient has been treated for lung cancer for 3 years. Over the past few months, the patient has noticed that the opioid analgesic is not helping as much as it had previously and more medication is needed for the same pain relief. The nurse is aware that this patient is experiencing which of these?
Explanation
Opioid tolerance occurs when the body becomes less responsive to the effects of opioids over time. This means that higher doses of the medication are needed to achieve the same level of pain relief that was previously achieved with lower doses. Opioid tolerance is a common phenomenon in long-term opioid therapy and can occur in patients who have been using opioids for an extended period.
Opioid abstinence syndrome, also known as opioid withdrawal, refers to the set of symptoms that occur when a person abruptly stops or reduces their use of opioids after developing physical dependence.
Opioid toxicity refers to the harmful effects that occur when an individual takes an excessive dose of opioids, leading to potentially life-threatening complications. It is characterized by symptoms such as respiratory depression, sedation, pinpoint pupils, and decreased level of consciousness.
Opioid addiction is a complex condition characterized by compulsive drug-seeking behavior, loss of control over opioid use, and continued use despite negative consequences.
A patient is receiving Gabapentin (Neurontin), an anticonvulsant, but has no history of seizures. The nurse expects that the patient is receiving this drug for which condition?
Explanation
Gabapentin (Neurontin) is often used to treat neuropathic pain, including pain associated with peripheral neuropathy. It may also be used to manage other types of chronic pain, such as pain associated with fibromyalgia. While gabapentin is primarily an anticonvulsant medication, it is also used off-label for various other conditions, such as mood disorders and anxiety.
The initial bundle of care in sepsis includes which of the following? (Select all that apply.)
Explanation
The initial bundle of care in sepsis includes the following:
- Obtain blood cultures: Blood cultures help identify the specific microorganism causing the infection, which is important for guiding appropriate antibiotic therapy.
- Administer broad-spectrum antibiotics: Early administration of antibiotics is crucial in sepsis to target the suspected or likely infectious organisms. Broad-spectrum antibiotics cover a wide range of potential pathogens until more specific information from culture results is available.
- Obtain lactate levels: Measuring lactate levels helps assess tissue perfusion and can be used as an indicator of the severity of sepsis. Elevated lactate levels are associated with tissue hypoperfusion and increased mortality.
- Administer IV fluid bolus: Early aggressive fluid resuscitation is an essential component of sepsis management. Administering intravenous fluids helps restore intravascular volume and improve tissue perfusion.
- Administration of vasopressors: Especially in the setting of hypotension and to maintain MAP above 65mmHg.
The nurse is admitting a client diagnosed with acute renal failure (ARF). The nursing assessment will prioritize ...
Explanation
Acute renal failure is characterized by a sudden decline in kidney function, resulting in the inability of the kidneys to adequately filter waste products and maintain fluid and electrolyte balance. Monitoring urine output is essential in assessing kidney function and determining the severity of renal failure. A decrease in urine output or anuria may indicate worsening renal function and the need for immediate interventions.
Assessing electrolyte levels, such as sodium, potassium, calcium, and phosphorus, is crucial because renal failure can disrupt the balance of these electrolytes in the body. Imbalances can lead to complications such as electrolyte abnormalities, cardiac dysrhythmias, and neuromuscular disturbances. Prompt identification and management of electrolyte imbalances are essential in preventing further complications and supporting optimal patient outcomes.
The nurse is teaching a client with chronic renal failure (CRF) about the use of recombinant human erythropoietin (Epogen) Subcutaneous injections. Which statement indicates the client understands the teaching?
Explanation
Recombinant human erythropoietin is a medication commonly used in the treatment of anemia associated with chronic renal failure. It stimulates the production of red blood cells in the bone marrow, helping to improve anemia.
The other statements mentioned do not accurately reflect the expected outcomes or effects of recombinant human erythropoietin:
Chronic renal failure leads to impaired kidney function, and while recombinant human erythropoietin can help address anemia, it does not directly improve creatinine (Cr) and blood urea nitrogen (BUN) levels, which are markers of kidney function.
Furosemide is a diuretic commonly used in the management of fluid retention in renal failure. Recombinant human erythropoietin does not replace or eliminate the need for diuretic therapy.
Chronic renal failure typically involves decreased kidney function and impaired urine production. Recombinant human erythropoietin does not directly affect urine output.
The nurse is caring for an infant with a hip spica cast who has just returned from surgery. Which nursing action will be priority for this patient?
Explanation
Hip spica casts are typically used to immobilize the hip joint and are often used in the management of hip dysplasia or after surgery. These casts can cause restricted mobility and limit blood flow to the legs and feet, which can lead to complications such as swelling, decreased circulation, or pressure sores.
Checking capillary refill in the toes is a critical nursing intervention to assess for the presence of adequate circulation and blood flow to the affected limb. If capillary refill is slow or absent, it may indicate compromised circulation and require immediate intervention to prevent further complications.
Palpating a brachial pulse, assessing bilateral radial pulses, or auscultating the heart rate apically are not the priority nursing actions for an infant with a hip spica cast. While monitoring vital signs and circulation are important components of nursing care, the priority at this stage is to assess and manage the immediate postoperative needs of the patient, including monitoring for potential complications related to the hip spica cast.

A school nurse is performing screening examinations for scoliosis. Which signs of scoliosis should the nurse assess for?
Explanation
Unequal scapula and hip heights can be indicative of spinal curvature, a key characteristic of scoliosis. As the spine curves, it can cause the shoulders and hips to appear uneven when observed from behind. This asymmetry is an important visual clue that warrants further assessment and evaluation.
Equal rib prominence and tight-fitting clothes, equal waist and shoulder angles, and symmetric chest expansion with deep breaths are not specific signs of scoliosis. These signs may not be affected by spinal curvature and are not typically used in the screening process for scoliosis.
It's important to note that scoliosis screenings may involve more comprehensive assessments, including the use of scoliometers or other measuring tools to evaluate the degree of spinal curvature. Any concerns or suspicions of scoliosis should be reported to appropriate healthcare professionals for further evaluation and management.

Why it is important to immobilize a suspected fracture. The nurse explains that immobilizing a fracture will... (SELECT ALL THAT APPLY)
Explanation
The nurse explains that immobilizing a fracture will:
- Help align the bone fragments and reduce movement, which is crucial for proper healing. Immobilization can help maintain the stability of the fracture site, allowing the bones to knit together and heal.
- Help to minimize movement and subsequent pain. It provides support and reduces stress on the injured area, which can help alleviate discomfort and promote a more comfortable healing process.
- Help to minimize movement and reduce the risk of fat globules from bone marrow entering the bloodstream and causing a fat embolism, a potentially serious complication.
Preventing blood clots, preventing malignant hyperthermia, and immobilizing a fracture are not directly related. Preventing blood clots typically involves other measures such as early mobilization, elevation, and medication to prevent deep vein thrombosis. Malignant hyperthermia is a rare, potentially life-threatening reaction to certain medications used during anesthesia, and immobilization does not directly prevent it.
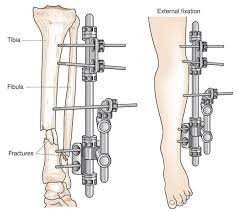
A patient with a right lower leg fracture will be discharged home with an external fixation device in place. Which information will the nurse teach?
Explanation
Pin site care is essential to prevent infections and other complications associated with external fixation devices. The nurse should instruct the patient to clean the pin insertion sites daily with a sterile saline solution or as per healthcare provider's instructions. The patient should also observe for signs of infection, such as redness, swelling, warmth, and drainage, and report any concerns to the healthcare provider.
Assessing the skin under the foam boot twice daily is not specific to external fixation devices, and it may not be relevant to this patient's care plan. The nurse should focus on teaching the patient about external fixation device care specifically.
Taking prophylactic antibiotics before any dental work for the rest of your life is not relevant to external fixation devices or right lower leg fractures. It is a recommendation for patients with certain heart conditions who may be at risk of developing infective endocarditis during dental procedures.
Removing the external fixator for the shower is not recommended as the device should be kept dry to prevent infections. The nurse should instruct the patient to cover the device with a waterproof dressing or plastic bag during showering to protect it from getting wet.
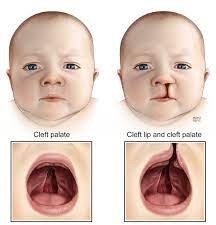
During the first few days after surgery for cleft lip, which intervention should the nurse implement?
Explanation
Suctioning secretions away from the suture line helps maintain the surgical site's cleanliness and promotes healing. It helps prevent accumulation of mucus or oral secretions that can interfere with the healing process and increase the risk of infection. The nurse should use a gentle suctioning technique to avoid disrupting the surgical site.
Applying Neosporin to the surgical site is not typically recommended unless specifically prescribed by the healthcare provider. It is important to follow the provider's instructions regarding wound care.
Applying elbow immobilizers when not being held is not necessary for cleft lip surgery. Elbow immobilizers are usually used in other surgical procedures or for other reasons, such as preventing contractures.
Feeding increased amounts of formula to prevent weight loss is not an appropriate intervention for the first few days after cleft lip surgery. The surgical site may be sensitive, and the child may experience difficulty with feeding initially. The nurse should provide guidance and support for feeding techniques appropriate for the child, which may include using specialized bottles or positioning techniques.
Which assessment information is most important for the nurse to obtain when evaluating whether treatment of a patient with anaphylactic reaction has been effective?
Explanation
Anaphylaxis is a severe and potentially life-threatening allergic reaction that can lead to a rapid drop in blood pressure, known as hypotension. This drop in blood pressure is a critical indicator of the severity of the reaction and the effectiveness of the treatment provided. The nurse needs to monitor the patient's blood pressure closely to ensure it stabilizes and returns to a safe range.
While oxygen saturation, heart rate, and orientation are also important parameters to assess, they are secondary to blood pressure in evaluating the effectiveness of treatment for anaphylaxis. Oxygen saturation can help determine the adequacy of oxygenation, heart rate can indicate the presence of tachycardia (which may be a sign of an ongoing reaction or hypoperfusion), and orientation can provide information about the patient's mental status and potential complications.
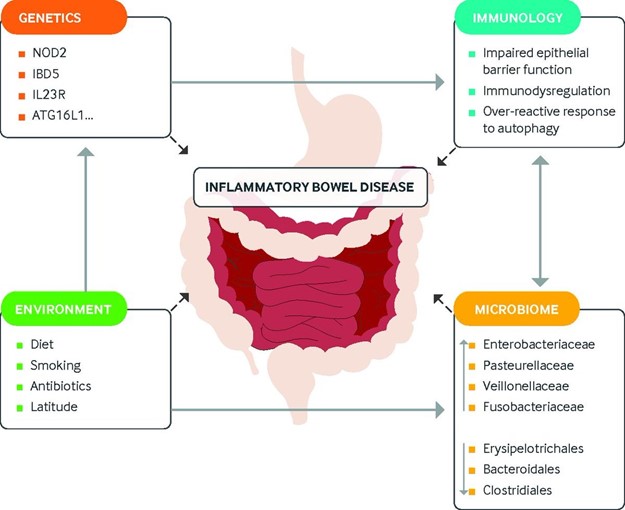
A child is admitted to the hospital and diagnosed with inflammatory bowel disease. The nurse should evaluate the patient for which most likely associated symptoms?
Explanation
IBD, which includes conditions such as Crohn's disease and ulcerative colitis, is characterized by chronic inflammation of the gastrointestinal tract. The symptoms can vary depending on the type and severity of the disease, but common symptoms in children with IBD include:
- Children with IBD often experience increased frequency of bowel movements, which may be loose or watery. This is often accompanied by urgency and a sense of incomplete evacuation.
- Chronic inflammation in the gastrointestinal tract can interfere with nutrient absorption, leading to poor appetite, decreased intake, and subsequent weight loss. In severe cases, malnutrition may occur.
- Inflammatory processes in the intestines can lead to increased motility and peristalsis, resulting in hyperactive bowel sounds.
Therapeutic management for an adolescent with Crohn's Disease includes which treatment?
Explanation
Crohn's Disease is an inflammatory bowel disease that can affect any part of the digestive tract. The goal of treatment is to control inflammation, relieve symptoms, and prevent complications. To achieve this, the healthcare provider may prescribe medication such as anti-inflammatory drugs, immunosuppressants, or biologic therapies that target specific inflammatory pathways.
These medications can help reduce inflammation and improve symptoms.
In addition to medication, nutritional therapy may also be recommended to help manage Crohn's Disease. However, dietary restrictions to reduce calorie and fat intake to lose weight or restrict foods containing gluten to control symptoms are not specific treatments for Crohn's Disease.
Keeping the child in isolation to prevent the spread of the infection is not relevant to Crohn's Disease, as it is not contagious.
What are the most important nursing interventions for clients with possible renal calculi? List two.
Explanation
Lithotripsy and Encourage increased fluid intake are the most important interventions.
A client is admitted with Diabetic Ketoacidosis (DKA). The client asks the nurse "Why did this happen? I have been taking my insulin as prescribed and following my diet carefully" The nurse reviews the client's chart and realizes that this emergency may be related to which common causes of DKA?
Explanation
Prednisone is a corticosteroid medication that can increase blood glucose levels by promoting gluconeogenesis (the production of glucose from non-carbohydrate sources) and reducing glucose utilization in the body. This can lead to elevated blood sugar levels, especially in individuals with diabetes. The client's history of urinary tract infection and the use of Prednisone suggest that the infection might have triggered the development of DKA.
It's important to note that DKA can occur even when a person is taking insulin as prescribed and following their diet carefully if other factors contribute to the development of DKA, such as an underlying infection or the use of certain medications like Prednisone. The nurse should further assess the client's condition and notify the healthcare provider to initiate appropriate management for DKA.
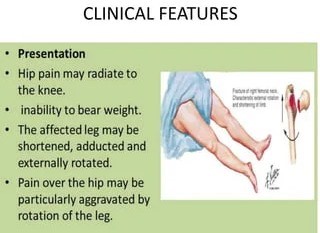
An older adult client fell while getting out of bed. Which assessment finding indicates a possible hip fracture?
Explanation
This finding suggests that the client may have experienced a hip fracture. The shorter leg can be a result of the fractured bone, causing a misalignment or displacement. The protruding bump on the side can be a sign of a dislocated or fractured hip joint. It is important to assess and confirm this suspicion through appropriate diagnostic measures, such as X-rays, to provide the necessary medical intervention and management.
Sign Up or Login to view all the 68 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

