Med Surg, Urinary, Fluid and Electrolytes
Total Questions : 40
Showing 25 questions, Sign in for moreThe nurse caring for a client reviews the medical record and determines the client is at risk for developing a potassium deficit because of which situation?
Explanation
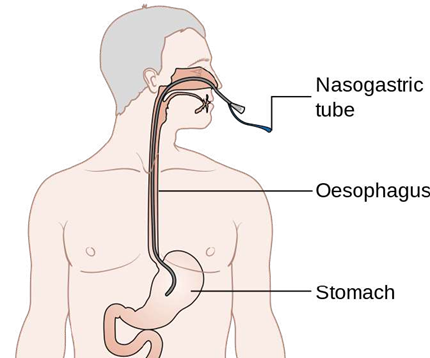
Nasogastric suction removes gastric secretions that contain potassium, leading to a loss of potassium from the body. This can cause hypokalemia, which is a low level of potassium in the blood.
Choice A is wrong because Addison’s disease causes hyperkalemia, which is a high level of potassium in the blood.
Choice B is wrong because tissue damage can release potassium from the cells into the blood, causing hyperkalemia.
Choice C is wrong because uric acid level is not related to potassium level.
Uric acid is a waste product of purine metabolism that can cause gout or kidney stones if elevated.
The nurse is assessing a client with hypocalcemia.
What clinical manifestation would the nurse expect to note in this client?
Explanation
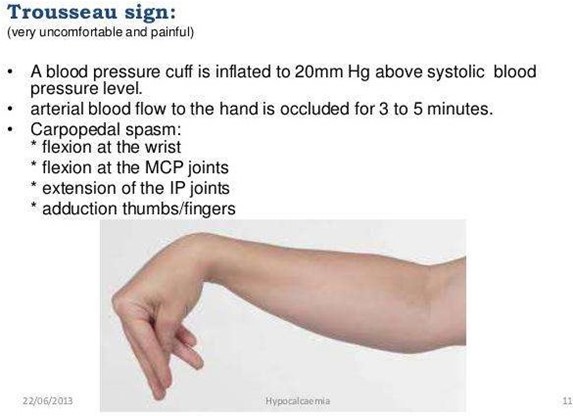
Trousseau’s sign is a test for hypocalcemia that involves inflating a blood pressure cuff on the arm and observing for carpal spasm. A positive sign indicates low calcium levels in the blood, which can cause neuromuscular irritability.
Choice B is wrong because hyperactive deep tendon reflexes are a sign of hypomagnesemia, which is a low level of magnesium in the blood.
Choice C is wrong because hyperactive bowel sounds are a sign of hyperkalemia, which is a high level of potassium in the blood.
Choice D is wrong because muscle twitching can be caused by many factors, such as anxiety, caffeine, or electrolyte imbalance, and is not specific to hypocalcemia.
The client has an IV of dextrose 5% in 0.45% normal saline. The physician has ordered a transfusion of one unit of packed red blood cells (PRBCs).
Before hanging the blood, the nurse will prime the blood tubing with which of the following solutions?
Explanation
This is the only solution that is isotonic and compatible with blood products. It will not cause hemolysis or clotting of the blood cells.
Choice B is wrong because lactated Ringer’s is a balanced electrolyte solution that contains calcium, which can cause clotting of the blood cells.
Choice C is wrong because 5% dextrose is a hypotonic solution that can cause hemolysis of the blood cells.
Choice D is wrong because 5% dextrose in 0.45% sodium chloride is a hypertonic solution that can cause hemolysis of the blood cells.
The nurse on a urology unit is caring for a client diagnosed with calcium oxalate renal calculi.
When planning this client's health education, what nutritional guidelines should the nurse provide?
Explanation

Protein intake can increase the excretion of calcium and oxalate in the urine, which can promote the formation of calcium oxalate stones. The client should limit animal protein sources, such as meat, poultry, fish, eggs, and dairy products.
Choice A is wrong because purine-rich foods, such as organ meats, shellfish, and beer, can increase the production of uric acid, which can cause uric acid stones.
Choice B is wrong because a low-calcium diet can increase the absorption of oxalate in the intestine, which can increase the risk of calcium oxalate stones.
The client should consume a moderate amount of calcium from dietary sources, such as milk, cheese, yogurt, and green leafy vegetables.
Choice C is wrong because potassium-rich foods, such as bananas, oranges, potatoes, and tomatoes, can help prevent calcium oxalate stones by increasing the urinary pH and citrate levels.
The client should consume adequate amounts of potassium from dietary sources.
A client who is NPO has an order for 1000 mL of D5W 0.45% NS with 40 mEq of potassium over 24 hours.
How many mL/h should the IV pump be programmed for?
Math instructions: IV calculations: (rate-mL/hr).
Although some IV pumps do allow calibration to the tenth or hundredth, for the purpose of exams, IV rate calculations will be rounded to the nearest whole number.
Explanation
To find the IV rate, divide the total volume by the total time. In this case, 1000 mL / 24 hours = 41.67 mL/h.
Round this to the nearest whole number, which is 42 mL/h.
However, this does not account for the potassium that is added to the solution.
Potassium has a volume of 1 mL per mEq, so 40 mEq of potassium will add 40 mL to the total volume.
Therefore, the adjusted volume is 1000 mL + 40 mL = 1040 mL.
Divide this by 24 hours to get the new IV rate: 1040 mL / 24 hours = 43.33 mL/h. Round this to the nearest whole number, which is 44 mL/h.
Choice A is wrong because it does not account for the potassium volume. Choice A is wrong because it does not account for the potassium volume.
Choice D is wrong because it adds too much volume for the potassium.
The physician has prescribed 30 mEq of potassium gluconate to be given orally once a day in orange juice.
The available concentration of potassium gluconate is 20 mEq per 15 mL.
What is the amount of mL the nurse will administer Instructions: Rounding: For adult clients, the answer should be rounded to the nearest whole number (mg, mcg, and m).
Explanation
The correct answer is 22.5 mL.
To find the amount of mL, use the formula: (desired dose / available dose) x available volume.
In this case, desired dose = 30 mEq, available dose = 20 mEq, and available volume = 15 mL.
Plug these values into the formula: (30 mEq / 20 mEq) x 15 mL = 22.5 mL.
However, since the instructions say to round to the nearest whole number for adult clients, the final answer is 23 mL.
The physician's orders read: Give cortisone 0.015 grams every 8 hours orally. The pharmacy sends cortisone 10mg tablets.
How many tablet(s) will the nurse give Instructions: Rounding: For adult clients, the answer should be rounded to the nearest tenth (mg, mcg, and m).
Explanation
The correct answer is 1.5 tablets.
To find the number of tablets, use the formula: (desired dose / available dose) x 1 tablet.
In this case, desired dose = 0.015 grams, and available dose = 10 mg.
However, these units are not the same, so they need to be converted to a common unit.
One gram is equal to 1000 mg, so 0.015 grams is equal to 15 mg.
Plug these values into the formula: (15 mg / 10 mg) x 1 tablet = 1.5 tablets.
However, since the instructions say to round to the nearest tenth for adult clients, the final answer is 1.5 tablets.
What is the normal value (NV) for sodium in the blood.
Explanation
According to Healthline1 and Mayo Clinic, the normal blood sodium level is between 135 and 145 milliequivalents per liter (mEq/L).
Choice A is wrong because it is the normal range for potassium, not sodium.
Choice B is wrong because it is the normal range for calcium, not sodium.
Choice D is wrong because it is the normal range for chloride, not sodium
What is the most accurate indicator of fluid loss or gain in acutely ill patients?
Explanation
The correct answer is choice A. Daily weight.

According to MDCalc, daily weight is the most accurate indicator of fluid loss or gain in acutely ill patients, as it reflects changes in total body water.
A weight change of 1 kg corresponds to a fluid change of approximately 1 L.
Choice B is wrong because intake and output measurements can be inaccurate or incomplete, and do not account for insensible fluid losses.
Choice C is wrong because serum osmolality reflects the concentration of solutes in the blood, not the volume of fluid.
Choice D is wrong because urine specific gravity reflects the concentration of solutes in the urine, not the volume of fluid.
What is the term for an excess of urea and other nitrogenous wastes in the blood as a result of kidney insufficiency?
Explanation

Uremia is a condition where there is an excess of urea and other nitrogenous wastes in the blood, usually excreted by the kidneys into the urine. It occurs when the kidneys stop filtering toxins out through your urine and can be a sign of end-stage renal (kidney) disease.
Choice A is wrong because azotemia is the buildup of nitrogen waste products in the blood, not urea.
Choice C is wrong because anuria is the absence or reduction of urine output.
Choice D is wrong because oliguria is the low output of urine.
Which of the following would be the best indicator of adequate hydration?
Explanation
Increased urine output is a sign of adequate hydration, as it means the kidneys are filtering waste and fluids from the body through the urine. The urine should be pale straw or lemonade colored, which indicates good hydration.
Choice B is wrong because decreased urine output is a sign of dehydration, as it means the kidneys are not working well and waste products are accumulating in the blood.
The urine may be dark and strong smelling, which indicates poor hydration.
Choice C is wrong because dry mucous membranes are a sign of dehydration, as they indicate a lack of fluid in the body tissues.
Choice D is wrong because hypertension is not a direct indicator of hydration status, although dehydration can cause low BP due to reduced blood volume.
The nurse is caring for a patient with hyponatremia.
Which of the following interventions would be appropriate?
Explanation

Hyponatremia is a condition where the serum sodium level is below 135 mEq/L, which can affect the normal functioning of cells, muscles, and organs.
Administering intravenous fluids with a high sodium content can help restore the sodium balance and prevent complications such as confusion, seizures, and coma.
Choice A is wrong because encouraging the patient to consume a low-sodium diet would worsen the hyponatremia and increase the risk of electrolyte imbalance.
Choice C is wrong because administering a diuretic medication to increase urine output would cause further fluid and sodium loss and exacerbate the hyponatremia.
Choice D is wrong because encouraging the patient to increase fluid intake would dilute the sodium concentration and lower the serum sodium level.
The nurse is assessing a patient with acute renal failure.
Which of the following would be a priority nursing intervention?
Explanation
This is because acute renal failure is a condition where the kidneys lose their ability to filter waste and excess fluid from the blood. This can lead to fluid overload, electrolyte imbalances, and metabolic acidosis. Therefore, the nurse should monitor the patient’s urine output and fluid balance to assess the severity of the renal impairment and prevent complications.
Choice A is wrong because administering a potassium-sparing diuretic would worsen the patient’s hyperkalemia, which is a common complication of acute renal failure.
Choice B is wrong because encouraging the patient to consume a high-sodium diet would increase the patient’s fluid retention and blood pressure, which can further damage the kidneys.
Choice D is wrong because administering intravenous antibiotics is not a priority intervention for acute renal failure unless there is a specific indication of infection.
The nurse is caring for a patient with hyperkalemia.
Which of the following interventions would be appropriate?
Explanation

This is because hyperkalemia is a condition where the blood potassium level is too high.
This can cause cardiac arrhythmias, muscle weakness, and paralysis. Therefore, the nurse should administer intravenous insulin and glucose to lower the blood potassium level by shifting it into the cells.
Choice A is wrong because encouraging the patient to consume a high- potassium diet would increase the blood potassium level and worsen the condition.
Choice C is wrong because administering a potassium-sparing diuretic would prevent the excretion of excess potassium and aggravate the hyperkalemia.
Choice D is wrong because encouraging the patient to limit fluid intake is not relevant to the management of hyperkalemia and may cause dehydration.
The nurse is assessing a patient with a urinary catheter.
Which of the following would be a priority nursing intervention?
Explanation
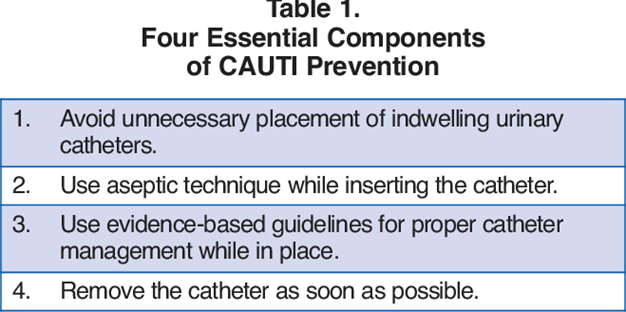
This is because urinary catheters are a common source of catheter associated urinary tract infections (CAUTIs), which can lead to complications such as pyelonephritis, sepsis, and renal failure. Therefore, the nurse should remove the catheter as soon as possible to reduce the risk of infection and promote normal urinary function.
Choice B is wrong because ensuring that the catheter is properly secured to prevent accidental dislodgement is not a priority intervention for a patient with a urinary catheter.
While this is an important nursing action to prevent trauma and bleeding, it does not address the main complication of catheterization, which is infection.
Choice C is wrong because encouraging the patient to drink fluids to prevent dehydration is not a priority intervention for a patient with a urinary catheter.
While this is a good nursing practice to maintain hydration and renal perfusion, it does not affect the risk of infection associated with catheterization.
Choice D is wrong because administering antibiotics to prevent infection is not a priority intervention for a patient with a urinary catheter.
While this may be indicated for some patients who have signs and symptoms of UTI or who are at high risk of infection, it is not a routine measure for all patients with catheters and may contribute to antibiotic resistance.
A client is admitted with dehydration and hypokalemia.
Which of the following signs and symptoms would the nurse expect to find (Select all that apply).
Explanation
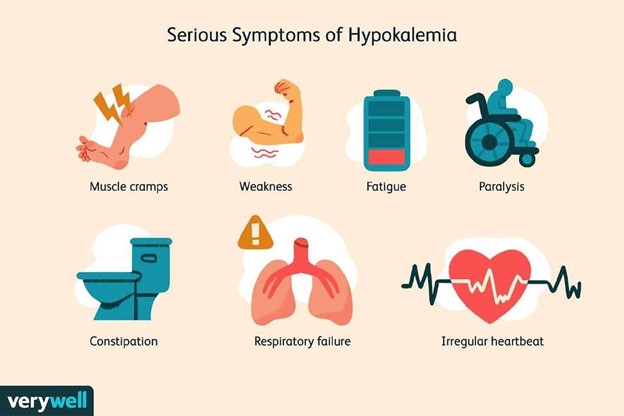
These are all signs and symptoms of hypokalemia, which is a condition where the blood potassium level is too low. This can affect the function of the muscles, nerves, and heart. Therefore, the nurse would expect to find these signs and symptoms in a client with dehydration and hypokalemia.
Choice C is wrong because hyperreflexia is not a sign or symptom of hypokalemia.
Hyperreflexia is a condition where the reflexes are exaggerated or overactive.
This can be caused by conditions such as spinal cord injury, stroke, or electrolyte imbalances such as hypocalcemia or hypomagnesemia.
A client is receiving intravenous fluid therapy with 0.9% sodium chloride solution.
The nurse understands that this type of solution is classified as:
Explanation
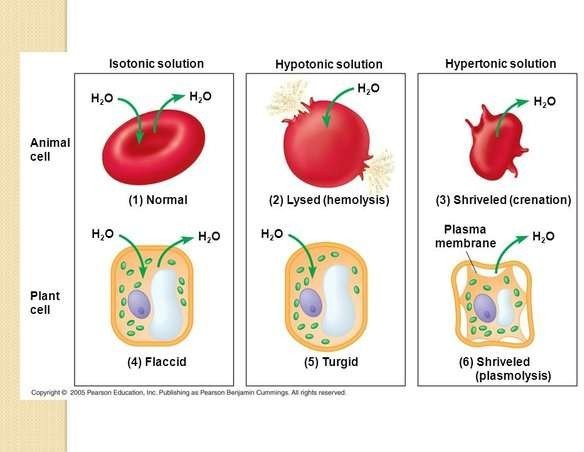
An isotonic solution has the same concentration of solutes as the blood plasma. 0.9% sodium chloride solution is an example of an isotonic solution.
It is used to supply water and salt to the body and to prevent hypotension induced by spinal anaesthesia.
Choice A is wrong because a hypotonic solution has a lower concentration of solutes than the blood plasma.
It can cause water to move into the cells and cause them to swell.
Choice C is wrong because a hypertonic solution has a higher concentration of solutes than the blood plasma.
It can cause water to move out of the cells and cause them to shrink.
Choice D is wrong because a colloid solution contains large molecules that do not pass through the capillary walls.
It is used to increase the blood volume and pressure in cases of shock or severe blood loss.
A client is diagnosed with syndrome of inappropriate antidiuretic hormone (SIADH).
The nurse would monitor the client for which of the following electrolyte imbalances?
Explanation
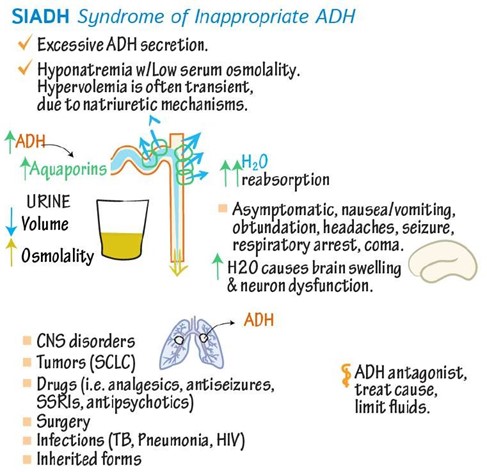
SIADH is a condition in which your body makes too much antidiuretic hormone (ADH), which controls how your body releases and conserves water.
SIADH makes it harder for your kidneys to release water and causes the levels of electrolytes, like sodium, to fall due to water retention.
This leads to hyponatremia, which is when you have low levels of sodium in your blood.
Choice B is wrong because hypernatremia is when you have high levels of sodium in your blood.
This can occur due to dehydration, excessive salt intake, or kidney problems.
Choice C is wrong because hyperkalemia is when you have high levels of potassium in your blood.
This can occur due to kidney failure, acidosis, or certain medications.
Choice D is wrong because hypokalemia is when you have low levels of potassium in your blood.
This can occur due to vomiting, diarrhea, diuretics, or alkalosis.
A client is experiencing metabolic acidosis.
The nurse anticipates that the client’s respiratory rate will be:
Explanation
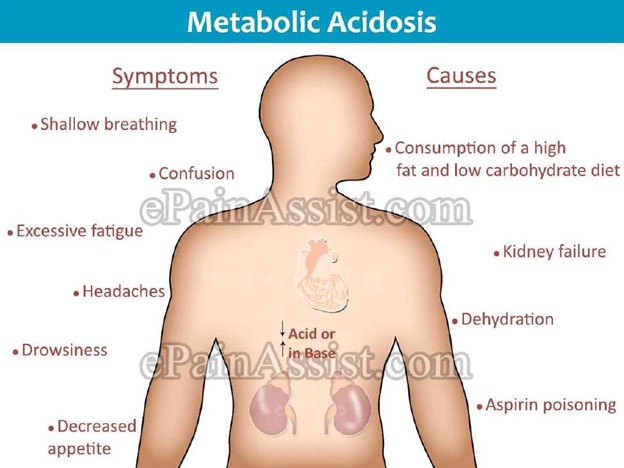
Metabolic acidosis is a condition in which there is excess acid in the body fluids.
It causes rapid breathing, confusion, tiredness, headache, and increased heart rate.
Rapid breathing is a compensatory mechanism that helps to lower the carbon dioxide levels and increase the pH of the blood.
Choice B is wrong because decreased respiratory rate would worsen the acidosis by retaining more carbon dioxide and lowering the pH of the blood.
Choice C is wrong because normal respiratory rate would not be adequate to compensate for the metabolic acidosis and would result in acidemia (low blood pH).
Choice D is wrong because irregular respiratory rate is not a typical response to metabolic acidosis and could indicate other problems such as brain injury or drug overdose.
A client is prescribed oral potassium supplements for hypokalemia. The nurse instructs the client to take the medication:
Explanation

Oral potassium supplements can cause stomach irritation or laxative effect if taken without enough fluid or food.
Taking the medication with food or a full glass of water can help prevent these side effects and improve absorption.
Choice B is wrong because taking the medication on an empty stomach with a sip of water can increase the risk of stomach irritation or laxative effect and reduce absorption.
Choice C is wrong because taking the medication with milk or antacids can interfere with the absorption of potassium and cause hyperkalemia (high blood potassium levels).
Choice D is wrong because taking the medication with grapefruit juice can also interfere with the absorption of potassium and cause hyperkalemia.
Grapefruit juice can also interact with some medications that affect potassium levels, such as angiotensin-converting enzyme (ACE) inhibitors and potassium- sparing diuretics.
A client is experiencing symptoms of fluid overload.
Which of the following interventions would the nurse anticipate as appropriate for this client?
Explanation
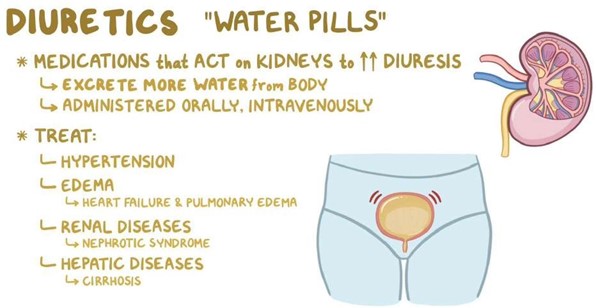
Fluid overload, also called hypervolemia, is a condition in which the body has too much water.
It can cause edema, hypertension, shortness of breath, and cardiovascular problems.
Diuretics are medications that help the body remove excess fluid through urine.
They are commonly used to treat fluid overload caused by heart failure, kidney failure, cirrhosis, and other conditions.
Choice B is wrong because encouraging increased fluid intake would worsen the fluid overload and increase the risk of complications.
Choice C is wrong because providing a high-sodium diet would also worsen the fluid overload and increase the risk of complications.
Sodium is an electrolyte that regulates fluid balance in the body.
Excess sodium intake can cause water retention and increase blood pressure.
Choice D is wrong because elevating the affected extremities is not an appropriate intervention for fluid overload.
Elevating the extremities can help reduce swelling caused by local factors such as injury or inflammation, but it does not address the underlying cause of fluid overload.
A client is admitted with hyponatremia.
Which of the following interventions should the nurse prioritize for this client?
Explanation

This is because hyponatremia is a condition where sodium levels in your blood are lower than normal, usually due to too much water in your body that dilutes the sodium. A hypertonic saline solution is a fluid that has a higher concentration of sodium than blood, and it can help restore the normal sodium balance by drawing water out of the cells.
Choice A is wrong because restricting fluid intake may not be enough to correct severe hyponatremia, and it may worsen the symptoms of dehydration.
Choice C is wrong because encouraging increased fluid intake will further lower the sodium levels and increase the risk of complications such as brain swelling.
Choice D is wrong because administering a loop diuretic will cause more sodium and water loss from the kidneys, which can worsen hyponatremia and dehydration.
Normal ranges for blood sodium levels are between 135 and 145 milliequivalents per liter (mEq/L).
Hyponatremia is defined as a blood sodium level below 135 mEq/L1.
A client is receiving intravenous (IV) potassium replacement therapy.
Which of the following actions should the nurse take to prevent complications?
Explanation
This is because intravenous potassium supplementation is indicated for patients with profound hypokalemia (plasma K+ <2.5 mmol/L) or cardiac arrhythmia. The rate of infusion should not exceed 10 mmol/hour to prevent complications such as hyperkalemia, cardiac arrhythmias, and phlebitis.
Choice A is wrong because monitoring urine output every 8 hours is not sufficient to prevent complications from intravenous potassium replacement therapy.
Urine output should be monitored more frequently (at least every 4 hours) to assess renal function and fluid balance.
Choice B is wrong because administering potassium via a bolus injection is dangerous and can cause fatal cardiac arrhythmias.
Potassium should never be given by intravenous push or intramuscular injection.
Choice D is wrong because encouraging the client to eat potassium-rich foods is not appropriate for patients receiving intravenous potassium replacement therapy.
Oral potassium supplementation is preferred for patients with mild to moderate hypokalemia (plasma K+ 2.5-3.5 mmol/L) who can eat and absorb oral potassium.
Potassium-rich foods include potatoes, legumes, juices, seafood, leafy greens, dairy, tomatoes and bananas.
A client with end-stage renal disease is receiving peritoneal dialysis.
Which of the following actions should the nurse take to prevent infection?
Explanation
Performing hand hygiene before and after handling the dialysis equipment is essential to prevent infection in peritoneal dialysis.

Hand washing and appropriate use of a mask can help avoid peritonitis, which is a serious complication of peritoneal dialysis.
Choice A is wrong because administering antibiotics prophylactically is not recommended for peritoneal dialysis patients, as it can increase the risk of antibiotic resistance and adverse effects.
Choice C is wrong because allowing the client to handle the dialysis equipment independently may increase the risk of contamination and infection.
The client should be supervised and instructed by a nurse on how to use sterile technique when connecting and disconnecting the transfer set.
Choice D is wrong because discontinuing the peritoneal dialysis if the client develops a fever may worsen the client’s condition and lead to fluid overload and electrolyte imbalance.
The client should be evaluated for signs of infection and treated accordingly.
A client with acute kidney injury is receiving hemodialysis.
Which of the following interventions should the nurse prioritize during the dialysis treatment?
Explanation
Monitoring the client’s electrolyte levels before and after the treatment. This is because acute kidney injury (AKI) can cause electrolyte imbalances such as hyperkalemia, hyperphosphatemia, hypocalcemia, and metabolic acidosis. Hemodialysis can help correct these imbalances by removing excess fluid and waste products from the blood. However, hemodialysis can also cause electrolyte shifts and complications such as hypotension, muscle cramps, and arrhythmias. Therefore, it is important to monitor the client’s electrolyte levels before and after the treatment to assess the effectiveness and safety of hemodialysis.
Choice A is wrong because monitoring the client’s blood pressure every 4 hours is not frequent enough during hemodialysis.
Hemodialysis can cause rapid changes in blood pressure due to fluid removal and vascular access.
Therefore, blood pressure should be monitored more often, such as every 15 to 30 minutes during hemodialysis.
Choice B is wrong because administering a loop diuretic before the treatment is not indicated for AKI patients receiving hemodialysis.
Loop diuretics are used to increase urine output and reduce fluid overload in AKI patients who have some residual kidney function.
However, hemodialysis can achieve the same goal by removing excess fluid from the blood.
Moreover, loop diuretics can cause electrolyte depletion and ototoxicity, which can worsen the condition of AKI patients.
Choice C is wrong because assessing the client’s respiratory status every 2 hours is not specific enough for hemodialysis treatment.
Hemodialysis can affect respiratory mechanics by altering fluid balance, acid- base status, and oxygen delivery.
Therefore, respiratory status should be assessed more frequently and comprehensively during hemodialysis, such as by measuring respiratory rate, oxygen saturation, arterial blood gas, and chest auscultation.
Sign Up or Login to view all the 40 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

