Med Surge Exam 1
Total Questions : 27
Showing 25 questions, Sign in for moreThe nurse is providing preoperative education to a client at high risk for breast cancer who is scheduled for an incisional biopsy is being done instead of excisional biopsy.
Which answer by the nurse is appropriate?
Explanation
“An incisional biopsy is performed to confirm a diagnosis and so that special studies can be done that will help determine the best treatment”
The appropriate answer is b because an incisional biopsy is typically performed to obtain a tissue sample from a suspicious mass to confirm a diagnosis and to help determine the best treatment approach. It is not performed primarily to assess potential for recovery or to select a less painful or more accurate test, nor is it limited to a specific age group or health status. The nurse should provide accurate and relevant information to the client to help them understand the purpose and benefits of the procedure, and to alleviate any concerns or fears they may have.
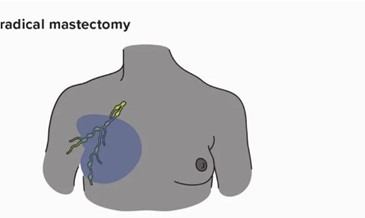
The nurse is caring for a client who has just had a radical mastectomy and axillary node dissection. When
providing teaching to the client, which is the most appropriate?
Explanation
After a radical mastectomy and axillary node dissection, the client may experience swelling and discomfort in the affected arm, known as lymphedema. Lifting heavy objects with the affected arm can worsen the swelling and increase the risk of developing lymphedema. Therefore, it is important for the client to avoid lifting heavy objects with the affected arm and to limit activity that could cause strain or injury to the arm. However, gentle exercise and movement of the arm can help improve circulation and reduce the risk of lymphedema. Using a sling is not typically necessary after this type of surgery, and keeping cuticles clipped neatly is not directly related to post-operative care for a mastectomy and axillary node dissection.
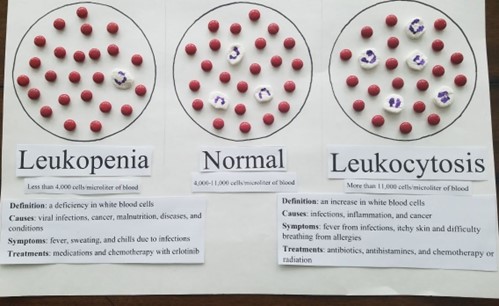
The nurse is caring for a client with ovarian cancer. The client is to receive chemotherapy consisting of
Explanation
The nurse should look out for leukopenia, which is a common adverse effect of chemotherapy drugs like paclitaxel and carboplatin. Leukopenia refers to a decrease in the number of white blood cells in the body, which can increase the risk of infections. It is important for the nurse to monitor the client's white blood cell count regularly during chemotherapy and report any significant changes to the healthcare provider. Metabolic acidosis, hyperphosphatemia, and respiratory alkalosis are not typically associated with paclitaxel and carboplatin chemotherapy.
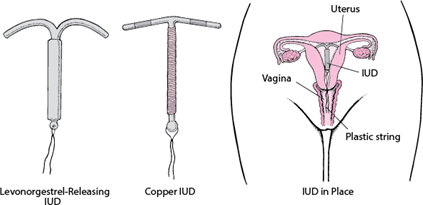
A nurse is preparing a presentation about contraception for a young adult community group. Which is the most effective means of contraception?
Explanation
IUDs are highly effective, with a failure rate of less than 1% per year, and they do not require daily atention or use. The intervaginal contraceptive ring and the transdermal contraceptive patch are also effective methods of contraception, with a failure rate of less than 1% per year when used correctly, but they require consistent use and proper application. The male condom is a highly effective method of contraception when used consistently and correctly, with a failure rate of about 2% per year. However, it is not as effective as the IUD, and its efficacy can be affected by improper use or condom breakage.
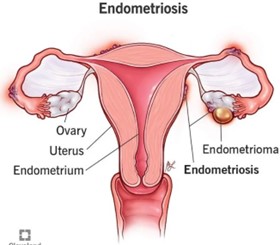
The nurse is teaching a client with endometriosis. What should the nurse include in the teaching?
Explanation
Endometriosis is a condition in which tissue like the lining of the uterus grows outside of the uterus, often on the ovaries, fallopian tubes, or other organs in the pelvic area. This tissue can cause pain, inflammation, and in some cases, fertility problems.
The other options are incorrect. Option A describes endometritis, which is an infection of the lining of the uterus. Option c suggests that endometriosis causes the lining of the uterus to be too thin, which is not accurate. Option d describes adenomyosis, which is a separate condition in which the lining of the uterus grows into the muscular wall of the uterus, causing thickening and pain.
The nurse is planning an educational activity about cancer, which term describes a procedure in which
Explanation
The procedure you are referring to is called a "cone biopsy." It is a medical procedure in which a cone-shaped section of cervical tissue is removed for examination under a microscope. Cone biopsies are typically performed when abnormal cells are detected on a woman's cervix during a routine Pap test or other cervical cancer screening tests. The biopsy can help to determine if the abnormal cells are cancerous or pre-cancerous and can guide further treatment decisions.
The nurse is teaching a client about the treatment of gonorrhea. Which statement by the client indicates
Explanation
This statement shows that the client understands that gonorrhea is a sexually transmited infection that requires treatment for both sexual partners to prevent reinfection. Options a and b are incorrect because douching and over-the-counter medications are not recommended for the treatment of gonorrhea. Option c is also incorrect because while penicillin used to be the recommended treatment for gonorrhea, many strains of the bacteria have developed resistance to it, and other antibiotics are now used instead.
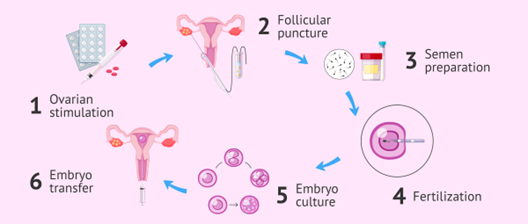
The charge nurse is teaching a new graduate nurse about infertility issues. What statement by the graduate
nurse indicates the need for further teaching?
Explanation
IVF is a complex and involved process that involves hormonal stimulation, egg retrieval, fertilization in a laboratory setting, and then the transfer of the resulting embryo(s) to the uterus. It is not a simple or easy procedure, and it also carries risks such as multiple gestations, ovarian hyperstimulation syndrome, and ectopic pregnancy. The other statements are accurate and indicate a good understanding of infertility issues.
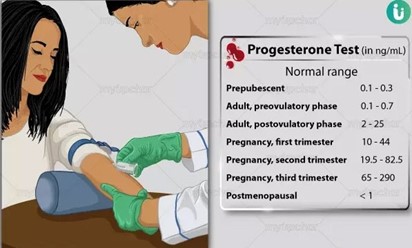
A couple has come to the infertility clinic because they have been unable to get pregnant. Whichdiagnostic test is planned to determine if ovulation is regular and when to time implantation?
Explanation
Progesterone is a hormone produced by the ovaries after ovulation has occurred. By measuring the levels of progesterone in the blood, healthcare providers can determine whether ovulation is occurring regularly and at what point in the menstrual cycle it is happening. This information can be used to time implantation during fertility treatments such as intrauterine insemination (IUI) or in-vitro fertilization (IVF). The other options listed, such as abdominal CT, oocyte viability test, and urine testosterone, are not relevant diagnostic tests for assessing ovulation or timing implantation.
A client calla the clinic and tells the nurse they have thick white, curd-like discharge from the vagina. How should the nurse best interpret this preliminary information?
Explanation
Thick white, curd-like discharge is a common symptom of a yeast infection, which is caused by an overgrowth of candida. However, it is important to note that other conditions, such as bacterial vaginosis or Trichomonas infection, can also cause changes in vaginal discharge.
Therefore, further assessment and evaluation by a healthcare provider is necessary to determine the underlying cause and appropriate treatment plan. A Pap smear is not indicated based on the client's symptoms.
The nurse is performing a comprehensive health history of a client who is in their 50s. The nurse should identify what risk factor that increases risk of complications?
Explanation
The nurse should identify the risk factor of the client giving birth to their first child at age 40 as this is associated with an increased risk of certain pregnancy complications and health problems for both the mother and the baby, such as gestational diabetes, preeclampsia, preterm delivery, and chromosomal abnormalities in the baby. Breastfeeding, experiencing peri-menopausal symptoms, and menarche at age 13 are not significant risk factors in this context. However, it is important to note that each of these factors may be relevant to the client's overall health history and should be documented and taken into consideration as appropriate.
The nurse is caring for a client with cervical cancer who is receiving active brachytherapy. Which statement by the client indicates the client understands the precautions and potential complications associated with active brachytherapy
Explanation
This statement shows that the client understands the potential side effects of the treatment and knows to report any unusual symptoms to their healthcare provider. This is important because brachytherapy can cause vaginal bleeding, fever, or abdominal pain, which may be signs of infection or other complications.
Option a is partially correct, as it is important for clients undergoing active brachytherapy to restrict activity and avoid vigorous movements to prevent the dislodgement of radiation sources. However, this statement alone does not indicate that the client understands the potential complications or knows when to report them to the healthcare provider.
Option b is not directly related to the client's treatment or potential complications and does not indicate an understanding of the precautions and potential complications associated with active brachytherapy.
Option d is not necessarily required, as the client may not need to be in a private room during active brachytherapy. This option does not directly relate to the precautions or potential complications of the treatment.
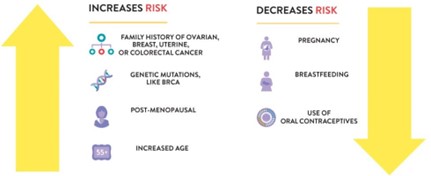
The nurse is leading an educational activity about ovarian cancer. Which client has the highest risk of ovarian cancer?
Explanation
Ovarian cancer risk is increased in women who have not been pregnant, have a family history of ovarian cancer, have a personal history of breast or colon cancer, and have inherited gene mutations such as BRCA1 and BRCA2.
Hormonal contraceptives, having children, and the age at which a woman had her first child have been associated with a reduced risk of ovarian cancer. However, these factors do not completely eliminate the risk. It is still possible for women taking hormonal contraceptives, women who have had children, and women who had their first child at an early age to develop ovarian cancer
.
On discharge, a client who underwent left modified radical mastectomy expresses relief that -the cancer- has been treed. When discharged, which is the best recommendation?
Explanation
Breast self-examination is an essential part of breast cancer detection and should be performed regularly by all women, regardless of their medical history. While the client may have undergone a left modified radical mastectomy, this does not eliminate the possibility of developing breast cancer in the right breast or other parts of the body. Therefore, it is essential to continue performing breast self-examination regularly to detect any changes that may occur in the right breast.
Option b, "Is lucky that the cancer was caught in time" and option c, "should schedule a follow- up appointment in 6 months" may also be appropriate responses depending on the client's specific situation but option a is the most universally applicable response.
Option d, "I have irregular menses" is unrelated to the topic and does not address the client's
concern or needs.
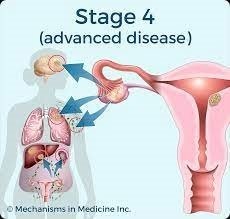
The nurse is teaching a client with stage IV ovarian cancer. Which statement by the client indicates the need for further teaching?
Explanation
Stage IV ovarian cancer is an advanced stage, and it is unlikely that the cancer can be cured. While treatment may help manage the symptoms and slow down the progression of the disease, it is essential to have realistic expectations and understand the limitations of treatment options.
Option b, "My type of cancer has spread to other tissues" is a correct understanding of the situation and indicates the client has understood their diagnosis.
Option c, "I have chemotherapy after my hysterectomy" is an accurate statement about treatment and indicates the client has understood the plan of care.
Option d, "I may need to talk with my family about hospice" is also an appropriate statement, as clients with stage IV ovarian cancer may need to consider end-of-life care and hospice services
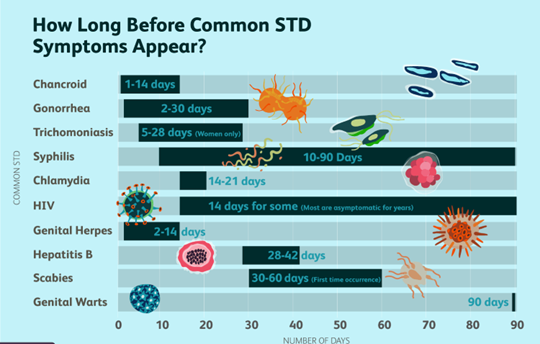
The nurse is providing community teaching on sexually transmitted infections, which key point most important the nurse to emphasize?
Explanation
All the options are important for the nurse to include in their community teaching, but the most important key point for the nurse to emphasize would be option C: many people are asymptomatic and show no symptoms of the disease. This is important because individuals who have sexually transmitted infections but are asymptomatic may unknowingly spread the infection to others, including their sexual partners. It is essential for individuals to understand that they may have an infection even if they feel perfectly healthy, and to get tested regularly to prevent the spread of sexually transmitted infections.
A client with ovarian cancer is admitted to the hospital for surgery and the nurse is completing the clients health history. Which clinical manifestation should the nurse look out for?
Explanation
Lower abdominal pelvic pain is a common clinical manifestation of ovarian cancer. Ovarian cancer may not cause any noticeable symptoms in its early stages, but as the cancer grows and spreads, symptoms may develop. Pelvic pain or pressure is a common symptom, along with bloating, difficulty eating or feeling full quickly, and urinary urgency or frequency. Other symptoms may include fatigue, indigestion, back pain, constipation, and menstrual irregularities. A fish-like odor (a symptom of bacterial vaginosis) increased abdominal girth,
fever and chills, and leukocytosis are not typically associated with ovarian cancer. However, leukocytosis (an elevated white blood cell count) may be present in response to inflammation or infection. It is important for the nurse to assess the client's symptoms thoroughly and report any concerning findings to the healthcare provider.
The nurse is caring for a client who was recently diagnosed with breast cancer. What is the most important information needed to determine the treatment of
Explanation
The breast cancer stage and grade are critical factors in determining the appropriate treatment plan. The stage describes the extent of the cancer, including how large it is and whether it has spread to nearby lymph nodes or other parts of the body. The cancer grade provides information about how abnormal the cancer cells look under a microscope, which can help predict how fast the cancer is likely to grow and spread.
While CBC results (option a) and vital signs (option b) may provide some information about the client's overall health, they are not the most important factors in determining breast cancer treatment. Similarly, while the family's wishes for treatment (option d) are important to consider, they should not be the sole determining factor in deciding the best course of action for the client's cancer treatment.

A client has been diagnosed with endometriosis. When planning this clients care, the nurse should prioritize what nursing diagnosis?
Explanation
Endometriosis is a condition in which tissue like the lining of the uterus grows outside of the uterus, causing pain and discomfort. Acute pain is a common symptom of endometriosis and can be severe enough to interfere with daily activities and quality of life. Therefore, pain management should be a priority in the care of clients with endometriosis.
While anxiety related to risk of transmission (option a) and excess fluid volume related to abdominal distention (option d) may also be concerns for some clients with endometriosis, they are generally not the most urgent priorities. Ineffective tissue perfusion related to hemorrhage (option c) may be a concern in rare cases of severe endometriosis, but it is not a common or typical complication.
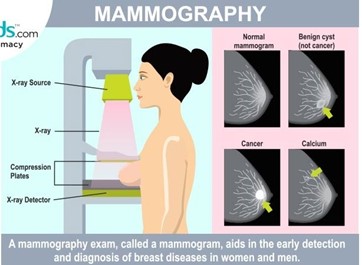
The nurse is leading an education activity about annual mammograms. At what age should the nurse recommend annual screening?
Explanation
The current recommendation from the American Cancer Society is that women with an average risk of breast cancer should undergo annual mammography screening starting at age 45, although women may choose to start screening as early as age 40. Therefore, the nurse should recommend annual mammography screening starting at age 45. However, it is important to note that women with certain risk factors for breast cancer, such as a family history of the disease, may need to begin screening earlier or undergo additional screening tests. The nurse can provide more individualized recommendations based on each woman's specific risk factors.
A nurse is preparing a presentation about contraception for a young adult group. Which of the following is the most recommended?
Explanation
The most recommended contraceptive method for young adults depends on various factors such as their medical history, lifestyle, preferences, and sexual behavior. However, in general, healthcare providers recommend starting with the least invasive and reversible options before considering more permanent methods.
Therefore, the most recommended contraceptive method for young adults is usually barrier methods, such as condoms or diaphragms, or hormonal contraception, such as birth control
pills, patches, or rings. These methods are highly effective when used correctly and consistently
and do not affect long-term fertility.
Abstinence is also an effective way to prevent pregnancy and sexually transmitted infections, but it may not be a realistic option for everyone. Sterilization, on the other hand, is a permanent method that should only be considered by individuals who are sure that they do not want to have children in the future.
It is important for the nurse to provide comprehensive information on all contraceptive options, their effectiveness, benefits, and risks, to help the young adult group make informed decisions about their reproductive health.
The nurse is teaching methods of contraception with a young client. The client decides on the contraceptive sponge as her method of choice Which information should the Nurse include in the teaching?
Explanation
The contraceptive sponge is a barrier method of contraception that is inserted into the vagina before sexual intercourse. It contains spermicide and blocks the sperm from reaching the egg. The sponge must be left in place for at least 6 hours after intercourse before it is removed. Don't leave it in for more than a total of 30 hours.
a. "You can use this at any time, even when you are menstruating" is incorrect information because the contraceptive sponge should not be used during menstruation.
c. "You need to have the sponge fited before using it" is incorrect information because the contraceptive sponge is a one-size-fits-all device and does not require fitting.
d. "Clean the with mild soap and water after using it" is also incorrect information because the contraceptive sponge is a disposable device and should be discarded after use. It should not be reused or washed.

The nurse is planning health education for a client who has experienced a vaginal infection. What
guidelines should the nurse Include in the teaching?
Explanation
- Avoid commercial feminine hygiene products. such as sprays.
The nurse should provide the following guidelines for a client who has experienced a vaginal
infection:
c. Avoid commercial feminine hygiene products, such as sprays, which can disrupt the natural pH balance of the vagina and increase the risk of infection.
d. Do not restrict daily washing but avoid using harsh soaps and perfumed products in the genital area, as these can also disrupt the natural pH balance.
- Wear loose-fitting cotton underwear instead of tight-fitting synthetic underwear, as cotton allows for better air circulation and helps to keep the genital area dry.
- Do not douche, as this can also disrupt the natural pH balance of the vagina and increase the
risk of infection.
In addition to these guidelines, the nurse should also encourage the client to maintain good overall hygiene, including showering or bathing regularly and wiping from front to back after using the toilet. The nurse should also advise the client to seek medical attention if any symptoms of a vaginal infection reoccur or worsen.
- Avoid commercial feminine hygiene products. such as sprays.
The nurse should provide the following guidelines for a client who has experienced a vaginal
infection:
c. Avoid commercial feminine hygiene products, such as sprays, which can disrupt the natural pH balance of the vagina and increase the risk of infection.
d. Do not restrict daily washing but avoid using harsh soaps and perfumed products in the genital area, as these can also disrupt the natural pH balance.
- Wear loose-fitting cotton underwear instead of tight-fitting synthetic underwear, as cotton allows for better air circulation and helps to keep the genital area dry.
- Do not douche, as this can also disrupt the natural pH balance of the vagina and increase the
risk of infection.
In addition to these guidelines, the nurse should also encourage the client to maintain good overall hygiene, including showering or bathing regularly and wiping from front to back after using the toilet. The nurse should also advise the client to seek medical attention if any symptoms of a vaginal infection reoccur or worsen.
An infertile couple has used at-home ovulation testing using basal body temperature without conceiving.
The nurse understands that what will be used first to treat this infertile couple?
Explanation
If a couple has used at-home ovulation testing with basal body temperature and has not conceived, the first treatment option may depend on the underlying cause of infertility. However, the most common first-line treatment for infertility is selective estrogen receptor modulator clomiphene. This medication stimulates ovulation and can increase the chances of conception.
Surgery to reduce endometriosis may be considered if endometriosis is the underlying cause of infertility. However, surgery is not always successful and may not be the first option.
Intrauterine insemination (IUI) with sperm from the husband is another option that may be considered if the male partner has mild to moderate sperm abnormalities or if there is unexplained infertility. IUI involves placing washed sperm directly into the uterus during ovulation.
Assisted reproductive technologies (ART), such as in vitro fertilization (IVF), may be considered if other treatments have been unsuccessful or if there are more severe fertility issues. ART involves combining eggs and sperm outside of the body and transferring the resulting embryo(s) into the uterus.
The choice of treatment will depend on the underlying cause of infertility, the age of the couple, and other factors that may impact fertility. It is important for the couple to consult with a healthcare provider who specializes in fertility treatments to determine the best course of action.
You are the nurse at a community high school. A student calls the office and says she thinks she has a “yeast infection”. What signs and symptoms should the nurse expect?
Explanation
a. Intense itching and dysuria
d. Thick white cottage cheese-like discharge
Common symptoms of a yeast infection may include itching, burning, and redness in the vaginal area. Some women may also experience pain or discomfort during sexual intercourse or while urinating. It is important for the nurse to conduct a thorough assessment and obtain a detailed history from the student to determine the appropriate course of action, such as recommending over-the-counter treatments or referring the student to a healthcare provider for further evaluation and treatment.
Sign Up or Login to view all the 27 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

