Medical-Surgical Exam 3
Total Questions : 45
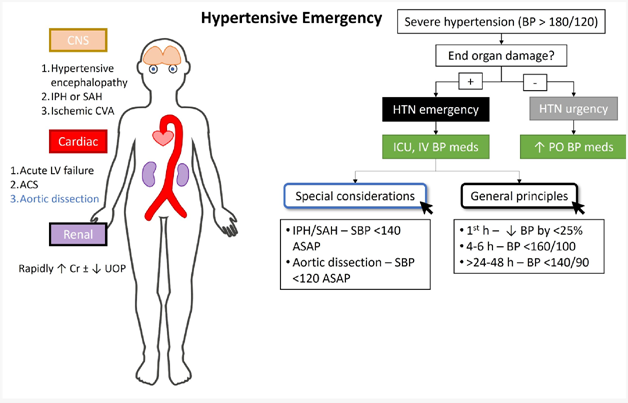
Showing 25 questions, Sign in for moreThe nurse is assessing a client with a hypertensive emergency. Which finding is most important to report to the health care provider?
Explanation
The client reports a headache with pain at level 5 of 10.: While a headache can be a symptom of high blood pressure, a pain level of 5 out of 10 alone does not indicate an immediate life-threatening condition. It is important to assess and manage the client's pain, but it may not be the most critical finding to report in this situation.
The client has epistaxis after blowing his nose several times. : Epistaxis, or a nosebleed, can occur due to high blood pressure, but it is not the most urgent or critical symptom in a hypertensive emergency. While it is essential to address the nosebleed and monitor blood pressure, other symptoms may indicate more severe consequences of uncontrolled high blood pressure.
The client has a urine output of 120 mL over 4 hours.: While decreased urine output can be a concerning sign, it is not the most significant finding to report in a hypertensive emergency. In this scenario, the focus is on acute complications related to high blood pressure, such as organ damage or impending stroke, which require immediate attention.
In summary, the finding that is most important to report to the healthcare provider in a client with a hypertensive emergency is the presence of new-onset blurry vision and facial asymmetry. These symptoms suggest potential neurological involvement and the need for urgent medical intervention to prevent serious complications like stroke.
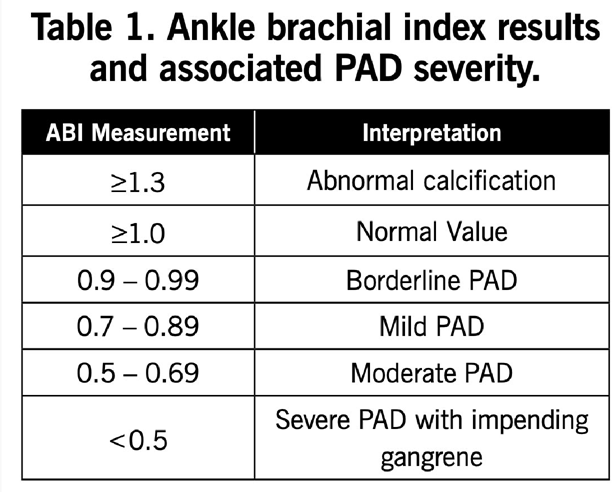
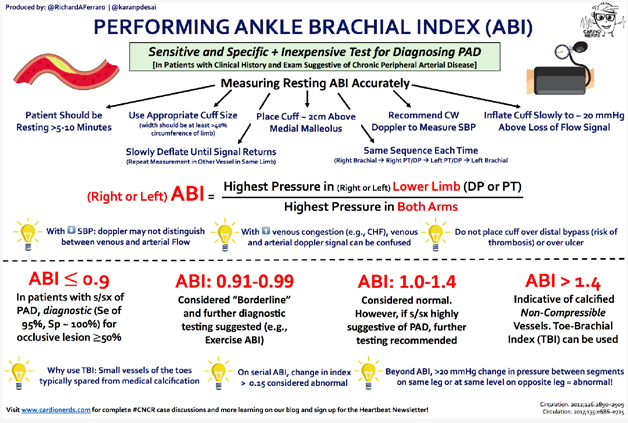
The nurse is assessing a client with a presumptive diagnosis of peripheral arterial disease. The nurse obtains an Ankle-Brachial index of 0.89. Which intervention should the nurse take next?
Explanation
An ABI of 0.89 indicates a reduced blood flow to the lower extremities, which is suggestive of peripheral arterial disease (PAD). In PAD, there is narrowing or blockage of the arteries that supply blood to the legs and feet. Medications like clopidogrel and simvastatin are commonly prescribed for individuals with PAD to manage the condition and reduce the risk of complications.
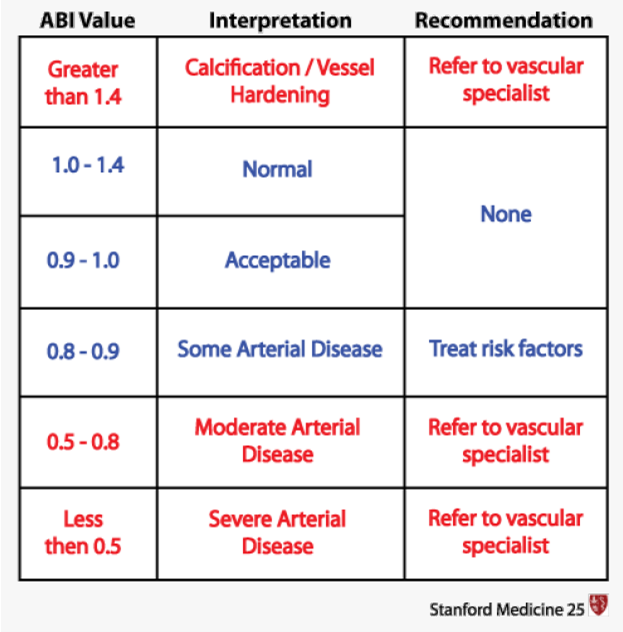
Here's an explanation of why the other options are not the most appropriate interventions:
Document the information as a normal finding: An ABI of 0.89 is not considered a normal finding. An ABI value below 0.9 is generally indicative of PAD or reduced blood flow to the lower extremities.
Prepare the client for an arterial bypass: An ABI value of 0.89 alone does not warrant immediate preparation for an arterial bypass. Arterial bypass surgery is typically considered for severe cases of PAD with significant symptoms that significantly impact the client's quality of life and other conservative treatments have not been successful.
Educate the client about the use of compression stockings: While compression stockings may be a part of the overall management of PAD, the ABI result alone does not indicate an immediate need for education about compression stockings. Other interventions, such as medication management, lifestyle modifications, and possibly revascularization procedures, may be more appropriate based on the severity of the PAD.
A nurse is assessing a client with a history of high blood pressure. The client's blood pressure is 210/106 mm Hg during the assessment. What follow-up question should the nurse ask?
Explanation
Choice D: This question is crucial as it addresses the client's adherence to their prescribed medication regimen for managing high blood pressure. Consistent medication use is essential for controlling blood pressure and reducing the risk of complications associated with hypertension. The elevated blood pressure reading suggests that the current medication regimen may not be effectively controlling the client's blood pressure. By assessing medication adherence, the nurse can determine if non-adherence is contributing to the high blood pressure reading or if adjustments to the medication regimen are required.
"Have you recently taken any antihistamines?": Asking about recent antihistamine use is not directly relevant to the client's high blood pressure reading of 210/106 mm Hg. Antihistamines are medications primarily used to relieve allergy symptoms and do not typically have a significant impact on blood pressure levels.
"Have there been recent stressful events in your life?": While stress can contribute to temporary increases in blood pressure, asking about recent stressful events is not the most critical follow-up question in this situation. The client's blood pressure reading of 210/106 mm Hg indicates a severe elevation that requires immediate attention and management beyond stress reduction alone.
"Did you take any acetaminophen today?": Acetaminophen, also known as paracetamol, is a pain reliever and fever reducer. It does not typically have a significant effect on blood pressure. Therefore, asking about acetaminophen use is not the most relevant follow-up question for the client's high blood pressure reading.
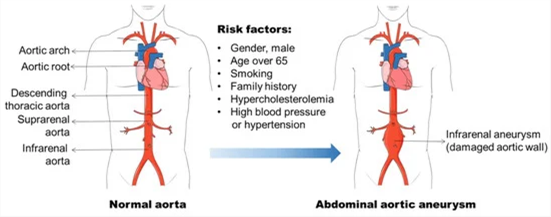
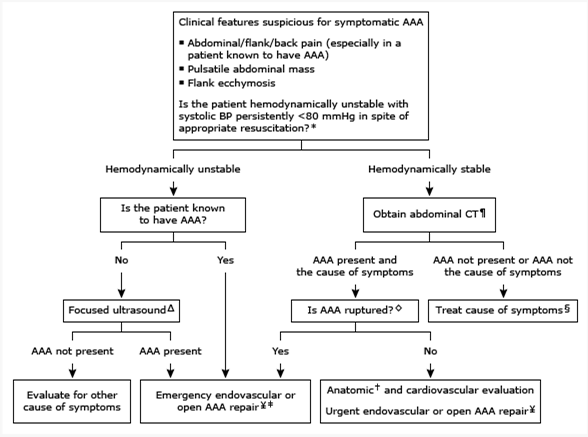
The nurse is caring for a client immediately after repair of an abdominal aortic aneurysm. On assessment, the client has absent popliteal, posterior tibial, and dorsalis pedis pulses. The leg cool and mottled. Which action should the nurse take first?
Explanation
The nurse should prioritize notifying the surgeon and anesthesiologist as the first action. The absent pulses, coolness, and mottled appearance of the leg indicate potential compromised blood flow to the lower extremity, which could be a sign of vascular compromise or acute limb ischemia. These findings are concerning after the repair of an abdominal aortic aneurysm and require immediate medical attention.
Wrap both legs in a warming blanket: While it is important to maintain the client's body temperature, this action alone may not address the underlying issue of compromised blood flow and potential limb ischemia. Notifying the surgeon and anesthesiologist is the priority to address the immediate concern.
Compare findings to the preoperative assessment of the pulses: While comparing findings to the preoperative assessment is important for evaluating the client's condition, it should not delay immediate action. The priority in this situation is to promptly notify the surgeon and anesthesiologist to address the potential vascular compromise.
Document the findings and recheck in 15 minutes: Documenting the findings is an important step in the nursing process, but it should not take precedence over immediate intervention. The concerning signs of absent pulses, coolness, and mottled appearance require urgent attention, and delaying notification could lead to further complications.
A nurse is preparing a client for scheduled transesophageal echocardiography. Which action should the nurse perform?
Explanation
Transesophageal echocardiography is a diagnostic procedure that involves inserting a probe into the esophagus to obtain detailed images of the heart. In some cases, an access line may be initiated in the femoral artery to monitor blood pressure during the procedure and administer medications if needed. Informing the client about this aspect of the procedure helps ensure that they are aware of what to expect and can provide informed consent.
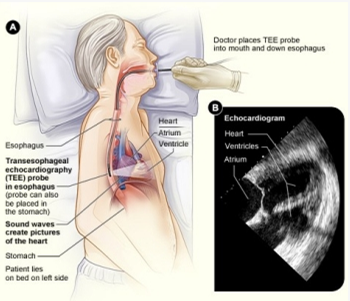
Let's go through the other options and explain why they are not the most appropriate actions:
Instruct the client to drink 1 L of water before the test: This action is not necessary for transesophageal echocardiography. Drinking water before the test is typically done for certain abdominal or pelvic ultrasound examinations to provide better visualization. However, for TEE, the probe is inserted into the esophagus, and drinking water is not required.
Administer intravenous (IV) benzodiazepines and opioids: The administration of intravenous benzodiazepines and opioids is not a routine part of preparing a client for TEE. The need for sedation or analgesia during the procedure would be determined based on the individual client's condition and level of discomfort.
Inform the client that the client will remain on bed rest following the procedure: While some post-procedure instructions may be given to the client, such as avoiding eating or drinking until the effects of sedation wear off, informing the client that they will remain on bed rest following the procedure is not a specific requirement for TEE. Post-procedure instructions can vary depending on the individual client's condition and the healthcare provider's recommendations.
The nurse on the intermediate care unit received change-of-shift report on four clients with hypertension. Which patient should the nurse assess first?
Explanation
The nurse should assess the client with a blood pressure of 190/92 mm Hg who reports chest pain first. Chest pain can be a symptom of myocardial ischemia or a heart attack, which requires immediate attention. The combination of high blood pressure and chest pain is concerning and may indicate acute coronary syndrome. Prompt assessment and intervention are crucial to evaluate the cause of the chest pain and initiate appropriate treatment.
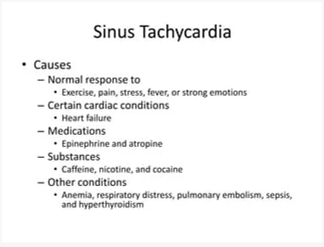
A client with a blood pressure of 190/104 mm Hg who has sinus tachycardia: While sinus tachycardia may indicate increased heart rate, it does not necessarily require immediate assessment unless other concerning symptoms are present. However, the nurse should address the elevated blood pressure in a timely manner.
Intermittent claudication refers to leg pain or discomfort during physical activity due to reduced blood flow. While it is important to assess and manage this symptom, it is not typically considered an urgent condition requiring immediate assessment compared to chest pain.
The client scheduled for a stress test may have elevated blood pressure, but if they are stable and not currently experiencing symptoms, they may not require immediate assessment compared to a client with chest pain.
The nurse is assessing a client with a heart rate of 124 bpm. What clinical finding(s) should the nurse assess as causes of tachycardia? Select all that apply.
Explanation
Pain level of 10 out of 10: Severe pain can stimulate the sympathetic nervous system and result in an increased heart rate.
Temperature 101.9°F: Fever can lead to an elevated heart rate as the body's response to infection or inflammation.
Hemoglobin: 7 g/dL: Low hemoglobin levels, known as anemia, can cause the heart to pump faster in an attempt to compensate for the decreased oxygen-carrying capacity of the blood.
Cocaine abuse: Cocaine is a stimulant drug that can significantly increase heart rate and cause tachycardia.
The following clinical finding would not typically be associated with tachycardia:
Blood glucose 90 mg/dL: While low or high blood glucose levels can cause symptoms, they are not directly associated with tachycardia unless they lead to significant physiological stress or hormonal imbalances.
A nurse accompanies a client to an exercise stress test. The client can achieve the target heart rate, but the electrocardiogram indicates ST-segment elevation. Which procedure will the nurse prepare the patient for?
Explanation
ST-segment elevation during exercise stress testing is a concerning finding that may indicate reduced blood flow to the heart muscle. It can be a sign of myocardial ischemia or coronary artery disease. Cardiac catheterization is a diagnostic procedure that allows direct visualization of the coronary arteries and helps identify any blockages or narrowing that may be causing the ST-segment elevation.
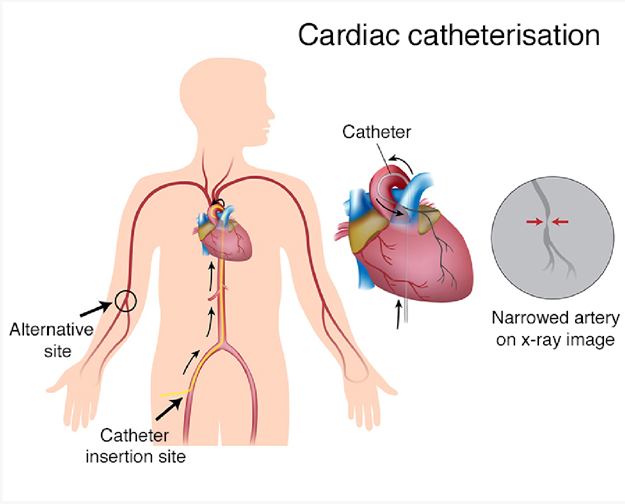
Here's an explanation of why the other options are not the most appropriate procedures:
Transesophageal echocardiogram: Transesophageal echocardiogram (TEE) is a diagnostic test that involves inserting a probe into the esophagus to obtain detailed images of the heart. It is not typically used to evaluate ST-segment elevation, which primarily indicates coronary artery issues rather than structural abnormalities.
Telemetry monitoring: Telemetry monitoring involves continuous monitoring of a patient's heart rhythm and can be used for various cardiac conditions. While telemetry monitoring may be necessary for ongoing cardiac assessment, it is not a specific procedure to address the ST-segment elevation found during the exercise stress test.
Pharmacologic stress test: A pharmacologic stress test is an alternative to an exercise stress test for patients who cannot exercise. It involves administering medications that stimulate the heart to mimic the effects of exercise. While a pharmacologic stress testcan also reveal ST-segment changes, the presence of ST-segment elevation usually requires further evaluation with a more invasive procedure like cardiac catheterization.
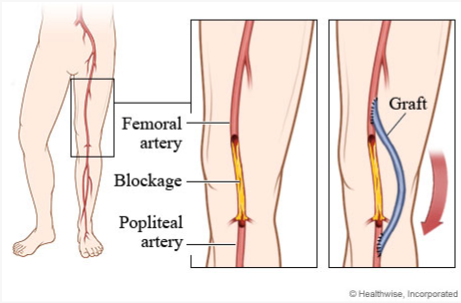
A client who has undergone a femoral to popliteal bypass graft surgery returns to the surgical unit. Which assessments should the nurse perform during the first postoperative day?
Explanation
Assess pulse of the affected extremity every 15 minutes at first: Frequent assessment of the pulse in the affected extremity is important to monitor for any changes in blood flow. This allows the nurse to identify any potential complications such as graft occlusion or compromised circulation promptly.
Palpate the affected leg for pain during every assessment: Assessing for pain in the affected leg is crucial to identify any signs of ischemia or inadequate perfusion. Increased pain could indicate reduced blood flow or other complications that require immediate attention.
Assess the client for signs and symptoms of compartment syndrome every 2 hours: Compartment syndrome can occur after vascular surgeries, and early recognition is vital. The nurse should assess for signs and symptoms such as pain, numbness, tingling, increased swelling, and tense compartments. Regular assessment every 2 hours can help detect compartment syndrome promptly and prevent further complications.
Perform Doppler evaluation once daily: Doppler evaluation may be ordered by the healthcare provider to assess blood flow and graft patency. However, the frequency of Doppler evaluation may vary depending on the client's condition and the healthcare provider's orders. Once daily assessment is not sufficient if there are concerns regarding blood flow or graft viability.
The nurse is caring for a client in a hypertensive emergency. Which action will be included in the plan of care during hypertensive emergency who is receiving nifedipine?
Explanation
The action that will be included in the plan of care for a client in a hypertensive emergency receiving nifedipine is to use an automated noninvasive blood pressure machine to obtain frequent measurements.
In a hypertensive emergency, the client's blood pressure is severely elevated, requiring immediate treatment and close monitoring. Nifedipine is a calcium channel blocker commonly used to lower blood pressure in such situations. Continuous blood pressure monitoring is crucial to assess the effectiveness of the medication and ensure that the blood pressure is brought under control safely.
Organize nursing activities so that the patient has 8 hours of undisturbed sleep at night: While providing a conducive environment for sleep is important for overall patient well-being, in a hypertensive emergency, the priority is to manage and monitor the blood pressure. Sleep hygiene may not be the immediate concern in this situation.
Keep the hypertensive emergency NPO to prevent aspiration caused by nausea and possible vomiting: NPO (nothing by mouth) orders are typically implemented when there is a risk of aspiration or pending a procedure requiring anesthesia. In a hypertensive emergency, the focus is on managing blood pressure and ensuring appropriate hydration and nutrition as needed. NPO status may not be necessary unless specifically indicated for the individual patient.
Assist the patient up in the chair for meals to avoid complications associated with immobility: While mobilization and preventing complications associated with immobility are important aspects of care, in a hypertensive emergency, the primary focus is on managing blood pressure and stabilizing the client's condition. Mobilization may be appropriate once the blood pressure is under control and the client's condition permits.
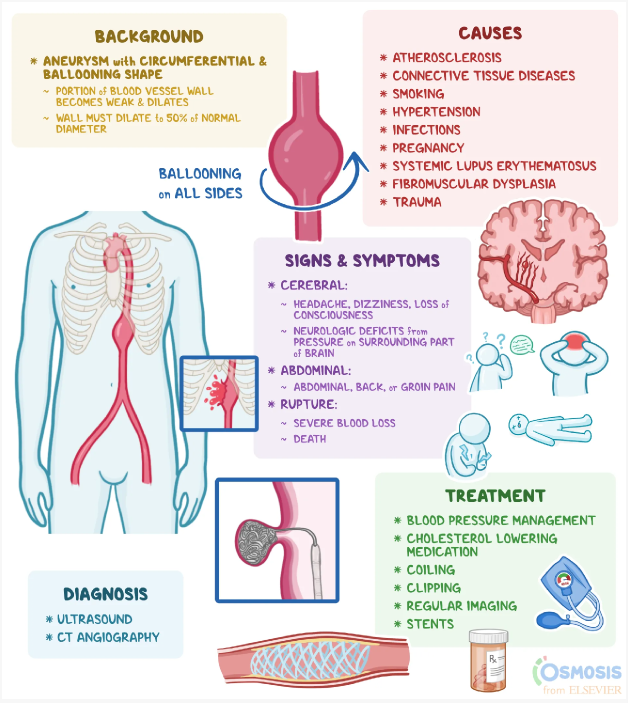
The client is diagnosed with an abdominal aortic aneurysm. Which statement would the nurse expect the client to make during the admission assessment?
Explanation
Abdominal aortic aneurysms (AAA) often do not present with specific symptoms in the early stages. It is not uncommon for individuals with AAA to be asymptomatic or have vague symptoms. Therefore, the absence of abdominal pain or any problems related to the abdomen is a common finding during the assessment of a client with an abdominal aortic aneurysm.
Let's briefly review the other statements:
"I have stomach pain every time I eat a big, heavy meal": This statement is more suggestive of gastrointestinal issues such as indigestion or acid reflux rather than specifically related to an abdominal aortic aneurysm.
"I have periodic episodes of constipation and then diarrhea": This statement may indicate gastrointestinal issues, but it is not a typical symptom associated with an abdominal aortic aneurysm. AAA is primarily related to the aorta, the main blood vessel in the abdomen, and its symptoms are not directly linked to bowel function.
"I belch a lot, especially when I lay down after eating": This statement suggests gastrointestinal symptoms such as acid reflux or gastroesophageal reflux disease (GERD). While these symptoms may be unrelated to the abdominal aortic aneurysm itself, they can coexist with other conditions.
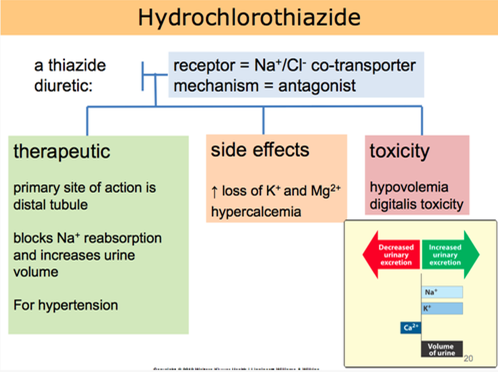
A nurse is teaching a hypertensive client who is taking hydrochlorothiazide. What client statement indicates understanding about hydrochlorothiazide?
Explanation
Hydrochlorothiazide is a diuretic medication commonly prescribed for hypertension. It works by increasing urine output, which helps to reduce fluid volume and lower blood pressure. Taking the medication in the morning is beneficial because the increased urine production during the day can help prevent nighttime disruptions due to frequent urination.
Let's go through the other statements and explain why they are not accurate:
"I will not take this medicine when my blood pressure is okay":
This statement indicates a misunderstanding about the purpose of hydrochlorothiazide. It is important to take prescribed medications consistently, even when blood pressure readings are within the normal range, as they are intended to help maintain blood pressure control.
"I will check blood pressure in both arms and legs before taking the drug":
Checking blood pressure in both arms and legs is not directly related to hydrochlorothiazide use. Blood pressure should be monitored regularly, but it is not necessary to perform these measurements specifically before taking the medication.
"I will decrease potassium foods such as bananas in my diet":
Hydrochlorothiazide can cause potassium loss as a side effect. However, reducing potassium-rich foods without healthcare provider guidance may not be appropriate. It is important for the client to discuss dietary adjustments and potassium supplementation with their healthcare provider if needed.
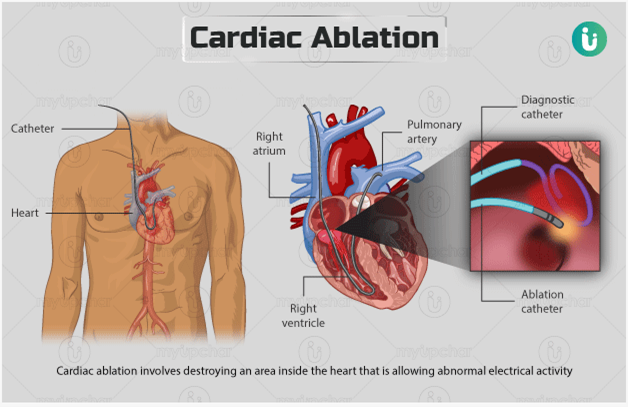
The nurse is teaching a client with atrial flutter who is scheduled for a catheter ablation? What should the nurse include in the teaching plan?
Explanation
The procedure uses electrical energy to destroy areas of the conduction system: Catheter ablation is a minimally invasive procedure performed to treat abnormal heart rhythms, such as atrial flutter. During the procedure, a catheter is inserted into the heartand used to deliver electrical energy to specific areas of the heart tissue. This energy is used to destroy or ablate the abnormal conduction pathways that are causing the atrial flutter.
Let's go through the other options and explain why they are not accurate:
The procedure stimulates the growth of new pathways between the atria: Catheter ablation does not stimulate the growth of new pathways. Instead, it aims to eliminate or modify existing abnormal pathways in the heart to restore normal electrical conduction.
The procedure uses cold therapy to stop the formation of the flutter waves: Catheter ablation does not use cold therapy. It primarily utilizes radiofrequency energy or other sources of heat to ablate the targeted areas of the heart tissue.
The procedure prevents or minimizes the patient's risk for sudden cardiac death: While catheter ablation can be an effective treatment for certain arrhythmias, including atrial flutter, it is not primarily performed to prevent or minimize the risk of sudden cardiac death. Its main purpose is to restore normal heart rhythm and alleviate symptoms associated with the arrhythmia.
While assessing a client, the nurse notes that the client's ankle-brachial index (ABI) of the right leg is 0.40. How should the nurse best follow up this assessment finding?
Explanation
The nurse should best follow up the assessment finding of an ankle-brachial index (ABI) of 0.40 in the right leg by implementing interventions relevant to arterial narrowing.
An ankle-brachial index is a non-invasive test used to assess peripheral arterial disease (PAD). An ABI value below 0.90 indicates significant arterial narrowing and impaired blood flow to the lower extremities. An ABI of 0.40 suggests severe arterial narrowing, which puts the client at risk for reduced perfusion and potential complications such as tissue ischemia, ulceration, and gangrene.
Implementing interventions relevant to arterial narrowing is crucial in this case. These interventions may include:
- Collaborating with the healthcare provider to develop a treatment plan: This may involve prescribing medications to improve blood flow, such as antiplatelet agents or vasodilators.
- Encouraging lifestyle modifications: This can include smoking cessation, regular exercise, and maintaining a healthy diet low in saturated fats and high in fruits and vegetables.
- Promoting optimal cardiovascular health: This can involve managing other risk factors for arterial narrowing, such as hypertension, diabetes, and high cholesterol levels.
- Educating the client about the signs and symptoms of PAD: This includes teaching them to monitor for changes in skin color, temperature, and sensation in the affected limb, as well as the importance of seeking prompt medical attention if these changes occur.
Let's review the other options:
Assessing the client's use of over-the-counter dietary supplements: While it is important to assess for potential interactions between medications and dietary supplements, this would not be the immediate follow-up action for a severely reduced ABI.
Encouraging the client to increase intake of foods high in vitamin K: While maintaining a balanced diet is important for overall health, increasing vitamin K intake is not specifically indicated for addressing arterial narrowing or improving the ABI.
Adjusting the client's activity level to accommodate decreased coronary output:
Coronary output refers to blood flow to the heart muscle. Arterial narrowing in the leg does not directly affect coronary output. However, it is important to encourage appropriate physical activity for the client based on their overall cardiovascular health and exercise tolerance.
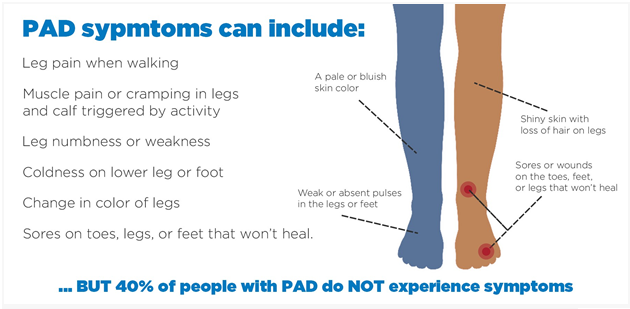
The nurse is teaching a client with peripheral arterial disease. Which information should the nurse include in the teaching plan?
Explanation
Wear fitted closed toe shoes daily: It is important for clients with peripheral arterial disease to wear properly fitted closed toe shoes. This helps protect the feet from injury and provides support. Closed toe shoes also help maintain warmth and prevent heat loss, which is especially important for individuals with impaired circulation.
Let's review the other options and explain why they may not be appropriate:
Soak feet in warm water for an hour each day: Soaking the feet in warm water for a prolonged period can actually worsen symptoms in individuals with peripheral arterial disease. It can cause further dilation of blood vessels, leading to increased blood pooling and potential tissue damage. Therefore, soaking the feet for extended periods of time is not recommended.
Set heating pads on a low temperature: Using heating pads, especially at high temperatures, can be harmful to individuals with peripheral arterial disease. It can increase the risk of burns or thermal injury due to reduced sensation in the affected areas. Heating pads should be used with caution and on a low temperature setting, if necessary.
Use callus remover for corns or calluses: Individuals with peripheral arterial disease have reduced blood flow to the lower extremities, which can impair wound healing. It is important to avoid self-treatment of corns or calluses, as it can increase the risk of skin breakdown and infection. Clients should be advised to consult a healthcare professional, such as a podiatrist, for appropriate management of corns and calluses.
The nurse is caring for a client scheduled for a cardiac stress test at 1100. When the nurse enters the client's room at 0800, the client requests toast or at least some coffee. What is the best response?
Explanation
The best response by the nurse would be to explain that no food or drink is allowed for 4 hours before the stress test.
The reason for this restriction is that consuming food or drink can affect the accuracy of the cardiac stress test results. Eating or drinking can increase heart rate and blood pressure, potentially altering the test's interpretation. It is important for the client to have an empty stomach to ensure accurate test results.
Let's review the other options and explain why they are not the best responses:
Asking the client's visitor to bring some coffee from the cafeteria for the client: This option goes against the restriction of no food or drink before the stress test. It is important to adhere to the guidelines provided to ensure accurate test results.
Making up a small breakfast tray from what is available on the unit: Similarly, providing breakfast to the client goes against the restriction of no food before the stress test. The client should have an empty stomach for the test.
Offering hot tea or coffee only: While hot tea or coffee might be tempting for the client, it still violates the requirement of no food or drink before the stress test. The client should only be allowed to consume water during the fasting period.
The charge nurse observes a new registered nurse (RN) doing discharge teaching for a client with hypertension who has a new prescription for enalapril (Vasotec). Which statement of the nurse to the patient would require the charge nurse's intervention?
Explanation
Enalapril (Vasotec) is an angiotensin-converting enzyme (ACE) inhibitor medication commonly used to treat hypertension. One of the potential side effects of ACE inhibitors is hyperkalemia, which is an elevated level of potassium in the blood. Therefore, it is generally recommended for patients taking ACE inhibitors to avoid excessive intake of high-potassium foods.
The charge nurse should intervene because advising the client to increase their dietary intake of high-potassium foods contradicts the precautions associated with taking enalapril. Consuming high-potassium foods while taking this medication can potentially lead to an increased risk of hyperkalemia, which can have serious health consequences.
Let's review the other statements made by the nurse:
"Make an appointment with the dietitian for teaching": This is an appropriate statement as it encourages the client to seek professional guidance on dietary management of hypertension. A dietitian can provide valuable information on healthy eating habits and strategies to reduce blood pressure.
"Check your blood pressure at home at least once a day": This is also an appropriate statement as it promotes self-monitoring of blood pressure, which is important for clients with hypertension. Regular monitoring helps the client track their progress and detect any changes that may require medical attention.
"Move slowly when moving from lying to sitting to standing": This is a correct statement as it advises the client to practice orthostatic precautions. ACE inhibitors, including enalapril, can cause orthostatic hypotension, a drop in blood pressure upon standing. Moving slowly can help prevent dizziness and falls.
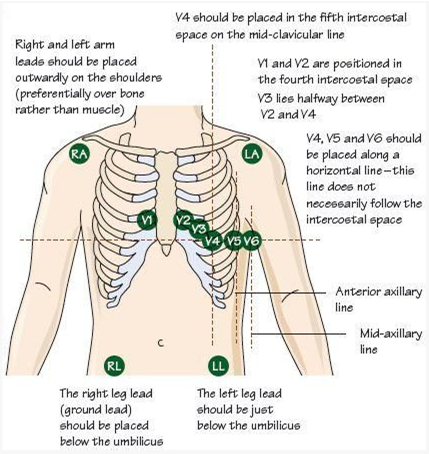
The nurse is performing a 12-lead ECG on a male client with abundant chest hair. What is the most appropriate nursing intervention to improve adhesion of the ECG leads?
Explanation
The most appropriate nursing intervention to improve adhesion of the ECG leads on a male client with abundant chest hair is to clip the chest hair with the patient's permission before applying the leads. Chest hair can interfere with the adhesion of the ECG leads, resulting in poor signal quality and potentially affecting the accuracy of the ECG recording. By clipping the chest hair, the nurse can improve the contact between the skin and the ECG leads, allowing for better adhesion and signal transmission.
It is important to obtain the patient's permission before clipping the chest hair to respect their autonomy and ensure their comfort during the procedure. The nurse should explain the reason for clipping the hair and address any concerns or questions the patient may have.
Let's review the other options and explain why they are not the most appropriate interventions:
Using alcohol swabs to clean the skin before applying the leads: While cleaning the skin with alcohol swabs is a routine practice to remove oils and dirt that can affect adhesion, it may not be sufficient in the presence of abundant chest hair. Clipping the hair would be more effective in this situation.
Applying the leads to the arms and legs only: This option would not provide an accurate 12-lead ECG recording, as the chest leads are essential for evaluating the electrical activity of the heart from different angles. It is important to have the leads properly placed on the chest for an accurate assessment.
Rescheduling the ECG: Unless there are other valid reasons for rescheduling, such as a medical condition that contraindicates the procedure, rescheduling solely due to abundant chest hair would be unnecessary. Clipping the hair is a practical and effective solution to improve adhesion.
The nurse is caring for a client with a pacemaker/ICD on a continuous cardiac monitor. Which trace should require immediate follow up by the nurse? Select all that apply
Explanation
The traces that should require immediate follow-up by the nurse are:
● Pacer spikes occur directly before the T waves.
Pacer spikes occurring on the T waves indicate an issue with the pacemaker's timing or sensing. This could lead to inappropriate pacing or pacing during the refractory period, which can be detrimental to the client's heart function.
● The heart rate is outside of programmed parameters.
If the heart rate is outside of the programmed parameters set for the client's pacemaker, it may indicate a malfunction or failure of the device or a change in the client's cardiac status. It is important for the nurse to assess the client's condition and notify the healthcare provider for further evaluation and intervention.
Let's review the other options and explain why they do not require immediate follow-up:
Pacer spikes are adequate in number: This indicates that the pacemaker is delivering the appropriate number of electrical impulses as programmed. As long as the other parameters are normal, this finding does not require immediate follow-up.
Pacer spikes occur directly before the P waves: This is the desired and expected pattern for a pacemaker in normal sinus rhythm. It indicates proper timing and coordination between the pacemaker and the client's intrinsic electrical activity.
Pacer spikes occur directly before the QRS waves: This is also the desired and expected pattern for a pacemaker in clients with ventricular pacing. It indicates proper timing and coordination between the pacemaker and the client's intrinsic electrical activity.
The heart rate is within programmed parameters: If the heart rate falls within the programmed parameters set for the client's pacemaker, it indicates that the device is functioning appropriately in maintaining the desired heart rate.
The nurse is interviewing a client with a complex cardiac history. Which questions related to the client's history are most important to ask? Select all that apply.
Explanation
The questions related to the client's history that are most important to ask are:
How would you describe your symptoms?: This question is important to assess the client's current cardiac symptoms and determine the severity, duration, and nature of their symptoms. It helps the nurse to evaluate the client's cardiac status and determine appropriate interventions.
Are you allergic to any medications or foods?: This question is crucial to identify any potential allergies that could impact the client's cardiac care. It helps the nurse ensure that medications and interventions are safe for the client and prevent any adverse reactions.
How did your mother die?:This question is important to gather information about the client's family history of cardiac diseases and potential risk factors. Understanding the family history helps the nurse assess the client's genetic predisposition to cardiac conditions and plan appropriate interventions and screenings.
Have you had shortness of breath or weight gain? : This question is important to assess for symptoms of heart failure or fluid retention. Shortness of breath and weight gain can indicate fluid accumulation, which is a common symptom in cardiac conditions. It helps the nurse evaluate the client's cardiac function and determine the need for furtherinterventions or medication adjustments.
Let's review the other options and explain why they are not the most important questions to ask:
Do you have any children?: While family history is important, specifically asking about children is not as relevant to the client's current cardiac condition. The focus should be on the client's own symptoms, medical history, and family history of cardiac diseases.
The nurse is reviewing the medical electronic record of a client with abdominal aortic aneurysm less than 3 cm in size. Which medical treatment should the nurse anticipate to be prescribed for the client?
Explanation
Based on the information provided, the nurse should anticipate that the medical treatment prescribed for a client with an abdominal aortic aneurysm less than 3 cm in size would be regular ultrasound screenings every six (6) months.
Monitoring the size of the abdominal aortic aneurysm through ultrasound is a common approach for managing small aneurysms. Regular ultrasound screenings allow healthcare providers to track the growth rate of the aneurysm and determine if any intervention, such as surgical repair, is necessary as the aneurysm progresses in size.
Let's review the other options and explain why they are not the most appropriate treatments for an abdominal aortic aneurysm less than 3 cm in size:
Intravenous pyelogram yearly: An intravenous pyelogram is an imaging test used to evaluate the urinary system, specifically the kidneys, ureters, and bladder. It is not directly related to the management or monitoring of an abdominal aortic aneurysm.
Assessment of abdominal girth monthly: Assessing the abdominal girth may be a part of the overall assessment of the client's condition, but it is not the primary treatment for managing an abdominal aortic aneurysm. Monitoring the aneurysm size through regular ultrasound screenings is a more specific and accurate approach.
Repair of abdominal aortic aneurysm: Repair of an abdominal aortic aneurysm is typically indicated when the aneurysm reaches a certain size threshold or if it poses a high risk of rupture. For an aneurysm less than 3 cm in size, repair is usually not the initial treatment option. Instead, regular monitoring through ultrasound screenings is recommended to assess the aneurysm's growth rate and determine the appropriate time for intervention.
The nurse is assessing a client with a presumptive diagnosis of peripheral arterial disease. The nurse obtains an Ankle-Brachial index of 0.89. Which intervention should the nurse take next?
Explanation
Based on the information provided, an Ankle-Brachial Index (ABI) of 0.89 indicates a mild reduction in blood flow to the lower extremities, suggesting peripheral arterial disease (PAD). In this case, the nurse should educate the client about the use of compression stockings.
Compression stockings are a conservative management approach for peripheral arterial disease. They help improve blood flow and alleviate symptoms by applying pressure to the legs, promoting venous return, and reducing swelling. Educating the client about the use of compression stockings can help improve circulation and manage symptoms such as pain, cramping, and fatigue.
Let's review the other options and explain why they are not the most appropriate interventions in this scenario:
Document the information as a normal finding: An ABI of 0.89 indicates an abnormal finding suggestive of peripheral arterial disease. It should not be documented as a normal finding, as it requires further assessment and intervention.
Prepare the client for an arterial bypass: An arterial bypass is a surgical intervention that is typically reserved for more severe cases of peripheral arterial disease. With an ABI of 0.89, which indicates mild reduction in blood flow, arterial bypass is not the first-line intervention. Conservative measures and medical management are usually recommended initially.
Anticipate a prescription for clopidogrel and simvastatin: Medications like clopidogrel (antiplatelet) and simvastatin (statin) may be prescribed for peripheral arterial disease. However, the next appropriate step after obtaining an ABI of 0.89 would be to educate the client about the use of compression stockings as a conservative management option before considering medication therapy.
The nurse is assessing a client with a hypertensive emergency. Which finding is most important to report to the health care provider?
Explanation
Among the given findings, the most important finding to report to the health care provider in a client with a hypertensive emergency is the new-onset blurry vision and facial asymmetry. These symptoms may indicate that the client is experiencing a hypertensive crisis with potential complications such as hypertensive encephalopathy or stroke.
Blurred vision and facial asymmetry are concerning neurological symptoms that suggest possible damage to the blood vessels or organs in the brain. It is crucial to notify the health care provider immediately so that appropriate interventions can be initiated to address the underlying cause and prevent further complications.
While the other findings may also be associated with elevated blood pressure, the new-onset blurry vision and facial asymmetry indicate possible neurological involvement and require immediate attention. Headache, epistaxis (nosebleed), and decreased urine output may be significant symptoms, but the potential neurological implications make the new-onset blurry vision and facial asymmetry the priority for reporting.
A nurse is assessing a client with a history of high blood pressure. The client's blood pressure is 210/106 mm Hg during the assessment. What follow-up question should the nurse ask?
Explanation
"Have you recently taken any antihistamines?": This question is not directly related to the client's high blood pressure. Antihistamines are medications used to treat allergic reactions and have minimal impact on blood pressure.
"Have there been recent stressful events in your life?": Stress can affect blood pressure levels, so this question is relevant. Stressful events can trigger temporary increases in blood pressure. However, it is important to note that consistently high blood pressure readings require medical attention beyond stress management alone.
"Did you take any acetaminophen today?": Acetaminophen (also known as paracetamol) is a pain reliever and fever reducer. It does not have a significant impact on blood pressure levels. Therefore, this question may not directly address the issue of high blood pressure.
"Have you consistently taken your medications?" : This question is the most appropriate follow-up question for a client with a history of high blood pressure. It addresses medication adherence, which is crucial for managing hypertension. The client's blood pressure reading of 210/106 mm Hg suggests that their current medication regimen may not be effectively controlling their blood pressure. Assessing medication consistency will help determine if the elevated blood pressure is due to non-adherence or if a change in medication is required.
Which assessment data would require immediate intervention by the nurse for the client who is six (6) hours post-operative abdominal aortic aneurysm repair?
Explanation
Absent bilateral pedal pulses indicate a potential vascular complication, such as impaired circulation or blood flow to the lower extremities. It may suggest compromised perfusion and could be a sign of arterial occlusion or thrombosis, which requires immediate intervention. The nurse should notify the healthcare provider promptly to assess the client's condition and initiate appropriate interventions to restore circulation to the lower extremities.
While complaints of pain at the site of the incision are significant, post-operative pain is expected after abdominal surgery. The nurse should assess the pain and provide appropriate pain management interventions, but it may not require immediate intervention unless the pain is severe or accompanied by other concerning symptoms.
A distended, tender abdomen could indicate various post-operative complications, such as bowel obstruction or peritonitis. Although it should be evaluated and reported to the healthcare provider, it may not require immediate intervention unless the client's condition deteriorates or other signs of a surgical emergency are present.
An elevated temperature of 100°F (37.8°C) alone, without other signs of infection or systemic complications, may not necessarily require immediate intervention. It could be a normal response to surgery or a mild post-operative infection. The nurse should monitor the client's temperature and assess for other signs of infection, and if necessary, report it to the healthcare provider for further evaluation.
Sign Up or Login to view all the 45 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

