Medical_surgical_nursing_2{NURSA_225_01C}_University_of_charleton
Total Questions : 52
Showing 25 questions, Sign in for more
Please identify the following rhythm: 
Explanation
Answer and explanation
The correct answer is C. Normal Sinus Rhythm.
Choice A rationale:
Asystole is the absence of all electrical activity in the heart, as evidenced by a flat line on the electrocardiogram (ECG). It is a medical emergency that requires immediate cardiopulmonary resuscitation (CPR) and defibrillation.
Key features of asystole on ECG:
No discernible P waves, QRS complexes, or T waves.
A completely flat or nearly flat line on the ECG tracing.
Choice B rationale:
Atrial flutter is a rapid heart rhythm that arises from abnormal electrical activity in the atria. It is characterized by a sawtooth pattern on the ECG, with atrial rates typically between 250 and 350 beats per minute.
Key features of atrial flutter on ECG:
Absence of distinct P waves, instead replaced by flutter waves (sawtooth pattern).
Regular, rapid atrial rate (typically 250-350 bpm).
QRS complexes may be normal or slightly irregular in appearance.
Choice C rationale:
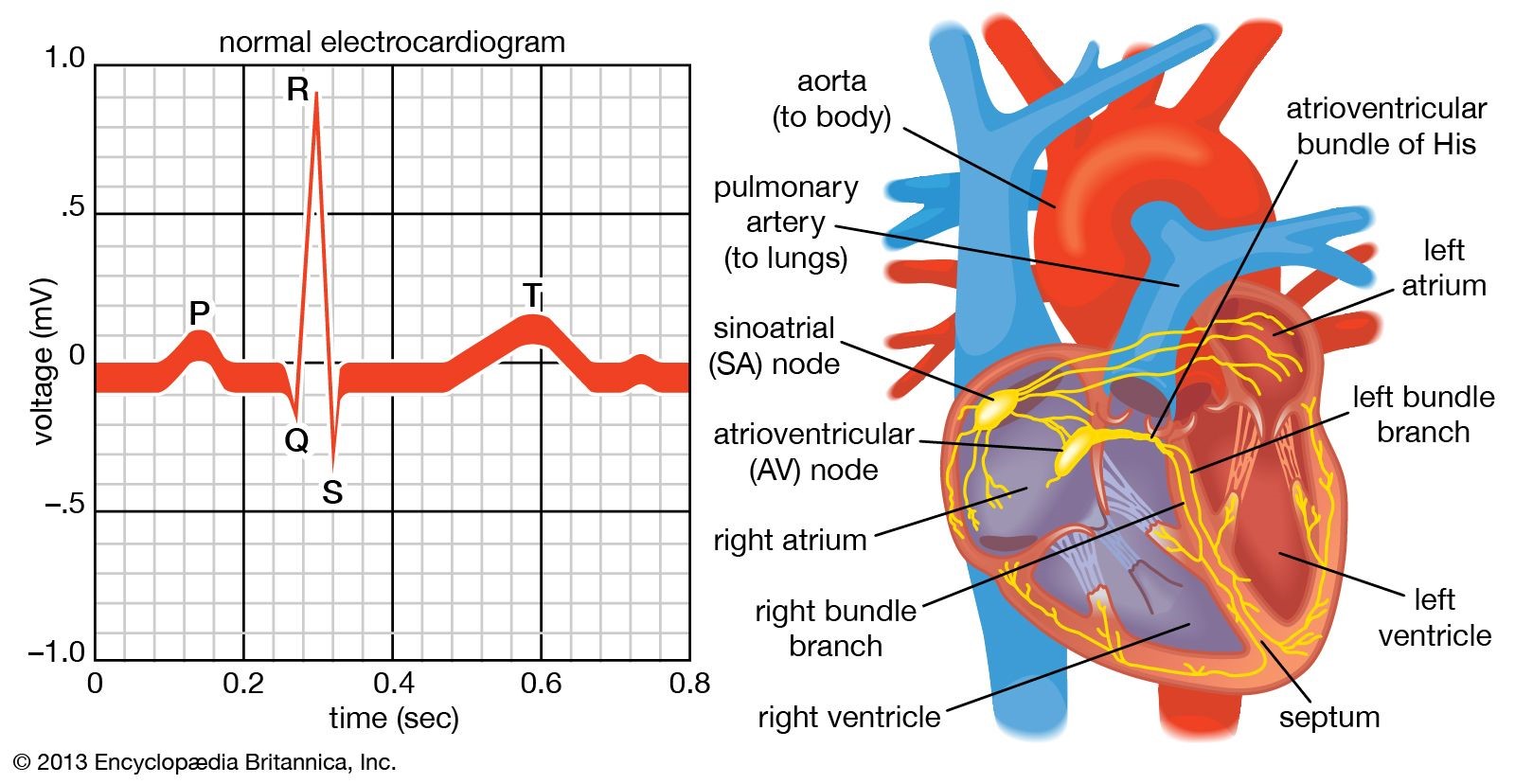
Normal sinus rhythm is the natural, healthy rhythm of the heart. It originates in the sinoatrial (SA) node, the heart's natural pacemaker, and is characterized by a regular rate of 60-100 beats per minute, with consistent P waves, QRS complexes, and T waves on the ECG.
Key features of normal sinus rhythm on ECG:
Presence of distinct P waves, QRS complexes, and T waves.
Regular rhythm with a rate of 60-100 beats per minute.
PR interval (the time between the P wave and QRS complex) is 0.12-0.20 seconds.
QRS duration (the time it takes for the ventricles to depolarize) is less than 0.12 seconds.
Choice D rationale:
Sinus bradycardia is a slow heart rhythm, with a rate below 60 beats per minute. It is often a normal finding in healthy individuals, especially athletes or during sleep. However, it can also be a sign of underlying medical conditions.
Key features of sinus bradycardia on ECG:
Presence of distinct P waves, QRS complexes, and T waves.
Regular rhythm with a rate less than 60 beats per minute.
PR interval and QRS duration are typically normal.
When assisting with defibrillating an adult client who has gone into ventricular fibrillation, what must the nurse do?
Explanation
Choice A rationale:
Calling "all clear" once before discharging the defibrillator is crucial for safety, but it's not the primary action that ensures effective defibrillation.
The purpose of calling "all clear" is to alert everyone in the vicinity to stay clear of the patient and avoid accidental shock.
However, even with a clear announcement, it's essential for the nurse to visually confirm that no one is touching the patient or bed before discharging the defibrillator.
Choice B rationale:
Maintaining firm contact between the paddles and the client's skin is essential for delivering the defibrillation shock effectively.
Here's a detailed breakdown of why this contact is so critical:
Maximizes energy transfer: Firm contact minimizes the impedance (resistance) between the paddles and the skin, allowing for the maximum amount of electrical energy to be transferred to the heart.
Reduces arcing: Arcing occurs when electrical energy jumps through the air instead of passing through the intended path (between the paddles and the heart). This can cause skin burns and reduce the effectiveness of the shock. Firm contact helps prevent arcing by ensuring a direct connection.
Ensures consistent current flow: Consistent contact ensures that the electrical current flows evenly across the chest, reaching all areas of the heart muscle. This increases the likelihood of successful defibrillation.
Minimizes energy loss: Any gaps or poor contact between the paddles and skin can lead to energy loss, reducing the shock's strength and effectiveness.
Choice C rationale:
Sync mode (synchronized cardioversion) is used for specific heart rhythm disturbances, such as atrial fibrillation or atrial flutter, where the shock needs to be timed with the QRS complex on the ECG.
Ventricular fibrillation, however, is a chaotic rhythm without distinct QRS complexes, so sync mode is not appropriate.
Using sync mode in ventricular fibrillation could delay the shock and potentially decrease its effectiveness.
Choice D rationale:
Water is not an appropriate conducting agent for defibrillation.
It can actually increase the risk of burns and decrease the effectiveness of the shock.
Approved conducting agents, such as gel pads or paste, should be used to ensure optimal energy transfer and patient safety.
A client converts from normal sinus rhythm at 80 bpm to atrial fibrillation with a ventricular response at 165 bpm.
Blood pressure is 162/74 mm Hg. Respiratory rate is 20 breaths per minute with normal chest expansion and clear lungs bilaterally.
IV heparin and Diltiazem are given.
What is the main goal of treatment?
Explanation
Choice A rationale:
While maintaining anticoagulation is important in atrial fibrillation to prevent blood clots, it is not the main goal of treatment in this specific scenario.
The client's blood pressure is elevated, suggesting that the rapid heart rate is the more immediate concern.
Additionally, the prompt indicates that heparin has already been administered, addressing the anticoagulation need.
Choice B rationale:
The client's respiratory rate and lung sounds are normal, indicating that oxygenation is not a primary concern at this time.
The fast heart rate is the more pressing issue, as it can lead to decreased cardiac output and potential complications.
Choice C rationale:
Controlling the ventricular heart rate is the main goal of treatment in this case.
Atrial fibrillation with a rapid ventricular response can lead to several detrimental consequences, including:
Decreased cardiac output due to shortened ventricular filling time
Increased myocardial oxygen demand, potentially causing angina or heart failure
Increased risk of stroke or other thromboembolic events
Diltiazem, a calcium channel blocker, is a medication commonly used to slow the heart rate in atrial fibrillation.
By slowing the conduction of electrical impulses through the atrioventricular (AV) node, it effectively reduces the number of impulses that reach the ventricles, thereby controlling the ventricular response.
Choice D rationale:
Decreasing SA node conduction is not a primary goal in this situation.
The SA node is responsible for initiating the normal electrical impulses that trigger heart contractions.
In atrial fibrillation, the electrical activity is chaotic and originates from multiple foci within the atria, rather than the SA node.
Therefore, targeting the SA node would not effectively address the underlying rhythm disturbance.
The nurse is doing discharge teaching with a client who has coronary artery disease.
The client asks why he has to take an aspirin every day if he doesn’t have any pain.
What would be the nurse’s best response?
Explanation
Choice A rationale:
While aspirin can help improve heart function in certain cases, such as by reducing inflammation, it's not accurate to say it directly restores normal heart function. This statement oversimplifies aspirin's mechanism of action and could mislead the client.
It's essential to emphasize aspirin's role in preventing clots, which is the primary reason for its use in coronary artery disease.
Choice B rationale:
Aspirin does not affect the oxygen-carrying capacity of blood. This function is primarily carried out by hemoglobin in red blood cells.
Stating that aspirin increases oxygen-carrying capacity could create misunderstandings about its role in coronary artery disease.
Choice C rationale:
Aspirin does not directly make blood penetrate the heart more freely. Its action primarily involves preventing blood clots from forming within blood vessels.
This statement could lead to a misconception about aspirin's mechanism of action, potentially affecting adherence to treatment.
Choice D rationale:
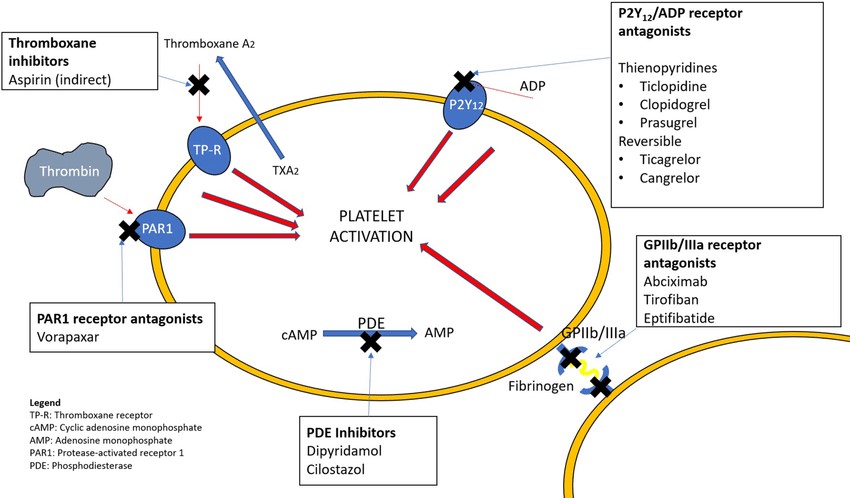
This is the most accurate and comprehensive response. It directly addresses the client's question and highlights the primary reason for daily aspirin use in coronary artery disease.
Aspirin inhibits platelet aggregation, reducing the risk of blood clots that can obstruct coronary arteries and trigger heart attacks or chest pain.
By preventing these blockages, aspirin can help prevent future cardiovascular events and improve the client's overall health outcomes.
A 35-year-old male patient presents to the Emergency Room with complaints of sudden onset chest pain, numbness and tingling in the left arm, and shortness of breath.
What labs can the nurse anticipate the physician ordering upon arrival? (Select all that Apply) A. Creatine Kinase (CK)
Explanation
The correct answers are B. Complete Blood Count (CBC) and D. Troponin. B. Complete Blood Count (CBC) rationale:
Assessment of blood cell counts: A CBC provides essential information about the patient's blood cells, including red blood cells (RBCs), white blood cells (WBCs), and platelets. This information can help rule out or identify potential causes of the patient's symptoms:
Anemia: A low RBC count could indicate anemia, which can contribute to shortness of breath and chest pain.
Infection: An elevated WBC count could suggest an infection, which might be contributing to the patient's symptoms.
Platelet count: Abnormalities in platelet count could indicate bleeding disorders or clotting problems, which are relevant in the context of potential acute coronary syndrome (ACS).
Baseline for further investigations: A CBC often serves as a baseline for further investigations and monitoring of the patient's condition.
D. Troponin rationale:
Cardiac-specific biomarker: Troponin is a protein found in heart muscle cells. It is released into the bloodstream when heart muscle is damaged, making it a highly sensitive and specific biomarker for myocardial infarction (MI).
Early detection of MI: Elevated troponin levels can indicate myocardial injury, even before significant ECG changes or clinical symptoms fully manifest. Early detection of MI is crucial for prompt treatment and improved outcomes.
Differentiation of MI from other causes: Troponin levels can help differentiate MI from other potential causes of chest pain, such as pulmonary embolism, pericarditis, or musculoskeletal pain.
Rationale for exclusion of other choices:
A. Creatine Kinase (CK): While CK can be elevated in MI, it is not as specific as troponin and can be elevated in other conditions such as muscle injury or strenuous exercise.
C. C-Reactive Protein (CRP): CRP is a marker of inflammation, but it is not specific for cardiac injury. It can be elevated in various inflammatory conditions, including infections and autoimmune diseases.
A nurse is describing the process by which blood is ejected into circulation as the chambers of the heart become smaller.
How does the nurse categorize this action of the heart?
Explanation
Choice A Rationale:
Repolarization is a phase in the cardiac cycle that involves the restoration of electrical charges in heart muscle cells, enabling them to prepare for the next contraction. It does not directly refer to the physical contraction and ejection of blood from the chambers.
During repolarization, the heart muscle cells regain their negative electrical charge after depolarization, which triggered the contraction.
Repolarization is essential for maintaining the heart's rhythmic electrical activity and ensuring coordinated contractions.
It does not, however, cause the chambers to become smaller and eject blood, which is the defining feature of systole.
Choice C Rationale:
Diastole is the phase of the cardiac cycle when the heart chambers relax and fill with blood. It is the opposite of systole.
During diastole, the heart muscle relaxes, allowing the chambers to passively expand and collect blood from the veins.
The atrioventricular valves (mitral and tricuspid valves) open during diastole, allowing blood to flow from the atria into the ventricles.
While diastole is crucial for ensuring adequate blood supply to the heart, it does not involve the forceful ejection of blood into circulation that characterizes systole.
Choice D Rationale:
Ejection fraction is a measurement of the heart's pumping efficiency. It represents the percentage of blood that is ejected from the left ventricle with each contraction.
A normal ejection fraction is typically between 55% and 70%.
While ejection fraction is related to systole, it is not a synonym for it. Ejection fraction is a quantitative measure of how well the heart is pumping, while systole refers to the specific phase of the cardiac cycle when contraction and ejection occur.
An older adult client’s assessment reveals the following data: Lying BP 144/82 mm Hg, sitting BP 121/69 mm Hg, standing BP 98/56 mm Hg. What nursing diagnosis should be identified in the client’s plan of care?
Explanation
correct answer is Choice B.
Choice B rationale:
Orthostatic hypotension is a significant drop in blood pressure that occurs when a person stands up from a lying or sitting position. It's characterized by a decrease in systolic blood pressure of at least 20 mmHg or a decrease in diastolic blood pressure of at least 10 mmHg within 3 minutes of standing.
The client's assessment data clearly demonstrates orthostatic hypotension, with a systolic blood pressure drop of 23 mmHg and a diastolic drop of 13 mmHg upon standing.
Orthostatic hypotension is a major risk factor for falls, especially in older adults. This is because the sudden decrease in blood pressure can lead to lightheadedness, dizziness, blurred vision, weakness, and even fainting.
Falls in older adults can result in serious injuries, such as fractures, head trauma, and even death. Therefore, it's crucial to identify and address orthostatic hypotension to prevent falls and their associated complications.
Rationales for other choices:
Choice A: Ineffective breathing pattern is not directly related to orthostatic hypotension. While hypotension can cause shortness of breath in some cases, it's not the primary concern in this scenario.
Choice C: Ineffective role performance can be a consequence of frequent falls, but it's not the most immediate or pressing nursing diagnosis in this case.
Choice D: Risk for imbalanced fluid balance is a potential concern in some cases of orthostatic hypotension, but it's not the most likely diagnosis based on the client's assessment data.
Identify the following rhythm:
Explanation
Atrial fibrillation (AF) is characterized by disorganized electrical activity in the atria, resulting in an irregular and often rapid heart rate.
On an ECG, AF typically presents with absent P waves, irregular R-R intervals, and a rapid ventricular rate (usually >100 beats per minute).
However, the rhythm in the question does not display these characteristic features of AF.
Key features of AF that are absent in the rhythm include:
P waves: AF lacks identifiable P waves, while the rhythm in question may have discernible P waves, although they may be irregular or abnormal.
Regularity: AF is typically irregular, while the rhythm in question is chaotic and without any discernible pattern.
QRS complexes: AF usually has narrow QRS complexes, while the rhythm in question often has wide and bizarre QRS complexes. Choice B rationale:
Ventricular tachycardia (VT) is a rapid heart rhythm originating from the ventricles, with a rate typically exceeding 100 beats per minute.
On an ECG, VT typically presents with wide QRS complexes (>0.12 seconds), a regular or slightly irregular rhythm, and a rate often exceeding 150 beats per minute.
While the rhythm in question is rapid and may have wide QRS complexes, it lacks the regular or slightly irregular pattern often seen in VT.
Key features of VT that distinguish it from the rhythm in question include:
Regularity: VT often has a regular or slightly irregular pattern, while the rhythm in question is chaotic and without any discernible pattern.
QRS morphology: VT typically has monomorphic (uniform) QRS complexes, while the rhythm in question often has polymorphic (varying) QRS complexes.
Choice D rationale:
Premature ventricular contractions (PVCs) are extra heartbeats originating from the ventricles, interrupting the normal heart rhythm.
On an ECG, PVCs appear as early, wide QRS complexes that are often followed by a compensatory pause.
The rhythm in question does not exhibit the characteristic pattern of PVCs, which typically occur as isolated beats or short runs of beats interspersed within a normal rhythm.
Key features of PVCs that are absent in the rhythm include:
Isolation: PVCs typically occur as isolated beats or short runs of beats, while the rhythm in question is sustained and chaotic.
Compensatory pause: PVCs are often followed by a compensatory pause, which is not a feature of the rhythm in question.
The patient’s cardiac rhythm suddenly changes on the monitor.
There are no P waves, instead there are fibrillatory waves before each QRS complex.
How would the nurse interpret the rhythm?
Explanation
Atrial fibrillation (AF) is characterized by the absence of P waves on the ECG, the presence of fibrillatory waves, and an irregularly irregular rhythm. This is due to chaotic electrical activity in the atria, which results in disorganized atrial contractions. The fibrillatory waves, which are often described as "f" waves or "sawtooth" waves, represent the rapid and irregular electrical activity in the atria. They are typically best seen in lead II, V1, or V2 of the ECG.
Here is a more detailed explanation of the key features of AF that support this answer:
Absence of P waves: In normal sinus rhythm, the P wave represents the electrical impulse that originates in the sinoatrial (SA) node and depolarizes the atria. In AF, the SA node is no longer in control of the atrial rhythm, and there is no organized atrial depolarization. As a result, P waves are absent on the ECG.
Presence of fibrillatory waves: The fibrillatory waves seen in AF represent the disorganized electrical activity in the atria. They are typically irregular in amplitude and frequency, and they can vary in appearance from patient to patient.
Irregularly irregular rhythm: The ventricular rhythm in AF is also irregular because the impulses from the atria are not conducted to the ventricles in a regular pattern. This results in an irregularly irregular rhythm, which is a hallmark feature of AF.
Key points to remember:
AF is the most common type of cardiac arrhythmia.
It can be asymptomatic or cause a variety of symptoms, including palpitations, shortness of breath, fatigue, and lightheadedness.
AF is a risk factor for stroke and heart failure.
Treatment for AF may include medications to control heart rate or rhythm, blood thinners to reduce the risk of stroke, and in some cases, procedures to restore normal heart rhythm.
A client with angina has been prescribed nitroglycerin.
Before administering the drug, what potential adverse effects should the nurse inform the client about?
Explanation
Choice A rationale:
Drowsiness and blurred vision are not common adverse effects of nitroglycerin.
While some individuals may experience mild drowsiness, it's not a primary concern.
Blurred vision is not typically associated with nitroglycerin use.
Choice B rationale:
Nervousness and paresthesia (tingling or numbness in the extremities) are not common adverse effects of nitroglycerin.
Some individuals may experience transient anxiety or nervousness, but it's not a characteristic side effect.
Paresthesia is more commonly associated with other medications or conditions.
Choice C rationale:
Throbbing headache and dizziness are the most common adverse effects of nitroglycerin.
They occur due to nitroglycerin's vasodilatory effect, which causes blood vessels to relax and widen.
This can lead to a temporary drop in blood pressure, resulting in headaches and dizziness.
The headaches are often described as throbbing or pulsating, and they typically occur in the frontal or temporal regions of the head.
Dizziness may be mild or severe, and it may be accompanied by lightheadedness or a feeling of unsteadiness.
Choice D rationale:
Tinnitus (ringing in the ears) and diplopia (double vision) are not common adverse effects of nitroglycerin.
They may occur in rare cases, but they are not typically associated with its use.
The ED nurse is caring for a client who has gone into cardiac arrest.
During external defibrillation, what action should the nurse perform?
Explanation
Choice B rationale:
It is crucial to ensure that no one is touching the client during defibrillation to prevent accidental electrical shock to others. The electrical current delivered by the defibrillator is extremely powerful and can cause serious injury or even death if it passes through another person's body. This includes both healthcare professionals and bystanders.
Here are key points to emphasize this rationale:
Electrical conduction: The human body is a good conductor of electricity. If someone is touching the client during defibrillation, the electrical current from the defibrillator can easily pass through their body, potentially causing harm.
Cardiac rhythm disruption: Any contact with the client during shock delivery can interfere with the defibrillator's ability to accurately assess the client's heart rhythm and deliver the appropriate shock. This could potentially worsen the client's condition.
Muscle contractions: The electrical current from the defibrillator can cause involuntary muscle contractions. If someone is touching the client, these contractions could cause them to jerk or move suddenly, potentially causing injury to themselves or others.
Safety guidelines: It is a standard safety guideline in all healthcare settings to clear the area around a client before defibrillation to ensure the safety of everyone involved.
I'll now address the other choices, even though they are not the correct answer, to provide a comprehensive understanding:
Choice A rationale:
While ventilation is important during cardiac arrest, it should be temporarily paused during defibrillation. The chest compressions and electrical shock can cause movement of air in the lungs, which can interfere with the effectiveness of the defibrillation. Additionally, the risk of accidental shock to the person providing ventilation is increased if they are close to the client during defibrillation.
Choice C rationale:
Waiting 3 minutes between shocks is not necessary with modern defibrillators. Current guidelines recommend immediate defibrillation for shockable rhythms such as ventricular fibrillation or pulseless ventricular tachycardia. Delaying defibrillation can decrease the chances of successful resuscitation.
Choice D rationale:
The placement of gel pads is important for effective conduction, but it is not the priority action during defibrillation. Ensuring safety by clearing the area and delivering the shock promptly is more critical in the initial moments of defibrillation.
Aspirin is administered to the client experiencing an MI because of its:
Explanation
Choice A rationale:
Antipyretic action refers to the ability to reduce fever. While aspirin does have antipyretic properties, this is not the primary reason it is administered during an MI. Fever is not a characteristic symptom of MI, and reducing fever would not directly address the underlying cause of the MI, which is the formation of a blood clot in a coronary artery.
Choice B rationale:
Antiplatelet action is the ability to prevent platelets from clumping together and forming blood clots. This is the crucial mechanism by which aspirin helps in the setting of an MI.
During an MI, a blood clot forms in a coronary artery, blocking blood flow to the heart muscle. This blockage can cause severe damage to the heart muscle, leading to chest pain, shortness of breath, and potentially life-threatening complications.
Aspirin irreversibly inhibits the enzyme cyclooxygenase (COX), which is essential for platelet aggregation. By blocking COX, aspirin prevents platelets from sticking together and forming new clots. This can help to:
Limit the size of the existing clot in the coronary artery.
Prevent the formation of additional clots that could further block blood flow.
Allow for better blood flow to the heart muscle, reducing damage and improving outcomes.
Choice C rationale:
Analgesic action refers to the ability to relieve pain. While aspirin does have analgesic properties, this is not the primary reason it is administered during an MI. Pain relief is an important aspect of managing MI symptoms, but it does not directly address the underlying cause of the MI, which is the blood clot.
Choice D rationale:
Antithrombotic action is a broader term that encompasses any action that prevents or reduces blood clot formation. Aspirin's antiplatelet action is a specific type of antithrombotic action. However, it's important to note that aspirin does not directly dissolve existing clots; it primarily prevents new clots from forming.
A patient who had a myocardial infarction asks the nurse why they are receiving morphine.
Which benefits of morphine should the nurse explain to this patient? (Select all that apply)
Explanation
Choice A rationale:
Pain relief is a primary benefit of morphine administration in the setting of myocardial infarction.
Pain can trigger a stress response, leading to increased heart rate, blood pressure, and myocardial oxygen demand.
Morphine effectively reduces pain, thereby lessening the stress response and its detrimental effects on the heart.
This helps to minimize myocardial ischemia and potential further damage to the heart muscle.
Pain control also improves patient comfort and overall well-being, which can indirectly contribute to better cardiac outcomes.
Choice B rationale:
Sedation is another important benefit of morphine in this context.
It promotes rest and relaxation, which can lower heart rate, blood pressure, and myocardial oxygen demand.
This is crucial for patients with myocardial infarction, as their hearts require reduced workload to heal and recover.
Sedation also helps to alleviate anxiety and agitation, which can further strain the heart.
By inducing a state of calmness, morphine can indirectly protect the heart from additional stress.
Choice C rationale:
While morphine does have diuretic effects, increasing urinary output is not a primary goal in the management of myocardial infarction.
In fact, excessive diuresis could potentially lead to dehydration and hypotension, which could be detrimental to cardiac function.
Therefore, while morphine may slightly increase urine output, this is not a major reason for its use in this setting.
Choice D rationale:
Decreasing myocardial demand is a key benefit of morphine administration in patients with myocardial infarction.
Morphine achieves this by:
Reducing pain and the associated stress response
Promoting sedation and relaxation
Diminishing anxiety and agitation
Exerting a direct vasodilatory effect on blood vessels
This collective action of morphine leads to a decrease in heart rate, blood pressure, and the heart’s overall workload.
As a result, the heart requires less oxygen and experiences reduced strain, allowing for better healing and recovery following a myocardial infarction.
understanding of the significance of these levels?
A. The increased LDL will decrease the amount of cholesterol deposited on the artery walls.
Explanation
Choice A rationale:
Pain relief is a primary benefit of morphine administration in the setting of myocardial infarction.
Pain can trigger a stress response, leading to increased heart rate, blood pressure, and myocardial oxygen demand.
Morphine effectively reduces pain, thereby lessening the stress response and its detrimental effects on the heart.
This helps to minimize myocardial ischemia and potential further damage to the heart muscle.
Pain control also improves patient comfort and overall well-being, which can indirectly contribute to better cardiac outcomes.
Choice B rationale:
Sedation is another important benefit of morphine in this context.
It promotes rest and relaxation, which can lower heart rate, blood pressure, and myocardial oxygen demand.
This is crucial for patients with myocardial infarction, as their hearts require reduced workload to heal and recover.
Sedation also helps to alleviate anxiety and agitation, which can further strain the heart.
By inducing a state of calmness, morphine can indirectly protect the heart from additional stress.
Choice C rationale:
While morphine does have diuretic effects, increasing urinary output is not a primary goal in the management of myocardial infarction.
In fact, excessive diuresis could potentially lead to dehydration and hypotension, which could be detrimental to cardiac function.
Therefore, while morphine may slightly increase urine output, this is not a major reason for its use in this setting.
Choice D rationale:
Decreasing myocardial demand is a key benefit of morphine administration in patients with myocardial infarction.
Morphine achieves this by:
Reducing pain and the associated stress response
Promoting sedation and relaxation
Diminishing anxiety and agitation
Exerting a direct vasodilatory effect on blood vessels
This collective action of morphine leads to a decrease in heart rate, blood pressure, and the heart’s overall workload.
As a result, the heart requires less oxygen and experiences reduced strain, allowing for better healing and recovery following a myocardial infarction.
The nurse is conducting patient teaching about cholesterol levels.
When discussing the patient’s elevated LDL and lowered HDL levels, which statement by the patient indicates an understanding of the significance of these levels?
Explanation
Choice B rationale:
LDL (low-density lipoprotein) cholesterol is often referred to as "bad" cholesterol. It contributes to the buildup of plaque in the arteries, which narrows the arteries and can lead to coronary artery disease (CAD). CAD is a major risk factor for heart attack and stroke.
HDL (high-density lipoprotein) cholesterol is often referred to as "good" cholesterol. It helps to remove LDL cholesterol from the arteries and transport it back to the liver, where it can be broken down and removed from the body. Therefore, a high HDL level is protective against heart disease.
An elevated LDL level and a lowered HDL level are both associated with an increased risk of CAD. This is because the elevated LDL level contributes to plaque buildup, while the lowered HDL level means that there is less "good" cholesterol available to remove the "bad" cholesterol from the arteries.
Therefore, the statement "Increased LDL and decreased HDL increase my risk of coronary artery disease" indicates an understanding of the significance of these cholesterol levels.
Choice A rationale:
This statement is incorrect. An increased LDL level will actually increase the amount of cholesterol deposited on the artery walls.
Choice C rationale:
This statement is also incorrect. A decreased HDL level will decrease the amount of cholesterol moved away from the artery walls.
Choice D rationale:
This statement is incorrect. Increased LDL has the potential to increase, not decrease, the risk of heart disease.
In preparation for cardiac surgery, a patient was taught about measures to prevent venous thromboembolism.
Which statement indicates that the patient clearly understood this education?
Explanation
Choice A rationale:
Venous thromboembolism (VTE) is a blood clot that forms in a vein, usually in the legs. It can be a serious condition, as the clot can break loose and travel to the lungs, causing a pulmonary embolism (PE).
Crossing the legs at the knees can impede blood flow in the veins of the legs, increasing the risk of VTE. This is because it compresses the veins, slowing the flow of blood and making it more likely for clots to form.
The patient's statement that they will make sure not to cross their legs when resting in bed demonstrates that they understand this important risk factor for VTE and are taking steps to prevent it.
Choice B rationale:
While keeping pillows under the knees can help to improve circulation, it is not a specific measure to prevent VTE. It is more important to avoid crossing the legs and to engage in regular movement and activity to promote blood flow.
Choice C rationale:
Compression stockings can help to reduce the risk of VTE by compressing the veins in the legs and promoting blood flow. However, they should be worn as instructed by a healthcare professional, and not only if the patient experiences pain in their calves. Pain in the calves can be a symptom of VTE, so it is important to seek medical attention if it occurs.
Choice D rationale:
Bed rest is actually a risk factor for VTE, as it can lead to decreased blood flow in the legs. It is important to get up and move around as soon as possible after surgery, even if it is just for short periods of time. This will help to promote blood flow and reduce the risk of VTE.
A patient is scheduled for catheter ablation therapy.
When describing this procedure to the patient’s family, what aspect of the treatment should the nurse address? A. Clearance of partially occluded coronary arteries.
Explanation
Choice A rationale:
Clearance of partially occluded coronary arteries is not a primary goal of catheter ablation therapy. This procedure is not designed to remove blockages in the coronary arteries. Instead, it focuses on targeting and disrupting abnormal electrical signals within the heart.
While coronary artery disease (CAD) can coexist with heart rhythm problems, and both may share risk factors like high blood pressure and cholesterol, catheter ablation specifically addresses electrical disturbances, not structural blockages in blood vessels.
Procedures like angioplasty or coronary artery bypass grafting (CABG) are used to address coronary artery blockages.
Choice B rationale:
Resetting of the heart’s contractility is not the primary mechanism of catheter ablation. While the procedure can sometimes improve heart function by reducing abnormal heart rhythms, its primary aim is to eliminate the abnormal electrical signals that cause arrhythmias, not directly enhance the heart's pumping ability.
Medications like beta-blockers or calcium channel blockers are often used to address contractility issues.
Choice C rationale:
Destruction of specific cardiac cells is the correct answer. Catheter ablation works by using energy (usually radiofrequency or cryoablation) to destroy small areas of heart tissue that are responsible for generating or conducting abnormal electrical signals.
By targeting these specific cells, the procedure can interrupt the pathways that cause arrhythmias, effectively eliminating or significantly reducing their occurrence.
This targeted approach is what distinguishes catheter ablation from medications, which often act on the entire heart rather than specific areas.
Choice D rationale:
Correction of structural cardiac abnormalities is not a goal of catheter ablation. This procedure is designed to address electrical problems within the heart, not structural defects like valve problems or holes in the heart walls.
Surgical procedures are typically used to correct structural abnormalities.
A patient who is a candidate for an implantable cardioverter defibrillator (ICD) asks the nurse about the purpose of this device.
What would be the nurse’s best response?
Explanation
Choice A rationale:
Bradycardia refers to a slow heart rate, typically defined as less than 60 beats per minute.
While some ICDs can provide pacing for bradycardia, this is not their primary purpose.
Their primary goal is to prevent sudden cardiac death from life-threatening arrhythmias.
Therefore, Choice A is not the best response.
Choice B rationale:
Atrial fibrillation (AFib) is a common heart rhythm disorder characterized by rapid and irregular beating of the atria.
While ICDs can sometimes be used in patients with AFib, this is not their primary indication.
AFib is typically managed with medications to control heart rate and rhythm, or with ablation procedures to disrupt the abnormal electrical pathways.
Therefore, Choice B is not the best response.
Choice C rationale:
Ventricular fibrillation (VF) and ventricular tachycardia (VT) are life-threatening arrhythmias that originate in the ventricles of the heart.
VF is characterized by chaotic, disorganized electrical activity in the ventricles, leading to ineffective pumping and cardiac arrest.
VT is a very fast heart rhythm that can degenerate into VF.
ICDs are specifically designed to detect and treat VF and VT.
They do this by delivering electrical shocks to the heart, which can restore a normal rhythm.
Therefore, Choice C is the best response.
Choice D rationale:
While ICDs can deliver shocks during a heart attack, this is not their primary purpose.
Heart attacks are caused by a blockage of blood flow to the heart muscle, and they are typically treated with medications, such as aspirin, nitroglycerin, and clot-busting drugs.
ICDs are primarily used to prevent sudden cardiac death from life-threatening arrhythmias, not to treat heart attacks themselves.
Which statement is true regarding Premature Ventricular Contractions (PVCs)?
Explanation
Choice A rationale:
Incorrect. PVCs are not caused by a malfunctioning SA node. The SA node is responsible for initiating the normal heartbeat, while PVCs originate from the ventricles. The underlying cause of PVCs can vary, but it's not directly related to SA node dysfunction. Choice C rationale:
Incorrect. Ventricular tachycardia (VT) is a rapid heart rhythm originating from the ventricles, typically defined as three or more consecutive PVCs. Two PVCs in a row are usually classified as a couplet, not VT.
Choice D rationale:
Incorrect. While PVCs are often harmless, they can sometimes be associated with underlying heart disease or lead to complications, especially if they are frequent or occur in specific patterns. Therefore, careful assessment and potential treatment are necessary.
Choice B rationale:
Correct. Treatment for PVCs is generally only recommended if the patient experiences concerning symptoms or if the PVCs are associated with a risk of developing more serious arrhythmias. Additionally, the QRS complex on the EKG/ECG should be evaluated. A narrow QRS complex during PVCs typically suggests a less concerning origin within the ventricles, while a wide QRS complex may indicate a higher risk of complications.
Toxicity from which of the following medications may cause a patient to see a green-yellow halo around lights?
Explanation
Choice A rationale:
Metoprolol (Lopressor) is a beta-blocker that primarily affects the heart and blood vessels. It does not have a direct effect on the visual system, and therefore, it is not associated with the green-yellow halo symptom.
Common side effects of metoprolol include:
Fatigue
Bradycardia (slow heart rate)
Hypotension (low blood pressure)
Dizziness
Cold extremities
Bronchospasm (narrowing of the airways)
Diarrhea
Tinnitus (ringing in the ears)
Decreased exercise tolerance
Glucose intolerance
Masking of hypoglycemia symptoms Choice B rationale:
Enalapril (Vasotec) is an angiotensin-converting enzyme (ACE) inhibitor that primarily affects the kidneys and blood vessels. It does not have a direct effect on the visual system, and therefore, it is not associated with the green-yellow halo symptom.
The most common side effect of enalapril is a dry cough. This cough is thought to be caused by an increase in bradykinin levels, which can lead to the constriction of bronchial smooth muscle.
Choice D rationale:
Furosemide (Lasix) is a loop diuretic that primarily affects the kidneys and fluid balance. It does not have a direct effect on the visual system, and therefore, it is not associated with the green-yellow halo symptom.
Toxicity with furosemide manifests as extensions of its diuretic activity. Signs and symptoms of overdose or toxicity include:
Dehydration
Reduced blood volume
Electrolyte imbalances, particularly hypokalemia (low potassium levels) Choice C rationale:
Digoxin (Lanoxin) is a cardiac glycoside that affects the heart's electrical activity and muscle contractions. It has a narrow therapeutic index, meaning that there is a small difference between the therapeutic dose and the toxic dose.
One of the most characteristic signs of digoxin toxicity is a visual disturbance known as the "green-yellow halo sign." This symptom is thought to be caused by the inhibition of an enzyme in the retina called Na+/K+-ATPase.
Other common signs and symptoms of digoxin toxicity include:
Nausea and vomiting
Anorexia (loss of appetite)
Fatigue
Headache
Confusion
Arrhythmias (irregular heartbeats)
A nurse is caring for two patients who had a coronary artery stent placed yesterday.
What medication should the nurse expect to administer based on the patients’ daily medication administration record?
Explanation
Choice A rationale:
Clopidogrel is an antiplatelet medication that is essential for preventing blood clots from forming within coronary artery stents. It works by inhibiting the binding of adenosine diphosphate (ADP) to its receptors on platelets, thereby reducing platelet aggregation. This is crucial following stent placement because the stent itself can act as a trigger for platelet activation and clotting. By suppressing platelet function, clopidogrel helps to maintain blood flow through the stented artery and reduces the risk of stent thrombosis, a potentially life-threatening complication.
Here's a detailed explanation of why the other choices are incorrect:
Choice B: Ibuprofen
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that is primarily used to treat pain and inflammation.
It does not have significant antiplatelet effects and is not typically used for the prevention of stent thrombosis.
While it might be prescribed for pain management after stent placement, it would not be the primary medication expected on the daily medication administration record for this purpose.
Choice C: Dipyridamole
Dipyridamole is an antiplatelet medication, but it is not as potent as clopidogrel and is not considered the first-line agent for preventing stent thrombosis.
It might be used in combination with clopidogrel in certain cases, but it would not be the sole antiplatelet medication expected on the daily medication administration record.
Choice D: Acetaminophen
Acetaminophen is a pain reliever and fever reducer.
It does not have any antiplatelet effects and would not be used to prevent stent thrombosis.
It might be prescribed for pain or fever after stent placement, but it would not be the primary medication expected on the daily medication administration record for this purpose.
A patient with sinus bradycardia has a heart rate of 45 and a blood pressure of 82/60 and is reporting dizziness.
What intervention should the nurse anticipate will be ordered?
Explanation
Choice A rationale:
Digoxin is a medication that slows the heart rate. It would be contraindicated in this patient because they are already bradycardic.
Administering digoxin could further slow the heart rate and worsen the patient's symptoms.
Additionally, digoxin can have a negative inotropic effect, which could further compromise the patient's hemodynamic status. Choice B rationale:
While it is important to continue to monitor the patient, this is not an intervention that will address the patient's bradycardia and hypotension.
The patient is already symptomatic, and their heart rate and blood pressure are likely to continue to decline without intervention. Choice C rationale:
Defibrillation is used to treat life-threatening arrhythmias such as ventricular fibrillation and pulseless ventricular tachycardia.
It is not indicated for sinus bradycardia.
Choice D rationale:
Transcutaneous pacing is a non-invasive method of pacing the heart.
It can be used to temporarily increase the heart rate in patients with symptomatic bradycardia.
This is the most appropriate intervention for this patient because it will address the underlying problem of bradycardia and improve the patient's hemodynamic status.
Please identify the following rhythm:
Explanation
Choice A rationale:
Ventricular Fibrillation (VF) is a chaotic, disorganized rhythm that arises from the ventricles of the heart. It is characterized by the absence of distinct QRS complexes, P waves, and T waves on the ECG. Instead, the ECG shows a rapid, irregular pattern of waveforms that vary in amplitude and frequency. This indicates that the electrical activity in the ventricles is completely disorganized, preventing effective contraction of the heart muscle and leading to a lack of cardiac output. VF is a lifethreatening emergency that requires immediate defibrillation to restore a normal heart rhythm.
Key features of VF on ECG:
Absence of distinct QRS complexes
Absence of P waves
Absence of T waves
Rapid, irregular pattern of waveforms Varying amplitude and frequency of waveforms Pathophysiology of VF:
VF occurs when multiple ectopic foci in the ventricles fire rapidly and asynchronously, leading to disorganized electrical activity. This can be caused by a variety of factors, including:
Acute myocardial infarction (heart attack)
Myocardial ischemia (reduced blood flow to the heart muscle)
Electrolyte imbalances (such as low potassium or magnesium)
Electrical shock
Certain medications
Drug overdoses
Clinical manifestations of VF:
Loss of consciousness
Absence of pulse
Apnea (absence of breathing)
Cardiac arrest
Treatment of VF:
Immediate defibrillation
CPR
Advanced cardiac life support (ACLS) medications Choice B rationale:
Atrial Flutter is a rapid, regular atrial rhythm that is characterized by a sawtooth pattern on the ECG. It is caused by a reentrant circuit in the atria, which leads to a rapid firing of atrial impulses. Atrial flutter can sometimes be difficult to distinguish from VF on ECG, but it is important to differentiate between the two rhythms because the treatment is different.
Choice C rationale:
Ventricular Tachycardia (VT) is a rapid, regular ventricular rhythm that is characterized by wide QRS complexes on the ECG. It is caused by an abnormal focus of electrical activity in the ventricles. VT can be life-threatening, but it is not as immediately life-threatening as VF.
Choice D rationale:
Asystole is the absence of any electrical activity in the heart. It is a form of cardiac arrest and is characterized by a flat line on the ECG. Asystole is a life-threatening emergency that requires immediate CPR and advanced cardiac life support (ACLS) measures.
A B-type natriuretic peptide (BNP) sample has been drawn from an older adult patient who has been experiencing vital fatigue and shortness of breath.
What diagnosis will this test allow the care team to investigate?
Explanation
Choice A rationale:
B-type natriuretic peptide (BNP) is a hormone produced primarily by the ventricles of the heart in response to stretching of the heart muscle fibers. It plays a crucial role in regulating blood volume and pressure by promoting the excretion of sodium and water by the kidneys. Elevated levels of BNP in the blood are strongly suggestive of heart failure, as the heart muscle is working harder to pump blood, leading to increased BNP production.
Key points supporting A as the correct answer:
BNP is a highly sensitive and specific marker for heart failure. Studies have demonstrated its accuracy in diagnosing heart failure, even in early stages when symptoms may be subtle.
The patient's clinical presentation aligns with heart failure. Vital fatigue and shortness of breath are both classic symptoms of heart failure, resulting from the heart's inability to meet the body's demands for oxygenated blood.
Other choices are less likely based on the information provided. Pleurisy (inflammation of the lining of the lungs), cardiomyopathy (disease of the heart muscle), and valve dysfunction can all cause shortness of breath, but they would not typically lead to elevated BNP levels unless heart failure is also present.
Additional considerations:
BNP levels can be influenced by factors other than heart failure, such as age, kidney function, and certain medications. However, in the context of a patient with typical heart failure symptoms, an elevated BNP level strongly supports the diagnosis.
BNP testing is often used to guide treatment decisions in patients with heart failure. Serial BNP measurements can help assess the effectiveness of therapy and monitor for disease progression.
A patient who is a candidate for an implantable cardioverter defibrillator (ICD) asks the nurse about the purpose of this device.
What would be the nurse’s best response?
Explanation
Choice A rationale:
While an ICD can sometimes be used to treat bradycardia (an abnormally slow heart rate), this is not its primary function.
Pacemakers are more commonly used to manage bradycardia.
They work by continuously monitoring the heart's rhythm and delivering electrical impulses to the heart muscle when needed to maintain a normal heart rate.
Choice B rationale:
Atrial fibrillation (AFib) is a type of arrhythmia that causes the upper chambers of the heart (atria) to beat irregularly and rapidly.
ICDs are not typically used to treat AFib.
Instead, medications such as beta-blockers or calcium channel blockers are often used to control the heart rate and rhythm in patients with AFib. In some cases, a procedure called ablation may be used to destroy the areas of the heart that are causing the abnormal electrical signals.
Choice C rationale:
The primary purpose of an ICD is to detect and treat ventricular arrhythmias, which are potentially life-threatening rhythm disturbances that originate in the lower chambers of the heart (ventricles).
Ventricular fibrillation (VF) is a chaotic, rapid rhythm that prevents the heart from pumping blood effectively.
Ventricular tachycardia (VT) is a very fast heart rhythm that can also lead to cardiac arrest.
ICDs can deliver electrical shocks to the heart to restore a normal rhythm when these dangerous arrhythmias occur.
This can prevent sudden cardiac death (SCD).
Choice D rationale:
While an ICD can deliver a shock to the heart in the event of a heart attack, this is not its primary purpose.
It's important to note that an ICD cannot prevent a heart attack from happening; it can only treat the life-threatening arrhythmias that may result from a heart attack.
Sign Up or Login to view all the 52 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

