Newborn Nutrition > Maternal & Newborn
Exam Review
More Questions
Total Questions : 22
Showing 22 questions, Sign in for moreA nurse is caring for a newborn who has jaundice and is receiving phototherapy.
Which of the following actions should the nurse take?
Explanation
Cover the newborn’s eyes with a mask or shield.This is because phototherapy can cause eye damage and the mask or shield protects the newborn’s eyes from the light.
Some additional explanations are:
• Choice A is wrong because increasing fluid intake by 25% to prevent dehydration is not necessary for a newborn receiving phototherapy.The newborn should be fed on demand or according to a regular schedule and monitored for signs of dehydration such as poor skin turgor, dry mucous membranes, sunken fontanels, and decreased urine output.
• Choice C is wrong because applying lotion or oil to the newborn’s skin to prevent drying is not recommended for a newborn receiving phototherapy.Lotion or oil can increase the absorption of light and cause skin burns.
• Choice D is wrong because turning off the phototherapy lights during feedings is not advised for a newborn receiving phototherapy.The lights should be on continuously to maximize the effectiveness of the treatment and reduce the duration of exposure.
A nurse is preparing to bottle feed a newborn who is formula fed.
Which of the following actions should the nurse take?
Explanation
Hold the newborn in a semi-upright position during feeding.This prevents the formula from flowing back into the baby’s ears and causing infections.It also helps the baby swallow less air and reduces the risk of choking.
Choice A is wrong because warming the formula in a microwave oven can create hot spots that can burn the baby’s mouth.The formula should be warmed by running it under warm tap water or placing it in a bowl of warm water.
Choice B is wrong because discarding any unused formula after 2 hours at room temperature is too long.Bacteria can grow rapidly in warm milk that is left sitting out and unused.The formula should be discarded after one hour at room temperature or within 24 hours if refrigerated.
Choice D is wrong because burping the newborn after finishing each ounce of formula is not necessary.Burping can interrupt the feeding and make the baby lose interest in finishing the bottle.The baby should be burped only when they show signs of discomfort or after finishing the feeding.
Normal ranges for formula intake vary depending on the baby’s age, weight and appetite.In general, newborn babies need around 150 to 200 ml per kilo of their weight a day until they’re 6 months old.The baby should be fed when they show signs of hunger, such as rooting, sucking or crying, and not forced to finish the bottle if they are full.
A nurse is reviewing laboratory results for a newborn who is breastfed.
Which of the following findings indicates adequate nutrition?
Explanation
Hemoglobin level of 11 g/dL.This is within the normal range for a newborn, which is 13.4-19.9 g/dL for the first month.
Hemoglobin is the oxygen-carrying protein in red blood cells.
Choice B is wrong because serum calcium level of 8 mg/dL is below the normal range for a newborn, which is 8.5-10.6 mg/dL for the first month.
Calcium is important for bone health and muscle function.
Choice C is wrong because serum bilirubin level of 15 mg/dL is above the normal range for a newborn, which is less than 12 mg/dL for the first week.
Bilirubin is a waste product from the breakdown of red blood cells.
High levels can cause jaundice, a yellowing of the skin and eyes.
Choice D is wrong because serum sodium level of 130 mEq/L is below the normal range for a newborn, which is 135-145 mEq/L.
Sodium is an electrolyte that helps regulate fluid balance and nerve impulses.
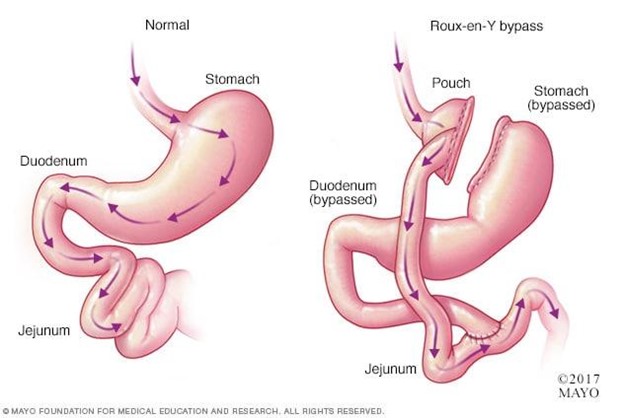
A nurse is providing teaching to a client who has dumping syndrome due to gastric bypass surgery.
Which of the following dietary modifications should the nurse recommend?
Explanation
Eat small, frequent meals throughout the day.This will help prevent dumping syndrome, which is a condition that occurs when food moves too fast from the stomach to the duodenum, causing symptoms such as abdominal cramps, diarrhea, nausea, vomiting, flushing, dizziness and rapid heart rate.Eating small, frequent meals will reduce the amount of food that enters the small intestine at once and slow down gastric emptying.
Choice B is wrong because drinking fluids with meals rather than between meals will increase the volume of food that enters the small intestine and worsen dumping syndrome symptoms.Fluids should be consumed at least 30 minutes after a meal.
Choice C is wrong because increasing intake of simple carbohydrates such as fruit juice will cause a rapid rise and fall of blood sugar levels, leading to late dumping syndrome symptoms such as sweating, hunger, low blood sugar, fatigue, dizziness and weakness.Simple carbohydrates should be avoided and replaced with complex carbohydrates such as whole grains, fruits and vegetables.
Choice D is wrong because avoiding foods that are high in fat and protein will not help prevent dumping syndrome.In fact, fat and protein can slow down gastric emptying and stabilize blood sugar levels.A moderate amount of fat and protein should be included in each meal.However, too much fat at one time can have the opposite effect and trigger dumping syndrome symptoms.
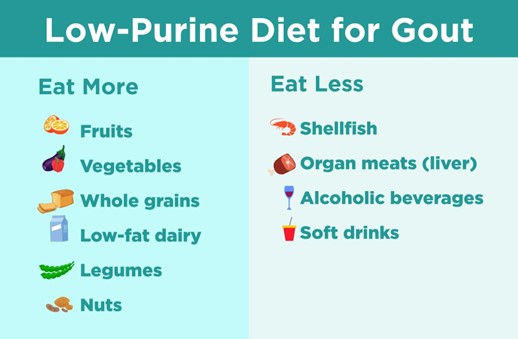
A nurse is evaluating a client’s understanding of a low-purine diet for gout management.
Which of the following food choices by the client indicates an understanding of the teaching?
Explanation
Grilled cheese sandwich with tomato soup.This food choice indicates an understanding of the teaching because it is low in purines, which are chemicals that break down into uric acid and can trigger gout attacks.
Some additional information for the response are:
• Choice A.Liver and onions with mashed potatoes is wrong because liver is an organ meat that is high in purines and should be avoided by people with gout.
• Choice C.Roast beef with green beans and rice is wrong because roast beef is a red meat that is high in purines and should be limited by people with gout.
• Choice D.Sardines on whole wheat crackers with cheese is wrong because sardines are a type of oily fish that is high in purines and should be avoided by people with gout.
• A low-purine diet for gout management should include fruits, vegetables, whole grains, legumes, nuts, and low-fat dairy products.It should also limit sugar, alcohol, and meat consumption.
A nurse is assisting a postpartum client who is breastfeeding her newborn for the first time 2 hr after birth.
Which of the following actions should the nurse take? (Select all that apply.)
Explanation
The nurse should assess for proper latch-on technique and encourage skin-to-skin contact between mother and infant.
These actions promote successful breastfeeding and bonding.
Choice C is wrong because limiting feeding time to 10 min per breast can interfere with the infant’s intake of hindmilk, which is rich in fat and calories.The infant should be allowed to nurse until satisfied, which may take longer than 10 min per breast.
Choice D is wrong because instructing the client to offer both breasts at each feeding can lead to nipple soreness and engorgement.The client should offer one breast until it is emptied, then switch to the other breast if the infant is still hungry.
Choice E is wrong because advising the client to feed the infant every 2 to 3 hr can disrupt the infant’s natural feeding cues and rhythms.The client should feed the infant on demand, which may be more or less frequent than every 2 to 3 hr.
A nurse is reviewing discharge instructions with a postpartum client who plans to breastfeed her newborn exclusively for at least 6 months.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
I will drink at least eight glasses of water every day.This statement indicates that the client understands the importance of hydration for breast milk production and the prevention of constipation.
Some possible explanations for the other choices are:
• Choice A is wrong because iron supplements are not necessary for breastfeeding mothers unless they have anemia.Iron supplements can also cause constipation and stomach upset in some women.
• Choice C is wrong because dairy products are not harmful for breastfeeding mothers or their infants, unless there is a history of allergy or intolerance.Dairy products can provide calcium, protein and vitamin D for the mother and the infant.
• Choice D is wrong because infants should not be given any solid foods before 6 months of age, according to the American Academy of Pediatrics.Introducing solids too early can interfere with breastfeeding, increase the risk of allergies and infections, and cause choking or aspiration.
A nurse is caring for a newborn who was born at 38 weeks of gestation, weighs 3 kg (6 lb 10 oz), and is receiving formula feedings every 3 hr.
The nurse should expect that at each feeding this newborn will consume how many mL?
Explanation
90 mL.According to the CDC, babies who are only getting infant formula and no breast milk need about2.5 ounces (75 mL) of formula per pound of body weight each day.
A newborn who weighs 3 kg (6 lb 10 oz) would need about15 ounces (450 mL) of formula per day, divided into 8 to 12 feedings.
This means that at each feeding, the newborn would consume about90 mLof formula.
Choice A is wrong because30 mLis too little for a newborn who weighs 3 kg.
This would only provide about10 ounces (300 mL) of formula per day, which is not enough for adequate growth and development.
Choice B is wrong because60 mLis also too little for a newborn who weighs 3 kg.
This would only provide about20 ounces (600 mL) of formula per day, which is still below the recommended amount.
Choice D is wrong because120 mLis too much for a newborn who weighs 3 kg.This would provide about40 ounces (1200 mL) of formula per day, which is more than the maximum amount of32 ouncesthat most babies need before they start solids.
Overfeeding can cause problems such as spitting up, gas, and obesity.
A nurse is assessing a postpartum client who delivered vaginally without complications and has chosen not to breastfeed her newborn infant.
Which of these findings would indicate that lactation suppression has been successful?
Explanation
Breasts are soft without engorgement or leakage.This indicates that lactation suppression has been successful and the woman is not experiencing any discomfort or risk of infection from milk accumulation.
Breasts are firm with mild tenderness or leakage is wrong because it suggests that lactation is still occurring and the woman may need to express some milk for comfort or use other non-pharmacological methods to suppress it.
Breasts are hard with moderate pain or leakage is wrong because it indicates that the woman is suffering from breast engorgement, which can lead to mastitis if not treated.The woman may need pharmacological intervention to suppress lactation and relieve pain.
Breasts are swollen with severe pain or leakage is wrong because it shows that the woman has developed mastitis, which is a bacterial infection of the breast tissue that requires antibiotics and analgesics.The woman may also need to drain the infected breast by expressing milk or using a pump.
Normal ranges for lactation suppression vary depending on the individual and the method used.Generally, lactation suppression can take from a few days to a few weeks.
A nurse is assessing a postpartum client who delivered vaginally without complications and has chosen not to breastfeed her newborn infant.
Which of these findings would indicate that lactation suppression has been successful?
Explanation
Breasts are soft without engorgement or leakage.This indicates that lactation suppression has been successful and the woman is not experiencing any discomfort or risk of infection from milk accumulation.
Breasts are firm with mild tenderness or leakage is wrong because it suggests that lactation is still occurring and the woman may need to express some milk for comfort or use other non-pharmacological methods to suppress it.
Breasts are hard with moderate pain or leakage is wrong because it indicates that the woman is suffering from breast engorgement, which can lead to mastitis if not treated.The woman may need pharmacological intervention to suppress lactation and relieve pain.
Breasts are swollen with severe pain or leakage is wrong because it shows that the woman has developed mastitis, which is a bacterial infection of the breast tissue that requires antibiotics and analgesics.The woman may also need to drain the infected breast by expressing milk or using a pump.
Normal ranges for lactation suppression vary depending on the individual and the method used.Generally, lactation suppression can take from a few days to a few weeks.
A nurse is teaching a group of parents about infant nutrition.
The nurse explains that iron-fortified infant formula is recommended for infants who are not breastfed because:
Explanation
Iron is essential for brain development.Iron helps red blood cells carry oxygen through the body and supports a child’s ability to learn.Iron deficiency can cause anemia, which is when there are not enough red blood cells in the body or the child’s ability to carry oxygen throughout the body is lowered.
Choice B is wrong because iron does not prevent constipation in infants.In fact, iron-fortified formula may cause constipation in some infants.
Choice C is wrong because iron does not enhance immune system function.Iron is important for hemoglobin production, but it does not directly affect the immune system.
Choice D is wrong because iron does not improve skin color and tone.Iron deficiency can cause pale skin, but iron supplementation does not change the natural color or tone of the skin.
A nurse is caring for a newborn who is receiving breast milk and supplemental vitamin D drops daily.
The nurse knows that vitamin D supplementation is necessary for breastfed infants because:
Explanation
Breast milk does not contain enough vitamin D for bone health.Vitamin D is needed to support healthy bone development and to prevent rickets, a condition that causes weak or deformed bones.Breast milk alone does not provide infants with an adequate amount of vitamin D.The Dietary Guidelines for Americans and American Academy of Pediatrics recommend breastfed and partially breastfed infants be supplemented with 400 IU per day of vitamin D beginning in the first few days of life.
Choice B is wrong because breast milk does not interfere with vitamin D absorption from sunlight.However, reducing sun exposure is important for preventing skin cancer, and other factors such as clothing, air pollution, and skin type can also decrease the amount of vitamin D a person can make from sunlight.
Choice C is wrong because breast milk does not increase vitamin D excretion in urine.
Vitamin D is a fat-soluble vitamin that is stored in the body and not easily lost in urine.
Choice D is wrong because breast milk does not inhibit vitamin D synthesis in the liver.Vitamin D is synthesized in the skin from exposure to sunlight, and then activated in the liver and kidneys to its active form.
Breast milk does not affect this process.
A nurse is preparing to administer an oral liquid medication to a 3-month-old infant who is receiving powdered infant formula.
The nurse should:
Explanation
Use an oral syringe to squirt the medication into the side of the mouth.
This is because an oral syringe allows the nurse to measure the exact dose of the medication and deliver it slowly and safely into the infant’s mouth, avoiding choking or aspiration.
The other choices are wrong for the following reasons:
• Choice A) Mixing the medication with formula in a bottle can alter the taste and effectiveness of the medication, and also make it difficult to ensure that the infant receives the full dose.
• Choice C) Placing the medication on a pacifier can cause the infant to spit out the pacifier or the medication, and also increase the risk of infection from contaminated pacifiers.
• Choice D) Dipping a cotton swab in the medication and rubbing it on the gums can irritate the oral mucosa and cause pain or bleeding, and also waste some of the medication on the swab.
A nurse is planning to introduce complementary foods to an infant who is six months old and exclusively breastfed.
Which of the following foods should the nurse recommend as a good source of zinc?
Explanation
Meat is a good source of zinc for infants who are six months old and exclusively breastfed.Zinc is a mineral that is important for immune function, wound healing, and the senses of smell and taste.Children 7 to 24 months need 3 mg of zinc each day.
Choice B is wrong because yogurt is not a good source of zinc for infants.Yogurt is a dairy product that contains some zinc, but not as much as meat.
Choice C is wrong because broccoli is not a good source of zinc for infants.Broccoli is a vegetable that contains very little zinc.
Choice D is wrong because mango is not a good source of zinc for infants.Mango is a fruit that contains almost no zinc.
A nurse is educating a mother about complementary feeding for her infant who is eight months old.
Which of the following statements by the mother indicates an understanding of the teaching?
Explanation
“I will give my baby soft finger foods that he can pick up and eat by himself.” This statement indicates an understanding of the teaching because it shows that the mother knows how to provide appropriate complementary foods for her infant who is eight months old.Complementary feeding, also known as weaning, mixed feeding or introduction of solid foods, should begin for infants by six months of age (26 weeks) but not before 17 weeks.Breast milk or infant formula should continue during the complementary feeding period with amounts gradually reduced as the variety of foods increases.WHO and UNICEF recommend that infants start receiving complementary foods at 6 months of age in addition to breast milk.Initially, they should receive complementary foods 2–3 times a day between 6–8 months and increase to 3–4 times daily between 9–11 months and 12–24 months of age.Complementary foods should be nutritionally adequate, safe, and properly fed.
Choice A is wrong because pureed foods are not suitable for an eight-month-old infant who can handle more textured foods.
Pureed foods are recommended for infants who are just starting complementary feeding at around six
A nurse is reviewing the dietary intake of an infant who is receiving complementary foods and drinks along with breast milk.
Which of the following foods should the nurse instruct the mother to limit or avoid to prevent dental caries?
Explanation
Honey should be limited or avoided to prevent dental caries in infants.
Honey is a type of sugar that can feed the bacteria that cause cavities, especially if it is left on the teeth for a long time.Honey can also contain spores of a bacterium that can cause botulism, a serious illness, in infants.
Choice B is wrong because cheese is not a risk factor for dental caries in infants.Cheese can actually help prevent cavities by stimulating saliva production and neutralizing acids in the mouth.
Choice C is wrong because avocado is not a risk factor for dental caries in infants.Avocado is a healthy fat that does not contain sugars that can feed cavity-causing bacteria.
Choice D is wrong because green leafy vegetables are not a risk factor for dental caries in infants.Green leafy vegetables are rich in vitamins and minerals that can support oral health and general health.
A nurse is promoting exclusive breastfeeding for the first six months of life and continued breastfeeding for up to two years or beyond.
Which of the following benefits of breastfeeding should the nurse include in her education?
Explanation
Breastfeeding provides optimal nutrition and immunological protection for infants.This is because breastmilk contains all the energy and nutrients that the infant needs for the first six months of life, and it also contains antibodies that help protect against many common childhood illnesses.
Choice A is wrong because breastfeeding reduces the risk of infections, allergies, and chronic diseases in infants and children, but this is not the only benefit of breastfeeding.Breastfeeding also has benefits for mothers, such as reducing the risk of breast and ovarian cancers.
Choice B is wrong because breastfeeding enhances maternal-infant bonding and attachment, but this is not the only benefit of breastfeeding.Breastfeeding also has benefits for the environment, such as reducing waste and greenhouse gas emissions.
Choice C is wrong because breastfeeding helps mothers lose weight and prevent postpartum hemorrhage, but this is not the only benefit of breastfeeding.Breastfeeding also has benefits for society, such as reducing health care costs and improving productivity.
A nurse is supporting a mother to continue breastfeeding or formula feeding when she returns to work or school.
Which of the following strategies should the nurse suggest to help the mother maintain her milk supply?
Explanation
The nurse should suggest all of these strategies to help the mother maintain her milk supply when she returns to work or school.
Choice A is correct because pumping or expressing milk at least every 3 to 4 hours during work or school hours stimulates the production of prolactin, the hormone that regulates milk synthesis.
Choice B is correct because storing milk in clean glass or plastic containers with tight-fitting lids in a refrigerator or freezer preserves the quality and safety of the milk.
Choice C is correct because labeling milk containers with the date and time of expression and using them in order of oldest to newest ensures that the milk is used before it spoils.
Choice D is correct because it includes all of the above strategies.
A nurse is referring a mother and her infant to specialized care for severe diseases or complications related to nutrition and feeding.
Which of the following conditions would warrant such a referral?
Explanation
All of these conditions would warrant a referral to specialized care for severe diseases or complications related to nutrition and feeding.
Choice A is wrong because phenylketonuria (PKU) in the infant is a genetic disorder that causes an amino acid called phenylalanine to build up in the body.This can lead to intellectual disability, seizures, and other neurological problems if not treated with a special diet that limits phenylalanine.
Choice B is wrong because gestational diabetes mellitus (GDM) in the mother is a condition where the mother has high blood sugar levels during pregnancy.This can increase the risk of complications for both the mother and the baby, such as preeclampsia, macrosomia, birth injuries, and neonatal hypoglycemia.
Choice C is wrong because cleft lip or palate in the infant is a birth defect where the upper lip or roof of the mouth does not form properly.This can affect the infant’s ability to feed, speak, and breathe, and may require surgery and other interventions.
A nurse is reinforcing teaching about growth and development evaluation to a group of parents of preschoolers.
Which of the following information should the nurse include in the teaching?
Explanation
Growth and development evaluation should be done annually until adulthood, plotted on appropriate growth charts and compared with expected norms for age and sex, and used to identify any deviations from normal or expected patterns of growth and development.
Choice A is wrong because growth and development evaluation should not be done only annually, but also at specific ages recommended by the American Academy of Pediatrics (AAP), such as 9 months, 18 months, 24 months, and 30 months.
Choice B is wrong because growth and development evaluation should not only be plotted on appropriate growth charts and compared with expected norms for age and sex, but also include developmental milestones in playing, learning, speaking, behaving, and moving.
Choice C is wrong because growth and development evaluation should not only be used to identify any deviations from normal or expected patterns of growth and development, but also to monitor the child’s progress and provide early intervention if needed.
A nurse is assessing an 18-month-old toddler’s gross motor development during a well-child visit.
Which of the following actions by the toddler indicates normal development?
Explanation
Runs with a wide stance.This indicates normal gross motor development for an 18-month-old toddler.Gross motor skills are the abilities to use large muscles for movements such as walking, running, jumping, and climbing.
Choice A is wrong because walking up and down stairs with assistance is a skill that most toddlers can do by 24 months.
Choice C is wrong because kicking a ball forward without falling is a skill that most toddlers can do by 24 months.
Choice D is wrong because jumping in place with both feet is a skill that most toddlers can do by 30 months.
A nurse is collecting data from a 3-year-old child during a well-child visit.
Which of the following findings should alert the nurse to a possible developmental delay?
Explanation
The child has frequent temper tantrums.This is because temper tantrums are not a normal part of a 3-year-old child’s development and can indicate emotional or behavioral problems.According to the height and weight chart for children, a 3-year-old child should be able to do the following:
• Speak in three-word sentences
• Copy a circle with a crayon
• Ride a tricycle using pedals
Therefore, choices A, B and C are wrong because they are expected developmental milestones for a 3-year-old child.
A nurse should collect data from the child and the parents to determine the cause and frequency of the temper tantrums and provide appropriate interventions and referrals.
Sign Up or Login to view all the 22 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

