Chemotherapy Agents and Oncology Pharmacology > Pharmacology
Exam Review
More Questions
Total Questions : 14
Showing 14 questions, Sign in for moreA nurse is caring for a client who has lung cancer and is receiving combination chemotherapy with cisplatin and etoposide. Which of the following interventions should the nurse implement to prevent nephrotoxicity from cisplatin?
Explanation
Choice D reason:
These are all interventions that can prevent nephrotoxicity from cisplatin, which is a potent and valuable chemotherapy drug that can cause kidney damage or failure. Nephrotoxicity is one of the most serious and doselimiting adverse effects of cisplatin, which can affect up to 30% of patients. Nephrotoxicity is caused by the accumulation of cisplatin in the renal tubular cells, leading to cell injury, inflammation, and ischemia³.
Choice A reason:
Administering mannitol as prescribed before cisplatin infusion can prevent nephrotoxicity by increasing urine output and reducing the concentration of cisplatin in the kidney. Mannitol is an osmotic diuretic that draws water from the extracellular space into the tubular lumen, thereby increasing urine volume and flow rate. Mannitol can also scavenge free radicals and reduce oxidative stress induced by cisplatin⁴.
Choice B reason:
Monitoring serum creatinine and blood urea nitrogen levels daily can prevent nephrotoxicity by detecting early signs of renal impairment and adjusting the dose of cisplatin accordingly. Serum creatinine and blood urea nitrogen are markers of kidney function that reflect the glomerular filtration rate (GFR). An increase in these levels indicates a decrease in GFR and a loss of kidney function. The dose of cisplatin should be reduced or withheld if serum creatinine or blood urea nitrogen levels rise above a certain threshold⁴.
Choice C reason:
Encouraging fluid intake of at least 3 L per day during treatment can prevent nephrotoxicity by maintaining adequate hydration and preventing dehydration. Hydration is essential for preventing cisplatininduced renal toxicity, as it dilutes the concentration of cisplatin in the kidney and enhances its elimination. Dehydration can increase the risk of nephrotoxicity by reducing renal blood flow and causing tubular obstruction by uric acid crystals. Fluid intake can be oral or intravenous, depending on the patient's condition⁴.
A nurse is caring for a client who has breast cancer and is receiving doxorubicin, cyclophosphamide, and paclitaxel as adjuvant chemotherapy. The nurse should monitor the client for cardiotoxicity from doxorubicin by assessing for which of the following signs and symptoms?
Explanation
Choice A reason:
These are signs of cardiotoxicity from doxorubicin, which is a potent anthracycline chemotherapy drug that can cause damage to the heart muscle or valves. Cardiotoxicity is one of the most serious and doselimiting adverse effects of doxorubicin, which can affect up to 20% of patients. Cardiotoxicity can manifest as acute or chronic heart failure, arrhythmias, or myocardial infarction. The nurse should monitor the client for chest pain, dyspnea, palpitations, and edema, which indicate reduced cardiac function and fluid overload. The nurse should also measure the client's blood pressure, heart rate, oxygen saturation, and electrocardiogram (ECG) regularly³.
Choice B reason:
These are common side effects of chemotherapy, but they are not directly related to cardiotoxicity from doxorubicin. Nausea, vomiting, diarrhea, and abdominal pain can occur due to the effects of chemotherapy on the digestive system or the brain. They can also cause dehydration and electrolyte imbalance, which can affect the heart function. The nurse should assess the client for nausea, vomiting, diarrhea, and abdominal pain and provide antiemetics, fluids, and electrolytes as ordered.
Choice C reason:
These are not common signs of cardiotoxicity from doxorubicin, but rather of peripheral neuropathy from paclitaxel, which is another chemotherapy drug that is used in combination with doxorubicin and cyclophosphamide for breast cancer. Peripheral neuropathy is the damage to the nerves in the hands and feet, which can cause numbness, tingling, burning, or pain. Peripheral neuropathy can affect the client's quality of life and ability to perform daily activities. The nurse should assess the client for peripheral neuropathy and provide pain relief and supportive care as needed.
Choice D reason:
These are not common signs of cardiotoxicity from doxorubicin, but rather of infection from bone marrow suppression caused by chemotherapy. Bone marrow suppression is the decrease in the production of blood cells, such as red blood cells, white blood cells, and platelets. This can cause anemia, increased risk of infection, and bleeding problems. Infection can occur when the white blood cell count is low and the immune system is weakened. The nurse should monitor the client for fever, chills, sore throat, and mouth ulcers, which indicate infection and report them to the provider immediately.
A nurse is caring for a client who has lymphoma and is receiving vincristine, prednisone, and rituximab as induction chemotherapy. The nurse should identify that vincristine can cause neurotoxicity and instruct the client to report which of the following manifestations?
Explanation
Choice D reason:
These are manifestations of neurotoxicity from vincristine, which is a chemotherapy drug that belongs to the vinca alkaloids. Vinca alkaloids work by binding to tubulin and inhibiting the formation of microtubules, which are essential for cell division and function. Neurotoxicity is one of the most common and doselimiting adverse effects of vincristine, which can affect up to 80% of patients. Neurotoxicity can manifest as peripheral neuropathy, which is the damage to the nerves in the hands and feet, causing numbness, tingling, burning, or pain. The nurse should monitor the client for peripheral neuropathy and provide pain relief and supportive care as needed³.
Choice A reason:
These are not manifestations of neurotoxicity from vincristine, but rather of paralytic ileus from vincristine. Paralytic ileus is the loss of intestinal motility, causing constipation, urinary retention, and abdominal distension. Paralytic ileus is another common adverse effect of vincristine, which can affect up to 40% of patients. Paralytic ileus is caused by the inhibition of microtubules in the smooth muscle cells of the intestine and bladder, leading to reduced peristalsis and urine flow. The nurse should monitor the client for paralytic ileus and provide laxatives, catheterization, and fluids as ordered⁴.
Choice B reason:
These are not manifestations of neurotoxicity from vincristine, but rather of ototoxicity from cisplatin, which is another chemotherapy drug that is used in combination with vincristine and prednisone for lymphoma. Ototoxicity is the damage to the inner ear or hearing nerve, causing hearing loss, tinnitus, and vertigo. Ototoxicity is one of the most serious and doselimiting adverse effects of cisplatin, which can affect up to 50% of patients. Ototoxicity is caused by the accumulation of cisplatin in the cochlea and vestibular system, leading to oxidative stress and cell death. The nurse should monitor the client for ototoxicity and provide hearing tests and vestibular rehabilitation as needed .
Choice C reason:
These are not manifestations of neurotoxicity from vincristine, but rather of ocular toxicity from rituximab, which is another chemotherapy drug that is used in combination with vincristine and prednisone for lymphoma. Ocular toxicity is the damage to the eyes or vision, causing blurred vision, photophobia, and eye irritation. Ocular toxicity is a rare but serious adverse effect of rituximab, which can affect up to 1% of patients. Ocular toxicity is caused by the infusionrelated reactions or immunemediated reactions induced by rituximab, leading to inflammation and edema in the eyes. The nurse should monitor the client for ocular toxicity and provide eye drops and steroids as ordered .
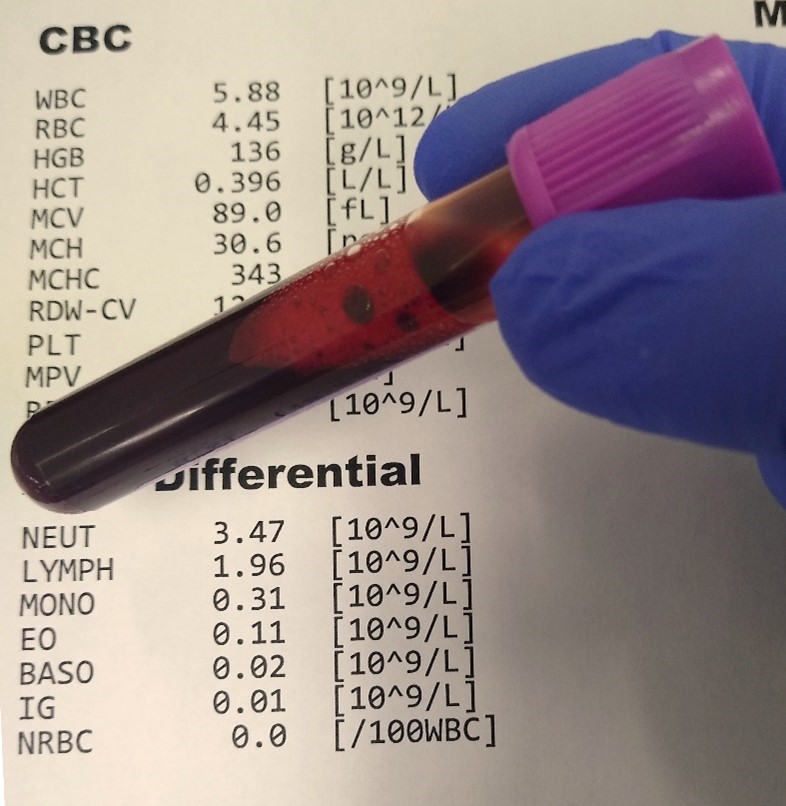
A nurse is caring for a client who has leukemia and is receiving cytarabine, an antimetabolite, as part of chemotherapy. Which of the following laboratory tests should the nurse monitor for adverse effects of this drug?
Explanation
Choice C reason:
This is the laboratory test that the nurse should monitor for adverse effects of cytarabine, which is an antimetabolite chemotherapy drug that works by slowing or stopping the growth of cancer cells. The main adverse effect of cytarabine is bone marrow suppression, which is the decrease in the production of blood cells, such as red blood cells, white blood cells, and platelets. This can cause anemia, increased risk of infection, and bleeding problems. The nurse should monitor the complete blood count and differential, which measure the number and type of blood cells in a sample of blood. The nurse should report any abnormal results to the provider and provide supportive care as ordered³.
Choice A reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of cisplatin, which is another chemotherapy drug that can cause kidney damage or failure. Cisplatin can accumulate in the kidney cells and cause oxidative stress and cell death. The nurse should monitor the serum creatinine and blood urea nitrogen levels, which are markers of kidney function that reflect the glomerular filtration rate (GFR). An increase in these levels indicates a decrease in GFR and a loss of kidney function. The nurse should report any abnormal results to the provider and provide fluids and electrolytes as ordered⁴.
Choice B reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of amphotericin B, which is an antifungal drug that can cause electrolyte imbalance. Amphotericin B can affect the transport of sodium and potassium across cell membranes and cause renal tubular acidosis. The nurse should monitor the serum potassium and magnesium levels, which are important electrolytes for nerve and muscle function. A decrease in these levels can cause muscle weakness, cramps, arrhythmias, and seizures. The nurse should report any abnormal results to the provider and provide supplements as ordered .
Choice D reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of methotrexate, which is another antimetabolite chemotherapy drug that can cause liver damage or failure. Methotrexate can interfere with the metabolism of folate and cause accumulation of toxic metabolites in the liver cells. The nurse should monitor the serum bilirubin and liver enzyme levels, which are markers of liver function that reflect the liver's ability to process bilirubin and other substances. An increase in these levels indicates liver injury or inflammation. The nurse should report any abnormal results to the provider and provide folinic acid as ordered .
A nurse is caring for a client who has ovarian cancer and is receiving vincristine, a natural product, as part of chemotherapy. Which of the following interventions should the nurse implement to prevent constipation from vincristine?
Explanation
Choice C reason:
This is the laboratory test that the nurse should monitor for adverse effects of cytarabine, which is an antimetabolite chemotherapy drug that works by slowing or stopping the growth of cancer cells. The main adverse effect of cytarabine is bone marrow suppression, which is the decrease in the production of blood cells, such as red blood cells, white blood cells, and platelets. This can cause anemia, increased risk of infection, and bleeding problems. The nurse should monitor the complete blood count and differential, which measure the number and type of blood cells in a sample of blood. The nurse should report any abnormal results to the provider and provide supportive care as ordered³.
Choice A reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of cisplatin, which is another chemotherapy drug that can cause kidney damage or failure. Cisplatin can accumulate in the kidney cells and cause oxidative stress and cell death. The nurse should monitor the serum creatinine and blood urea nitrogen levels, which are markers of kidney function that reflect the glomerular filtration rate (GFR). An increase in these levels indicates a decrease in GFR and a loss of kidney function. The nurse should report any abnormal results to the provider and provide fluids and electrolytes as ordered⁴.
Choice B reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of amphotericin B, which is an antifungal drug that can cause electrolyte imbalance. Amphotericin B can affect the transport of sodium and potassium across cell membranes and cause renal tubular acidosis. The nurse should monitor the serum potassium and magnesium levels, which are important electrolytes for nerve and muscle function. A decrease in these levels can cause muscle weakness, cramps, arrhythmias, and seizures. The nurse should report any abnormal results to the provider and provide supplements as ordered .
Choice D reason:
These are not the laboratory tests that the nurse should monitor for adverse effects of cytarabine, but rather of methotrexate, which is another antimetabolite chemotherapy drug that can cause liver damage or failure. Methotrexate can interfere with the metabolism of folate and cause accumulation of toxic metabolites in the liver cells. The nurse should monitor the serum bilirubin and liver enzyme levels, which are markers of liver function that reflect the liver's ability to process bilirubin and other substances. An increase in these levels indicates liver injury or inflammation. The nurse should report any abnormal results to the provider and provide folinic acid as ordered .
A nurse is caring for a client who has colon cancer and is receiving dactinomycin, an antineoplastic antibiotic, as part of chemotherapy. The nurse should identify that dactinomycin can cause which of the following adverse effects? (Select all that apply.)
Explanation
Choice A reason:
Bone marrow suppression is an adverse effect of dactinomycin, which is an antineoplastic antibiotic that works by binding to DNA and inhibiting RNA synthesis. Bone marrow suppression is the decrease in the production of blood cells, such as red blood cells, white blood cells, and platelets. This can cause anemia, increased risk of infection, and bleeding problems. The nurse should monitor the complete blood count and differential, which measure the number and type of blood cells in a sample of blood. The nurse should report any abnormal results to the provider and provide supportive care as ordered³.
Choice B reason:
Skin reactions are an adverse effect of dactinomycin, which can cause inflammation, rash, acne, erythema multiforme, or increased pigmentation of previously irradiated skin. Skin reactions can occur due to the direct toxicity of dactinomycin on the skin cells or due to the hypersensitivity or allergic reactions induced by dactinomycin. The nurse should monitor the skin appearance and texture and report any changes to the provider. The nurse should also provide skin care and topical agents as ordered³.
Choice E reason:
Extravasation injury is an adverse effect of dactinomycin, which can occur when the drug leaks out of the vein into the surrounding tissue during intravenous infusion. Extravasation injury can cause severe pain, swelling, redness, blistering, ulceration, or necrosis of the affected tissue. The nurse should monitor the infusion site and stop the infusion immediately if extravasation occurs. The nurse should also elevate the affected limb and apply cold compresses as ordered. The nurse should consult with the provider for further management of extravasation injury³.
Choice C reason:
Cardiotoxicity is not an adverse effect of dactinomycin, but rather of doxorubicin, which is another antineoplastic antibiotic that can cause damage to the heart muscle or valves. Cardiotoxicity can manifest as acute or chronic heart failure, arrhythmias, or myocardial infarction. The nurse should monitor the blood pressure, heart rate, oxygen saturation, and electrocardiogram (ECG) regularly and report any abnormal findings to the provider .
Choice D reason:
Pulmonary fibrosis is not an adverse effect of dactinomycin, but rather of bleomycin, which is another antineoplastic antibiotic that can cause scarring of the lung tissue. Pulmonary fibrosis can manifest as shortness of breath, coughing, or reduced lung function. The nurse should monitor the respiratory rate, breath sounds, and chest xray regularly and report any abnormal findings to the provider .
A nurse is caring for a client who has breast cancer and is receiving trastuzumab, a monoclonal antibody, as part of targeted therapy. Which of the following assessments should the nurse perform before and during the infusion of this drug?
Explanation
Choice A reason:
Blood pressure and pulse should be monitored before and during the infusion of trastuzumab, as this drug can cause cardiomyopathy and heart failure in some patients. These are serious side effects that can affect the heart's ability to pump blood effectively.
Choice B reason:
Respiratory rate and oxygen saturation should be monitored before and during the infusion of trastuzumab, as this drug can cause infusion reactions and pulmonary toxicity in some patients³. These are serious side effects that can affect the lungs' ability to exchange oxygen and carbon dioxide.
Choice C reason:
Temperature and skin condition should be monitored before and during the infusion of trastuzumab, as this drug can cause fever, chills, rash, and infection in some patients. These are common side effects that can indicate an allergic reaction or an infection.
Choice D reason:
All of the above assessments should be performed before and during the infusion of trastuzumab, as this drug can cause various side effects that can affect the heart, lungs, skin, and immune system of the patient. The nurse should also monitor for other signs and symptoms such as nausea, vomiting, diarrhea, headache, cough, sore throat, etc. The nurse should report any abnormal findings to the doctor and intervene as needed.
A nurse is caring for a client who has chronic myeloid leukemia (CML) and is receiving imatinib, a tyrosine kinase inhibitor, as part of targeted therapy. Which of the following laboratory tests should the nurse monitor for adverse effects of this drug?
Explanation
Choice A reason:
Liver function tests should be monitored for adverse effects of imatinib, as this drug can cause hepatotoxicity and liver failure in some patients³⁴. These are serious side effects that can affect the liver's ability to metabolize drugs and toxins.
Choice B reason:
Serum electrolytes are not directly affected by imatinib, as this drug does not cause significant changes in sodium, potassium, calcium, or magnesium levels³. However, electrolyte imbalances may occur due to other factors such as dehydration, diarrhea, vomiting, or kidney problems.
Choice C reason:
Coagulation studies are not directly affected by imatinib, as this drug does not cause significant changes in prothrombin time, partial thromboplastin time, or international normalized ratio³. However, bleeding disorders may occur due to other factors such as thrombocytopenia, anemia, or vascular damage.
Choice D reason:
Liver function tests are the only laboratory tests that should be monitored for adverse effects of imatinib, as this drug can cause serious liver damage in some patients. The other tests are not directly affected by imatinib, but may be influenced by other factors or conditions. The nurse should also monitor for other signs and symptoms such as nausea, vomiting, diarrhea, rash, edema, fatigue, infection, etc. The nurse should report any abnormal findings to the doctor and intervene as needed.

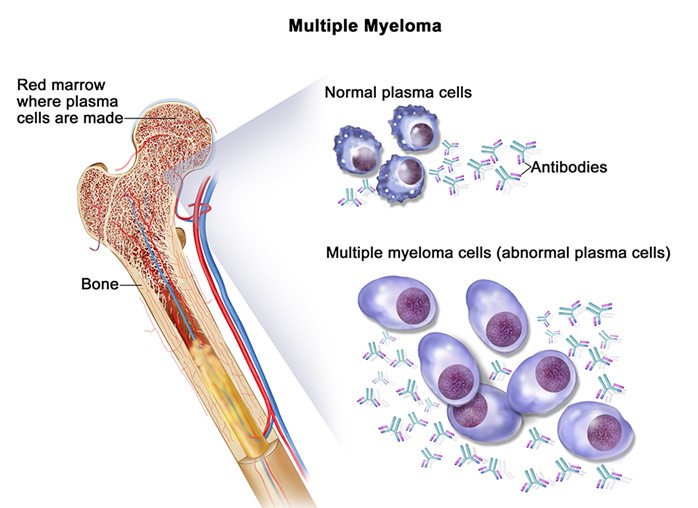
A nurse is caring for a client who has multiple myeloma and is receiving thalidomide, an angiogenesis inhibitor, as part of targeted therapy. The nurse should instruct the client to report which of the following adverse effects of this drug? (Select all that apply.)
Explanation
Choice A reason:
Numbness, tingling, or pain in the extremities are signs of peripheral neuropathy, which is a common and serious side effect of thalidomide³. This condition can affect the nerves that control sensation and movement in the arms and legs, and can lead to permanent nerve damage if not treated.
Choice B reason:
Drowsiness, dizziness, or confusion are signs of central nervous system depression, which is a common and serious side effect of thalidomide³. This condition can affect the brain's ability to regulate alertness, cognition, and coordination, and can increase the risk of falls, accidents, and injuries.
Choice C reason:
Constipation, nausea, or vomiting are signs of gastrointestinal distress, which is a common and mild side effect of thalidomide. This condition can affect the digestive system's ability to process food and fluids, and can lead to dehydration, malnutrition, and electrolyte imbalance if not managed.
Choice D reason:
Swelling, redness, or warmth in the legs are not directly related to thalidomide use, but may indicate a deep vein thrombosis (DVT), which is a blood clot that forms in a vein deep in the body. Thalidomide can increase the risk of DVT by affecting the blood's ability to clot normally. A DVT can be lifethreatening if it breaks off and travels to the lungs, causing a pulmonary embolism.
Choice E reason:
Rash, itching, or hives are signs of allergic reaction, which is a rare but serious side effect of thalidomide³. This condition can affect the skin's immune response to the drug, and can lead to severe skin reactions such as StevensJohnson syndrome or toxic epidermal necrolysis if not treated.
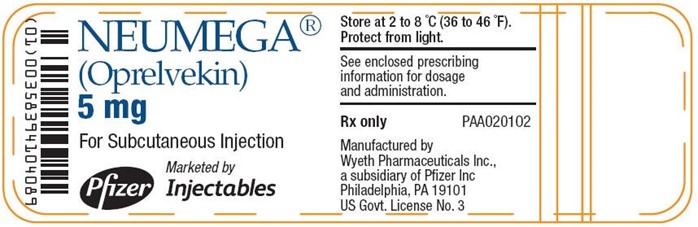
A nurse is caring for a client who has lymphoma and is receiving chemotherapy that causes thrombocytopenia. Which of the following drugs should the nurse administer to the client to stimulate the production of platelets in the bone marrow?
Explanation
Choice A reason:
Epoetin alfa (Epogen) is a drug that stimulates the production of red blood cells in the bone marrow, not platelets⁴. It is used to treat anemia caused by chemotherapy, chronic kidney disease, or other conditions.
Choice B reason:
Filgrastim (Neupogen) is a drug that stimulates the production of white blood cells in the bone marrow, not platelets⁴. It is used to prevent or treat neutropenia caused by chemotherapy, bone marrow transplant, or other conditions.
Choice C reason:
Sargramostim (Leukine) is a drug that stimulates the production of white blood cells and red blood cells in the bone marrow, not platelets⁴. It is used to prevent or treat neutropenia caused by chemotherapy, bone marrow transplant, or other conditions.
Choice D reason:
Oprelvekin (Neumega) is a drug that stimulates the production of platelets in the bone marrow⁴. It is used to prevent or treat thrombocytopenia caused by chemotherapy. It works by mimicking the action of thrombopoietin, a hormone that regulates platelet development.
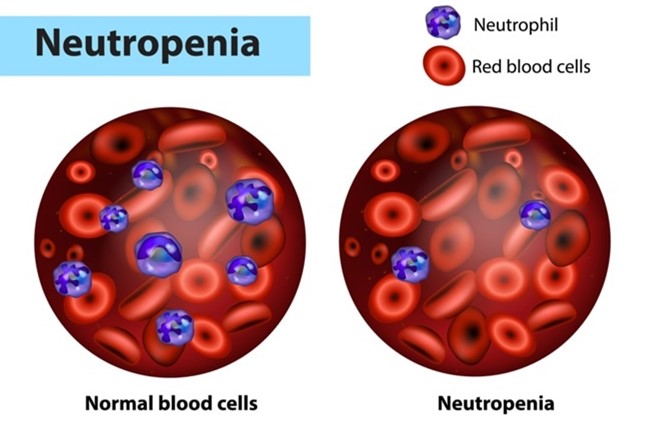
A nurse is caring for a client who has prostate cancer and is receiving chemotherapy that causes anemia and neutropenia. The nurse should identify that which of the following drugs can be used to treat both conditions by stimulating the production of red blood cells and neutrophils in the bone marrow? (Select all that apply.)
Explanation
Choice A reason:
Epoetin alfa (Epogen) is a drug that stimulates the production of red blood cells in the bone marrow, but not neutrophils. It is used to treat anemia caused by chemotherapy, chronic kidney disease, or other conditions.
Choice B reason:
Filgrastim (Neupogen) is a drug that stimulates the production of neutrophils in the bone marrow, but not red blood cells. It is used to prevent or treat neutropenia caused by chemotherapy, bone marrow transplant, or other conditions.
Choice C reason:
Sargramostim (Leukine) is a drug that stimulates the production of both red blood cells and neutrophils in the bone marrow. It is used to prevent or treat anemia and neutropenia caused by chemotherapy, bone marrow transplant, or other conditions.
Choice D reason:
Pegfilgrastim (Neulasta) is a drug that stimulates the production of both red blood cells and neutrophils in the bone marrow⁴. It is a longacting form of filgrastim that works in the same way but can be given less often. It is used to prevent or treat anemia and neutropenia caused by chemotherapy.
Choice E reason:
Darbepoetin alfa (Aranesp) is a drug that stimulates the production of red blood cells in the bone marrow, but not neutrophils. It is a longacting form of epoetin alfa that works in the same way but can be given less often. It is used to treat anemia caused by chemotherapy, chronic kidney disease, or other conditions.
A nurse is caring for a patient who has cervical cancer and is receiving chemotherapy that causes anemia and fatigue. The nurse should instruct the patient to report which of the following manifestations that indicate anemia and fatigue? (Select all that apply.)
Explanation
Choice A reason:
Pallor and weakness are signs of anemia, as they indicate a low level of hemoglobin or red blood cells that carry oxygen to the tissues. Pallor is the loss of color in the skin, especially in the face, nails, and inside of the eyelids. Weakness is the feeling of having less energy or strength than usual.
Choice B reason:
Dizziness and headache are signs of anemia, as they indicate a low level of oxygen in the brain. Dizziness is the feeling of being lightheaded or unsteady. Headache is the pain or discomfort in the head, scalp, or neck.
Choice C reason:
Shortness of breath and tachycardia are signs of anemia, as they indicate a low level of oxygen in the lungs and heart. Shortness of breath is the feeling of not being able to breathe enough or catch your breath. Tachycardia is the abnormally fast or irregular heartbeat.
Choice D reason:
Constipation and abdominal pain are not directly related to anemia or fatigue, but may indicate other conditions such as dehydration, bowel obstruction, or infection. Constipation is the difficulty or infrequency in passing stools. Abdominal pain is the pain or discomfort in the stomach or belly area.
Choice E reason:
Difficulty sleeping and concentrating are not directly related to anemia or fatigue, but may indicate other conditions such as stress, depression, or anxiety. Difficulty sleeping is the trouble falling asleep or staying asleep. Difficulty concentrating is the trouble focusing on tasks or remembering things.
A nurse is caring for a patient who has cervical cancer and is receiving combination chemotherapy with doxorubicin and cyclophosphamide. Which of the following interventions should the nurse implement to prevent cardiotoxicity from doxorubicin?
Explanation
Choice A reason:
Administering dexrazoxane as prescribed before doxorubicin infusion can help prevent cardiotoxicity by inhibiting the formation of DNA doublestrand breaks mediated by topoisomerase II beta, which is a key mechanism of doxorubicininduced cardiac damage³. Dexrazoxane is a chelating agent that binds to iron and prevents the generation of reactive oxygen species that can cause oxidative stress and DNA damage⁴. Dexrazoxane is the only drug approved by the Food and Drug Administration (FDA) for the prevention of doxorubicin cardiotoxicity in patients with metastatic breast cancer who have received a cumulative dose of 300 mg/m2 or more⁵.
Choice B reason:
Monitoring electrocardiogram (ECG) and cardiac enzymes during treatment can help detect cardiotoxicity from doxorubicin, but not prevent it. ECG can show changes such as ST segment depression, T wave inversion, arrhythmias, or conduction abnormalities that indicate cardiac ischemia or injury. Cardiac enzymes such as troponin and creatine kinaseMB (CKMB) can show elevation that indicates myocardial damage or necrosis.
Choice C reason:
Assessing for signs and symptoms of heart failure such as dyspnea, edema, and crackles can help diagnose cardiotoxicity from doxorubicin, but not prevent it. Dyspnea is the difficulty or discomfort in breathing that indicates reduced cardiac output or pulmonary congestion. Edema is the swelling of the lower extremities or abdomen that indicates fluid retention or rightsided heart failure. Crackles are the abnormal lung sounds that indicate pulmonary edema or leftsided heart failure.
Choice D reason:
Administering dexrazoxane as prescribed before doxorubicin infusion is the only intervention that can prevent cardiotoxicity from doxorubicin. Monitoring ECG and cardiac enzymes during treatment and assessing for signs and symptoms of heart failure can help detect and treat cardiotoxicity, but not prevent it. Other strategies that may help prevent doxorubicin cardiotoxicity include limiting the cumulative dose of doxorubicin to less than 450 to 550 mg/m2, administering the drug as an infusion rather than an injection, using a liposomal formulation of doxorubicin, and using other agents with antioxidant or antiinflammatory properties⁴.
A nurse is caring for a patient who has prostate cancer and is receiving combination chemotherapy with docetaxel and prednisone. The nurse should instruct the patient to report which of the following adverse effects that indicate peripheral neuropathy? (Select all that apply.)
No explanation
Sign Up or Login to view all the 14 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

