Umbilical cord prolapse > Maternal & Newborn
Exam Review
More questions on this topic
Total Questions : 15
Showing 15 questions, Sign in for moreA patient’s umbilical cord prolapses during labor.
The nurse should place her in which position? (Select all that apply.).
Explanation
The correct answer is choice A and B. The nurse should place the patient in knee-chest or Trendelenburg position to relieve the pressure of the fetal presenting part on the prolapsed cord and improve fetal oxygenation.These positions also allow gravity to help keep the cord in the uterus and prevent further descent.
Choice C is wrong because supine position can worsen cord compression and compromise fetal blood flow.Choice D is wrong because lithotomy position can also increase cord descent and reduce fetal perfusion.Choice E is wrong because Sims position can cause cord prolapse if the membranes are intact or rupture spontaneously.
Normal ranges for fetal heart rate are 110 to 160 beats per minute.Cord prolapse can cause fetal bradycardia with decelerations during contractions due to cord compression.
This is a sign of fetal distress and requires immediate intervention.
The nurse suspects umbilical cord prolapse in a patient whose membranes have just ruptured because she notes which assessment finding?
Explanation
The correct answer is choice D. A loop of umbilical cord protruding from her vagina.This is a sign of umbilical cord prolapse, which is a medical emergency that occurs when the cord slips past the fetal presenting part and becomes compressed, reducing blood flow and oxygen to the fetus.The nurse should immediately call for help, place the woman in a knee-chest or Trendelenburg position, insert two fingers into the vagina and lift the presenting part off the cord, cover the cord with sterile saline-soaked gauze, administer oxygen, and prepare for an emergency cesarean delivery.
Choice A is wrong because a sudden increase in fetal heart rate variability is not a specific sign of cord prolapse.It may indicate fetal well-being or distress depending on the pattern and duration of the variability.
Choice B is wrong because a large amount of clear amniotic fluid is not a sign of cord prolapse.It may indicate rupture of membranes, which is a risk factor for cord prolapse if the presenting part is not engaged.
Choice C is wrong because a change in fetal heart rate from 140 to 90 bpm is not a sign of cord prolapse.It may indicate fetal bradycardia, which can have many causes such as hypoxia, acidosis, medication effects, or fetal sleep cycle.
The nurse recognizes that which fetal presentation increases a patient’s risk for umbilical cord prolapse? (Select all that apply).
Explanation
The correct answer is choice B, C, D and E.These are all fetal presentations that increase a patient’s risk for umbilical cord prolapse.Umbilical cord prolapse is when the umbilical cord comes out of the uterus with or before the presenting part of the baby.This can cause fetal hypoxia and brain damage due to cord compression.
Choice A is wrong because vertex presentation is the most common and normal fetal position, where the head is down and fully flexed.
This does not increase the risk of cord prolapse.
Normal ranges for fetal presentation are:
• Vertex: 95% of term deliveries.
• Breech: 3% to 4% of term deliveries.
• Transverse lie: 0.5% of term deliveries.
• Face: 0.2% of term deliveries.
• Brow: 0.1% of term deliveries.
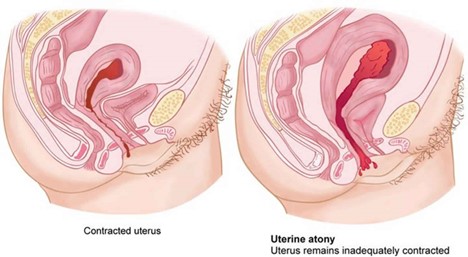
A nurse is caring for a client who has just delivered her second twin vaginally and notes that there is excessive bleeding from her vagina and that her uterus feels boggy on palpation.
The nurse should suspect which of the following complications?
Explanation
The correct answer is choice A. Uterine atony.
Uterine atony is the failure of the uterus to contract and retract after delivery, which can lead to excessive bleeding and hemorrhage.A boggy uterus on palpation is a sign of uterine atony.
Choice B. Uterine inversion is wrong because it is a rare complication in which the uterus turns inside out and protrudes through the cervix.It usually causes severe pain, shock, and hemorrhage.
Choice C. Uterine rupture is wrong because it is a life-threatening emergency in which the uterus tears open along the scar line of a previous cesarean delivery or other uterine surgery.It usually causes severe abdominal pain, fetal distress, and maternal hypovolemic shock.
Choice D. Uterine infection is wrong because it is an inflammation of the endometrium (the lining of the uterus) caused by bacteria.It usually causes fever, foul-smelling lochia, and lower abdominal tenderness.
Normal ranges for postpartum bleeding are about 500 ml for vaginal delivery and 1000 ml for cesarean delivery.The uterus should feel firm and midline at or below the umbilicus after delivery.
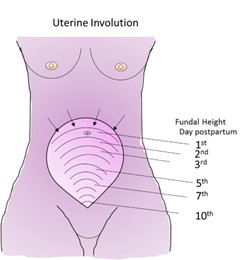
A nurse is assessing a client who had a vaginal delivery and notes that her fundus is firm, midline, and 2 cm below the umbilicus.
The nurse should document this finding as which of the following?
Explanation
The correct answer is choice A. Normal involution.
This means that the uterus is returning to its pre-pregnancy size and position after delivery.
The fundus is the upper part of the uterus and it should be firm, midline, and gradually descend into the pelvis.A fundus that is 2 cm below the umbilicus at 4 hours postpartum is within the normal range.
Choice B. Subinvolution is wrong because it refers to a delayed or incomplete involution of the uterus.
This can result in prolonged bleeding, infection, or retained placental fragments.A fundus that is above the umbilicus, boggy, or displaced to one side may indicate subinvolution.
Choice C. Retained placenta is wrong because it means that some or all of the placenta remains in the uterus after delivery.
This can cause heavy bleeding, infection, or uterine atony.A fundus that is high, soft, or tender may indicate retained placenta.
Choice D. Endometritis is wrong because it means that the lining of the uterus is inflamed due to infection.
This can cause fever, foul-smelling lochia, pelvic pain, or uterine tenderness.A fundus that is enlarged, tender, or malodorous may indicate endometritis.
Normal ranges for fundal height after delivery are:
• Immediately after delivery:
A nurse is providing discharge teaching to a client who had a cesarean delivery due to cord prolapse.
Which of the following instructions should the nurse include in the teaching?
Explanation
The correct answer is choiceA.
The nurse should instruct the client to avoid lifting anything heavier than the newborn for 6 weeks.This is because lifting heavy objects can strain the abdominal muscles and the incision site, and increase the risk of bleeding and infection.
ChoiceBis wrong because the nurse should advise the client to wait at least 4 to 6 weeks before resuming sexual intercourse.This is to allow the incision to heal and prevent infection and discomfort.
ChoiceCis wrong because the nurse should not recommend ibuprofen for pain relief as it can interfere with blood clotting and increase bleeding.The nurse should suggest acetaminophen or a prescribed analgesic instead.
ChoiceDis wrong because the nurse should not tell the client to report any foul-smelling vaginal discharge to the provider.
The client should expect some vaginal discharge (lochia) for several weeks after a cesarean delivery, which may have a mild odor.However, the nurse should instruct the client to report signs of infection such as fever, chills, redness, swelling, or increased pain at the incision site.
A patient’s umbilical cord prolapses during labor induction with oxytocin infusion.
Which action by the nurse takes priority?
Explanation
The correct answer is choice C. Apply pressure to presenting part with hand.
This is because cord prolapse is an emergency situation that requires immediate delivery to save the fetus.Applying pressure to the presenting part with hand can help relieve the compression of the cord and maintain fetal oxygenation until delivery.
Choice A is wrong because stopping oxytocin infusion will not prevent cord compression or fetal hypoxia.Oxytocin may be stopped after applying pressure to the presenting part and notifying the physician.
Choice B is wrong because placing the patient in knee-chest position may not be effective in relieving cord compression.
It may also be uncomfortable and difficult for the patient to maintain.A better position would be Trendelenburg or modified Sims.
Choice D is wrong because administering oxygen via non-rebreather mask is not a priority action.Oxygen may be given after applying pressure to the presenting part and notifying the physician, but it will not improve fetal oxygenation if the cord is compressed.

Which statement by a pregnant client indicates understanding of measures to prevent umbilical cord prolapse?
Explanation
The correct answer is choice C.“I will come to the hospital as soon as my water breaks.” This statement indicates understanding of measures to prevent umbilical cord prolapse, which is a complication that occurs when the umbilical cord drops out of the cervix before the baby during labor.This can cut off the baby’s blood and oxygen supply and cause permanent brain damage.Immediate delivery by C-section is usually necessary.
Choice A is wrong because squatting or sitting on hard surfaces does not increase the risk of umbilical cord prolapse.
Choice B is wrong because decreased fetal movement is not a sign of umbilical cord prolapse, but rather a sign of fetal distress that may have other causes.
Choice D is wrong because drinking plenty of fluids and resting on the left side are general measures to promote maternal and fetal well-being, but they do not prevent umbilical cord prolapse.
Some of the risk factors for umbilical cord prolapse include premature rupture of membranes, multiple pregnancy, breech presentation, excessive amniotic fluid, abnormal length of the umbilical cord and premature delivery.Some of the symptoms of umbilical cord prolapse include visible or palpable cord after water breaks, fetal heart rate abnormalities and maternal feeling of something coming out of the vagina.Umbilical cord prolapse can be diagnosed by physical examination, ultrasound or fetal heart rate monitoring.
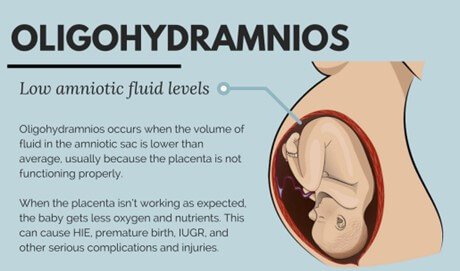
Which condition increases the risk of occult umbilical cord prolapse?
Explanation
This is a condition where there is too little amniotic fluid around the fetus.This increases the risk of umbilical cord prolapse because the cord can easily slip past the presenting part of the fetus and into the cervix or vagina.
This can cause fetal hypoxia and distress due to compression or occlusion of the cord.
Choice A. Transverse lie is wrong because this is a condition where the fetus lies horizontally across the uterus.This can increase the risk of cord prolapse if the membranes rupture and the cord descends alongside or before the fetus.
Choice B. Macrosomia is wrong because this is a condition where the fetus is larger than average.This can decrease the risk of cord prolapse because the presenting part of the fetus is more likely to fill the pelvis and prevent the cord from slipping past.
Choice D. Placenta previa is wrong because this is a condition where the placenta covers part or all of the cervix.This can increase the risk of bleeding during labor, but not necessarily cord prolapse.
Which of these clients is at greatest risk for umbilical cord prolapse?
Explanation
The correct answer is choice C. A client who has oligohydramnios.
Oligohydramnios is a condition where there is too little amniotic fluid around the fetus.This can cause the umbilical cord to slip down into the cervix or vagina before the baby, resulting in cord prolapse.
Cord prolapse can cut off the blood and oxygen supply to the baby and cause fetal distress or death.
Choice A is wrong because a client who is pregnant with twins is not at greater risk for cord prolapse unless there is also malpresentation of the fetuses, such as breech or transverse lie.
Choice B is wrong because a client who has gestational hypertension is not at greater risk for cord prolapse unless there is also polyhydramnios, which is excessive amniotic fluid around the fetus.
Choice D is wrong because a client who has placenta previa is not at greater risk for cord prolapse unless there is also artificial rupture of membranes by doctors.
What is the most common cause of variable decelerations in fetal heart rate?
Explanation
The correct answer is choice B. Umbilical cord compression.Variable decelerations are the most common type of fetal deceleration and they are caused by compression of the umbilical cord.They vary in shape, duration, and intensity and may not have a constant relationship with uterine contractions.
Choice A is wrong because uteroplacental insufficiency is the cause of late decelerations, not variable decelerations.Uteroplacental insufficiency is a decrease in the blood flow to the placenta that reduces the amount of oxygen and nutrients transferred to the fetus.
Choice C is wrong because maternal hypotension is one of the possible causes of late decelerations, not variable decelerations.Maternal hypotension can reduce the uteroplacental blood flow and cause fetal hypoxia.
Choice D is wrong because fetal head compression is the cause of early decelerations, not variable decelerations.Early decelerations are benign and uniform in shape and they occur when the fetal head is pressed against the cervix during a uterine contraction.
What is an occult cord prolapse?
Explanation
The correct answer is choice B. The cord is hidden, often next to but not in front of the fetal head.This is called anoccult cord prolapseand it occurs when the umbilical cord descends alongside–but not past–the presenting part of the baby.Occult cords can occur with ruptured or intact membranes.They can cause hypoxia, brain injury, and permanent disability in a baby, so medical personnel must address them rapidly and appropriately.
Choice A is wrong because it describes anovert cord prolapse, which means that the cord slips down into your cervix and vagina ahead of your baby during delivery.This is a medical emergency that can cut off your baby’s blood and oxygen supply during delivery.
Choice C is wrong because it describes avisible cord prolapse, which is a type of overt cord prolapse where the cord is visible or palpable outside of the vagina.This is also a medical emergency that requires immediate delivery.
Choice D is wrong because it describes anuchal cord, which means that the cord is wrapped around the fetal neck or body.This is not a prolapse, but it can cause complications such as reduced blood flow, fetal distress, or umbilical cord strangulation.
A patient’s umbilical cord prolapses during labor induction with oxytocin infusion.
The nurse immediately places her hand into the vagina and pushes up on the presenting part to relieve pressure on the cord until an emergency cesarean delivery can be performed.
What should be done with the oxytocin infusion?
Explanation
The correct answer is choice C. Stop it completely.This is because oxytocin infusion can cause uterine hyperstimulation, which can worsen the cord compression and compromise fetal oxygenation.Stopping the oxytocin infusion can reduce the frequency and intensity of contractions and relieve pressure on the cord.
Choice A is wrong because increasing the oxytocin infusion rate can increase the risk of cord prolapse and fetal hypoxia.Choice B is wrong because decreasing the oxytocin infusion rate may not be enough to prevent cord compression and fetal distress.Choice D is wrong because maintaining the oxytocin infusion rate can prolong the labor and increase the chance of fetal compromise.
Which of the following patients is at highest risk for umbilical cord prolapse?
Explanation
The correct answer is choice D. A patient who is 34 weeks pregnant with a breech presentation and ruptured membranes.This is because breech presentation and ruptured membranes are both risk factors for umbilical cord prolapse, which is where the umbilical cord descends through the cervix and is alongside or below the presenting part of the fetus.This can cause fetal hypoxia and distress.
Choice A is wrong because a cephalic presentation and intact membranes are not risk factors for umbilical cord prolapse.
Choice B is wrong because although twins and ruptured membranes are risk factors for umbilical cord prolapse, the risk is lower than in choice D. Choice C is wrong because although a transverse lie is a risk factor for umbilical cord prolapse, the risk is lower than in choice D if the membranes are intact.
Which of the following statements by a patient indicates understanding of how to prevent umbilical cord prolapse?
Explanation
The correct answer is choice A. “I will avoid squatting or sitting on the toilet after my water breaks.” This statement indicates that the patient understands how to prevent umbilical cord prolapse, which is a rare but serious complication that occurs when the umbilical cord slips out of the cervix before the baby during labor.This can cut off the baby’s blood and oxygen supply and require immediate delivery.
Choice B is wrong because drinking plenty of fluids does not affect the amniotic fluid level, which is determined by the placenta and the baby’s kidneys.Excessive amniotic fluid (polyhydramnios) can actually increase the risk of umbilical cord prolapse.
Choice C is wrong because monitoring the baby’s movements does not prevent umbilical cord prolapse, although it can help detect fetal distress if the cord is compressed.Decreased fetal movements can have other causes besides cord prolapse, such as fetal sleep cycle, maternal medication, or placental insufficiency.
Choice D is wrong because sleeping on the left side does not prevent umbilical cord prolapse, although it can improve blood flow to the baby and reduce the risk of supine hypotension syndrome.Umbilical cord prolapse can occur regardless of the maternal position.
Normal ranges for amniotic fluid index (AFI) are 5 to 25 cm.Normal ranges for fetal heart rate (FHR) are 110 to 160 beats per minute (bpm).
Sign Up or Login to view all the 15 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

