Multidimensional Module II Final Exam
Total Questions : 99
Showing 25 questions, Sign in for more
A wound has a bloodtinged liquid that is dripping from the surgical site. How does the nurse document this finding?
Explanation
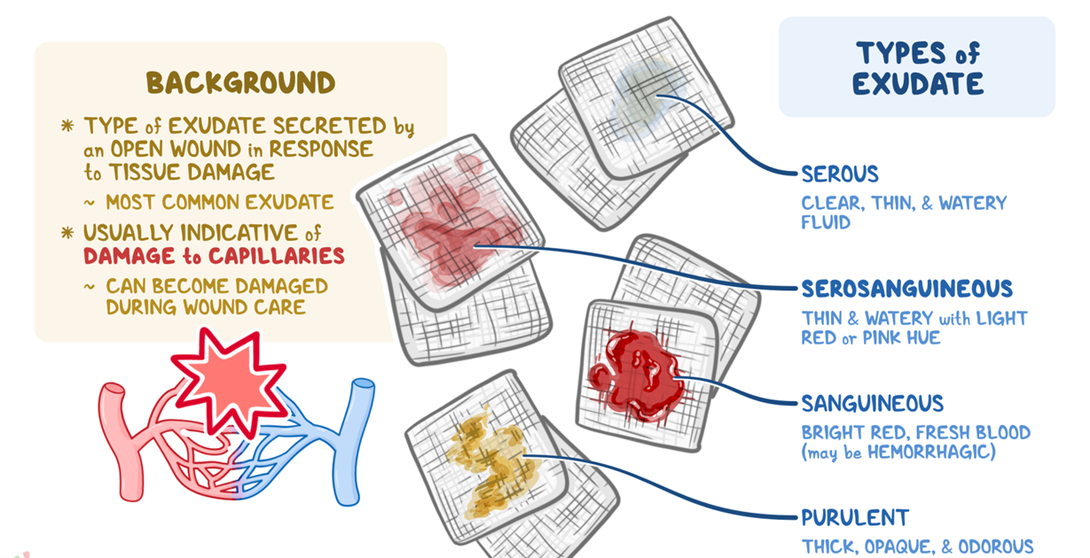
Choice A reason: Purulent exudate is a thick, yellowgreen, or brown pus that indicates infection. It is not bloodtinged and does not drip from the wound.
Choice B reason: Serous exudate is a clear, thin, and watery fluid that is normal in the inflammatory stage of wound healing. It does not contain blood cells and is not red in color.
Choice C reason: Serosanguineous exudate is a pink or red fluid that contains both serum and blood. It is common in the proliferative stage of wound healing and may drip from the wound due to increased capillary permeability.
Choice D reason: Sanguineous exudate is a bright or dark red fluid that consists mostly of blood. It indicates active bleeding and is usually seen in traumatic or surgical wounds. It is not diluted with serum and is more viscous than serosanguineous exudate.
A man has been admitted to the hospital unit with a medical diagnosis of chronic obstructive pulmonary disease (COPD). He is receiving supplemental oxygen at 2 L/min via a nasal cannula. Which positioning technique will best assist him with breathing?
Explanation
Choice A reason: Fowler's position is a semisitting position with the head of the bed elevated at 45 to 60 degrees. This position allows for maximum expansion of the chest and improves ventilation and oxygenation. It also reduces the work of breathing and prevents the abdominal organs from compressing the diaphragm.
Choice B reason: Sim's position is a sidelying position with the lower arm behind the back and the upper knee flexed. This position is used for patients who are unconscious, have difficulty swallowing, or are receiving an enema. It does not facilitate breathing or oxygenation for patients with COPD.
Choice C reason: Prone position is a lying position with the face down and the arms at the sides or bent at the elbows. This position is used for patients with acute respiratory distress syndrome (ARDS) or severe lung injury to improve oxygenation and reduce lung inflammation. It is not recommended for patients with COPD as it may increase the risk of aspiration, pressure ulcers, and nerve damage.
Choice D reason: Lateral position is a sidelying position with the upper leg slightly flexed and supported by a pillow. This position is used for patients who are resting or sleeping to prevent pressure ulcers and promote comfort. It does not improve breathing or oxygenation for patients with COPD.
A client has acquired immunodeficiency syndrome (AIDS). Which of these assessment findings indicate possible infection? (Select all that apply.)
Explanation
Choice A reason: A temperature of 101.3 degrees Fahrenheit is a sign of fever, which is a common symptom of infection. Clients with AIDS have a weakened immune system and are more susceptible to opportunistic infections. Fever indicates that the body is trying to fight off an infection.
Choice B reason: An oxygen saturation of 97% on room air is within the normal range and does not indicate infection. Oxygen saturation measures the percentage of hemoglobin that is bound to oxygen in the blood. A low oxygen saturation may indicate respiratory problems, such as pneumonia, which is a common infection in clients with AIDS.
Choice C reason: A respiratory rate of 22 breaths per minute is slightly above the normal range of 12 to 20 breaths per minute, but it does not necessarily indicate infection. Respiratory rate may vary depending on factors such as activity level, stress, pain, or anxiety. A high respiratory rate may indicate respiratory distress, which could be caused by infection or other conditions.
Choice D reason: Purulent drainage is a thick, yellowgreen, or brown pus that indicates infection. It may come from a wound, an abscess, or a body cavity. Purulent drainage is a sign of inflammation and infection and should be reported to the health care provider.
Choice E reason: A client's ability to ambulate 20 feet is not related to infection. Ambulation is a measure of mobility and function and may be affected by factors such as pain, fatigue, or muscle weakness. Ambulation does not reflect the presence or absence of infection.
A provider has ordered a wound culture for a client with a nonhealing wound. What is the nurse's first action?
Explanation
Choice A reason: Putting on nonsterile gloves is the first action that the nurse should take before performing a wound culture. This is to protect the nurse from exposure to blood and body fluids and to prevent crosscontamination. Nonsterile gloves are sufficient for wound care as long as the wound is not sterile or infected.
Choice B reason: Gently removing the soiled dressings is the second action that the nurse should take after putting on nonsterile gloves. This is to expose the wound and prepare it for irrigation and culture. The nurse should discard the soiled dressings in a biohazard bag and observe the wound for any signs of infection, such as redness, swelling, or odor.
Choice C reason: Irrigating the wound is the third action that the nurse should take after removing the soiled dressings. This is to cleanse the wound and remove any debris or bacteria. The nurse should use sterile normal saline or an antiseptic solution as prescribed by the provider and irrigate the wound with a syringe or a spray bottle. The nurse should avoid touching the wound with the irrigation device and collect the runoff in a basin or a towel.
Choice D reason: Labeling the specimen tube is the last action that the nurse should take after irrigating the wound and obtaining the culture. This is to ensure that the specimen is correctly identified and processed by the laboratory. The nurse should label the tube with the client's name, date, time, and site of the wound. The nurse should also document the procedure and the wound assessment in the client's chart.
The nurse has documented the following wound assessment: “Shallow, open, reddened ulcer with no drainage on the center of the right heel.” What stage is the wound?
Explanation
Choice A reason: Stage 1 is a wound that involves only the epidermis, the outermost layer of the skin. It appears as a nonblanchable redness, warmth, or hardness on intact skin. It does not have any breakage or ulceration of the skin.
Choice B reason: Stage 2 is a wound that involves the epidermis and the dermis, the second layer of the skin. It appears as a shallow, open, reddened ulcer with a partialthickness loss of skin. It may have some serous exudate, but no slough or eschar. It may also present as a blister or abrasion.
Choice C reason: Stage 3 is a wound that involves the epidermis, the dermis, and the subcutaneous tissue, the third layer of the skin. It appears as a deep, open, reddened ulcer with a fullthickness loss of skin. It may have some slough or eschar, but no exposed bone, tendon, or muscle. It may also have tunneling or undermining of the wound edges.
Choice D reason: Stage 4 is a wound that involves the epidermis, the dermis, the subcutaneous tissue, and the underlying structures, such as bone, tendon, or muscle. It appears as a deep, open, reddened ulcer with a fullthickness loss of skin and tissue. It has exposed bone, tendon, or muscle, which may be visible or palpable. It may also have slough, eschar, necrosis, infection, or osteomyelitis.
A nurse is caring for an intubated and sedated geriatric client. What intervention is most appropriate for reducing the risk of a friction and shear injury?
Explanation
Choice A reason: Postponing daily bed bath is not appropriate for reducing the risk of a friction and shear injury. Bed bath is a hygiene measure that helps to keep the skin clean and dry and prevent infection. Friction and shear are caused by the rubbing and pulling of the skin against the bed surface, not by the bed bath itself.
Choice B reason: Elevating the client’s head of the bed to 45 degrees is not appropriate for reducing the risk of a friction and shear injury. In fact, this may increase the risk as the client may slide down the bed due to gravity and cause more friction and shear on the skin. The head of the bed should be kept at the lowest possible angle, preferably less than 30 degrees, unless contraindicated by the client’s condition.
Choice C reason: Caregiver independently slides the client up in bed is not appropriate for reducing the risk of a friction and shear injury. This may cause more damage to the skin as the caregiver may exert excessive force and drag the client’s skin along the bed surface. The caregiver should use a draw sheet or a slide board to lift and reposition the client with the help of another person.
Choice D reason: Use a mechanical lift to reposition the client every 2 hours is the most appropriate intervention for reducing the risk of a friction and shear injury. A mechanical lift is a device that helps to transfer and reposition the client safely and comfortably. It reduces the friction and shear on the skin by lifting the client off the bed surface and avoiding any sliding or dragging. It also prevents the caregiver from injuring themselves by lifting the client manually. The client should be repositioned every 2 hours to relieve the pressure on the skin and prevent pressure ulcers.
What should the nurse do first if they are stuck by a needle?
Explanation
Choice A reason: Flushing the exposed skin with water is the first action that the nurse should take if they are stuck by a needle. This is to reduce the amount of blood or body fluid that may have entered the wound and to prevent infection. The nurse should flush the skin for at least 15 minutes and avoid using soap, antiseptic, or bleach as they may damage the skin or increase the risk of infection.
Choice B reason: Reporting the exposure is the second action that the nurse should take after flushing the exposed skin with water. This is to inform the supervisor, the occupational health department, or the infection control team about the incident and to initiate the postexposure protocol. The nurse should provide the details of the exposure, such as the type and source of the needle, the depth and location of the wound, and the status of the source patient.
Choice C reason: Seeking medical attention is the third action that the nurse should take after reporting the exposure. This is to receive a medical evaluation and treatment, such as testing, prophylaxis, counseling, and followup. The nurse should consult a health care provider as soon as possible and follow the recommendations for preventing or treating any potential infections, such as hepatitis B, hepatitis C, or HIV.
Choice D reason: Completing an incident report is the last action that the nurse should take after seeking medical attention. This is to document the exposure and the actions taken and to identify the causes and the preventive measures for the future. The nurse should fill out the incident report form accurately and objectively and submit it to the appropriate authority. The incident report is not a part of the client's record and should not be mentioned in the client's chart.
The nurse is most concerned about which of these findings in a client with systemic lupus erythematosus (SLE)?
Explanation
Choice A reason: The client having a butterfly rash is not a concerning finding in a client with SLE. A butterfly rash is a malar rash that appears across the cheeks and the bridge of the nose. It is a common sign of SLE and may flare up or fade depending on the disease activity. It does not indicate any serious complication or organ damage.
Choice B reason: A blood pressure of 126/85 mm Hg is not a concerning finding in a client with SLE. This blood pressure is within the normal range and does not indicate hypertension or hypotension. Hypertension is a possible complication of SLE that may affect the kidneys, the heart, or the brain. Hypotension may indicate shock, dehydration, or infection.
Choice C reason: The client reporting chronic fatigue is not a concerning finding in a client with SLE. Chronic fatigue is a common symptom of SLE that affects the quality of life and the ability to perform daily activities. It may be caused by inflammation, pain, anemia, depression, or medication side effects. It does not indicate any acute or lifethreatening condition.
Choice D reason: A urine output of 20 mL/hour is a concerning finding in a client with SLE. This urine output is below the normal range of 30 to 50 mL/hour and indicates oliguria, which is a reduced urine production. Oliguria may indicate acute kidney injury, which is a serious complication of SLE that may lead to renal failure or death. The nurse should monitor the client's urine output, fluid balance, electrolytes, and kidney function and report any abnormal findings to the provider.
A client is recovering from a fractured radius that occurred 8 weeks ago. In which stage of bone healing is the callus resorbed and transformed into bone?
Explanation
Choice A reason: Stage 4 is the remodeling stage of bone healing, which occurs from 6 to 12 weeks after the fracture. In this stage, the callus, which is a mass of fibrous tissue and cartilage that forms around the fracture site, is gradually resorbed and replaced by mature bone. The bone becomes stronger and more compact and regains its original shape and function.
Choice B reason: Stage 3 is the callus formation stage of bone healing, which occurs from 2 to 6 weeks after the fracture. In this stage, the granulation tissue, which is a soft tissue that fills the fracture gap, is replaced by a callus that bridges the fracture ends. The callus is composed of fibroblasts, chondroblasts, and osteoblasts that produce collagen, cartilage, and bone matrix. The callus stabilizes the fracture and prepares it for remodeling.
Choice C reason: Stage 5 is not a valid stage of bone healing. There are only four stages of bone healing: stage 1 is the inflammatory stage, stage 2 is the reparative stage, stage 3 is the callus formation stage, and stage 4 is the remodeling stage.
Choice D reason: Stage 1 is the inflammatory stage of bone healing, which occurs from the time of the fracture to 3 to 5 days after the fracture. In this stage, the blood vessels around the fracture site are ruptured and form a hematoma, which is a blood clot that surrounds the fracture ends. The hematoma triggers an inflammatory response that involves the release of cytokines, growth factors, and inflammatory cells that initiate the healing process. The hematoma also provides a scaffold for the granulation tissue to grow.
The nurse is caring for a client who develops compartment syndrome from a severely fractured arm. The client asks the nurse why this can happen. What is the best response by the nurse?
Explanation
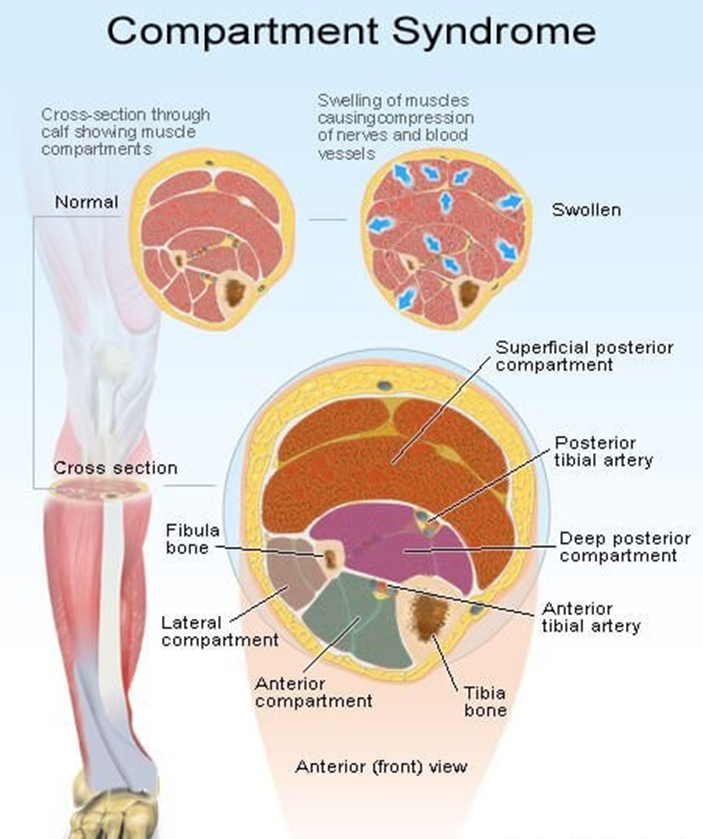
Choice A reason: A bone fragment has injured the nerve supply in the area is not the best response by the nurse. This may be a possible complication of a fracture, but it does not explain the mechanism of compartment syndrome. Compartment syndrome is a condition where the pressure within a closed space (such as a muscle compartment) exceeds the perfusion pressure and causes ischemia and necrosis of the tissues. A bone fragment may damage the nerve, but it does not cause increased pressure in the compartment.
Choice B reason: An injured artery causes impaired arterial perfusion through the compartment is not the best response by the nurse. This may be a possible cause of compartment syndrome, but it is not the most common one. Compartment syndrome is more often caused by venous obstruction than arterial obstruction. An injured artery may reduce the blood flow to the compartment, but it does not cause increased pressure in the compartment.
Choice C reason: Bleeding and swelling cause increased pressure in an area that cannot expand is the best response by the nurse. This is the most common cause of compartment syndrome and explains the pathophysiology of the condition. Bleeding and swelling are the result of inflammation and tissue injury that occur after a fracture. They increase the volume of fluid in the compartment, which cannot expand due to the rigid fascia that surrounds it. This leads to increased pressure in the compartment, which compresses the blood vessels, nerves, and muscles and causes ischemia and necrosis of the tissues.
Choice D reason: The fascia expands with injury, causing pressure on underlying nerves and muscles is not the best response by the nurse. This is not a correct statement, as the fascia does not expand with injury. The fascia is a tough connective tissue that encloses the muscle compartments and limits their expansion. The fascia is part of the problem, not the cause, of compartment syndrome. The fascia prevents the compartment from accommodating the increased volume of fluid and causes increased pressure in the compartment.
The client states, "Why am I getting protein supplements while I'm healing from a bed sore?" What is the best response by the nurse?
Explanation
Choice A reason: "Because it is easy to digest." is not the best response by the nurse. This is not a valid reason for giving protein supplements to a client with a bed sore. Protein supplements may or may not be easy to digest depending on the type and amount of protein and the client's digestive system. The ease of digestion is not the main goal of protein supplementation.
Choice B reason: "If you don't like it, you don't have to take it." is not the best response by the nurse. This is a dismissive and unprofessional response that does not address the client's question or concern. Protein supplements are prescribed for a reason and the client should be educated on the benefits and risks of taking or refusing them. The nurse should also respect the client's preferences and choices and offer alternatives if possible.
Choice C reason: "These supplements have nothing to do with your wound." is not the best response by the nurse. This is a false and misleading statement that contradicts the evidencebased practice of wound care. Protein supplements have a lot to do with wound healing as they provide the essential nutrients for tissue repair and regeneration. Protein deficiency can impair wound healing and increase the risk of infection and complications.
Choice D reason: "Protein has amino acids that promote wound healing." is the best response by the nurse. This is a factual and informative statement that explains the rationale for giving protein supplements to a client with a bed sore. Protein is composed of amino acids, which are the building blocks of cells and tissues. Amino acids are involved in various processes of wound healing, such as collagen synthesis, angiogenesis, and immune response. Protein supplementation can enhance wound healing and prevent protein malnutrition.
Explanation
Choice A reason: Candidiasis is an opportunistic infection associated with AIDS. Candidiasis is a fungal infection caused by Candida species, which normally live in the mouth, throat, vagina, and intestines. In people with AIDS, the immune system is weakened and cannot control the growth of Candida, leading to oral thrush, esophagitis, vaginitis, or systemic candidiasis.
Choice B reason: Hodgkin's lymphoma is not an opportunistic infection associated with AIDS. Hodgkin's lymphoma is a type of cancer that affects the lymphatic system, which is part of the immune system. It is characterized by the presence of ReedSternberg cells, which are abnormal lymphocytes. The exact cause of Hodgkin's lymphoma is unknown, but it is not related to any specific infection.
Choice C reason: Pneumocystis jiroveci pneumonia is an opportunistic infection associated with AIDS. Pneumocystis jiroveci pneumonia is a fungal infection caused by Pneumocystis jiroveci, which normally lives in the lungs of healthy people without causing any symptoms. In people with AIDS, the immune system is weakened and cannot prevent the invasion of Pneumocystis jiroveci, leading to pneumonia, which is a serious and potentially fatal lung infection.
Choice D reason: Clostridium difficile is not an opportunistic infection associated with AIDS. Clostridium difficile is a bacterial infection caused by Clostridium difficile, which normally lives in the colon of healthy people without causing any problems. In some cases, the use of antibiotics can disrupt the normal balance of bacteria in the colon and allow Clostridium difficile to overgrow and produce toxins, leading to diarrhea, colitis, or pseudomembranous colitis. This infection can affect anyone, regardless of their HIV status.
Choice E reason: NonHodgkin's lymphoma is an opportunistic infection associated with AIDS. NonHodgkin's lymphoma is a type of cancer that affects the lymphatic system, which is part of the immune system. It is characterized by the presence of abnormal lymphocytes, which may be B cells, T cells, or natural killer cells. NonHodgkin's lymphoma is associated with several infections, such as EpsteinBarr virus, human herpesvirus 8, hepatitis C virus, and human Tcell leukemia virus, which may trigger the transformation of lymphocytes in people with AIDS.
Explanation
Choice A reason: Heberden's nodes are not a symptom of lupus. Heberden's nodes are bony swellings that form on the distal interphalangeal joints of the fingers. They are a sign of osteoarthritis, which is a degenerative joint disease that causes pain, stiffness, and reduced mobility.
Choice B reason: Chvostek's sign is not a symptom of lupus. Chvostek's sign is a facial twitch that occurs when the facial nerve is tapped near the ear. It is a sign of hypocalcemia, which is a low level of calcium in the blood. Hypocalcemia may be caused by various conditions, such as hypoparathyroidism, vitamin D deficiency, or renal failure.
Choice C reason: OsgoodSchlatter's disease is not a symptom of lupus. OsgoodSchlatter's disease is a condition that affects the growth plate of the tibia, which is the shin bone. It causes pain, swelling, and tenderness below the knee. It is common in adolescents who are active in sports that involve running, jumping, or bending the knee.
Choice D reason: Butterfly rash is a classic symptom of lupus. Butterfly rash is a malar rash that appears across the cheeks and the bridge of the nose. It is a common sign of systemic lupus erythematosus (SLE), which is an autoimmune disease that causes inflammation and damage to various organs and tissues. The rash may flare up or fade depending on the disease activity and exposure to sunlight.
A client is bedridden and appears to be frail and malnourished. Which nursing interventions will most effectively prevent skin injury? (Select all that apply.)
Explanation
Choice A reason: Cleansing the skin routinely after soiling occurs is an effective intervention to prevent skin injury. This is because soiling from urine, feces, sweat, or wound drainage can irritate the skin and cause inflammation, infection, or breakdown. The nurse should use a gentle cleanser and warm water and pat the skin dry. The nurse should also avoid using harsh chemicals, alcohol, or perfumes on the skin.
Choice B reason: Applying moisturizer to dry areas of skin is an effective intervention to prevent skin injury. This is because dry skin is more prone to cracking, peeling, or tearing. The nurse should use a hypoallergenic moisturizer and apply it to the skin after cleansing and drying. The nurse should also avoid using products that contain alcohol, fragrances, or dyes on the skin.
Choice C reason: Using a Hoyer lift for all transfers is an effective intervention to prevent skin injury. This is because a Hoyer lift is a mechanical device that helps to lift and move the client safely and comfortably. It reduces the friction and shear on the skin by lifting the client off the bed surface and avoiding any sliding or dragging. It also prevents the nurse from injuring themselves by lifting the client manually.
Choice D reason: Massaging the client’s reddened shoulders and heels is not an effective intervention to prevent skin injury. In fact, this may worsen the skin injury by increasing the pressure and damage to the tissues. The nurse should avoid massaging any areas that are reddened, swollen, or blistered, as these are signs of pressure ulcers. The nurse should instead relieve the pressure by repositioning the client or using pressurerelieving devices, such as pillows, foam pads, or air mattresses.
Choice E reason: Repositioning the client once per shift is not an effective intervention to prevent skin injury. This is because repositioning the client once per shift is not frequent enough to prevent the development of pressure ulcers. Pressure ulcers are caused by prolonged pressure on the skin that reduces the blood flow and oxygen to the tissues. The nurse should reposition the client at least every 2 hours or more often if needed, depending on the client's condition and risk factors.
What is an infectious disease that can be transmitted directly from one person to another?
Explanation
Choice A reason: A susceptible host is not an infectious disease, but a factor that influences the transmission of an infectious disease. A susceptible host is a person who is vulnerable to infection due to factors such as age, health status, immunization, or genetic predisposition. A susceptible host may become infected by a communicable disease, but it is not the disease itself.
Choice B reason: A communicable disease is an infectious disease that can be transmitted directly from one person to another. A communicable disease is caused by a pathogen, such as a virus, bacterium, fungus, or parasite, that can spread through contact, droplet, airborne, vector, or vehicle transmission. Examples of communicable diseases are influenza, tuberculosis, measles, malaria, and HIV/AIDS.
Choice C reason: A portal of entry to a host is not an infectious disease, but a factor that influences the transmission of an infectious disease. A portal of entry to a host is a route through which a pathogen can enter the body of a susceptible host and cause infection. A portal of entry to a host may be a break in the skin, a mucous membrane, or a body opening, such as the mouth, nose, eyes, or genitals. A portal of entry to a host may facilitate the transmission of a communicable disease, but it is not the disease itself.
Choice D reason: A portal of exit from the reservoir is not an infectious disease, but a factor that influences the transmission of an infectious disease. A portal of exit from the reservoir is a route through which a pathogen can leave the body of an infected person or animal and reach another susceptible host. A portal of exit from the reservoir may be a body fluid, such as blood, saliva, urine, or feces, or a body part, such as the skin, hair, or nails. A portal of exit from the reservoir may enable the transmission of a communicable disease, but it is not the disease itself.
What client is a susceptible host most at risk for infection?
Explanation
Choice A reason: A client with leukemia is a susceptible host most at risk for infection. Leukemia is a type of cancer that affects the blood cells, especially the white blood cells, which are responsible for fighting infections. Leukemia causes the production of abnormal and immature white blood cells that cannot function properly and crowd out the normal ones. This leads to a condition called leukopenia, which is a low level of white blood cells. Leukopenia makes the client more vulnerable to infection by reducing the immune system's ability to defend against pathogens.
Choice B reason: A child who is immunized is not a susceptible host most at risk for infection. Immunization is a process that stimulates the immune system to produce antibodies against a specific disease. Immunization protects the child from getting infected by the disease or reduces the severity of the infection if it occurs. Immunization also prevents the spread of the disease to other people who are not immunized or who are immunocompromised.
Choice C reason: A 60yearold client is not a susceptible host most at risk for infection. Age is a factor that may influence the susceptibility to infection, but it is not the most important one. Older adults may have a weaker immune system due to aging, chronic diseases, or medications, but they may also have a stronger immune memory due to previous exposure to pathogens. The risk of infection in older adults depends on their overall health status, lifestyle, and preventive measures.
Choice D reason: A hospitalized 35yearold client is not a susceptible host most at risk for infection. Hospitalization is a factor that may increase the exposure to infection, but it is not the most significant one. Hospitalized clients may encounter various sources of infection, such as health care workers, other clients, medical equipment, or invasive procedures, but they may also receive adequate infection control measures, such as hand hygiene, isolation, sterilization, or prophylaxis. The risk of infection in hospitalized clients depends on their diagnosis, treatment, and compliance.
A client recently had an abovetheknee amputation and complains of pain distal to the amputation site. What type of pain is the client experiencing?
Explanation
Choice A reason: Nociceptive pain is not the type of pain that the client is experiencing. Nociceptive pain is caused by the stimulation of nociceptors, which are sensory receptors that detect tissue damage or potential harm. Nociceptive pain is usually localized, sharp, throbbing, or aching. It is associated with injuries such as cuts, burns, sprains, or fractures. The client's pain is not caused by any tissue damage or harm in the distal part of the amputated limb, as there is no tissue left there.
Choice B reason: Neuropathic pain is the type of pain that the client is experiencing. Neuropathic pain is caused by the damage or dysfunction of the nervous system, such as the peripheral nerves, the spinal cord, or the brain. Neuropathic pain is usually chronic, burning, shooting, or tingling. It is associated with conditions such as diabetes, shingles, stroke, or amputation. The client's pain is caused by the disruption of the nerve signals from the amputated limb, which creates a phantom sensation of pain in the missing part.
Choice C reason: Cutaneous pain is not the type of pain that the client is experiencing. Cutaneous pain is caused by the stimulation of the cutaneous receptors, which are sensory receptors that detect touch, temperature, or pressure on the skin. Cutaneous pain is usually superficial, brief, or pricking. It is associated with stimuli such as pinching, scratching, or cold. The client's pain is not caused by any touch, temperature, or pressure on the skin of the distal part of the amputated limb, as there is no skin left there.
Choice D reason: Visceral pain is not the type of pain that the client is experiencing. Visceral pain is caused by the stimulation of the visceral receptors, which are sensory receptors that detect stretch, inflammation, or ischemia in the internal organs. Visceral pain is usually deep, dull, or cramping. It is associated with conditions such as appendicitis, pancreatitis, or bowel obstruction. The client's pain is not caused by any stretch, inflammation, or ischemia in the internal organs of the distal part of the amputated limb, as there are no organs left there.
An nurse is caring for a client who has acute osteomyelitis. Which of the following interventions is the nurse's priority?
Explanation
Choice A reason: Providing the client with antipyretic therapy is not the nurse's priority. Antipyretic therapy is a treatment that lowers the body temperature and reduces fever. Fever is a common symptom of acute osteomyelitis, which is a bacterial infection of the bone and bone marrow. Antipyretic therapy may help to relieve the discomfort and inflammation caused by fever, but it does not address the underlying cause of the infection.
Choice B reason: Administering antibiotics to the client is the nurse's priority. Antibiotics are medications that kill or inhibit the growth of bacteria. Antibiotics are the main treatment for acute osteomyelitis, as they target the specific type of bacteria that is causing the infection. Antibiotics can prevent the spread of the infection to other bones or organs and reduce the risk of complications, such as chronic osteomyelitis, septic arthritis, or sepsis.
Choice C reason: Increasing the client's protein intake is not the nurse's priority. Protein intake is a nutritional factor that affects the wound healing and immune system. Protein is composed of amino acids, which are the building blocks of cells and tissues. Protein intake can enhance the repair and regeneration of the bone and the soft tissues that are damaged by the infection. Protein intake can also support the immune system's ability to fight off the infection. However, protein intake alone is not sufficient to treat acute osteomyelitis, as it does not eliminate the bacteria that are causing the infection.
Choice D reason: Teaching relaxation breathing to reduce the client's pain is not the nurse's priority. Relaxation breathing is a technique that involves deep and slow breathing that helps to relax the body and mind. Relaxation breathing can help to reduce the pain and stress that are associated with acute osteomyelitis. Pain is a common symptom of acute osteomyelitis, which is caused by the inflammation and pressure on the bone and the surrounding tissues. Relaxation breathing can help to ease the pain and improve the mood and quality of life of the client. However, relaxation breathing alone is not enough to treat acute osteomyelitis, as it does not address the source of the pain.
What can the nurse teach the client with acquired immunodeficiency syndrome (AIDS) to reduce the risk of infection? (Select all that apply.)
Explanation
Choice A reason: Washing your hands thoroughly is an important measure to reduce the risk of infection. Hand washing is one of the most effective ways to prevent the transmission of germs that can cause diseases. Hand washing can remove dirt, bacteria, viruses, and other contaminants from the skin and prevent them from entering the body or spreading to others. The nurse should teach the client with AIDS to wash their hands frequently and properly, especially before and after eating, using the bathroom, touching their face, or handling any objects that may be contaminated.
Choice B reason: Avoiding cleaning your toothbrush with bleach is not a measure to reduce the risk of infection. Cleaning your toothbrush with bleach is not a recommended practice, as bleach is a harsh chemical that can damage the toothbrush and irritate the mouth. However, cleaning your toothbrush with bleach does not increase the risk of infection, as bleach can kill most germs that may be present on the toothbrush. The nurse should teach the client with AIDS to rinse their toothbrush with water after each use and replace it every 3 to 4 months or sooner if the bristles are worn or frayed.
Choice C reason: Avoiding raw fruits and vegetables is a measure to reduce the risk of infection. Raw fruits and vegetables may be contaminated with bacteria, parasites, or pesticides that can cause foodborne illnesses. The client with AIDS has a weakened immune system that cannot fight off these infections effectively and may develop serious complications, such as diarrhea, dehydration, or malnutrition. The nurse should teach the client with AIDS to wash, peel, or cook their fruits and vegetables before eating them and to avoid any that are bruised, moldy, or spoiled.
Choice D reason: Avoiding crowds is a measure to reduce the risk of infection. Crowds are places where many people gather and interact, such as public transportation, shopping malls, schools, or workplaces. Crowds increase the exposure to germs that can cause respiratory, gastrointestinal, or skin infections. The client with AIDS has a lowered resistance to these infections and may contract them more easily and severely. The nurse should teach the client with AIDS to avoid crowds as much as possible and to wear a mask, practice social distancing, and use hand sanitizer if they have to be in a crowded place.
Choice E reason: Not sharing toothpaste with family members is a measure to reduce the risk of infection. Sharing toothpaste with family members can transfer saliva, blood, or other body fluids that may contain germs that can cause oral, dental, or systemic infections. The client with AIDS is more susceptible to these infections and may also transmit the HIV virus to their family members through their body fluids. The nurse should teach the client with AIDS to use their own toothpaste and toothbrush and to store them separately from their family members' ones.
Explanation
Choice A reason: Inflammation is not an example of a client's primary defense to infection. Inflammation is a secondary defense to infection, which is activated after the primary defense has been breached. Inflammation is a complex process that involves the release of chemical mediators, the dilation of blood vessels, the increase of blood flow, the migration of white blood cells, and the formation of exudate. Inflammation aims to contain, neutralize, and eliminate the infectious agent and to repair the damaged tissue.
Choice B reason: Fever is not an example of a client's primary defense to infection. Fever is a secondary defense to infection, which is activated after the primary defense has been breached. Fever is an elevation of the body temperature above the normal range, which is usually 36.5 to 37.5 degrees Celsius or 97.7 to 99.5 degrees Fahrenheit. Fever is a systemic response to infection that is regulated by the hypothalamus, which is the part of the brain that controls the body's thermostat. Fever enhances the immune system's activity and inhibits the growth of some pathogens.
Choice C reason: Phagocytosis is not an example of a client's primary defense to infection. Phagocytosis is a secondary defense to infection, which is activated after the primary defense has been breached. Phagocytosis is a process that involves the engulfment and destruction of foreign particles, such as bacteria, by specialized cells, such as macrophages and neutrophils. Phagocytosis is a type of cellular immunity that eliminates the infectious agent and prevents its spread.
Choice D reason: Intact skin is an example of a client's primary defense to infection. Intact skin is the first and most important line of defense against infection, as it forms a physical barrier that prevents the entry of pathogens into the body. Intact skin also has chemical and biological properties that resist infection, such as the acidic pH, the secretion of sebum and sweat, and the presence of normal flora. Intact skin protects the underlying tissues and organs from infection and injury.
By providing measures to reduce skin breakdown, how does the nurse break the chain of infection?
Explanation
Choice A reason: Creating a susceptible host is not a way to break the chain of infection, but rather a way to facilitate it. A susceptible host is someone who is vulnerable to infection due to factors such as age, immunocompromised status, or chronic diseases.
Choice B reason: Maintaining the integrity of a portal of entry is a way to break the chain of infection, because it prevents the entry of microorganisms into the body. A portal of entry is any place where microorganisms can enter the body, such as the skin, mucous membranes, or respiratory tract. By reducing skin breakdown, the nurse is protecting the skin from becoming a portal of entry for infection.
Choice C reason: Creating a reservoir to decrease the risk of infection is a contradiction, because a reservoir is a place where microorganisms can multiply and survive, such as a human, animal, or environment. A reservoir increases the risk of infection, not decreases it.
Choice D reason: Sterilizing the area to reduce the reservoir risk is a way to break the chain of infection, but it is not related to reducing skin breakdown. Sterilizing the area means killing or removing all microorganisms from a surface or object, such as a surgical instrument or a wound dressing. This can reduce the reservoir risk, but it does not affect the integrity of the skin as a portal of entry.
The client is at risk for impaired skin integrity related to the need for several weeks of bed rest. The nurse evaluates the client after one week and finds the skin integrity is not impaired. In evaluating the plan of care, what is the nurse’s best action?
Explanation
Choice A reason: Removing the nursing diagnosis in the plan of care since it has not occurred is not a good action, because it does not account for the possibility of future impairment. The client is still at risk for impaired skin integrity due to the prolonged bed rest, and the nurse should continue to monitor and prevent any skin breakdown.
Choice B reason: Keeping the nursing diagnosis in the plan of care the same since the risk factors are still present is the best action, because it reflects the current situation and the potential problem. The client has not developed impaired skin integrity, but the risk factors have not changed. The nurse should maintain the interventions that have been effective in preventing skin impairment, such as turning, repositioning, moisturizing, and inspecting the skin.
Choice C reason: Modifying the nursing diagnosis in the plan of care to impaired skin integrity is not a good action, because it does not match the data. The client has not shown any signs of impaired skin integrity, such as redness, blanching, breakdown, or ulceration. The nurse should not change the diagnosis based on assumptions or predictions, but on evidence.
Choice D reason: Changing the nursing diagnosis in the plan of care to impaired mobility is not a good action, because it does not address the original problem. The client may have impaired mobility due to the bed rest, but that is not the focus of the question. The question is about the risk for impaired skin integrity, which is a different issue that requires different interventions. The nurse should not ignore or replace the existing diagnosis without justification.
The mother of a newborn baby is concerned that the baby will develop illnesses from being around people from outside the family. What is the nurse’s best response?
Explanation
Choice A reason: "You should never go around people after your baby is born." is not a good response, because it is unrealistic, rigid, and dismissive of the mother's concern. It does not acknowledge the benefits of social interaction and support for the mother and the baby, nor the risks of isolation and depression. It also does not provide any evidence or rationale for the advice.
Choice B reason: "Tell me more about that." is the best response, because it is openended, empathetic, and respectful of the mother's concern. It invites the mother to share her feelings and thoughts, and allows the nurse to explore the source and extent of the mother's anxiety. It also creates an opportunity for the nurse to provide education and reassurance based on the mother's needs.
Choice C reason: "I did that, and my kids turned out just fine." is not a good response, because it is personal, irrelevant, and unprofessional. It does not address the mother's concern, but rather shifts the focus to the nurse's own experience, which may not be applicable or helpful to the mother. It also implies that the mother's concern is unfounded or exaggerated, and may make the mother feel judged or defensive.
Choice D reason: "Why do you think that is a bad idea?" is not a good response, because it is closedended, confrontational, and accusatory. It does not show empathy or respect for the mother's concern, but rather challenges or criticizes it. It may make the mother feel defensive or guilty, and may discourage further communication.
Explanation
Choice A reason: Ischemia is a cause of a pressure ulcer, because it means reduced blood flow to the tissues, which can lead to tissue hypoxia, necrosis, and ulceration. Ischemia can result from factors such as compression, friction, shear, or vascular disease.
Choice B reason: Immobility is a cause of a pressure ulcer, because it means prolonged pressure on the bony prominences, which can impair blood flow and cause ischemia, tissue damage, and ulceration. Immobility can result from factors such as paralysis, injury, illness, or sedation.
Choice C reason: Poor nutrition is a cause of a pressure ulcer, because it means inadequate intake or absorption of nutrients, such as protein, calories, vitamins, and minerals, which are essential for tissue repair and wound healing. Poor nutrition can result from factors such as anorexia, malabsorption, or poverty.
Choice D reason: Moisture is a cause of a pressure ulcer, because it means excessive wetness or dampness of the skin, which can weaken the skin barrier, increase the risk of infection, and delay wound healing. Moisture can result from factors such as incontinence, perspiration, or wound drainage.
Choice E reason: Adequate perfusion is not a cause of a pressure ulcer, but rather a protective factor. Adequate perfusion means sufficient blood flow to the tissues, which can prevent ischemia, tissue damage, and ulceration. Adequate perfusion can be promoted by factors such as regular repositioning, pressure relief, and exercise.
The nurse is providing education to a client regarding the administration of eye drops. Which of the following actions indicates the need for further client education?
Explanation
Choice A reason: The client instills the prescribed number of eye drops into the conjunctival sac is a correct action, because it ensures that the medication reaches the eye surface and does not spill out. The conjunctival sac is the space between the eyelid and the eyeball.
Choice B reason: The client washes her hands before instilling the eye drops is a correct action, because it prevents the introduction of microorganisms or foreign substances into the eye. Hand hygiene is an essential infection control measure.
Choice C reason: The client sets the cap to the eye drop container down in a manner that does not contaminate it is a correct action, because it preserves the sterility of the eye drop solution and prevents crosscontamination. The cap should be placed on a clean surface with the inner side facing up.
Choice D reason: The client touches the administration dropper to the eye is an incorrect action, because it can cause injury, infection, or contamination of the eye drop solution. The administration dropper should be held close to the eye, but not touch it.
Sign Up or Login to view all the 99 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

