NACE Foundations of Nursing
Total Questions : 196
Showing 25 questions, Sign in for moreWhen providing nursing care to a client, the nurse provides family-centered nursing care. What is the best rationale for this nursing action?
Explanation
Illness in one family member can affect the other family members. This is because family-centered nursing care recognizes that the family is the basic unit of society and that each member's health influences the whole family's health. Family-centered nursing care also involves collaborating with the family to provide care that meets their needs, preferences, and values.
Choice A is wrong because the nurse does not provide family-centered nursing care to avoid the client’s loneliness. Loneliness is a psychosocial need, not a physiologic one, and it can be addressed by other means than involving the family.
Choice B is wrong because the client’s compliance with medical instructions is not the primary goal of family-centered nursing care. Compliance is influenced by many factors, such as motivation, education, culture, and trust, and it may not always depend on the family’s involvement.
Choice C is wrong because the family’s willingness to listen to instructions is not the main reason for providing family-centered nursing care. The nurse should respect the family’s autonomy and decision-making, and not impose instructions that may conflict with their beliefs or values.
A client on digitalis has a lab report of potassium 3.0 mEq/L.
The nurse would instruct the client to eat which of these foods?
Explanation
The client on Digitalis has a low potassium level of 3.0 mEq/L, below the normal range of 3.5-5.0 mEq/L. Low potassium levels can increase the risk of digitalis toxicity, which can cause nausea, abdominal discomfort, visual changes, and cardiac arrhythmias.
The nurse would instruct the client to eat foods high in potassium, such as cantaloupe, to prevent or correct hypokalemia.

Choice A. Asparagus is wrong because asparagus is a low-potassium food that contains only 202 mg of potassium per cup.
Eating asparagus would not help to raise the client’s potassium level.
Choice C. Blackberries are wrong because blackberries are also a low-potassium food that contains only 233 mg of potassium per cup.
Eating blackberries would not help to raise the client’s potassium level.
Choice D. Cucumbers is wrong because cucumbers are a very low-potassium food that contains only 76 mg of potassium per cup.
Eating cucumbers would not help to raise the client’s potassium level and may even lower it further.
The unlicensed assistive personnel (UAP) is feeding a client with dysphagia. What action would cause the nurse to intervene?
Explanation
This action would cause the nurse to intervene because it increases the risk of choking and aspiration for a client with dysphagia, which is difficulty swallowing. The nurse would instruct the UAP to feed the client small amounts of food slowly, allowing time for chewing and swallowing.
Choice A is wrong because offering thickened liquids is a safe practice for a client with dysphagia. Thickened liquids allow for easier swallowing and less choking, thus decreasing the chance of aspiration.
Choice B is wrong because placing the client in an upright position is also a safe practice for a client with dysphagia. This position helps prevent food from entering the airway and facilitates swallowing.
Choice D is wrong because allowing ample time between bites is another safe practice for a client with dysphagia. This helps the client avoid feeling rushed or overwhelmed and reduces the risk of aspiration.
Warfarin sodium (Coumadin) is ordered for a client.
The client asks the nurse about dietary restrictions while taking this medication. Which of the following foods should be limited?
Explanation
This is because spinach and salads contain a lot of vitamin K, which can make warfarin less effective at preventing blood clots.

Vitamin K helps the blood to clot, so eating foods high in vitamin K can counteract the effect of warfarin.
Choice A is wrong because wheat bread and butter do not contain a lot of vitamin K and do not affect warfarin.
Choice B is wrong because mangoes and tomatoes do not contain a lot of vitamin K and do not affect warfarin.
Choice D is wrong because aged cheeses and wine do not contain a lot of vitamin K and do not affect warfarin.
It is important to keep a stable diet while taking warfarin and avoid sudden changes in the amount of vitamin K intake. Foods that are high in vitamin K include green leafy vegetables, chickpeas, liver, egg yolks, avocado, and olive oil.
These foods should be limited but not eliminated from the diet. Do not drink cranberry or grapefruit juice while taking warfarin as they can increase the risk of bleeding.
A client is diagnosed with hearing loss.
Which nursing intervention will best facilitate communication with the client?
Explanation
Face the client while speaking and ask them to verify understanding. This intervention would help the client to read the nurse’s lips and confirm the message.
It would also show respect and empathy for the client’s condition.
Choice A is wrong because using exaggerated mouth and hand movements when speaking can be distracting and insulting to the client.
It can also distort the words and make them harder to understand.
Choice C is wrong because standing in front of a light when speaking to the client can create glare and make it difficult for the client to see the nurse’s face.
Touching the client to be sure they know where you are can be startling and unnecessary if the client is not visually impaired.
Choice D is wrong because obtaining an interpreter for sign language is inappropriate unless the client knows sign language.
Not all hearing-impaired clients use sign language, and some may prefer other methods of communication.
A client has undergone a surgical procedure and develops a weak, rapid pulse.
Which intervention should the nurse recommend to provider during their SBAR communication?
Explanation
A weak, rapid pulse indicates that the client is experiencing hypovolemia or low blood volume due to blood loss during surgery.
The nurse should recommend to the provider to administer intravenous fluids to restore the client’s circulating volume and improve their hemodynamic status.
Choice A is wrong because anticholinergics are drugs that block the action of acetylcholine, a neurotransmitter that stimulates the parasympathetic nervous system.
Anticholinergics can cause tachycardia, dry mouth, urinary retention, and blurred vision. They are not indicated for hypovolemia.
Choice B is wrong because urinary catheter placement is not a priority intervention for a client with hypovolemia.
Urinary catheterization can help monitor urine output and renal perfusion but does not address the underlying cause of low blood volume.
Choice C is wrong because beta blockers are drugs that block the action of epinephrine and norepinephrine, neurotransmitters that stimulate the sympathetic nervous system.
Beta-blockers can lower blood pressure, heart rate, and cardiac output.
They are not indicated for hypovolemia and can worsen the client’s condition.
To communicate this information using the SBAR tool, the nurse should follow these steps: Situation: Identify yourself, the client, and the problem.
For example: “I am (name), the nurse caring for (client name) in room (number).
I am calling because I am concerned that the client has developed hypovolemia after surgery.”
Background: Provide relevant and brief information related to the situation.
For example: “The client had a surgical procedure (name and type) at (time) today. They have lost (amount) of blood during and after surgery.
Their current vital signs are: blood pressure (value), pulse (value), respiratory rate (value), temperature (value), oxygen saturation (value).”
Assessment: Share your analysis and considerations of options. For
Which is the most appropriate order to remove (doff) personal protective equipment (PPE)?
Explanation
Remove gloves, wash hands, remove face shield, gown, mask, and wash hands again. This is because gloves are the most contaminated piece of PPE and should be removed first to avoid touching other parts of the body or environment with them. Washing hands after removing gloves is also important to reduce the risk of infection. Face shields, gowns, and masks should be removed in that order, as they are less contaminated than gloves and can be handled with clean hands. Washing hands again after removing all PPE is the final step to ensure hygiene.
Choice A is wrong because it does not include washing hands after removing gloves, which is a crucial step to prevent contamination. It also removes the gown before the gloves, which can cause the gown to touch the face or hair and contaminate them.
Choice B is wrong because it does not include washing hands between removing gloves and gown, which can transfer germs from the gloves to the gown and then to the face or hair when removing the face shield and mask.
Choice D is wrong because it does not include washing hands between removing gloves and gown, which can transfer germs from the gloves to the gown and then to the face or hair when removing the face shield and mask. It also removes the gown before the face shield, which can cause the gown to touch the face or hair and contaminate it.
Normal ranges for PPE removal are not applicable as different types of PPE may require different methods of removal. However, some general principles are to remove PPE in a way that minimizes contact with contaminated surfaces, perform hand hygiene frequently, and dispose of PPE properly.
A nurse is developing a plan of care for a client diagnosed with constipation. Which nursing interventions should be included in planning? (Select all that apply).
Explanation
These nursing interventions can help promote bowel movement and prevent constipation. According to, constipation is a common gastrointestinal symptom caused by various factors such as a low-fiber diet, inadequate fluid intake, decreased gastrointestinal motility, medication use, and insufficient activity.
Therefore, encouraging high-fiber food choices, increasing fluid intake to 2,000 mL per day, and encouraging ambulation several times daily are appropriate interventions to address these factors and improve bowel function.
These nursing interventions can help promote bowel movement and prevent constipation. According to, constipation is a common gastrointestinal symptom caused by various factors such as a low-fiber diet, inadequate fluid intake, decreased gastrointestinal motility, medication use, and insufficient activity.
Therefore, encouraging high-fiber food choices, increasing fluid intake to 2,000 mL per day, and encouraging ambulation several times daily are appropriate interventions to address these factors and improve bowel function.
Choice D is wrong because administering antacids as necessary per the bowel management program is not a nursing intervention for constipation.
Antacids are used to neutralize stomach acid and relieve heartburn or indigestion.
They do not have any effect on bowel movement or constipation. In fact, some antacids may cause constipation as a side effect.
Therefore, this intervention is not relevant to the plan of care for a client diagnosed with constipation.
A client states “I don’t want to have surgery.” Which of the following is a therapeutic response to the client?
Explanation
What is your understanding of the situation?”. This is a therapeutic response because it respects the client’s autonomy and invites them to share their concerns and feelings about the surgery.
Choice A is wrong because it is authoritarian and dismissive of the client’s feelings. It does not acknowledge the client’s right to refuse treatment.
Choice C is wrong because it is nontherapeutic and shows agreement with the client’s refusal. It also implies that the nurse and the doctor are on different sides.
Choice D is wrong because it is manipulative and guilt-tripping. It implies that the client does not care about their loved ones or their own life.
A nurse is out in public when an individual suddenly falls to the ground with a generalized tonic- clonic (grand mal) seizure.
Which action should the nurse take first?
Explanation
This is because the recovery position helps maintain the airway and prevent aspiration, and loosening the necktie prevents breathing restriction.
The other choices are wrong because:
Choice A is wrong because placing a stick or any object in the person’s mouth can cause injury to the teeth, gums, tongue or jaw and obstruct the airway. The person cannot swallow or bite their tongue during a seizure.
Choice B is wrong because recording the time of the seizure is not the first priority. The first priority is to ensure the safety and comfort of the person.
Choice C is wrong because restraining the limbs can cause injury or fracture, increase agitation and prolong the seizure. The nurse should protect the person from injury by moving furniture away and padding the head.
Normal ranges for seizure duration are usually less than 5 minutes for generalized tonic-clonic seizures and less than 15 seconds for absence seizures. If the seizure lasts longer than 5 minutes, or if the person has repeated seizures without regaining consciousness, it is considered a medical emergency and requires immediate treatment.
A health care provider prescribes guaifenesin with dextromethorphan 1 tablespoon every 6 hours for a client who has a nonproductive cough.
How many milliliters should a nurse administer for each dose?
Explanation
This is because the prescribed dose is 1 tablespoon, which is equivalent to 15 ml. Therefore, to get the amount of milliliters for each dose, you need to multiply 15 ml by 2, which gives you 30 ml.
Choice A is wrong because 10 ml is less than 1 tablespoon.
Choice B is wrong because 5 ml is equal to 1 teaspoon, which is one-third of a tablespoon.
Choice C is wrong because 15 ml is equal to 1 tablespoon, which is half of the prescribed dose.
Which technique is the proper method to administer otic drops to an adult client?
Explanation
Gently pull the auricle up and back before instilling the drops. This technique straightens the auditory canal and allows the drops to reach the eardrum.
It also prevents contamination of the ear canal by the finger.
Choice A is wrong because pulling the auditory canal down and toward the front is the proper method for children, not adults.
This technique is used for children because their auditory canal is shorter and more curved than adults.
Choice C is wrong because lowering the head and taking a deep breath during the instillation has no effect on the administration of otic drops.
It may also cause discomfort or dizziness for the client.
Choice D is wrong because wearing sterile gloves and inserting one finger in the canal is unnecessary and potentially harmful.
It may introduce bacteria or damage the ear canal or eardrum.
Which statement best documents the situation when a client becomes extremely agitated after receiving a sedative?
Explanation
An idiosyncratic drug effect is an unpredictable and uncommon reaction to a drug that is not related to the dose, the pharmacology, or the patient’s allergy or intolerance. It may be caused by genetic factors, metabolic abnormalities, or interactions with other drugs or substances. An example of an idiosyncratic drug effect is paradoxical agitation or excitement after receiving a sedative.
B. A toxic drug effect is a harmful reaction to a drug that is related to the dose or the pharmacology of the drug. It may cause symptoms such as nausea, vomiting, drowsiness, confusion, or respiratory depression. A toxic drug effect is unlikely to cause agitation after receiving a sedative unless there is an overdose or a drug interaction that increases the level of the sedative in the blood.
C. An allergic drug response is an immunological reaction to a drug that is not related to the dose or the pharmacology of the drug. It may cause symptoms such as rash, itching, swelling, fever, or anaphylaxis. An allergic drug response is unlikely to cause agitation after receiving a sedative unless there is a severe anaphylactic reaction that affects the brain or the circulation.
D. An unexpected drug interaction is a modification of the effect of one drug by another drug or substance that is not predictable based on their pharmacology. It may cause an increase or a decrease in the efficacy or toxicity of one or both drugs. An unexpected drug interaction may cause agitation after receiving a sedative if there is a synergistic effect that enhances the central nervous system stimulation of another drug or substance (such as caffeine, cocaine, or amphetamines) or if there is an antagonistic effect that reduces the central nervous system depression of the sedative (such as flumazenil, naloxone, or physostigmine). However, these interactions are usually known and avoidable by checking the patient’s history and medication list.
Which intervention should the nurse include while caring for a client who has been diaphoretic for the past six hours?
Explanation
This is because a client who has been diaphoretic for the past six hours is likely to have wet and uncomfortable bed linens that can cause skin breakdown and infection. Changing the bed linens frequently can help keep the client dry and comfortable.
Choice A is wrong because offering the client a bedpan every three hours is not related to diaphoresis and may not meet the client’s elimination needs.
Choice B is wrong because keeping an emesis basin near the bedside is not related to diaphoresis and may not be necessary unless the client has nausea or vomiting.
Choice C is wrong because providing oral care every four hours is not enough to prevent dehydration and dry mouth in a client who has been diaphoretic for the past six hours. The client may need more frequent oral care and fluid intake.
Which intervention should the nurse include while caring for a client who has been diaphoretic for the past six hours?
Explanation
This is because a client who has been diaphoretic for the past six hours is likely to have wet and uncomfortable bed linens that can cause skin breakdown and infection. Changing the bed linens frequently can help keep the client dry and comfortable.
Choice A is wrong because offering the client a bedpan every three hours is not related to diaphoresis.
The client may or may not need to use the bedpan depending on their fluid intake and output.
Choice B is wrong because keeping an emesis basin near the bedside is not related to diaphoresis.
The client may or may not need to vomit depending on their underlying condition.
Choice C is wrong because providing oral care every four hours is not enough for a client who has been diaphoretic for the past six hours. The client may have dry mouth and dehydration due to excessive sweating and may need more frequent oral care and hydration.
Which nursing intervention should be performed before applying client restraints?
Explanation
This is because restraints should only be used as a last resort when other alternatives have failed to ensure the patient’s safety and when there is a valid order from the primary healthcare provider.
Assessing the need for restraints placement involves evaluating the patient’s condition, behavior, risk factors, and potential benefits and harms of using restraints.
Choice A is wrong because visual inspection of skin for placement is done after applying restraints, not before.
This is to check for any signs of injury, irritation, or circulation impairment caused by the restraints.
Choice B is wrong because positioning for proper body alignment is done during and after applying restraints, not before.
This is to prevent complications such as pressure ulcers, contractures, or nerve damage due to improper positioning.
Choice D is wrong because reviewing facility policy before usage is not a nursing intervention, but a legal and ethical requirement.
Nurses should be familiar with the facility policy and guidelines regarding the use of restraints and follow them accordingly.
However, this does not replace the need for individualized assessment and evaluation of each patient’s situation.
Which instructions should a nurse give to a client prior to obtaining a throat culture?
Explanation
This is the proper way to obtain a throat culture, which is a test to look for infections in the back of the throat.

Some possible explanations for the other choices are:
Choice B is wrong because there is no need to avoid eating or drinking after a throat culture.
The swab does not interfere with the normal function of the mouth or throat.
Choice C is wrong because coughing while swabbing the throat could contaminate the sample or cause discomfort to the client. The swab should be gently passed along the back area of the throat and tonsils.
Choice D is wrong because swabbing only the anterior tongue would not collect enough cells from the infected area. The swab should reach the back of the throat where bacteria or fungi may grow.
Which statement provides the best documentation of the amount of wound drainage?
Explanation
Two 4x4 gauze cloths saturated with purulent drainage. This statement provides the best documentation of the amount of wound drainage because it specifies the size and number of gauze cloths, the type and amount of exudate, and the presence of infection
Choice B is wrong because it does not indicate the size or number of dressings, the type or amount of exudate, or the presence of infection.
Choice C is wrong because it does not indicate the size or number of dressings, the type of exudate, or the presence of infection.
Choice D is wrong because it does not indicate the size or number of dressings, the type of exudate, or the presence of infection.
Normal ranges for wound drainage are categorized as scant, minimal, moderate, or large/copious The type of wound drainage can be described as serous, sanguineous, serosanguineous, or purulent
Following a uterine biopsy, a client asks a nurse, “Do you think I have cancer?” Which response by the nurse would most likely prompt the client to elaborate on their concerns?
Explanation
I’d like to hear what you are thinking.” This response by the nurse would most likely prompt the client to elaborate on their concerns because it acknowledges the uncertainty of the situation and invites the client to share their feelings and thoughts.
It also shows empathy and respect for the client’s perspective.
Choice A is wrong because it may give false reassurance or minimize the client’s anxiety. Biopsies are not always negative and the nurse cannot predict the outcome.
Choice B is wrong because it may imply that the nurse is avoiding the question or shifting the responsibility to the health care provider.
It also does not address the client’s emotional state or encourage communication.
Choice D is wrong because it may dismiss the client’s fears or imply that they are irrational. It also does not explore the client’s understanding of the procedure or the possible results.
A uterine biopsy is a procedure that involves removing a small piece of tissue from the lining of the uterus (endometrium) for examination under a microscope. It is usually done to diagnose abnormal bleeding, infections, or cancer. The normal range of endometrial thickness varies depending on the menstrual cycle, age, and hormonal status of the woman.
A nurse is reluctant to pray when a client requests to pray together.
Which statement by the nurse would best meet the client’s spiritual needs?
Explanation
“I feel uncomfortable praying with you, but I will find someone who won’t feel that way.” This statement by the nurse would best meet the client’s spiritual needs because it acknowledges the nurse’s own boundaries and feelings while also respecting the client’s request and finding a way to fulfill it.
Some possible explanations for why the other choices are wrong are:
Choice A is wrong because it does not address the client’s request to pray together and it assumes that the client wants a Bible without asking.
Choice B is wrong because it implies that the nurse does not want to pray with the client and that the client’s visitors would be more suitable for this task, which could make the client feel rejected or unsupported.
Choice C is wrong because it directly rejects the client’s request and discloses the nurse’s personal beliefs, which could create a sense of disconnection or conflict between the nurse and the client.
A client asks a nurse, “Why do I have to remove my nail polish in order for my pulse oximetry to be monitored?” Which is the best response by the nurse?
Explanation
Pulse oximetry works by measuring the amount of light that passes through your finger and reaches a sensor on the other side.
The amount of light that is absorbed by your blood depends on how much oxygen it carries. Nail polish can block or reflect some of the light, making it harder for the pulse oximeter to get an accurate reading of your oxygen level.
Choice A is wrong because the color of your nailbed is not relevant for pulse oximetry.
The pulse oximeter does not measure the color of your nailbed, but the amount of light that passes through it.
Choice C is wrong because the sensor does not react with the nail polish causing an allergic reaction.
The sensor is a non-invasive device that does not touch your skin or nail polish directly.
Choice D is wrong because the chemicals in the nail polish do not cause falsely decreased readings of your oxygen level.
The chemicals in the nail polish do not affect the amount of oxygen in your blood, but only the amount of light that reaches the sensor.
Normal ranges for pulse oximetry vary depending on your health condition and altitude, but generally they are between 95% and 100%. If your pulse oximetry reading is lower than 90%, you may have hypoxia, which means your tissues are not getting enough oxygen.
Which strategy should a nurse include when communicating with a client who is blind?
Explanation
Orient the client to the arrangement of the room to promote independence. This strategy helps the client who is blind to navigate the environment safely and confidently. It also shows respect for the client’s autonomy and dignity.
Choice A is wrong because speaking loudly is not necessary for a client who is blind, unless they also have hearing impairment. Speaking loudly may imply that the client is less intelligent or capable, which is not true.
Choice B is wrong because touching the client prior to speaking may startle or frighten them. It is better to identify oneself verbally and ask for permission before touching the client.
Choice D is wrong because keeping the bed in the highest position may increase the risk of injury if the client tries to get out of bed alone. It also restricts the client’s mobility and independence, which may affect their self-esteem and quality of life.
A client is to have a two-hour post-prandial blood glucose drawn.
Which statement should the nurse make to inform the client when the two-hour test will be performed?
Explanation
A two-hour postprandial glucose test is done to check your blood sugar level two hours after you eat a meal.
This test helps to diagnose diabetes or monitor its treatment. A normal blood sugar level for this test is less than 140 mg/dL.
Choice A is wrong because fasting means not eating for at least eight hours before the test. This is done for a fasting blood glucose test, not a postprandial one.
Choice B is wrong because before breakfast means before you eat anything in the morning. This is also done for a fasting blood glucose test, not a postprandial one.
Choice D is wrong because before glucose is consumed means before you drink a sugary liquid for a glucose tolerance test. This test measures how your body handles glucose after drinking it, not after eating a meal.
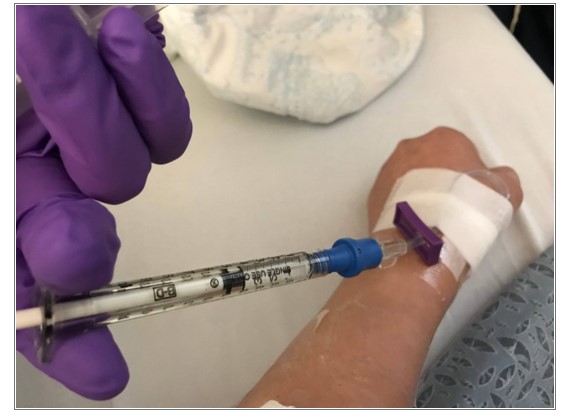
A client with difficult venous access has an intravenous insertion site located at the bend of the wrist.
Which action would be most appropriate for a nurse to take?
Explanation
This is because immobilizing the wrist prevents kinking or dislodgement of the intravenous catheter and reduces the risk of complications such as infiltration, phlebitis, or infection.
Some additional information for the response are:
Choice A is wrong because placing the arm across the client’s chest may compromise venous return and increase the risk of thrombosis.
Choice B is wrong because using a wrist restraint may cause skin breakdown, nerve damage, or impaired circulation.
Choice D is wrong because instructing the client to limit use the of that arm may not be sufficient to prevent catheter movement or accidental removal.
Normal ranges for venous access depend on the type and location of the catheter, but some general values are: potassium (3 to 5 mEq/L), blood urea nitrogen (10 to 20 mg/dL), and central venous pressure (8 to 12 mmHg).
At the end of the shift, a nurse enters a crowded elevator and is standing near a client’s health care provider.
Which response of the nurse is most appropriate when the health care provider asks, “How is my client in room 913 doing?”.
Explanation
The nurse should respect the client’s privacy and confidentiality by not discussing the client’s condition in a crowded elevator, even with the health care provider. The nurse should suggest a more private area to have the conversation.
Choice A is wrong because it shows a lack of professionalism and accountability. The nurse should be able to provide a brief update on the client’s status to the health care provider, even if the nurse is off duty.
Choice B is wrong because it implies that the healthcare provider does not have the right to access the client’s information, which is not true. The health care provider is part of the health care team and has a legitimate need to know the client’s condition.
Choice D is wrong because it violates the client’s privacy and confidentiality by disclosing sensitive information in front of other people. The nurse should not share any details about the client’s condition or treatment without the client’s consent or unless it is necessary for the client’s care.
Sign Up or Login to view all the 196 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

