NS 228 BSN FINAL EXAM 2022
Total Questions : 68
Showing 25 questions, Sign in for moreA client is diagnosed with schizophrenia. A physician orders haloperidol (Haldol), 50 mg bid: benztropine (Cogentin), 1 mg prn: and zolpidem (Ambien). 10 mg HS. Which client behavior would warrant the nurse to administer benztropine?
Explanation
A. Tactile hallucinations: Benztropine is not typically indicated for the treatment of tactile hallucinations. It is primarily used to manage extrapyramidal symptoms (EPS) associated with antipsychotic medications.
B. Reports of hearing disturbing voices: Benztropine is not the first-line treatment for auditory hallucinations in schizophrenia. Antipsychotic medications, such as haloperidol, are more commonly used for this purpose.
C. Hypotension: Benztropine is not used to treat hypotension. It is used to manage extrapyramidal symptoms, such as rigidity and restlessness, that may result from antipsychotic medication use.
D. Restlessness and muticle rigidity: This is the correct answer. Benztropine is an anticholinergic medication that can help alleviate extrapyramidal symptoms (EPS) caused by antipsychotic drugs like haloperidol. Restlessness and muticle rigidity are symptoms of EPS, and benztropine can be used to counteract these side effects.
A nurse on an in-patient unit received the report at 15:00 hours. Which client should the nurse see first?
Explanation
Client diagnosed with hypomania who is speaking loudly on the unit: While hypomanic individuals may exhibit increased energy and talkativeness, the urgency is lower compared to a client expressing active suicidal ideations. This client does not pose an immediate threat to themselves or others.
B. Client diagnosed with mania who expressed active suicidal ideations: This is the correct answer. A client with active suicidal ideations is at an elevated risk and requires immediate attention. Suicidal thoughts in the context of mania can be impulsive, and prompt intervention is crucial to ensure the client's safety.
C. Client with a history of mania who is pacing in the hallway: Pacing may be a symptom of mania, but without additional information about the client's current state and any potential immediate risks, the client expressing active suicidal ideations takes precedence.
D. Client diagnosed with hypomania who is complaining of pain: Pain complaints, in the absence of other urgent factors, do not take precedence over active suicidal ideations. The risk of harm to oneself or others is a higher priority.
What is being assessed when a nurse asks a client to identify name date, residential address, and situation?
Explanation
Orientation: When a nurse asks a client to identify their name, date, residential address, and situation, they are assessing the client's orientation. Orientation refers to an individual's awareness of time, place, person, and situation.
B. Affect: Affect refers to the observable expression of emotions. It involves the client's emotional tone, such as being happy, sad, angry, or flat. It is not directly assessed by asking about personal information.
C. Perception: Perception involves the way individuals interpret and make sense of sensory information. Asking about personal information is more related to orientation than perception.
D. Mood: Mood refers to a more sustained emotional state. It is not directly assessed by asking for specific personal information about the current situation or location.
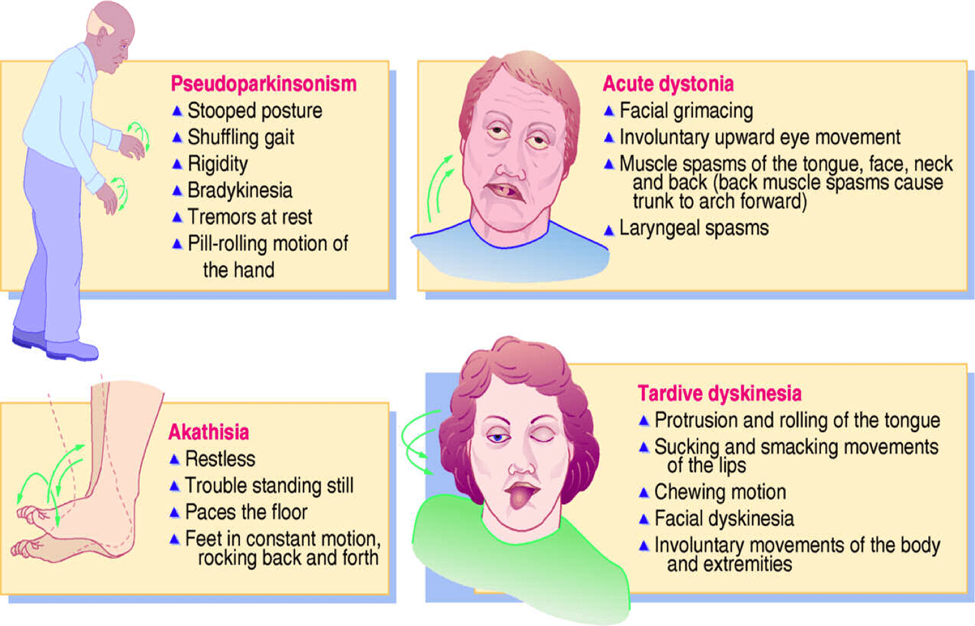
A client diagnosed with schizophrenia, who has been taking antipsychotic medication for the last 5 months, presents in an emergency department (ED) with uncontrollable tongue movements, stiff neck, and difficulty swallowing. The nurse would expect the physician to recognize which condition and implement which treatment?
Explanation
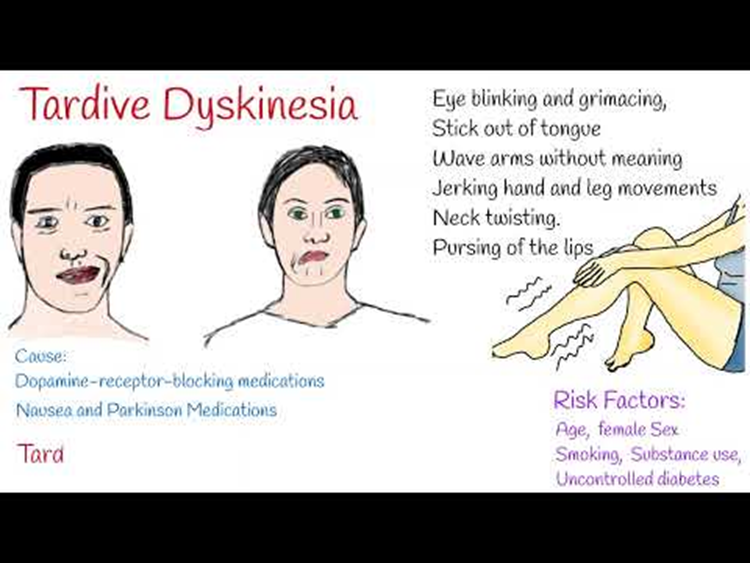
A. Neuroleptic malignant syndrome, treated by discontinuing antipsychotic medications: The symptoms described (uncontrollable tongue movements, stiff neck, difficulty swallowing) are more indicative of tardive dyskinesia than neuroleptic malignant syndrome. Neuroleptic malignant syndrome is characterized by hyperthermia, autonomic dysregulation, altered mental status, and generalized muscle rigidity. Treatment involves discontinuing antipsychotic medications and supportive care.
B. Agranulocytosis treated by administration of clozapine (Clozaril): Agranulocytosis is a rare but serious side effect of clozapine, not a treatment for the symptoms described. The symptoms presented are more consistent with tardive dyskinesia.
C. Tardive dyskinesia treated by discontinuing antipsychotic medication: This is the correct answer. Tardive dyskinesia is a movement disorder characterized by involuntary and abnormal movements, including tongue protrusion and facial grimacing. It can result from long-term use of antipsychotic medications, and discontinuing or reducing the dose of the antipsychotic is a primary intervention.
D. Headache treated by administration of Hydrochlorothiazide: Hydrochlorothiazide is a diuretic used to treat conditions like high blood pressure and edema, not headache or the symptoms described, which are more indicative of tardive dyskinesia.
A client diagnosed with borderline personality disorder brings up a conflict with the staff in a community meeting and develops a following of clients who unreasonably demand modification of unit rules. How can the nursing staff best handle this situation?
Explanation
A. Maintain consistency of care by open communication to avoid staff manipulation: This is the correct answer. Borderline personality disorder (BPD) clients may engage in splitting behaviors, which involve polarized views of staff as either all good or all bad. Maintaining consistency of care and open communication can help prevent manipulation and ensure fair and transparent interactions.
B. Maintain unit order by the application of autocratic leadership: Autocratic leadership, characterized by a top-down approach with limited input from others, may not be the most effective strategy in this situation. It may lead to resistance from clients and potentially escalate the conflict.
C. Allow the clients to apply the democratic process when developing unit rules: While democratic processes are generally beneficial, allowing clients to unreasonably demand modifications of unit rules without considering the overall impact on the therapeutic environment may not be appropriate. It's important to balance client involvement with maintaining a structured and therapeutic milieu.
D. Allow the client spokesperson to verbalize concerns during a unit staff meeting: While it's important to provide a platform for clients to express concerns, allowing a spokesperson to verbalize concerns during a staff meeting should be done in a manner that maintains order and follows the therapeutic goals of the unit. It should not involve unreasonably demanding modifications without a careful consideration of the impact on the overall treatment milieu.
depressed client states. I have a chemical imbalance in my brain. I have no control over my behavior. Medications are my only hope to feel normal again. Which nursing response is appropriate?
Explanation
A. Researchers have been unable to demonstrate a link between nature (biology and genetics) and nurture (environment): This statement is inaccurate. There is substantial evidence supporting the interaction between nature (biology and genetics) and nurture (environment) in the development of mental health conditions, including depression.
B. Medications are one way to address chemical imbalances. Environmental and interpersonal factors can also have an impact on biological factors: This is the correct answer. It acknowledges the role of medications in addressing chemical imbalances but also emphasizes the importance of environmental and interpersonal factors in influencing biological factors. This response aligns with a biopsychosocial model of understanding mental health.
C. Because biological factors are the sole cause of depression, medications will improve your mood: This statement oversimplifies the complex etiology of depression. Depression is a multifactorial condition influenced by biological, psychological, and environmental factors. Medications may be part of the treatment, but they are not the sole solution.
D. Environmental factors have been shown to exert the most influence in the development of depression: This statement is also incorrect. Depression is influenced by a combination of biological, psychological, and environmental factors. No single factor is solely responsible for the development of depression.
Which nursing intervention would be most appropriate when caring for an acutely agitated client with paranoia?
Explanation
A. Provide personal space to respect the client's boundaries: This is the correct answer. Personal space is crucial when caring for an agitated client with paranoia. Respecting the client's need for distance helps to reduce anxiety and prevent escalation of agitation.
B. Maintain continual eye contact throughout the interview: Continuous eye contact may be perceived as confrontational and can increase anxiety, especially in individuals with paranoia. It is important to be mindful of non-verbal cues and adapt the approach to the client's comfort level.
C. Provide neon lights and soft music: Introducing external stimuli like neon lights and music may not be appropriate for an agitated client with paranoia. It could potentially exacerbate their distress. The focus should be on creating a calm and non-threatening environment.
D. Use therapeutic touch to increase trust and rapport: While therapeutic touch can be beneficial in certain situations, it may not be suitable for a client experiencing paranoia. Touch can be perceived as intrusive and may escalate agitation in this context.
A nurse is discussing bias issues in mental health with a newly licensed nurse. Which of the following statements should the nurse include in the discussion?
Explanation
A. Favoring clients over others based upon their mental health diagnosis is not an indication of bias: This statement is incorrect. Favoring or discriminating against clients based on their mental health diagnosis is a clear indication of bias, and it is an issue that the nursing profession aims to address.
B. Displaying basis & conscious art: It seems like there might be a typo in this option. Assuming it means "Displaying bias, conscious or not," this could be a relevant point in discussing unconscious biases that individuals may hold, impacting their interactions with clients.
C. There is a negative stigmatization for mental lives: This is the correct answer. This statement acknowledges the existence of negative stigmatization associated with mental health. Addressing and reducing mental health stigma is an essential aspect of providing quality mental health care.
D. Bias is often isolated to inpatient hospitalization: This statement is not accurate. Bias can manifest in various healthcare settings, not just inpatient hospitalization. It is important to address bias across all levels of care to ensure equitable and unbiased treatment for individuals with mental health concerns.
The patient admitted with antisocial disorder will display which symptom(s)?
Explanation
A. Concern for others: Individuals with antisocial personality disorder typically lack genuine concern for others and may exploit or manipulate them for personal gain.
B. Actively engaged in all unit activities: While engagement in activities can vary, the key feature of antisocial personality disorder is not a high level of engagement but rather a disregard for rules and the rights of others.
C. Mindful of following all of the unit rules: Individuals with antisocial personality disorder often have a history of rule-breaking and may not be consistently mindful of following societal or institutional rules. They may engage in behaviors that violate rules or laws.
D. Manipulative: This is the correct answer. Antisocial personality disorder is characterized by manipulative behaviors, where individuals exploit others for personal gain or pleasure. Manipulation is a key feature of this disorder.

A 16-year-old client diagnosed with schizophrenia experiences command hallucinations to harm others. The clients parents ask a nurse. Where do the voices come from? Which is the appropriate nursing reply?
Explanation
A. Your child has a chemical imbalance of the brain, which leads to altered thoughts: This is the correct answer. It acknowledges the role of a chemical imbalance in the brain contributing to altered thoughts and hallucinations in the context of schizophrenia.
B. Your child's hallucinations are caused by medication interactions: This explanation is not likely in this context. While medications can have side effects, command hallucinations in schizophrenia are primarily related to the underlying disorder.
C. Your child has too little serotonin in the brain causing delusions and hallucinations: While serotonin is involved in mood regulation, attributing hallucinations solely to low serotonin levels oversimplifies the complex neurobiology of schizophrenia.
D. Your child's abnormal hormonal changes have precipitated auditory hallucinations: Hormonal changes are not considered a primary cause of auditory hallucinations in schizophrenia. The emphasis is on neurobiological and genetic factors influencing brain function.
A nurse cares for four patients who are receiving clozapine, lithium, fluoxetine, and venlafaxine, respectively. For which patient should the nurse be most alert for alterations in cardiac or cerebral electrical conductivity as well as fluid and electrolyte imbalance? The patient receiving:
Explanation
A. fluoxetine (Prozac):
Fluoxetine is a selective serotonin reuptake inhibitor (SSRI) commonly used to treat depression and anxiety disorders. While SSRIs can have side effects, significant alterations in cardiac or cerebral electrical conductivity and fluid/electrolyte imbalance are not typically associated with fluoxetine. The primary concerns with SSRIs are related to serotonin levels and can include gastrointestinal disturbances, insomnia, and sexual dysfunction.
B. Lithium (Lithobid):
This is the correct answer. Lithium is known to have potential side effects related to cardiac and cerebral function, as well as fluid and electrolyte balance. Monitoring blood levels of lithium is crucial to avoid toxicity, which can affect the cardiovascular and central nervous systems. Lithium toxicity can lead to symptoms such as tremors, confusion, ataxia, and, in severe cases, seizures.
C. venlafaxine (Effexor):
Venlafaxine is a serotonin-norepinephrine reuptake inhibitor (SNRI) commonly used to treat depression and anxiety disorders. While it can cause some cardiovascular effects, the concern for significant alterations in cardiac or cerebral electrical conductivity and fluid/electrolyte imbalance is generally lower compared to lithium. The primary side effects of venlafaxine are related to serotonin and norepinephrine levels and may include increased blood pressure and heart rate.
D. clozapine (Clozaril):
Clozapine is an atypical antipsychotic medication used to treat schizophrenia. While antipsychotics can have side effects related to metabolic changes, significant alterations in cardiac or electrolyte imbalances are not typically associated with clozapine as the primary concern. Regular monitoring for metabolic side effects, such as weight gain and changes in lipid and glucose levels, is important with antipsychotic medications.
What is the purpose of a nurse gathering client information?
Explanation
A. Enables the nurse to assign the appropriate Axis I diagnosis: Nurses typically do not assign Axis I diagnoses. Diagnosing mental health conditions is typically the responsibility of psychiatrists, psychologists, or other licensed mental health professionals. Nurses, however, play a crucial role in gathering information to contribute to the overall assessment process.
B. Enables the nurse to prescribe the appropriate medications: Nurses do not prescribe medications; that is the responsibility of physicians, nurse practitioners, or other prescribers. However, gathering client information is essential for providing accurate information to the prescriber, assisting in medication management, and monitoring for side effects.
C. Enables the nurse to modify behaviors related to personality disorders: While nurses can assist in the management of behaviors related to mental health conditions, the primary purpose of gathering client information is not to modify behaviors related to personality disorders. It is more about understanding the client's needs and tailoring care accordingly.
D. Enables the nurse to make sound clinical judgments and plan appropriate care: This is the correct answer. Gathering client information is a fundamental step in the nursing assessment process. It provides the necessary data for the nurse to make informed clinical judgments, identify health problems, and plan appropriate care interventions. It allows the nurse to understand the client's unique needs, preferences, and potential risks, leading to individualized and effective care planning.
A client is diagnosed with bipolar disorder and admitted to an inpatient psychiatric unit. Which is the priority outcome for this client?
Explanation
While all the outcomes are important in the overall care of a client with bipolar disorder, the safety of the client takes precedence, especially during the acute phase of the disorder. Bipolar disorder is characterized by mood swings that can include episodes of mania, which may involve risky behaviors or even thoughts of self-harm.
A. The client will remain safe throughout hospitalization: This is the priority outcome. Ensuring the safety of the client during hospitalization involves monitoring for any signs of self-harm or harm to others, managing any acute manic or depressive symptoms, and providing a secure environment.
B. The client will accomplish activities of daily living independently by discharge: While independence in activities of daily living is a valuable outcome, it may not be the immediate priority during the acute phase of bipolar disorder. Addressing safety and stabilization come first.
C. The client will use problem-solving to cope adequately after discharge: Coping skills are important for long-term management, but ensuring safety and stabilization during the hospitalization phase takes precedence. Coping skills can be addressed as part of the overall treatment plan.
D. The client will verbalize feelings during group sessions by discharge: Expression of feelings is an important aspect of mental health treatment, but safety and stabilization remain the priority, especially during the acute phase of bipolar disorder.
A nurse on a mental health unit is caring for a client who has generalized anxiety disorder. The client received a telephone call that was upsetting and now the client is pacing up and down the corridors of the unit. Which of the following actions should the nurse take?
Explanation
A. Allow the client to pace alone until physically tired: While pacing can be a coping mechanism, leaving the client alone may not be the most therapeutic approach. It is important for the nurse to provide support and assess the client's emotional state.
B. Walk with the client at a gradually slower pace: This is the correct answer. Walking with the client at a gradually slower pace allows the nurse to offer support and engage in therapeutic communication. It provides a calming presence and can assist the client in self-regulating their anxiety.
C. Have a staff member escort the client to her room: Escorting the client to her room might be perceived as restrictive or punitive. It is generally more beneficial to engage in supportive interventions and encourage coping strategies.
D. Instruct the client to sit down and stop pacing: Giving direct orders to stop pacing may increase anxiety and may not be an effective approach. It is often better to engage in a supportive manner and explore ways to help the client manage their anxiety.
Thorazine 150mg PO was order for a client. Thorazine is available in 50mg tablets. How many tablets will you administer?
Explanation
To calculate the number of tablets needed, you can use the formula:
Number of tablets =Total dosage ordered/Dosage strength per tablet
In this case:
Number of tablets =150mg/50 mg/tablet
Number of tablets=3tablets
So, the correct answer is:
3.0 Tabs
A nurse on an in-patient unit received report at 15:00 hours. Which client should the nurse see first?
Explanation
A. A client diagnosed with hypomania who is speaking loudly on the unit: Hypomania involves elevated mood and increased activity, but it doesn't typically present an immediate risk of harm to self or others. While it may be disruptive, it doesn't have the same urgency as active suicidal ideation.
B. A client diagnosed with hypomania who is complaining of pain: Pain complaints should be addressed, but in the context of the given choices, it is not the highest priority. Assessing and addressing the potential for harm due to active suicidal ideation is more critical.
C. A client with a history of mania who is pacing in the hallway: Pacing in the hallway, while indicative of increased activity, does not necessarily indicate an immediate risk. The client expressing active suicidal ideations poses a more urgent concern that requires immediate attention.
D.A client diagnosed with mania who expressed active suicidal ideations
In determining priority, the nurse should consider the level of risk and the potential for harm to self or others. Suicidal ideation is a significant concern that requires immediate attention. A client expressing active suicidal thoughts poses an immediate risk to their safety.
A nurse is discussing the difference between mental illness and mental health with a newly licensed nurse. Which of the following statements by the newly licensed nurse indicates an understanding?
Explanation
A. Incorrect. Mental health and mental illness are not the same concepts. Mental health refers to a person's emotional, psychological, and social well-being, while mental illness refers to specific mental health conditions that significantly affect a person's thoughts, emotions, and behaviors.
B. Incorrect. Mental health and mental illness can both present at any age. Mental health is a broader concept that encompasses overall well-being, while mental illnesses can manifest at various stages of life.
C. Correct. This statement accurately distinguishes between mental health and mental illness. Mental health involves the ability to cope with daily stressors, while mental illness is characterized by disruptions in activities of daily living due to specific mental health conditions.
D. Incorrect. This statement confuses the relationship between mental health and mental illness. Mental health is a broader concept that contributes to overall well-being, while mental illness is a specific condition that may arise due to various factors, including poor mental health.
Which behavior displayed by a patient receiving a typical antipsychotic medication would be assessed as displaying behaviors characteristic of tardive dyskinesia (TD)?
Explanation
A. Incorrect. Falling asleep in the chair and refusing to eat lunch is not indicative of tardive dyskinesia (TD). TD is characterized by involuntary movements, not by changes in sleep patterns or appetite.
B. Correct. Grimacing and lip smacking are characteristic movements associated with tardive dyskinesia. TD is a side effect of long-term use of typical antipsychotic medications, and it involves involuntary, repetitive movements, often involving the face and mouth.
C. Incorrect. Excessive salivation and drooling are not specific to tardive dyskinesia. These symptoms may occur due to various reasons, and TD is primarily associated with abnormal, involuntary movements.
D. Incorrect. Experiencing muscle rigidity and tremors is more characteristic of other side effects or conditions, such as extrapyramidal symptoms, but it is not specific to tardive dyskinesia. TD typically involves repetitive, involuntary movements rather than tremors.
A newly admitted patient is severely depressed, lost 20 pounds over the past month, and expresses hopelessness for the future. Select the priority nursing diagnosis
Explanation
A. Priority. The patient is exhibiting severe depression, weight loss, and expressing hopelessness, which are all indicators of an increased risk for suicide. Assessing and addressing the risk for suicide is crucial to ensuring the safety and well-being of the patient.
B. Incorrect. While the patient may be at risk for injury due to factors such as poor nutrition and potential self-harm, the immediate concern in this case is the risk for suicide, given the patient's severe depression and expressed hopelessness.
C. Incorrect. Powerlessness may be a relevant nursing diagnosis for individuals experiencing depression, but the immediate concern in this case is the risk for suicide. Addressing the patient's sense of powerlessness can be part of the broader care plan, but it's not the priority.
D. Incorrect. While the patient has experienced significant weight loss, the priority at this time is addressing the risk for suicide. Once the immediate safety concern is addressed, nutritional concerns can be addressed as part of the overall care plan.
A client diagnosed with bulimia nervosa is to receive fluoxetine (Prozac) by oral solution. The medication is supplied in a 100-ml bottle. The label reads 20 mg/5mL.. The doctor orders 60 mg q day. Which dose of this medication should the nurse dispense?
Explanation
A. Correct. Using the proportion, the correct dose of fluoxetine (Prozac) for the prescribed 60 mg is 15 mL.
B. Incorrect. This is not the correct dose. The correct dose is 15 mL, not 20 mL.
C. Incorrect. This is not the correct dose. The correct dose is 15 mL, not 25 mL.
D. Incorrect. This is not the correct dose. The correct dose is 15 mL, not 10 mL.
Within the nurse's scope of practice, which function is exclusive to the advanced practice psychiatric nurse?
Explanation
A. Teaching clients about their illness: This function is within the scope of practice for both registered nurses and advanced practice psychiatric nurses. Registered nurses often provide education to clients about their illnesses, medications, and overall care.
B. Maintaining safety on the milieu: Both registered nurses and advanced practice psychiatric nurses are responsible for maintaining safety on the milieu. This includes monitoring the environment, assessing potential risks, and intervening to ensure the safety of clients and staff.
C. Prescribing medications: This function is exclusive to advanced practice psychiatric nurses, such as psychiatric nurse practitioners. Registered nurses do not have the authority to prescribe medications. Advanced practice psychiatric nurses receive additional education and training that allows them to prescribe medications as part of their role.
D. Administering medications: Registered nurses, including those specializing in psychiatric nursing, are authorized to administer medications. This is a common nursing function and does not require advanced practice authorization.
A client diagnosed with obsessive-compulsive disorder is admitted to a psychiatric unit. The client has an elaborate routine for toileting activities. Which would be an appropriate initial client outcome during the first week of hospitalization?
Explanation
A. The client will substitute a productive activity for rituals by day one: This outcome may be challenging to achieve within the first day, and it is important to set realistic goals. Moreover, focusing on substituting a productive activity might not address the immediate need to reduce ritualistic behaviors.
B. The client will refrain from ritualistic behaviors during daylight hours: This is an appropriate initial outcome. It acknowledges the challenge of completely eliminating rituals but sets a realistic goal of refraining from these behaviors during daylight hours. This allows for gradual progress without setting unrealistic expectations.
C. The client will participate in unit activities by day three: While participation in unit activities is a positive goal, it may be too optimistic to expect this within the first three days, especially considering the severity of obsessive-compulsive disorder symptoms.
D. The client will wake early enough to complete rituals prior to breakfast: This goal does not promote a reduction in ritualistic behaviors; instead, it may reinforce and accommodate the rituals. The aim of treatment for obsessive-compulsive disorder is to reduce the impact of these rituals, not to support them.
A nurse is caring for a client who has a mental illness and is without housing. The nurse should identify that which of the following interprofessional team members can help the client find housing?
Explanation
A. Psychiatrist: Psychiatrists focus primarily on medical and pharmacological interventions for mental illnesses. While they play a crucial role in diagnosing and treating mental health conditions, they typically do not have the expertise in housing assistance or social services.
B. Behavioral therapist: Behavioral therapists focus on psychotherapeutic interventions to address and modify behavior. They are not typically involved in addressing social determinants of health, such as housing.
C. Social worker: Social workers are specifically trained to address social issues, including housing. They work with clients to assess their social needs, connect them with resources, and advocate for their well-being. In this case, a social worker would be instrumental in helping the client find housing resources and support.
D. Psychologist: Psychologists primarily focus on psychological assessments, therapy, and interventions. Like psychiatrists, their expertise is more centered around mental health treatment rather than addressing the social determinants of health such as housing.
Which client statement would the nurse recognize as indicating that the client understands dietary teaching related to lithium carbonate (Lithobid) treatment?
Explanation
A. "I will take Lithobid on an empty stomach": This statement is incorrect. Lithobid is usually taken with meals or right after meals to minimize gastrointestinal side effects. Taking it on an empty stomach may lead to increased side effects.
B. "I will maintain normal salt intake": This statement is correct. Lithium levels in the blood can be influenced by sodium levels. Maintaining a consistent and normal salt intake is important for the proper functioning of lithium in the body. Both low and high sodium levels can affect lithium levels.
C. "I will consume more fluids": This statement is generally correct. Adequate fluid intake is important to prevent dehydration, as lithium is excreted by the kidneys. However, it should be balanced, and excessive fluid intake should be avoided to prevent lithium toxicity.
D. "I will limit my intake of fluids daily": This statement is incorrect. While fluid intake should be monitored and maintained at a reasonable level, restricting fluids too much can lead to dehydration and an increased risk of lithium toxicity.
A high school senior is diagnosed with anorexia nervosa and is hospitalized for severe malnutrition. The treatment team is planning to use behavior modification. What rationale should a nurse identify as the reasoning behind this therapy choice?
Explanation
A. "This therapy will increase the client's motivation to gain weight": Behavior modification focuses on changing specific behaviors through reinforcement or consequences. While motivation may be a component, the primary goal of behavior modification is to address and modify specific behaviors, such as eating habits, rather than solely relying on motivation.
B. "This therapy will provide the client with control over behavioral choices": Anorexia nervosa often involves issues of control, and behavior modification can empower the individual to regain control over their eating behaviors in a structured and supportive manner. It involves setting goals, reinforcing positive behaviors, and providing a sense of control within the therapeutic framework.
C. "This therapy will reward the client for perfectionist achievement": While anorexia nervosa is associated with perfectionism, rewarding for perfectionist achievement may inadvertently reinforce unhealthy behaviors. Behavior modification aims to promote positive behaviors related to health and well-being rather than reinforcing perfectionism.
D. "This therapy will protect the client from parental overindulgence": Behavior modification is not primarily focused on protecting the client from external factors like parental overindulgence. Instead, it aims to modify specific behaviors through positive reinforcement or consequences.
Sign Up or Login to view all the 68 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

