Nursing 2356 multidimensional care
Total Questions : 42
Showing 25 questions, Sign in for moreWhat client should be seen by the nurse first?
Explanation
A fractured hip in an elderly person can be a life-threatening injury due to the risk of complications such as blood clots, pneumonia, and infection.
It is important for the nurse to assess the man’s pain level, vital signs, and overall condition and initiate appropriate interventions as soon as possible.

Choice A) A client with acute diarrhea may require prompt attention to prevent dehydration, but it is not as urgent as a fractured hip.
Choice B) A client who is anxious may benefit from interventions to reduce anxiety, but it is not a life-threatening condition.
Choice C) A woman who feels isolated may benefit from social support and interventions to address her emotional needs, but it is not an urgent medical condition.
An older client is wearing a hearing aid.
What intervention can the nurse implement to improve communication?
Explanation
Background noise can interfere with the ability of a person with hearing loss to understand speech, even when wearing a hearing aid.
By turning off the television, the nurse can reduce background noise and improve communication with the client.
Choice A) Chewing gum is not an appropriate intervention to improve communication with a client who has hearing loss.
Choice C) Speaking loudly and clearly may help, but it is not as effective as reducing background noise.
Choice D) Using paper and pencil may be helpful in some situations, but it is not the most effective intervention to improve communication with a client who is wearing a hearing aid.
A client states that he is Muslim.
The client has type two diabetes mellitus and has been prescribed a long-acting insulin.
The client says that he fasts for Ramadan.
Explanation
Collaborate with the client and provider to develop a client-centered plan of care.
It is important for the nurse to respect the client’s cultural and religious beliefs while also ensuring that his medical needs are met.
By collaborating with the client and his healthcare provider, the nurse can help develop a plan of care that takes into account the client’s desire to fast during Ramadan while also managing his diabetes.

Choice A) Educating the client that fasting is not an option is not respectful of the client’s beliefs and may not be effective in promoting adherence to treatment.
Choice B) Telling the client not to take his insulin the night before is not appropriate as it may result in uncontrolled blood sugar levels.
Choice C) Informing the client that he will need to change his lifestyle completely is not a client-centered approach and may not be effective in promoting adherence to treatment.
Which set of vital signs, taken on an adult, is cause for concern and requires further evaluation?
Explanation
Temperature 97.0°F; pulse 54 bpm; respirations 14 breaths/minute; blood pressure 196/114 mmHg.
This set of vital signs is cause for concern because the blood pressure is significantly elevated.
A blood pressure reading of 196/114 mmHg is considered a hypertensive crisis and requires immediate medical attention.
Choice A) Temperature 96.9°F; pulse 100 bpm; respirations 20 breaths/minute; blood pressure 120/80 mmHg is within normal limits for an adult.
Choice C) Temperature 98.6°F; pulse 60 bpm; respirations 14 breaths/minute; blood pressure 110/66 mmHg is also within normal limits for an adult.
Choice D) Temperature 99°F; pulse 72 bpm; respirations 16 breaths/minute; blood pressure 100/60 mmHg is slightly elevated but not cause for immediate concern.
A client has decreased mobility.
What nursing intervention would be inappropriate to promote mobility?
Explanation
Encouraging bed rest would be an inappropriate nursing intervention to promote mobility for a client with decreased mobility.
Bed rest can lead to further complications of immobility1.

Choice A is not an answer because teaching the client to do active range of motion (AROM) exercises every 2 hours can help maintain joint mobility and muscle strength2.
Choice B is not an answer because evaluating the client’s need for ambulatory aids can help them move safely and independently1.
Choice C is not an answer because keeping skin clean and dry is important for preventing skin breakdown, which can be a complication of immobility1.
The nurse is teaching a community group about poisoning prevention.
Which of the following statements from an attendee would indicate the need for further teaching?
Explanation
Inducing vomiting is not always the appropriate first aid response for poisoning and can sometimes be harmful.
It is important to call the poison control center for guidance on what to do if you suspect poisoning1.
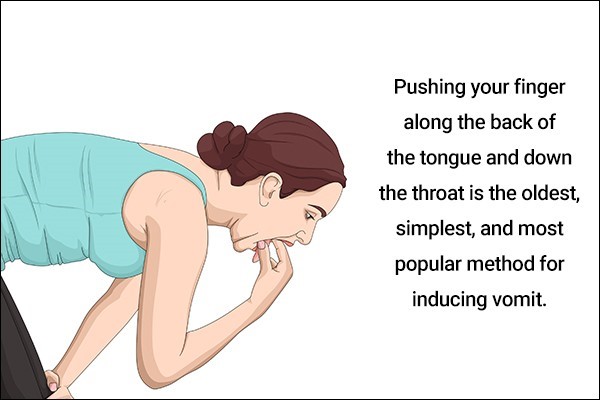
Choice A is not an answer because taking prescription medications only as prescribed can help prevent accidental poisoning1.
Choice B is not an answer because sharing prescription medications can be dangerous and lead to accidental poisoning2.
Choice D is not an answer because having the phone number for the poison control center easily accessible can help you quickly get guidance on what to do in case of suspected poisoning1.
A nurse is telling a new mother from Africa that she shouldn't carry her baby in a sling created from a large rectangular cloth.
The African woman tells the nurse that everyone in Mozambique carries babies this way.
The nurse believes that bassinets are safer for infants. What is this scenario an example of?
Explanation
This scenario is an example of cultural imposition.
Cultural imposition is when one person or group imposes their beliefs, values, and practices on another person or group.
Choice B is not an answer because cultural competency involves understanding and respecting the beliefs, values, and practices of different cultures.
Choice C is not an answer because stereotyping involves making assumptions about a person or group based on preconceived notions or generalizations.
Choice D is not an answer because racism involves discrimination or prejudice against a person or group based on their race.
What complication may be a result of decreased mobility?
Explanation
Pressure injuries may be a result of decreased mobility.
When a person has decreased mobility, they may spend extended periods of time in one position, which can put pressure on certain areas of the body and lead to the development of pressure injuries.
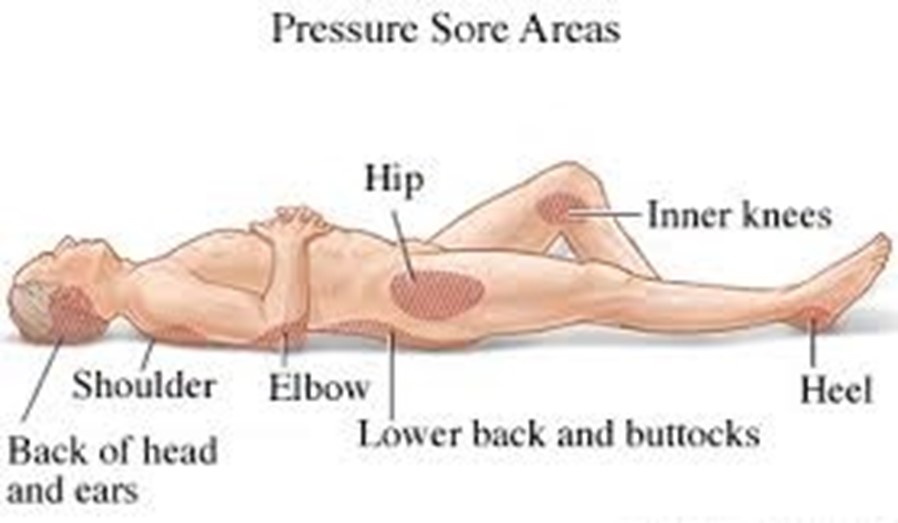
Choice B is not an answer because diarrhea is not typically a result of decreased mobility.
Choice C is not an answer because euphoria is not typically a result of decreased mobility.
Choice D is not an answer because increased energy is not typically a result of decreased mobility.
What is the primary purpose of an incident report?
Explanation
The primary purpose of an incident report is to identify opportunities for improvement.
Incident reports are used to document and analyze events that have occurred in order to identify areas for improvement and prevent similar incidents from happening in the future.
Choice A is not an answer because incident reports are not typically used as a tool for disciplinary action.
Choice B is not an answer because while incident reports can help identify and address errors, their primary purpose is not to eliminate unforeseen errors.
Choice D is not an answer because the primary purpose of incident reports is not to hold persons accountable for their errors, but rather to identify opportunities for improvement.
According to Maslow's Hierarchy of Needs, what do all people have?
Explanation
According to Maslow’s Hierarchy of Needs, all people have basic human needs that must be met before they can attend to higher needs.
These basic human needs are physiological (food and clothing), safety (job security), love and belonging needs (friendship), esteem, and self-actualization1.
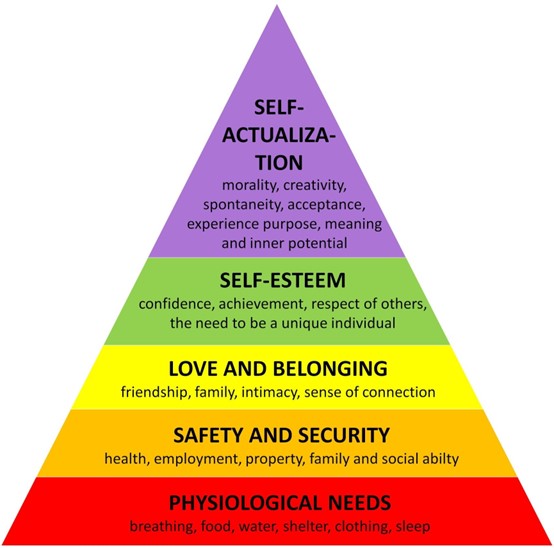
Choice A is incorrect because people do not have the same needs at the same time.
Choice B is incorrect because Maslow’s Hierarchy of Needs does not mention the risk of becoming ill.
Choice C is incorrect because not all people have a desire to be the best.
What is not a sign of inadequate perfusion?
Explanation
Bounding pulses are not a sign of inadequate perfusion.
Inadequate perfusion is when blood flow to a specific part of your body is reduced and that part will not receive essential nutrients.
Signs of inadequate perfusion include cyanosis (bluish discoloration of the skin due to lack of oxygen), pallor (paleness of the skin), and coolness1.

Choice B is incorrect because cyanosis is a sign of inadequate perfusion.
Choice C is incorrect because pallor is a sign of inadequate perfusion.
Choice D is incorrect because coolness is a sign of inadequate perfusion.
A client just received a diagnosis of cancer.
Which statement by the nurse best demonstrates empathy?
Explanation
Tell me more about it.” This statement acknowledges the difficulty of the situation and invites the patient to share their feelings and thoughts.
Choice A is incorrect because it does not acknowledge the patient’s current feelings and offers false reassurance.
Choice C is incorrect because it does not acknowledge the patient’s current feelings and may come across as intrusive.
Choice D is incorrect because it does not acknowledge the patient’s current feelings and offers false reassurance.
The nurse knows which of the following is a "never event"?
Explanation
A surgical sponge left in a client’s incision is a “never event”.
A “never event” is a serious, largely preventable safety incident that should not occur if the available preventative measures are implemented1.
These events include things like wrong-site surgery or foreign objects left in a person’s body after an operation2.
Choice A is incorrect because no blood incompatibility during a blood transfusion is not a “never event”.
Choice C is incorrect because a client falling in their own home is not a “never event”.
Choice D is incorrect because inserting a urinary catheter before surgery is not a “never event”.
Which of the following statements creates a barrier to communication?
Explanation
“Do you know how to change your dressing?” This statement can create a barrier to communication because it may make the patient feel judged or defensive if they do not know how to change their dressing.
It is better to phrase the question in a more open-ended and non-judgmental way, such as “Can you tell me about your experience with changing your dressing?”
Choice B is not an answer because it encourages the patient to share information about their hospitalization and promotes open communication.
Choice C is not an answer because it shows that the speaker is actively listening and engaging with the patient’s previous statements.
Choice D is not an answer because it encourages the patient to share information about their pain management and promotes open communication.
A nurse and client work on strategies to reduce weight.
What phase of the therapeutic relationship are the nurse and client in?
Explanation
Working.
The working phase of the therapeutic relationship is when the nurse and client work together to develop and implement strategies to achieve the client’s goals.
In this case, the goal is to reduce weight, so the nurse and client are working on strategies to achieve that goal.
Choice A is not an answer because the pre-interaction phase occurs before the nurse and client meet and involves the nurse preparing for the first interaction with the client.
Choice B is not an answer because the orientation phase is when the nurse and client get to know each other and establish trust and rapport.
Choice D is not an answer because the termination phase occurs when the therapeutic relationship ends and involves evaluating progress and planning for future care.
A client is diagnosed with narcolepsy. What is the nurse's priority intervention?
Explanation
Inform the client that driving would be dangerous.
Narcolepsy is a sleep disorder characterized by excessive daytime sleepiness and sudden attacks of sleep.
As a result, it can be dangerous for individuals with narcolepsy to engage in activities that require sustained attention and alertness, such as driving.
The nurse’s priority intervention would be to inform the client of this risk and advise them to avoid driving.

Choice A is not an answer because while avoiding caffeine after 6 pm may help improve sleep quality, it is not the priority intervention for a client with narcolepsy.
Choice B is not an answer because drinking two cups of regular coffee may worsen the symptoms of narcolepsy and is not a recommended intervention.
Choice C is not an answer because while participating in normal activities may be beneficial for overall health and well-being, it is not the priority intervention for a client with narcolepsy.
A client has insomnia.
Which of the following is not an appropriate client education for a client experiencing insomnia?
Explanation
Take naps when drowsy.
Taking naps during the day can disrupt nighttime sleep and worsen insomnia.
It is generally not recommended for individuals with insomnia to take naps, even if they feel drowsy during the day.
Choice B is not an answer because regular exercise can improve sleep quality and is a recommended intervention for individuals with insomnia.
Choice C is not an answer because limiting fluids before bedtime can reduce the need to urinate during the night and improve sleep quality.
Choice D is not an answer because limiting alcohol consumption before bedtime can improve sleep quality and reduce the risk of sleep disruptions.
What expected physiological changes of the older adult put them at risk of falls? (Select all that apply).
Explanation
Reduced muscle strength, sensory losses like vision and hearing, and slowing of reflexes are all expected physiological changes of the older adult that can put them at risk of falls.
Reduced muscle strength can make it more difficult for older adults to maintain balance and stability.
Sensory losses like vision and hearing can affect an older adult’s ability to perceive their environment and navigate safely.
Slowing of reflexes can make it more difficult for older adults to react quickly to changes in their environment and prevent falls.
Choice D is not an answer because dementia is not a physiological change but rather a cognitive condition that can increase the risk of falls.
Choice E is not an answer because the inability to adapt is not a specific physiological change but rather a general characteristic that can increase the risk of falls.
A fire is found in a client's room during a routine medication pass. What is the nurse's first action?
Explanation
The nurse’s first action when a fire is discovered in a client’s room is to evacuate any clients or visitors in immediate danger12.
This is because the safety of the clients and visitors is the top priority.
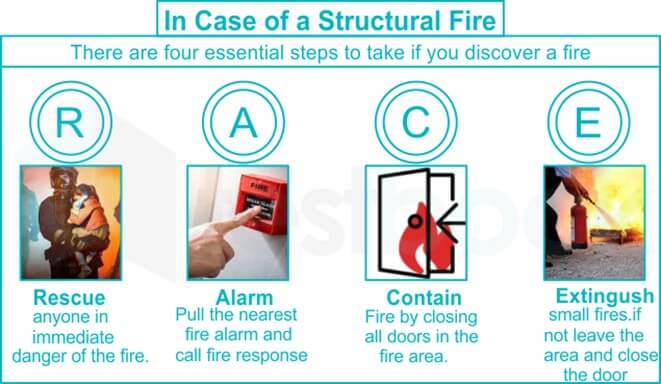
Choice A is not the correct answer because activating the fire alarm is not the first action that should be taken.
Choice B is not the correct answer because confining the fire by closing all doors and windows is not the first action that should be taken.
Choice C is not the correct answer because notifying the supervisor is not the first action that should be taken.
A nurse from a predominantly Latino culture works in a hospital that services a large Hmong population.
What action by the nurse best demonstrates cultural competence?
Explanation
The action that best demonstrates cultural competence is for the nurse to ask the clients what matters most to them in their illness and treatment.
Cultural competence describes the ability to effectively interact with people belonging to different cultures.
The importance of cultural competence in nursing focuses on health equity through patient-centered care, which requires seeing each patient as a unique person1.
Choice B is not the correct answer because telling clients that they should not continue taking herbs does not demonstrate cultural competence.
Choice C is not the correct answer because asking clients if they utilize shaman does not demonstrate cultural competence.
Choice D is not the correct answer because telling clients that they should follow the provider’s orders does not demonstrate cultural competence.
An eight-year-old child is eating a hotdog and begins coughing. What is the nurse's priority action?
Explanation
The nurse’s priority action when an eight-year-old child is eating a hotdog and begins coughing is to promote coughing.
Coughing is the body’s natural way of trying to clear an obstruction from the airway.
Choice A is not the correct answer because beginning the Heimlich maneuver quickly is not the first action that should be taken.
Choice B is not the correct answer because telling the child to put his hands by his neck to signify that he is choking is not the first action that should be taken.
Choice D is not the correct answer because leaving the child alone to find a phone is not the first action that should be taken.
When assessing the client's bowel elimination, the nurse understands that which is not a factor?
Explanation
Gender is not a factor that affects bowel elimination.
Many factors affect bowel elimination including age, diet, fluid intake, physical activity, psychological factors, personal habits, and medications1.
Choice A is not the correct answer because age is a factor that affects bowel elimination.
Choice B is not the correct answer because the diet is a factor that affects bowel elimination.
Choice C is not the correct answer because fluid intake is a factor that affects bowel elimination.
What is the mission of the Occupational Safety and Health Administration (OSHA)?
Explanation
The mission of the Occupational Safety and Health Administration (OSHA) is to ensure safe and healthful working conditions for workers by setting and enforcing standards and by providing training, outreach, education, and assistance1.
This was established by Congress with the Occupational Safety and Health Act of 19701.

Choice A is incorrect because OSHA’s mission is focused on protecting workers, not clients.
Choice C is incorrect because OSHA’s focus is on preventing work-related injuries, illnesses, and deaths, not injuries a nurse may incur at home.
Choice D is incorrect because OSHA’s mission is not focused on reducing client falls or providing emotional support.
What would be the best education for a nurse to give a client to prevent poisoning of a child in the home?
Explanation
To prevent poisoning of a child in the home, it is important to keep cleaning liquids and other potential poisons in a locked cabinet12.
This includes storing medicines, chemicals, and cleaners up high in a locked cupboard and in their original containers1.
Choice A is incorrect because it focuses on prescription medications and not on preventing the poisoning of a child in the home.
Choice C is incorrect because it focuses on taking medications correctly and not on preventing the poisoning of a child in the home.
Choice D is incorrect because storing medications in a visible and accessible place could increase the risk of poisoning if a child were to access them.
What level of Maslow's Hierarchy of Needs does food belong to?
Explanation
Food belongs to the physiological level of Maslow’s Hierarchy of Needs1.
This is the lowest level of the hierarchy and includes basic needs that are vital to survival, such as food, water, and shelter1.
Choice A is incorrect because love and belonging are at a higher level of Maslow’s Hierarchy of Needs and do not include food.
Choice B is incorrect because safety and security are also a higher level of Maslow’s Hierarchy of Needs and do not include food.
Choice D is incorrect because esteem is a higher level of Maslow’s Hierarchy of Needs and does not include food.
Sign Up or Login to view all the 42 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

