Nursing Fundamental 100 exam 2
Total Questions : 45
Showing 25 questions, Sign in for moreA patient presents to the Emergency Room with swollen legs and shortness of breath. He tells you that he has a history of heart failure which causes the fluid to build up m his legs and lungs. When you listen to his lung sounds you are most likely to hear which type of breathing sounds?
Explanation
Crackles, also known as rales, are discontinuous sounds that are typically heard during inspiration in patients with heart failure. These sounds are produced by the sudden opening of small airways and alveoli that are filled with fluid or collapsed due to pulmonary congestion. The sound can be described as similar to the sound of rubbing hair between fingers or the sound of Velcro being pulled apart.
Rhonchi are continuous, low-pitched sounds that are typically heard during expiration and are caused by the movement of air through narrowed airways, such as in patients with chronic obstructive pulmonary disease (COPD). Stridor is a high-pitched, continuous sound that is typically heard during inspiration and indicates upper airway obstruction, which can be life-threatening. Neither rhonchi nor stridor are typically heard in patients with heart failure.
Therefore, based on the patient's history and symptoms, the most likely type of breathing sound to be heard on auscultation is crackles/rales.

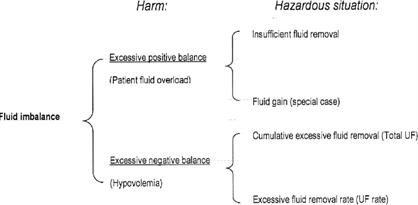
A dialysis unit nurse caring for a client with renal failure will expect the client to exhibit which fluid imbalance?
Explanation
Renal failure can cause a buildup of fluid in the body. When kidneys lose their filtering ability, dangerous levels of wastes may accumulate, and your blood’s chemical makeup may get out of balance. This can lead to fluid retention, causing swelling in your legs, ankles or feet.
The nurse is caring for a client who recently had surgery on her left hip. What should be the priority teaching for the patient after surgery to prevent complications?
Explanation
The use of an incentive spirometer is essential after surgery to prevent complications such as pneumonia and atelectasis. Atelectasis is the collapse of air sacs in the lungs, which can occur after surgery due to decreased respiratory effort and shallow breathing. An incentive spirometer helps the patient take deep breaths and increase their lung volume, preventing these complications.
Breathing rapidly to prevent pneumonia (option b) is not recommended as it can lead to hyperventilation and other respiratory complications.
Option c is incorrect because patient education is a crucial aspect of post-operative care, and the patient needs to be aware of the potential complications and how to prevent them.
The use of a chest tube (option d) is not usually required after hip surgery, and it is not a priority teaching for the patient.
A patient’s hemoglobin is severely low and she is complaining of being overly tired and fatigued. You are educating her on the role hemoglobin has with oxygenation and perfusion. You will know she understands the role of hemoglobin when she tells you hemoglobin transports:
Explanation
Hemoglobin is a protein found in red blood cells that plays a crucial role in transporting oxygen from the lungs to the body's tissues and organs. When oxygen is breathed in, it binds to the hemoglobin in red blood cells, forming oxyhemoglobin. This oxyhemoglobin is then transported throughout the body via the circulatory system, delivering oxygen to the cells that need it
 .
.
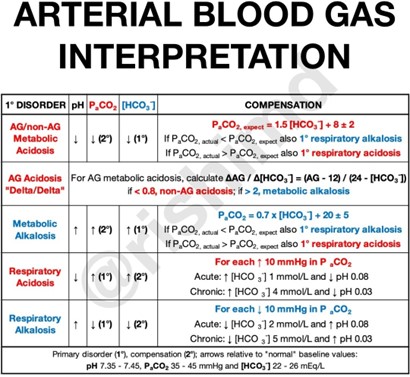
The nurse is caring for a client with chronic obstructive pulmonary disease (COPD). Which arterial blood gas data does the nurse anticipate finding in this patient?
Explanation
A. Respiratory acidosis.
COPD is a chronic lung disease that can lead to an accumulation of carbon dioxide (CO2) in the body. This can cause respiratory acidosis, a condition in which the blood pH is lower than normal due to an excess of CO2.
In respiratory acidosis, the partial pressure of carbon dioxide (PaCO2) in the blood is increased and the pH is decreased. The kidneys atempt to compensate for the acidosis by excreting more acid in the urine and retaining more bicarbonate, but this compensation is usually not enough to fully correct the problem.
Metabolic alkalosis (option B) is a condition in which the blood pH is higher than normal due to an excess of bicarbonate in the blood. This is usually caused by loss of acid from the body, such as through vomiting or use of diuretics.
Respiratory alkalosis (option C) is a condition in which the blood pH is higher than normal due to a decrease in PaCO2. This can be caused by hyperventilation, which leads to excessive elimination of CO2 from the lungs.
Metabolic acidosis (option D) is a condition in which the blood pH is lower than normal due to an excess of acid in the blood. This can be caused by a variety of factors, including kidney failure or lactic acidosis.
The nurse is caring for a client who requires IV fluids. which IV fluid type would be considered a hypertonic solution?
Explanation
Hypertonic solutions have a higher concentration of solutes (such as sodium, glucose, or mannitol) than the fluid in the body's cells, causing water to move out of the cells and into the bloodstream. This results in the shrinking of the cells and an increase in extracellular fluid volume.
Examples of hypertonic solutions include 10% dextrose in water (D10W), 3% saline, and 5% dextrose in 0.9% saline.
In contrast, isotonic solutions have the same concentration of solutes as the fluid in the body's cells, and hypotonic solutions have a lower concentration of solutes than the fluid in the body's cells.
Therefore, in this scenario, the nurse should administer a hypertonic solution to the client who requires IV fluids.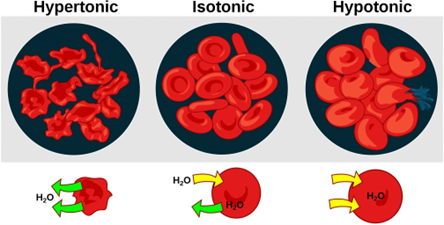
Coughing and Deep breathing is taught to a patient to prevent recurrent pneumonia. She is educated to breathe in deeply first to over expand lung volume: this is called what?
Explanation
Deep breathing or "diaphragmatic breathing" is a technique used to prevent recurrent pneumonia and improve lung function. During deep breathing, the patient is instructed to inhale deeply, expanding their lung volume as much as possible. This process is called inspiration.
Expiration, on the other hand, is the process of exhaling or breathing out air from the lungs. Intake refers to the process of taking in air or breathing in, while chest is a part of the body where the lungs are located.

You are setting up a room for your patient that has a new tracheostomy. Select all of the equipment you need bring with to ensure patient is safe should the tracheostomy become dislodged:
Explanation
A tracheostomy is a surgical procedure that involves creating an opening in the neck to establish a direct airway to the trachea. It is usually done in patients who require long-term mechanical ventilation or have upper airway obstruction. In case the tracheostomy becomes dislodged, the following equipment should be available to ensure the patient's safety:
Tracheostomy kit setup: This includes a new tracheostomy tube, obturator, and other equipment necessary to replace the dislodged tracheostomy tube.
Suction equipment: Dislodgement of the tracheostomy tube can cause airway obstruction due to the presence of secretions. Suction equipment can be used to remove the secretions and prevent airway obstruction.
Smaller Tracheostomy Tube and Same size Tracheostomy Tube: If the dislodged tracheostomy tube cannot be reinserted or is damaged, having smaller and same size tracheostomy tubes available can be helpful in establishing a new airway.
Ambu bag: This is a manual resuscitation device used to provide positive pressure ventilation to the patient. It can be used in case the patient's breathing is compromised due to airway obstruction.
Oxygen: The patient may require supplemental oxygen if their breathing is compromised due to airway obstruction.
Larger Tracheostomy Tube: A larger tracheostomy tube may not be needed immediately and may be contraindicated in some cases as it can cause trauma to the tracheal wall.

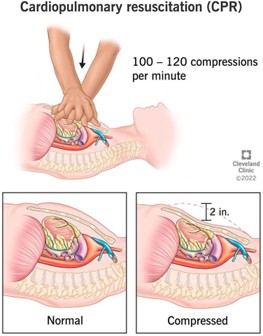
A nurse on a cardiac care unit oversees the care of different client’s cardiac health problems. Which action can be most appropriately delegated to personnel (UAP/CNA) when a patrent is found unresponsive?
Explanation
CPR (Cardiopulmonary Resuscitation) is a life-saving procedure that is performed when a person's heart has stopped beating. It involves chest compressions and rescue breathing to restore the circulation of oxygenated blood to the brain and other vital organs. The timely initiation of CPR can significantly increase the chances of a patient's survival.
In a healthcare setting, UAPs/CNAs are often trained to provide basic life support, including initiating CPR, until a healthcare provider arrives. However, giving IV epinephrine, intubating the patient, and obtaining arterial blood gases are all advanced medical procedures that require specialized training and expertise. These actions should only be performed by trained healthcare providers, such as registered nurses, physicians, or respiratory therapists, and cannot be delegated to UAPs/CNAs.
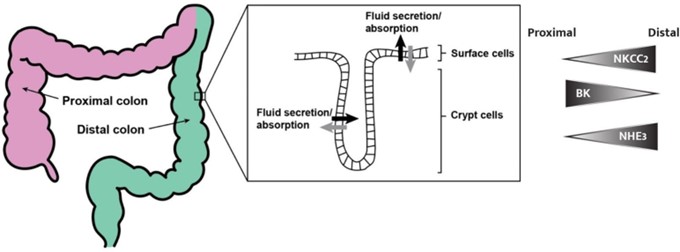
JD has been admited after a large portion of his colon has been removed due to cancer Which statement by the patient demonstrates that he understands the function of the Gastrointestinal tract as related to fluid and electrolyte balance.
Explanation
The colon is responsible for absorbing water and nutrients.
I am now at high risk for fluid and electrolyte imbalances. This statement demonstrates that the patient understands the function of the gastrointestinal tract in relation to fluid and electrolyte balance. The colon plays an important role in absorbing water and electrolytes from digested food, and after a large portion of the colon has been removed, the patient may be at higher risk for fluid and electrolyte imbalances.
Received message. The correct option is a. The colon is responsible for absorbing water and nutrients. I am now at high risk for fluid and electrolyte imbalances. This statement demonstrates that the patient understands the function of the gastrointestinal tract in relation to fluid and electrolyte balance. The colon plays an important role in absorbing water and electrolytes from digested food, and after a large portion of the colon has been removed, the patient may be at higher risk for fluid and electrolyte imbalances.
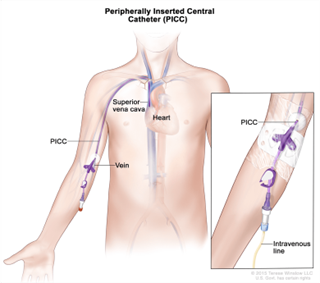
A patient on the cardiac floor has just had a PlCC line placed by the MD. the Xray team has not verified the position of the catheter tip, yet. You check the heart monitor and notice she begins having an irregular heart rhythm called Atrial Fibrillation. You anticipate that the PlCC line is touching which chamber of the heart?
Explanation
A PICC line is a long, thin tube that’s inserted through a vein in your arm and passed through to the larger veins near your heart 1. If the PICC line is touching a chamber of the heart, it is most likely touching the right atrium 2.

Albuterol is prescribed for a 79-year-old male patient with severe COPD and Asthma You notice that he is having difficulty timing inhalation to receive the maximum dose of Albuterol. You give him a device to atach to the end of the Albuterol Inhaler called an aero chamber. You then educate him to before pumping the medication into the chamber.
Explanation
Before pumping the medication into the chamber, you should educate the patient to exhale. This means that the patient should breathe out fully before using the inhaler. This helps to empty the lungs of air and create more space for the medication to be inhaled.

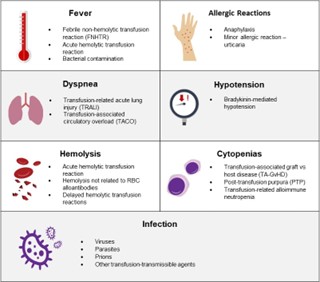
A nurse is administering a blood transfusion to a client. After 15 minutes, the client reports difficulty breathing. What is the first action by the nurse?
Explanation
Difficulty breathing is a sign of a potential transfusion reaction. When a client reports difficulty breathing during a blood transfusion, the nurse should stop the transfusion immediately to prevent the reaction from worsening. Once the transfusion is stopped, the nurse can then assess the client's vital signs and notify the healthcare provider of the client's response. Documentation of the findings should also be completed after the client's condition has stabilized. However, stopping the transfusion takes priority over documenting the findings.
The nurse is discussing car safety with the mother of a 6-year-old child. The child’s mother questions the need for the use of special car seats for her child. What information can be provided to her?
Explanation
Booster seats are recommended for children between the ages of 4 and 8, or until they are 4'9" tall. This is because seat belts are designed for adults and may not properly fit a child's smaller body. A booster seat helps to position the seat belt correctly on the child's body, improving the effectiveness of the seat belt and reducing the risk of injury in the event of a crash.
Option a is incorrect because 10 years old is too old to need a car seat. Option b is incorrect because children under the age of 8, or under 4'9" tall, should not use a seat belt alone. Option d is incorrect because car seats are recommended until children are at least 4 years old, not 3.
A client with renal disease requires IV fluids. It is important for the nurse to:
Explanation
: A client with renal disease may have impaired kidney function, which can affect fluid balance in the body. Giving fluids too quickly or increasing the infusion rate too quickly can lead to fluid overload,
which can exacerbate the client's condition. It is important for the nurse to monitor the amount of fluid the client is receiving to ensure that the infusion rate is appropriate for the client's condition and to prevent fluid overload. Checking the intravenous rate every two days is not sufficient; the nurse should monitor the rate regularly and adjust it as necessary based on the client's response.

You receive report from the off going nurse that patient L K is admited with hyponatremia. the nurse states he is becoming increasingly confused as the day goes on and management is considering restraining the patient, so he does not become a harm to himself. You assess the patient and note that the IV fluids hanging are 0.33% NaCI. What should you do next?
Explanation
Hyponatremia is a condition where the sodium levels in the blood are abnormally low. It can cause confusion, seizures, and even coma in severe cases. The IV fluids hanging are 0.33% NaCI, which means they have a low sodium concentration, and may be contributing to the patient's hyponatremia.
Given that the patient is becoming increasingly confused, it is important to assess his mental status and monitor him closely to prevent harm. However, restraining the patient should not be the first course of action. Instead, the nurse should focus on identifying the underlying cause of the hyponatremia and taking appropriate steps to address it.
Therefore, the next step would be to get an order for additional lab work to assess the patient's electrolyte levels and identify the cause of the hyponatremia. This will help to guide further treatment and management decisions for the patient.

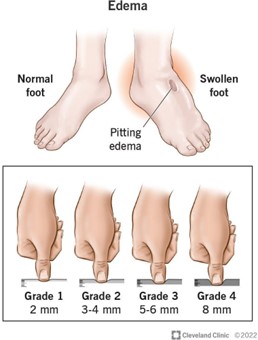
At the end of shift, you are calculating intake and output on your pat lent who was admited for a non- emergent gall bladder removal. She is alert and oriented and able to recall the amount of fluid she has drank all day. You can calculate the amount of IV fluids administered. Her intake is 2500ml and her output is 1200ml from a catheter bag. You realize she is not excreting enough urine me for water she is taking in.
Explanation
. Assess your patient’s lower extremities and lungs for fluid retention.
If a patient’s intake is 2500ml and her output is 1200ml from a catheter bag, and you are concerned that she may not be excreting enough urine for the amount of water she is taking in, the most appropriate next step would be to assess her lower extremities and lungs for fluid retention. This can help determine if the patient is retaining water and if further intervention is necessary.
The nurse scaring for a patient who will be needing a blood transfusion. The nurse knows that the universal recipient of blood would be considered blood type:
Explanation

AB+ blood type is known as the universal recipient because individuals with this blood type have both A and B antigens on the surface of their red blood cells, as well as the Rh antigen. This means that they can receive blood from donors of any ABO blood type (A, B, AB, or O) and Rh factor (positive or negative) without experiencing a transfusion reaction.
Therefore, in the case of a patient who will be needing a blood transfusion, if the nurse knows that the patient's blood type is unknown, it is ideal to give them AB+ blood type as it is considered the safest option.
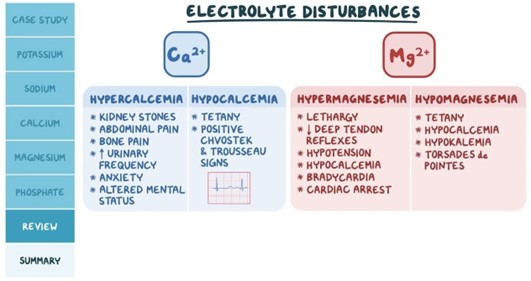
Patient MK is admited with Atrial Fibrillation an irregular heart rhythm. She is also complaining of muscle cramps to her legs and that she started a new diuretic last week. What lab value are you most likely to find on her Complete Metabolic Panel?
Explanation
Atrial fibrillation is a common arrhythmia, and diuretics are often used in the management of patients with this condition to help control fluid balance. However, diuretics can cause electrolyte imbalances, especially hypokalaemia (low potassium levels), which can lead to muscle cramps and other complications.
A Complete Metabolic Panel (CMP) is a blood test that measures various electrolytes, glucose, and other important components. Among the options given, the most likely lab value to be abnormal in Patient MK's case is a low level of potassium (K+), which is consistent with her symptoms and diuretic use. Option d, K+ -
-
- mEq/L, is the correct option as it represents a low level of potassium, which is defined as a value less than 3.5 mEq/L.
Option a, Mg2 – 20 mEq/L, represents high magnesium levels, which are not typically associated with diuretic use or muscle cramps. Option b, Na+ - 123 mEq/L, represents low sodium levels, which are less likely to occur with diuretic use, and are typically associated with other conditions. Option c, Ca2 – 10.0 mg/dl, represents normal calcium levels and is not typically affected by diuretic use.

The nurse is working in the intensive care unit and has just received lab results for her patients. Which of the following are considered electrolyte imbalances? (Select all That Apply)
Explanation
These are all electrolyte imbalances. Hyperkalaemia is an elevated level of potassium in the blood. Hypocalcaemia is a low level of calcium in the blood. Hyponatremia is a low level of sodium in the blood. Thrombocytopenia and anemia are not electrolyte imbalances. Thrombocytopenia is a low platelet count and anemia is a low red blood cell count or low hemoglobin levels.
A patient who is ordered a fluid restriction of 1000ml fluid restriction. He is on the list for a kidney transplant due to kidney failure. His mouth feels dry during the day. and he wants to know how he can moisten his mouth without going over his restriction:
Explanation
c. Sip the water he is allowed to have slowly to make it last throughout the day.
Option a is not recommended as hard candies may contain sugar and artificial sweeteners, which can be harmful to the patient's health.
Option b is not recommended because caffeinated tea has diuretic properties that can increase urine output, leading to further dehydration.
Option d is not recommended as Gatorade is a sports drink that contains high amounts of sugar and electrolytes, which can lead to fluid overload and imbalances.
Sipping the water slowly can help the patient moisten his mouth without going over his fluid restriction. This approach can also help him pace his fluid intake throughout the day, which can be beneficial for maintaining proper hydration levels and managing fluid overload.
The home care nurse visits a client with compromised lung function. The client has greenish yellow sputum with a musty odor. Which assessment is the priority for the
Explanation
The client's greenish-yellow sputum with a musty odor may indicate an infection, such as pneumonia or bronchitis, which can affect the client's lung function. By auscultating bilateral breath sounds, the nurse can assess for the presence of abnormal lung sounds, such as crackles or wheezing, which may indicate further respiratory compromise.
While obtaining a blood culture for tuberculosis (option b) may be appropriate in certain circumstances, the client's sputum color and odor do not necessarily indicate tuberculosis as the cause of their respiratory symptoms.
Requesting pulmonary function studies (option c) may also be beneficial in assessing the client's lung function, but this is not the priority assessment in this situation.
Finally, while documenting the findings (option d) is an important aspect of nursing care, it is not the priority action when the client is presenting with signs of compromised lung function.

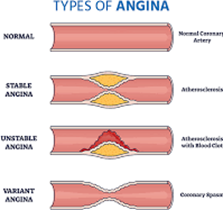
During a Cardiac Stress test, a patient complains of chest pain while running The chest pain subsides when he stops running and is relaxed. The patient is diagnosed with Stable angina and is given education by the nurse. He understands the lack of muscles is causing stable angina during exercise.
Explanation
During exercise, the heart has to work harder to pump blood and oxygen to the muscles. In patients with stable angina, there is a partial blockage of the coronary arteries, which reduces blood flow and oxygen delivery to the heart muscle. This lack of oxygen to the heart muscles causes chest pain or discomfort, which subsides when the patient stops exercising and is relaxed.
Therefore, it is important for the patient with stable angina to avoid activities that trigger chest pain, take prescribed medications, and make lifestyle modifications to manage their condition.
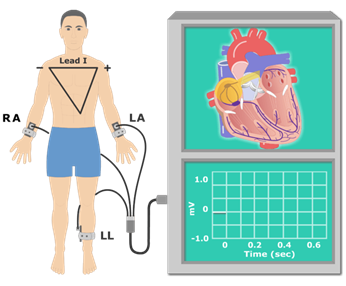
Your patient is ordered an EKG upon admission to the hospital. She is very scared and states she has never had one of these diagnostic tests before. Which answer is most appropriate by the nurse regarding EKG.
Explanation
This response provides the patient with accurate and reassuring information about the EKG procedure. It explains that the test is painless and describes what will happen during the test. The other responses do not provide as much information or reassurance to the patient.
The nurse is caring for a client with respiratory alkalosis. Which arterial blood gas data does the nurse anticipate finding?
Explanation
Respiratory alkalosis is a condition in which the blood pH is elevated due to a decrease in the partial pressure of carbon dioxide (CO2) in the blood. This can occur when a person breathes too rapidly or deeply (hyperventilation), causing them to exhale too much CO2. In this option, the pH is elevated (normal range is 7.35-7.45), the CO2 is low (normal range is 35-45 mmHg), and the bicarbonate (HCO3) level is within the normal range (22-26 mEq/L), which are all consistent with respiratory alkalosis.
Sign Up or Login to view all the 45 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

