Chemotherapy Agents and Oncology Pharmacology > Pharmacology
Exam Review
Nursing Interventions
Total Questions : 4
Showing 4 questions, Sign in for moreA nurse is preparing to administer chemotherapy to a patient who has lung cancer. Which of the following laboratory tests should the nurse review before giving the chemotherapy drugs?
Explanation
Choice A reason:
The nurse should review the complete blood count and differential before administering chemotherapy to a patient who has lung cancer. The complete blood count and differential measure the number and types of blood cells, such as red blood cells, white blood cells, and platelets. Chemotherapy drugs can cause bone marrow suppression, which can result in anemia, leukopenia, and thrombocytopenia. These conditions can increase the risk of infection, bleeding, and fatigue. The nurse should compare the patient's blood counts with the normal values and the provider's orders and report any abnormalities or contraindications to the provider.
Choice B reason:
The nurse should review the serum electrolytes and blood urea nitrogen before administering chemotherapy to a patient who has lung cancer. The serum electrolytes measure the levels of sodium, potassium, chloride, and bicarbonate in the blood. The blood urea nitrogen measures the amount of urea nitrogen, a waste product of protein metabolism, in the blood. Chemotherapy drugs can cause nephrotoxicity, which can impair the kidney's function and cause electrolyte imbalance, dehydration, and metabolic acidosis. The nurse should compare the patient's serum electrolytes and blood urea nitrogen with the normal values and the provider's orders and report any abnormalities or contraindications to the provider.
Choice C reason:
The nurse should review the liver function tests and serum bilirubin before administering chemotherapy to a patient who has lung cancer. The liver function tests measure the levels of enzymes and proteins that reflect the liver's function, such as alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), albumin, and total protein. The serum bilirubin measures the level of bilirubin, a pigment that is produced by the breakdown of red blood cells, in the blood. Chemotherapy drugs can cause hepatotoxicity, which can damage the liver cells and impair the liver's function. The nurse should compare the patient's liver function tests and serum bilirubin with the normal values and the provider's orders and report any abnormalities or contraindications to the provider.
Choice D reason:
All of the above laboratory tests are important to review before administering chemotherapy to a patient who has lung cancer. Chemotherapy drugs can cause various adverse effects that affect different organs and systems in the body. The nurse should monitor the patient's laboratory values closely and adjust the dosage or frequency of chemotherapy drugs as prescribed by the provider. The nurse should also provide supportive care and education to the patient to prevent or manage the adverse effects of chemotherapy.
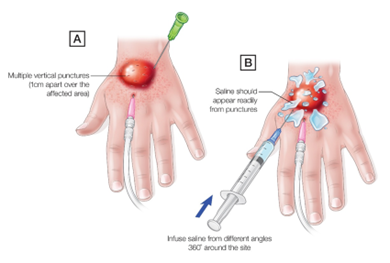
A nurse is administering chemotherapy to a patient who has colon cancer via an intravenous (IV) line. The nurse should monitor the IV site closely for signs of extravasation, which is:
Explanation
Choice A reason:
This is the definition of extravasation, which is a rare but serious complication of intravenous chemotherapy. Extravasation can cause tissue damage or necrosis, especially if the drug is a vesicant (a highly toxic substance that causes blisters). The nurse should monitor the IV site closely for signs of extravasation, such as tingling, burning, swelling, redness, or discomfort. If extravasation occurs, the nurse should stop the infusion immediately and follow the appropriate protocol to minimize the harm.
Choice B reason:
This is the definition of thrombophlebitis, which is inflammation of a vein due to a blood clot. Thrombophlebitis can occur as a complication of IV therapy, but it is not the same as extravasation. The nurse should monitor the IV site for signs of thrombophlebitis, such as redness, warmth, and tenderness along the vein. If thrombophlebitis occurs, the nurse should discontinue the IV line and apply warm compresses to the affected area³.
Choice C reason:
This is the definition of infiltration, which is the leakage of fluid into the tissues due to a dislodged or punctured IV catheter. Infiltration can cause edema, pallor, and decreased skin temperature around the IV site. Infiltration can also occur as a complication of IV therapy, but it is not as serious as extravasation. The nurse should monitor the IV site for signs of infiltration, such as swelling, coolness, or dampness. If infiltration occurs, the nurse should stop the infusion and remove the IV line³.
Choice D reason:
This is the definition of occlusion, which is the blockage of an IV catheter by a precipitate (a solid substance that forms when two solutions are mixed). Occlusion can cause reduced or absent flow rate and increased pressure in the IV line. Occlusion can also occur as a complication of IV therapy, but it is not related to extravasation. The nurse should monitor the IV line for signs of occlusion, such as difficulty in flushing or infusing fluids. If occlusion occurs, the nurse should try to clear the catheter by flushing with saline or heparin³.
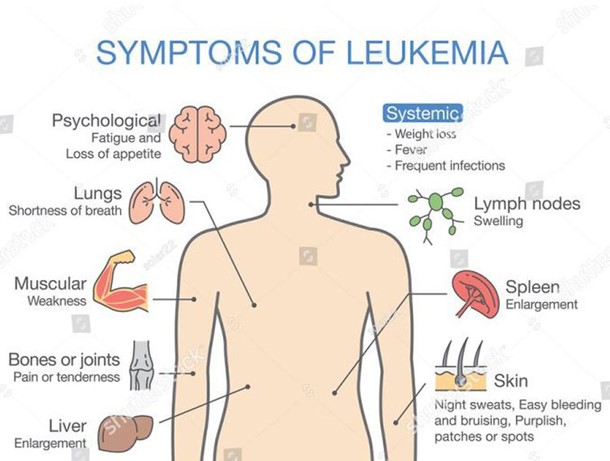
A nurse is caring for a patient who has leukemia and is receiving chemotherapy that causes bone marrow suppression. The nurse should assess the patient for which of the following manifestations that indicate bone marrow suppression?
Explanation
Choice B reason:
These are signs of infection, which can occur when the bone marrow is suppressed and cannot produce enough white blood cells to fight off germs. White blood cells are part of the immune system and help protect the body from infections. A low white blood cell count is called neutropenia, and it increases the risk of developing serious infections that may require hospitalization or antibiotics. The nurse should assess the patient for fever, chills, sore throat, or any other symptoms of infection and report them to the provider immediately³.
Choice A reason:
These are common side effects of chemotherapy, but they are not directly related to bone marrow suppression. Nausea, vomiting, and diarrhea can occur due to the effects of chemotherapy on the digestive system or the brain. They can also cause dehydration and electrolyte imbalance, which can affect the blood cells. The nurse should assess the patient for nausea, vomiting, and diarrhea and provide antiemetics, fluids, and electrolytes as ordered.
Choice C reason:
These are also common side effects of chemotherapy, but they are not directly related to bone marrow suppression. Hair loss, dry skin, and brittle nails can occur due to the effects of chemotherapy on the cells that produce hair and skin. They can also affect the patient's selfesteem and body image. The nurse should assess the patient for hair loss, dry skin, and brittle nails and provide supportive care and education.
Choice D reason:
These are signs of a cardiac problem, such as a heart attack or an arrhythmia. They are not directly related to bone marrow suppression. However, some chemotherapy drugs can affect the heart and cause cardiotoxicity, which can lead to heart failure or damage. The nurse should assess the patient for chest pain, dyspnea, and palpitations and report them to the provider immediately.
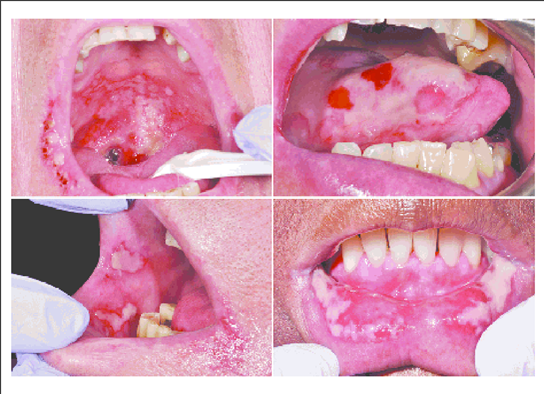
A nurse is providing supportive care to a patient who has lymphoma and is receiving chemotherapy that causes mucositis. The nurse should implement which of the following interventions to help the patient with mucositis?
Explanation
Choice D reason:
These are all interventions that can help the patient with mucositis, which is inflammation and ulceration of the mucous membranes in the mouth and throat. Mucositis can occur as a side effect of chemotherapy or radiotherapy that affects the rapidly dividing cells in the oral cavity. Mucositis can cause pain, difficulty swallowing, increased risk of infection, and reduced quality of life³.
Choice A reason:
Encouraging oral hygiene with a soft toothbrush or sponge and a mild mouthwash or saline solution can help prevent or reduce mucositis by keeping the mouth clean and moist. Oral hygiene can also prevent bacterial growth and infection in the mouth. The nurse should instruct the patient to avoid alcoholbased mouthwashes, as they can irritate the mucous membranes³.
Choice B reason:
Administering topical anesthetics or analgesics as prescribed can help relieve pain and discomfort caused by mucositis. Topical agents can numb the mouth and throat and allow the patient to eat and drink more comfortably. Systemic analgesics may also be needed for severe pain. The nurse should assess the patient's pain level and administer pain relief as ordered³.
Choice C reason:
Offering soft, bland, moist foods and fluids at room temperature or cooler can help the patient with mucositis by avoiding further irritation of the mucous membranes. Soft foods are easier to swallow and less likely to cause bleeding or damage to the ulcers. Bland foods are less likely to cause a burning sensation or inflammation. Moist foods and fluids can keep the mouth hydrated and prevent dryness. Room temperature or cooler foods and fluids can soothe the mouth and throat and reduce swelling³.
Sign Up or Login to view all the 4 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

