OB_Pediatric_Cumulative_Exam_Test_4_V _1_2023
Total Questions : 46
Showing 25 questions, Sign in for moreMagnesium sulfate is given to women with preeclampsia and eclampsia to:
Explanation
Magnesium sulfate is given to women with preeclampsia and eclampsia to prevent and treat convulsions.
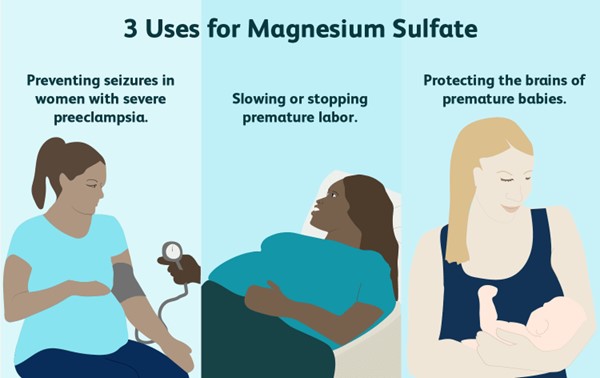
Magnesium sulfate is a mineral that reduces seizure risks in women with preeclampsia. A healthcare provider will give the medication intravenously. Sometimes, it’s also used to prolong pregnancy for up to two days. This allows drugs that speed up your baby’s lung development to be administered.
Choice A is wrong because magnesium sulfate does not improve patellar reflexes or increase respiratory efficiency. In fact, it may cause decreased or absent deep tendon reflexes and respiratory depression as side effects.
Choice B is wrong because magnesium sulfate does not shorten the duration of labor. It may actually prolong labor by inhibiting uterine contractions.
Choice D is wrong because magnesium sulfate does not prevent a boggy uterus or lessen the lochial flow. It has no effect on uterine tone or bleeding after delivery.
A pregnant woman has been receiving a magnesium sulfate infusion for the treatment of severe preeclampsia for 24 hours.
On assessment, the nurse finds the following vital signs: temperature of 37.3° C, pulse rate of 88 beats/min, respiratory rate of 10 breaths/min, blood pressure (BP) of 148/90 mm Hg, absent deep tendon reflexes, and no ankle clonus.
The patient complains, “I’m so thirsty and warm.” The nurse:
Explanation
The patient is showing signs of magnesium toxicity, such as respiratory depression, hyporeflexia, and flushing.
Magnesium sulfate is a high-alert medication that can cause serious adverse effects if not monitored closely.
The nurse should stop the infusion immediately and notify the provider.
Choice A is wrong because calling for a stat magnesium sulfate level will not address the immediate problem of toxicity.
The nurse should act quickly to prevent further complications.
Choice B is wrong because administering oxygen will not reverse the effects of magnesium toxicity.
Oxygen may be helpful for respiratory distress, but it will not correct the underlying cause.
Choice D is wrong because hydralazine is an antihypertensive medication that lowers blood pressure.
The patient’s blood pressure is already within the normal range for a pregnant woman with preeclampsia (140-160/90-110 mm Hg).
Hydralazine may cause hypotension and fetal distress.
A woman is in her seventh month of pregnancy.
She has been reporting nasal congestion and occasional epistaxis. The nurse suspects that:
Explanation
This is a normal respiratory change in pregnancy caused by elevated levels of estrogen. Estrogen increases blood flow and causes the nasal mucosa to swell, leading to congestion and nosebleeds. This condition is called pregnancy rhinitis and affects up to 20% of pregnant women.
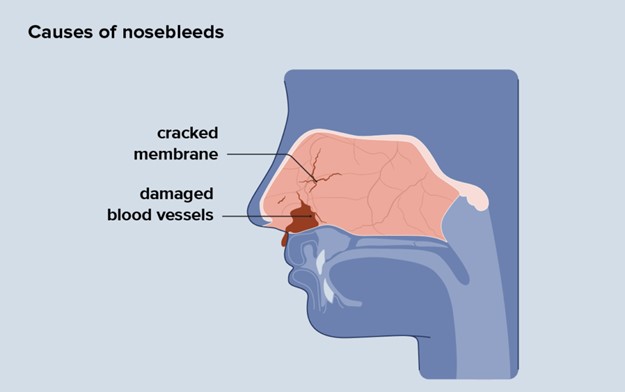
Choice B is wrong because this is not an abnormal cardiovascular change, and the nosebleeds are not an ominous sign. They are usually harmless and do not affect the pregnancy outcome.
Choice C is wrong because there is no evidence that the woman is a victim of domestic violence.
This is a serious accusation that should not be made without proper assessment and screening.
Choice D is wrong because there is no indication that the woman has been using cocaine intranasally. Cocaine use can cause nasal damage and bleeding, but it can also have other signs and symptoms such as agitation, euphoria, dilated pupils, increased heart rate and blood pressure, and risk of miscarriage or preterm labor.
Which infant would be more likely to have Rh incompatibility?
Explanation
choice A.
Infant of an Rh-negative mother and a father who is Rh-positive and homozygous for the Rh factor.
Rh incompatibility occurs when a woman is Rh-negative and her baby is Rh-positive. This can cause hemolytic disease of the neonate (HDN), a condition where the mother’s antibodies destroy the baby’s red blood cells.
Choice B is wrong because if both the mother and the baby are Rh-negative, there is no risk of Rh incompatibility.
Choice C is wrong because if the father is heterozygous for the Rh factor, there is a 50% chance that the baby will be Rh-negative and not affected by Rh incompatibility.
Choice D is wrong because if both the mother and the baby are Rh-positive, there is no risk of Rh incompatibility.
Human immunodeficiency virus (HIV) may be perinatally transmitted:
Explanation
The correct answer is choice D. Perinatal transmission of HIV is when HIV is passed from a woman with HIV to her child during pregnancy, childbirth, or breastfeeding.
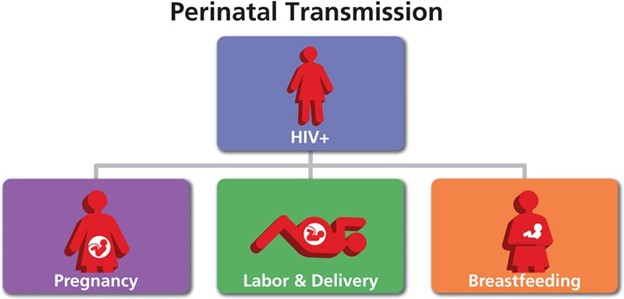
Breast milk from an infected mother can contain HIV and infect the baby.
Choice A is wrong because HIV can be transmitted at any stage of pregnancy, not only in the third trimester.
Choice B is wrong because needlestick injury is not a common mode of perinatal transmission of HIV. It is more likely to occur among health care workers who are exposed to contaminated needles or sharp objects.
Choice C is wrong because HIV can also be transmitted through the ingestion of amniotic fluid, but it is not the only way. Amniotic fluid is the fluid that surrounds and protects the baby in the womb.
A premature infant with respiratory distress syndrome receives artificial surfactant. How would the nurse explain surfactant therapy to the parents?
Explanation
choice A. Surfactant improves the ability of your baby’s lungs to exchange oxygen and carbon dioxide.
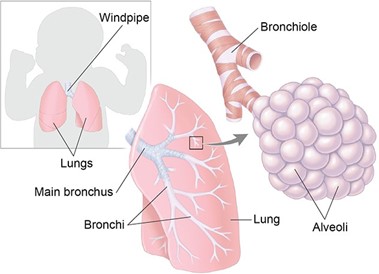
Surfactant is a substance that coats the inner surface of the alveoli, the tiny air sacs in the lungs.
It reduces the surface tension of the alveoli and prevents them from collapsing during exhalation.
Premature infants often lack enough surfactant, which leads to respiratory distress syndrome (RDS).
Artificial surfactant is given to these infants to help them breathe more easily. Choice B is wrong because surfactant has nothing to do with sedation.
Sedation is a state of reduced consciousness induced by drugs. Surfactant does not affect the level of consciousness of the infant.
Choice C is wrong because surfactant is not used to reduce episodes of periodic apnea.
Periodic apnea is a condition where the infant stops breathing for a short time, usually due to immature brainstem function.
Surfactant does not affect the brainstem or the control of breathing.
Choice D is wrong because surfactant is not used to fight a possible respiratory tract infection. Surfactant does not have any antibacterial or antiviral properties.
Surfactant is used to treat RDS, which is caused by a lack of surfactant, not by an infection.
A macrosomic infant is born after a difficult forceps-assisted delivery.
After stabilization, the infant is weighed, and the birth weight is 4550 g (9 lbs, 6 ounces). The nurse’s most appropriate action is to:
Explanation
choice D. Monitor blood glucose levels frequently and observe closely for signs of hypoglycemia. This is because a macrosomic infant (a newborn who’s much larger than average) is at risk of developing low blood sugar levels after birth, especially if the mother has diabetes. Hypoglycemia can cause neurological damage in the newborn, so it is important to detect and treat it promptly.
Choice A is wrong because leaving the infant in the room with the mother without monitoring the blood glucose levels may miss signs of hypoglycemia and delay treatment.
Choice B is wrong because taking the infant immediately to the nursery may separate the infant from the mother and interfere with breastfeeding, which can help prevent hypoglycemia.
Choice C is wrong because performing a gestational age assessment to determine whether the infant is large for gestational age is not urgent and does not address the risk of hypoglycemia.
Normal ranges for blood glucose levels in term infants are 2.6 mmol/L or higher at any time. A blood glucose level of 2.5 mmol/L or less is considered hypoglycemic.
The nurse administers vitamin K to the newborn for which reason?
Explanation
Bacteria that synthesize vitamin K is not present in the newborn’s intestinal tract. Vitamin K is essential for blood clotting, and newborns are at risk of bleeding problems due to their lack of vitamin K. Therefore, vitamin K is given by injection to prevent hemorrhagic disease in the newborn.
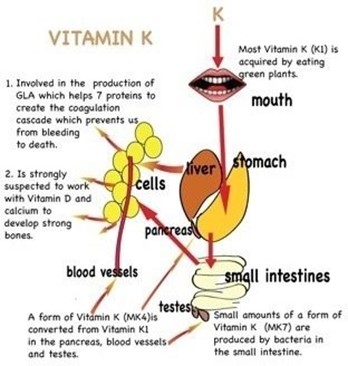
Choice A is wrong because most mothers do not have a diet deficient in vitamin K, and vitamin K deficiency in newborns is not related to the maternal diet.
Choice B is wrong because vitamin K does not prevent the synthesis of prothrombin in the liver, but rather enhances it. Prothrombin is a clotting factor that requires vitamin K for its production.
Choice D is wrong because the supply of vitamin K is not inadequate for at least 3 to 4 months, but rather for a few days until the newborn’s intestinal bacteria start producing it.
An Apgar score of 10 at 1 minute after birth would indicate a(n):
Explanation
An Apgar score of 10 at 1 minute after birth indicates that the infant is having no difficulty adjusting to extrauterine life but who should be assessed again at 5 minutes after birth. The Apgar score is a scoring system that evaluates the health of newborns at 1 and 5 minutes after birth based on five criteria: appearance, pulse, grimace, activity, and respiration. Each criterion is scored from 0 to 2, and the total score ranges from 0 to 10. A score of 7 to 10 is considered reassuring, a score of 4 to 6 is moderately abnormal, and a score of 0 to 3 is concerning.
Choice A is wrong because an Apgar score of 10 at 1 minute does not mean that the infant needs no further testing. The infant should still be assessed again at 5 minutes and monitored for any signs of distress or complications.
Choice B is wrong because an Apgar score of 10 at 1 minute does not indicate an infant in severe distress who needs resuscitation. An Apgar score of 0 to 3 would indicate a concerning condition that may require immediate intervention.
Choice C is wrong because an Apgar score of 10 at 1 minute does not predict a future free of neurologic problems. The Apgar score alone cannot be considered as evidence of, or a consequence of, asphyxia or brain injury; it does not predict individual neonatal mortality or neurologic outcome; and it should not be used for that purpose.
Normal ranges for each criterion are as follows:
- Appearance (color): pink all over (2 points), body pink but extremities blue (1 point), blue, bluish-gray, or pale all over (0 points)
- Pulse (heart rate): greater than 100 beats per minute (2 points), less than 100 beats per minute (1 point), absent (0 points)
- Grimace (response to stimulation): cough or sneeze, cry and withdrawal of foot with stimulation (2 points), facial movement/grimace with stimulation (1 point), absent (0 points)
- Activity (muscle tone): active movement (2 points), limbs flexed (1 point), limp or floppy (0 points)
- Respiration (breathing): good, strong cry (2 points), irregular, weak crying (1 point), absent (0 points)
A newborn is jaundiced and receives phototherapy via ultraviolet bank lights.
An appropriate nursing intervention when caring for an infant with hyperbilirubinemia and receiving phototherapy by this method would be to:
Explanation
Placing eye shields over the newborn’s closed eyes. This is because phototherapy can cause eye damage and irritation to the newborn, so eye protection is essential.
Choice A is wrong because oil-based lotion can increase the absorption of heat and cause burns to the newborn’s skin.
Choice B is wrong because limiting the newborn’s intake of milk can cause dehydration and increase the risk of hyperbilirubinemia.
Choice D is wrong because changing the newborn’s position every 4 hours is not frequent enough to prevent pressure ulcers and ensure even exposure to the light.
Normal ranges for bilirubin levels in newborns are 1 to 12 mg/dL for term infants and 3 to 14 mg/dL for preterm infants. Phototherapy is usually indicated when the bilirubin level exceeds 15 mg/dL for term infants and 10 mg/dL for preterm infants.
Nurses can prevent evaporative heat loss in the newborn by:
Explanation
Drying the baby after birth and wrapping the baby in a dry blanket

This prevents evaporative heat loss, which occurs when water on the skin surface evaporates and cools the skin. Evaporative heat loss is especially significant in newborns because they are wet at birth and have a large surface area relative to their body mass.
Choice B is wrong because it addresses convective heat loss, which occurs when air currents blow over the skin and carry away heat.
Convective heat loss can be prevented by keeping the baby out of drafts and away from air conditioners.
Choice C is wrong because it addresses radiant heat loss, which occurs when heat radiates from the skin to cooler objects in the environment.
Radiant heat loss can be prevented by placing the baby away from the outside wall and the windows.
Choice D is wrong because it addresses conductive heat loss, which occurs when heat transfers from the skin to cooler objects in contact with the skin.
Conductive heat loss can be prevented by warming the stethoscope and the nurse’s hands before touching the baby.
Normal body temperature for a newborn is 36.5°C to 37.5°C (97.7°F to 99.5°F).
The cheese-like, whitish substance that fuses with the epidermis and serves as a protective coating is called:
Explanation
Vernix caseosa is a cheese-like, whitish substance that fuses with the epidermis and serves as a protective coating for the newborn.

Some possible explanations for the other choices are:
- Choice B. Surfactant is a protein that lines the alveoli of the infant’s lungs and helps prevent them from collapsing.
- Choice C. Caput succedaneum is a swelling of the tissue over the presenting part of the fetal head caused by pressure during delivery.
- Choice D. Acrocyanosis is a bluish discoloration of the hands and feet due to reduced peripheral circulation.
Normal ranges for vernix caseosa are not applicable as it varies depending on the gestational age and skin maturity of the newborn. However, it is usually more abundant in preterm infants than in term or post-term infants.
As relates to rubella and Rh issues, nurses should be aware that:.
Explanation
The presence or absence of anxiety is a noninvasive assessment that the RN would perform to evaluate the patient’s psychological status and possible signs of hypovolemic shock.
Anxiety can indicate reduced cerebral perfusion due to blood loss and low blood pressure.
Choice A is wrong because pulse oximetry is a noninvasive assessment that the RN would perform to measure the oxygen saturation of the patient’s blood, not the circulatory status.
Choice B is wrong because heart sounds are a noninvasive assessment that the RN would perform to auscultate the cardiac rhythm and rate of the patient, not the circulatory status.
Choice C is wrong because arterial pulses are a noninvasive assessment that the RN would perform to palpate the strength and quality of the patient’s peripheral pulses, not the circulatory status.
Choice D is wrong because skin color, temperature, and turgor are noninvasive assessments that the RN would perform to observe the skin integrity and hydration of the patient, not the circulatory status.
Normal ranges for pulse oximetry are 95% to 100%, for heart rate, are 60 to 100 beats per minute, and for blood pressure are 120/80 mmHg.
Because a full bladder prevents the uterus from contracting normally, nurses intervene to help the woman empty her bladder spontaneously as soon as possible.
If all else fails, the last thing the nurse could try is:
Explanation

This is because oil peppermint can stimulate the micturition reflex and help the woman to void.
Some possible explanations for the other choices are:
Choice A is wrong because pouring water over the perineum may not be enough to trigger the micturition reflex and may cause discomfort or infection.
Choice C is wrong because analgesics may not address the underlying cause of urinary retention and may have side effects such as drowsiness or nausea.
Choice D is wrong because inserting a sterile catheter is an invasive procedure that carries risks such as trauma, infection, or bladder spasms. It should be used only as a last resort after other methods have failed.
Normal ranges for postpartum bladder function are:
- Urine output: 3000 to 5000 mL/day for the first 2 to 3 days after delivery.
- Urine specific gravity: 1.005 to 1.030.
- Urine pH: 4.6 to 8.0.
A 25-year-old gravida 2, para 2-0-0-2 gave birth 4 hours ago to a 9-lb, 7-ounce boy after augmentation of labor with Pitocin.
She puts on her call light and asks for her nurse right away, stating, “I’m bleeding a lot.” The most likely cause of afterbirth hemorrhage in this woman is:
Explanation
Uterine atony.
This is when the uterus does not contract enough to stop the bleeding from the placental site after delivery. It is the most common cause of postpartum hemorrhage, accounting for up to 80% of cases. Uterine atony can be caused by factors such as prolonged or augmented labor, large baby, multiple pregnancies, infection, or retained placenta.
The woman in question has some risk factors for uterine atony, such as a large baby and augmentation of labor with Pitocin.
The other choices are wrong because:
A . Retained placental fragments: This is when parts of the placenta remain attached to the uterine wall and prevent it from contracting properly. It is the second most common cause of postpartum hemorrhage.
However, there is no indication in the question that the woman had any difficulty with the delivery of the placenta or that it was incomplete
B. Unrepaired vaginal lacerations: This is when there are tears or cuts in the vagina or cervix that cause bleeding. It is a less common cause of postpartum hemorrhage.
However, there is no indication in the question that the woman had any trauma during delivery or that she was examined for lacerations
D. Puerperal infection: This is when there is an infection in the uterus or other parts of the reproductive tract after delivery.
It can cause fever, pain, and bleeding. It is a rare cause of postpartum hemorrhage.
However, there is no indication in the question that the woman had any signs or symptoms of infection, such as fever, chills, or foul-smelling discharge.
Normal ranges for blood loss after delivery are less than 500 mL for vaginal birth and less than 1000 mL for C-section.
Any amount above these thresholds can be considered postpartum hemorrhage and requires prompt evaluation and treatment.
What is an important nursing responsibility when dealing with a family experiencing the loss of an infant from sudden infant death syndrome (SIDS)?
Explanation
choice D. Make a follow-up home visit to parents as soon as possible after the infant’s death. This is because a competent, qualified professional should visit the family at home as soon as possible after the death and provide the family with printed information about SIDS.
Choice A is wrong because explaining how SIDS could have been predicted and prevented is inappropriate.
SIDS cannot be prevented or predicted. Discussions about the cause will only increase parental guilt.
Choice B is wrong because the parents should be asked only factual questions to determine the cause of death. Interviewing parents in-depth concerning the circumstances surrounding the infant’s death may be intrusive and stressful.
Choice C is wrong because parents should be allowed and encouraged to make a last visit with their infant. Discouraging parents from making a last visit with the infant may deprive them of an opportunity to say goodbye and grieve.
The nurse is caring for a child with suspected diabetes insipidus. Which clinical manifestation would be observable?
Explanation
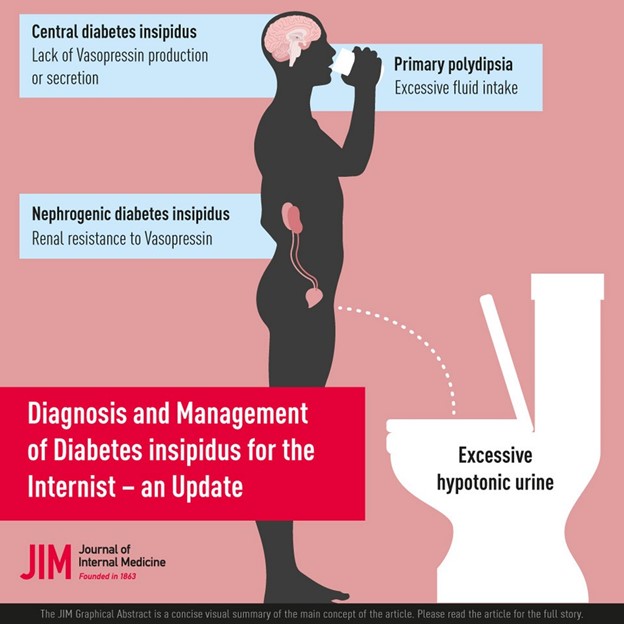
Diabetes insipidus is a disorder of the posterior pituitary gland that causes a deficiency of antidiuretic hormone (ADH). This leads to excessive urination (polyuria) and excessive thirst (polydipsia) as the body tries to balance the fluid loss. These symptoms may be so severe that the child does little other than drink and urinate.
Choice A is wrong because oliguria means decreased urine production and is not associated with diabetes insipidus.
Choice B is wrong because glycosuria means glucose in the urine and is associated with diabetes mellitus, not diabetes insipidus.
Choice C is wrong because nausea and vomiting are associated with inappropriate ADH secretion (SIADH), which causes fluid retention and hyponatremia, not diabetes insipidus.
Cystic fibrosis (CF) is suspected in a toddler. Which test is essential in establishing this diagnosis?
Explanation
This test measures the amount of chloride in the sweat, which is abnormally high in people with cystic fibrosis (CF). CF is an inherited disorder that affects the cells that produce mucus, sweat, and digestive juices.
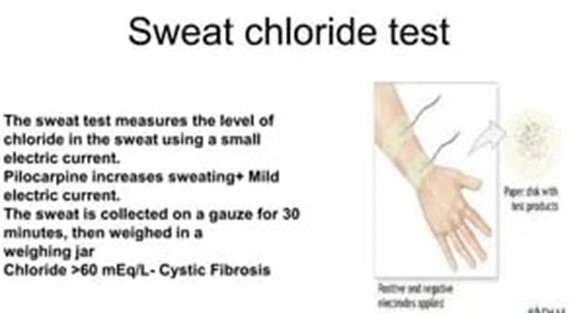
Choice A is wrong because bronchoscopy is a procedure that allows the doctor to examine the airways and lungs, but it is not essential for diagnosing CF.
Choice B is wrong because serum calcium is a blood test that measures the level of calcium in the blood, which is not related to CF.
Choice C is wrong because urine creatinine is a test that measures the amount of creatinine in the urine, which reflects the kidney function, but it is not relevant to CF.
Normal ranges for sweat chloride test are:
- Less than 40 millimoles per liter (mmol/L) for children and adults
- Less than 30 mmol/L for infants younger than 6 months
A sweat chloride level of more than 60 mmol/L is considered positive for CF.
A child is diagnosed with juvenile hypothyroidism. The nurse should expect to assess which symptoms are associated with hypothyroidism. (Select all that apply.).
Explanation
Sleepiness or fatigue and puffiness around the eyes are symptoms associated with hypothyroidism. Hypothyroidism is a condition where the thyroid gland does not produce enough thyroid hormones, which regulate the body’s metabolism and energy levels.
Choice A is wrong because weight loss is more likely to occur in hyperthyroidism, a condition where the thyroid gland produces too much thyroid hormones.
Choice C is wrong because diarrhea is also more likely to occur in hyperthyroidism, as the excess thyroid hormones speed up the digestive system.
Choice E is wrong because limited hair growth is not a specific symptom of hypothyroidism. Hair loss or thinning may occur in both hypothyroidism and hyperthyroidism, depending on the severity and duration of the condition.
Normal ranges for thyroid hormones are:
- TSH: 0.4 to 4.0 mIU/L
- T3: 100 to 200 ng/dL
- T4: 4.5 to 11.2 mcg/dL
What should the nurse stress in a teaching plan for the mother of an 11-year-old diagnosed with ulcerative colitis?
Explanation
Ulcerative colitis is a chronic inflammatory bowel disease that causes diarrhea, pain, and bleeding in the colon. Stress and certain foods can trigger or worsen the symptoms, so it is important to teach the mother how to help her son cope with stress and avoid triggers.
Choice A is wrong because ulcerative colitis is not an infectious disease that can spread to others.
Choice B is wrong because ulcerative colitis causes diarrhea, not constipation. Nutritional guidance is important, but not the main focus of teaching.
Choice C is wrong because the daily use of enemas is not part of the treatment plan for ulcerative colitis. Enemas can irritate the colon and cause more inflammation.
The nurse is meeting a 5-year-old child for the first time and would like the child to cooperate during a dressing change.
The nurse decides to do a simple magic trick using gauze. This should be interpreted as:
Explanation
A way to establish rapport. Doing a simple magic trick using gauze is a way to gain the child’s trust and attention, and to make the dressing change less stressful and more fun. This is appropriate for a 5-year-old child who is in the stage of initiative versus guilt according to Erikson’s theory of psychosocial development.
Choice A is wrong because 5-year-old children are curious and imaginative, and they enjoy magic tricks and fantasy play.
Choice C is wrong because a simple magic trick is not too distracting, but rather a way to engage the child and reduce anxiety.
Choice D is wrong because a simple magic trick is not inappropriate due to the child’s cognitive development. According to Piaget’s theory of cognitive development, 5-year-old children are in the preoperational stage, which means they can use symbols and language to represent objects and events.
A magic trick using gauze is a symbolic representation of something else, which the child can understand and appreciate.
A school-age child is admitted in vaso-occlusive sickle cell crisis.
The child’s care should include which intervention? (Select all that apply.)
Explanation
The child’s care should include adequate hydration and pain management. The management of an acute event of a vaso-occlusive crisis is the use of potent analgesics (opioids), rehydration with normal saline or Ringer’s lactate, treatment of malaria (whether symptomatic or not) using artemisinin combination therapy, and the use of oxygen via face mask, especially for acute chest syndrome.
Choice A is wrong because correction of acidosis is not a specific intervention for the vaso- occlusive crisis.
Acidosis may occur as a complication of sickle cell disease, but it is not the primary cause of the crisis.
Choice D is wrong because the administration of heparin is not recommended for the vaso-occlusive crisis.
Heparin is an anticoagulant that may increase the risk of bleeding and does not prevent or treat the sickling process.
Normal ranges for hemoglobin are 11.5 to 15.5 g/dl for children after 2 years of age.
Normal ranges for reticulocyte count are 0.5% to 1.5% for adults and 0.5% to 2.5% for children.
When caring for a child with Kawasaki disease, the nurse should understand that principle of care?
Explanation
Therapeutic management includes the administration of gamma globulin and aspirin. This is because Kawasaki disease causes inflammation in the walls of small to medium-sized blood vessels that carry blood throughout the body and can lead to complications such as coronary artery aneurysms. Gamma globulin is an intravenous immunoglobulin that can reduce the risk of these complications, and aspirin can help lower fever and inflammation.
Choice A is wrong because the child’s fever is usually not responsive to antibiotics within 48 hours. Kawasaki disease is not caused by a bacterial infection, so antibiotics are not effective.
Choice B is wrong because the principal area of involvement is not the joints. Kawasaki disease affects mainly the blood vessels, but it can also cause swelling in glands (lymph nodes) and mucous membranes inside the mouth, nose, eyes and throat. Joint pain or swelling may occur, but it is not the main feature of the disease.
Choice C is wrong because aspirin is not contraindicated. Aspirin is part of the standard treatment for Kawasaki disease, along with gamma globulin. However, aspirin should be used with caution and under medical supervision, as it can cause Reye’s syndrome in children with viral infections.
What is the nurse’s first action when planning to teach the parents of an infant with a congenital heart defect (CHD)?
Explanation
Assess the parents’ anxiety level and readiness to learn. This is because the nurse needs to evaluate the parent’s emotional state and their ability to comprehend and retain information before providing any teaching.
The nurse should also consider the parent'slearning style, cultural background, and literacy level.
Choice B is wrong because gathering literature for the parents is not the first action. The nurse should first assess the parents’ needs and preferences and then select appropriate materials that match their level of understanding and language.
Choice C is wrong because securing a quiet place for teaching is not the first action. The nurse should first assess the parents’ readiness to learn and then choose a suitable environment that minimizes distractions and promotes comfort.
Choice D is wrong because discussing the plan with the nursing team is not the first action. The nurse should first assess the parents’ anxiety level and readiness to learn and then collaborate with other health care professionals to provide consistent and accurate information.
What is the priority nursing goal for a 14-year-old diagnosed with Graves’ disease?
Explanation
Verbalizing the importance of monitoring for medication side effects.
Graves’ disease is an autoimmune disorder that causes hyperthyroidism, which means the thyroid gland produces too much thyroid hormone. This can lead to symptoms such as weight loss, increased appetite, nervousness, irritability, insomnia, heat intolerance, and palpitations. The medication methimazole is used to treat Graves’ disease by blocking the synthesis of thyroid hormone. However, methimazole can also cause serious side effects such as liver damage, agranulocytosis (low white blood cell count), and allergic reactions.
Therefore, the priority nursing goal for a 14 year old diagnosed with Graves’ disease is to verbalize the importance of monitoring for medication side effects and reporting them to the health care provider.
Choice A is wrong because relieving constipation is not a priority goal for Graves’ disease. Constipation is more likely to occur in hypothyroidism, which is the opposite of hyperthyroidism.
Choice B is wrong because allowing the adolescent to make decisions about whether or not to take medication is not a priority goal for Graves’ disease. While it is important to respect the adolescent’s autonomy and involve them in their care plan, they also need to understand the risks and benefits of taking medication and the consequences of not taking it.
Choice D is wrong because developing alternative educational goals is not a priority goal for Graves’ disease. Graves’ disease can affect the academic performance of adolescents due to cognitive and emotional changes caused by hyperthyroidism.
However, this does not mean that they need to change their educational goals. They may need extra support and accommodations from their teachers and parents to cope with their condition and achieve their potential.
Sign Up or Login to view all the 46 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

