Pathophysiology
Total Questions : 39
Showing 25 questions, Sign in for moreThe risk of developing coronary artery disease is increased up to threefold by
Explanation
Coronary artery disease (CAD) is a condition where the arteries that supply blood to the heart become narrowed or blocked due to a buildup of plaque. Several risk factors contribute to the development of CAD, including diabetes mellitus, hypertension, obesity, high alcohol consumption, smoking, and a family history of CAD.
Research suggests that individuals with diabetes mellitus are two to four times more likely to develop CAD than those without diabetes. This is because diabetes can lead to damage to the blood vessels and nerves that control the heart, as well as increased inflammation and high levels of blood glucose that can contribute to the buildup of plaque in the arteries.
While hypertension, obesity, and high alcohol consumption are also known risk factors for CAD, they generally do not increase the risk to the same degree as diabetes. Nonetheless, these factors can contribute to the development and progression of CAD and should be addressed through lifestyle modifications and medical interventions.
What is the usual source of pulmonary emboli
Explanation
A pulmonary embolism (PE) occurs when a blood clot, typically originating from the deep veins of the legs or pelvis, travels through the bloodstream and lodges in one of the pulmonary arteries in the lungs.
Deep venous thrombosis (DVT) is the most common source of pulmonary emboli. DVT occurs when a blood clot forms in the deep veins of the legs, pelvis, or arms, and can develop due to prolonged immobility, surgery, trauma, cancer, pregnancy, hormone therapy, or genetic factors.
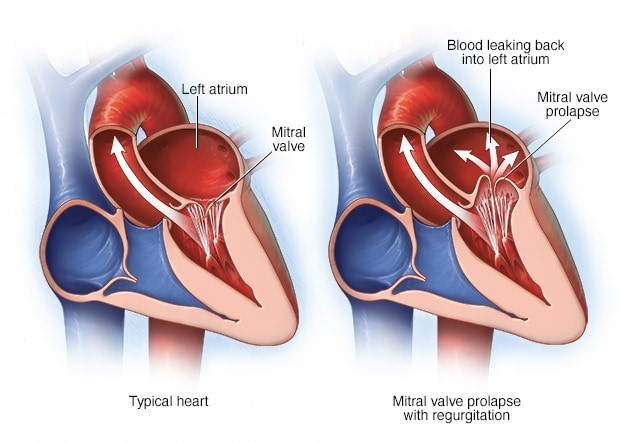
Endocarditis, valvular heart disease, and left heart failure are not typical sources of pulmonary emboli. Endocarditis is an infection of the heart valves and lining, which can lead to valve damage and heart failure, but does not usually cause blood clots. Valvular heart disease, which includes conditions such as aortic stenosis and mitral regurgitation, can cause blood flow disturbances and increase the risk of thrombosis, but does not directly cause blood clots. Left heart failure, which occurs when the left ventricle of the heart is unable to pump effectively, can cause fluid buildup in the lungs, but does not typically cause blood clots to form.
A patient is diagnosed with pulmonary disease and elevated pulmonary valvular resistance. Which of the following heart failures may result from this condition?
Explanation
Elevated pulmonary valvular resistance refers to a condition where there is increased resistance to blood flow through the pulmonary valve and into the lungs. This can lead to an increase in pressure within the right ventricle of the heart, which can eventually lead to right heart failure.
Right heart failure occurs when the right ventricle of the heart is unable to pump blood effectively, which can result in symptoms such as fatigue, shortness of breath, and fluid retention in the legs and abdomen. Causes of right heart failure include pulmonary hypertension, chronic obstructive pulmonary disease (COPD), pulmonary embolism, and other conditions that increase pressure within the pulmonary circulation.
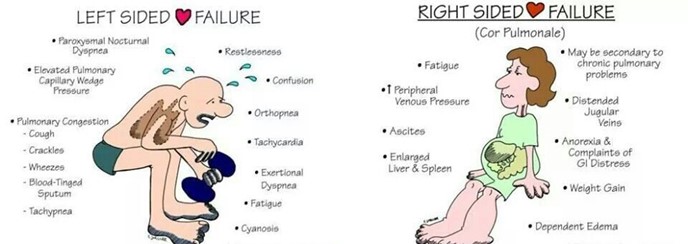
Left heart failure, on the other hand, occurs when the left ventricle of the heart is unable to pump blood effectively, which can lead to symptoms such as shortness of breath, fatigue, and fluid retention in the lungs and legs. Causes of left heart failure include coronary artery disease, hypertension, and valvular heart disease.
Low output failure occurs when the heart is unable to pump enough blood to meet the body's needs, and can result from a variety of conditions affecting the heart muscle or heart valves. High output failure occurs when the heart is working harder than normal to meet the body's demands, such as in conditions such as hyperthyroidism or severe anemia
What is the major effect of calcium channel blockers on cardiac contractions
Explanation
Calcium channel blockers (CCBs) are a class of medications that block the influx of calcium ions into cardiac and smooth muscle cells, leading to relaxation of these muscles and dilation of blood vessels.
In the heart, CCBs primarily affect the L-type calcium channels in the cardiac myocytes, which are responsible for the influx of calcium ions during the plateau phase of the cardiac action potential. By blocking these channels, CCBs decrease the amount of calcium that enters the cardiac myocytes, which in turn reduces the strength of cardiac contractions (i.e. contractility). 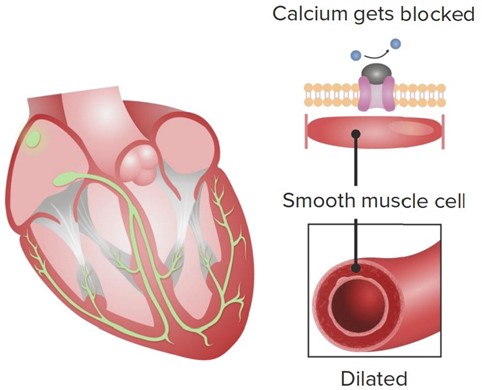
This reduction in contractility can be beneficial in certain conditions where the heart is working too hard or experiencing insufficient blood flow, such as in hypertension, angina, or some forms of arrhythmia. By reducing the workload of the heart, CCBs can help to lower blood pressure, decrease oxygen demand, and improve blood flow to the heart.
While CCBs can also have effects on the rate and rhythm of cardiac contractions, these effects are generally less pronounced than the reduction in contractility. Some CCBs, such as verapamil and diltiazem, can slow the heart rate by blocking the L-type calcium channels in the sinoatrial (SA) and atrioventricular (AV) nodes, while others, such as nifedipine, have little effect on heart rate.
The mitral and tricuspid valves close after the ventricles are filled with blood because the
Explanation
The mitral and tricuspid valves are located between the atria and ventricles in the heart, and they open and close to allow blood to flow in one direction through the heart. During diastole, when the heart is relaxed and filling with blood, the mitral and tricuspid valves are open to allow blood to flow from the atria into the ventricles.
Once the ventricles are filled with blood, they begin to contract during systole to pump the blood out to the lungs (right ventricle) and the rest of the body (left ventricle). As the ventricles contract, the pressure within them increases, which causes the mitral and tricuspid valves to be pushed closed by the blood within the ventricles. This closure prevents the backflow of blood into the atria during ventricular contraction (systole).
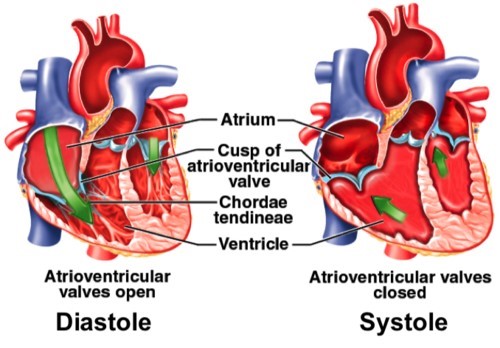
The chordae tendineae are thin, fibrous cords that connect the mitral and tricuspid valves to the papillary muscles within the ventricles. These structures help to anchor the valves in place during ventricular contraction, and prevent them from prolapsing (bulging back into the atria) and causing regurgitation (backflow of blood).
The trabeculae carneae are muscular ridges within the ventricles that help to increase the force of ventricular contraction, but they do not play a direct role in closing the mitral and tricuspid valves. Similarly, the reduced pressure in the atria during ventricular contraction is due to the fact that blood is being pumped out of the atria and into the ventricles, rather than the atria "pulling" the valves closed.
________ is the selective bulbous enlargement of the distal segment of a digit and is commonly associated with diseases that interfere with oxygenation of the blood
Explanation
Clubbing is a medical condition characterized by bulbous enlargement of the distal portion of a digit (usually a finger, but sometimes a toe) due to soft tissue proliferation and increased bone deposition. The affected digit takes on a rounded or "club-like" appearance, and the angle between the nail and nail bed (known as the Lovibond angle) increases to greater than 180 degrees.

Clubbing is commonly associated with a variety of medical conditions that interfere with oxygenation of the blood, including lung diseases such as chronic obstructive pulmonary disease (COPD), interstitial lung disease, and bronchiectasis; heart diseases such as congenital heart defects and cyanotic heart disease; and gastrointestinal diseases such as inflammatory bowel disease and cirrhosis.
The exact mechanism underlying clubbing is not fully understood, but it is thought to involve a combination of vascular, inflammatory, and neurogenic factors. Hypoxia (low oxygen levels) is believed to play a central role in the development
of clubbing, leading to the release of growth factors and cytokines that promote soft tissue and bone proliferation.
Clubbing is typically diagnosed based on physical examination findings, including the Lovibond angle and the presence of nail bed fluctuation (when the nail bed feels spongy or compressible). It is important to identify and treat any underlying medical conditions that may be contributing to clubbing, as these can have significant implications for the patient's health and quality of life.
Which elevated value may be protective of the development of atherosclerosis
Explanation
Atherosclerosis is a disease in which fatty deposits (plaques) build up in the walls of arteries, leading to narrowing and reduced blood flow. Elevated levels of certain lipids, including low density lipoprotein (LDL) cholesterol and triglycerides, are well-established risk factors for the development of atherosclerosis.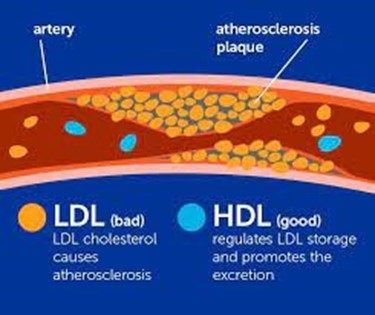
In contrast, high density lipoprotein (HDL) cholesterol has been shown to have a protective effect against atherosclerosis. HDL is often referred to as "good cholesterol" because it helps to transport excess cholesterol from peripheral tissues (including the walls of arteries) back to the liver for processing and excretion. HDL also has anti-inflammatory and antioxidant properties that may help to reduce the risk of atherosclerosis.
In general, higher levels of HDL cholesterol are associated with a lower risk of cardiovascular disease and atherosclerosis. However, the protective effect of HDL may vary depending on other factors such as smoking, obesity, and diabetes. It is important to maintain a healthy balance of lipids in the bloodstream, including a high level of HDL and low levels of LDL and triglycerides, in order to reduce the risk of atherosclerosis and other cardiovascular diseases.
Which of the following type of croup is most common
Explanation
Croup is a common respiratory illness in young children, characterized by inflammation of the upper airways (including the larynx and trachea) that leads to a characteristic barking cough and difficulty breathing. Croup is most commonly caused by viral infections, particularly parainfluenza virus, although other viruses such as respiratory syncytial virus (RSV) and influenza virus can also be responsible. 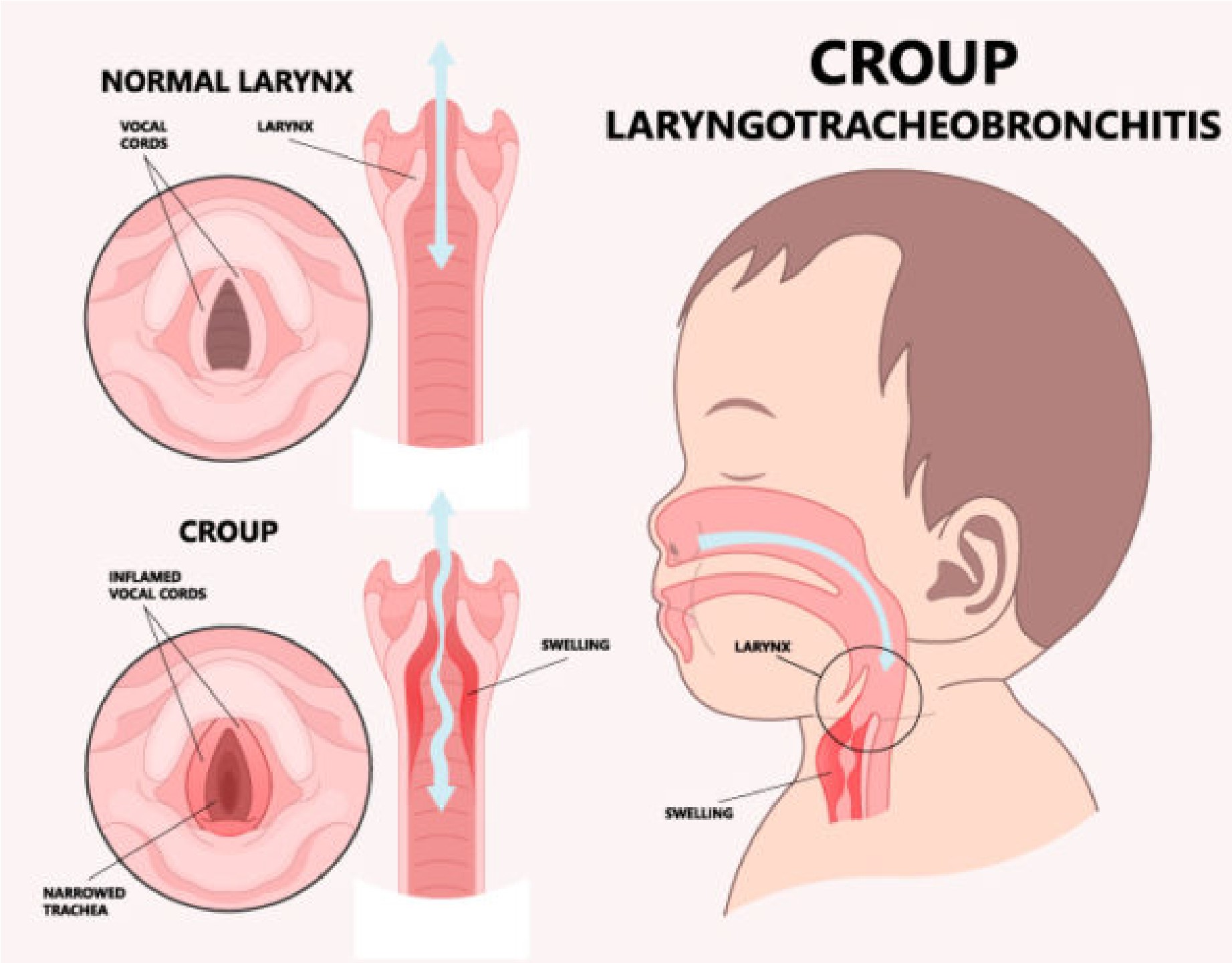
Bacterial croup is rare and usually occurs in children who have an underlying condition that makes them more susceptible to bacterial infections, such as immunodeficiency or a history of recurrent respiratory infections. Fungal croup is also rare and usually occurs in children with a weakened immune system or a history of exposure to contaminated soil or other environmental sources of fungi.
Autoimmune croup is not a recognized medical condition. While some autoimmune disorders can affect the respiratory system (such as systemic lupus erythematosus), they do not typically cause croup-like symptoms.
Patient wants to know what causes atherosclerosis. How should the nurse respond? In general, atherosclerosis is caused by
Explanation
Atherosclerosis is a complex disease process that involves the gradual buildup of plaques (fatty deposits) in the walls of arteries, leading to narrowing and reduced blood flow. The exact cause of atherosclerosis is not fully understood, but it is thought to involve a combination of genetic, lifestyle, and environmental factors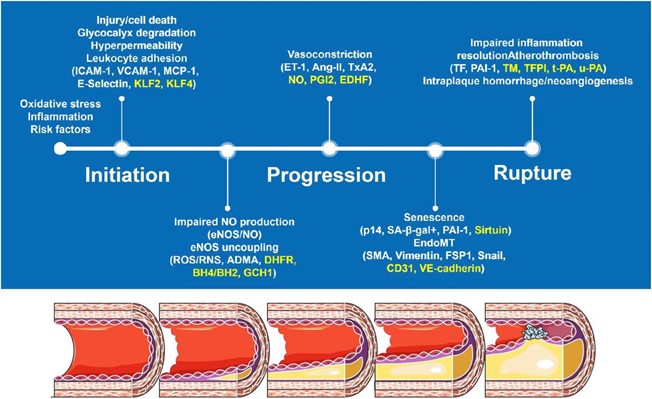
One of the key contributing factors to atherosclerosis is damage to the endothelial cells that line the walls of arteries. This damage can be caused by a variety of factors, including high blood pressure, smoking, high levels of lowdensity lipoprotein (LDL) cholesterol, and other inflammatory factors. When the endothelial cells are damaged, they release chemicals that attract white blood cells to the area. These white blood cells then migrate into the arterial wall, where they begin to accumulate and form fatty deposits called plaques.
Over time, these plaques can grow and calcify, leading to further narrowing of the artery and reducing blood flow to the affected tissue. In addition, plaques can rupture and form blood clots, which can completely block blood flow to the affected area and cause a heart attack or stroke.
While high serum cholesterol levels are a risk factor for atherosclerosis, they are not the sole cause. Similarly, an increase in antithrombotic substances (substances that prevent blood clots) and congenital heart disease are not primary causes of atherosclerosis, although they may contribute to the disease process in some cases.
The progression of chronic bronchitis is best halted by?
Explanation
Chronic bronchitis is a type of chronic obstructive pulmonary disease (COPD) that is characterized by inflammation and narrowing of the bronchial tubes, which can lead to symptoms such as cough, shortness of breath, and wheezing. The primary cause of chronic bronchitis is smoking, and the most effective way to halt its progression is by quitting smoking.
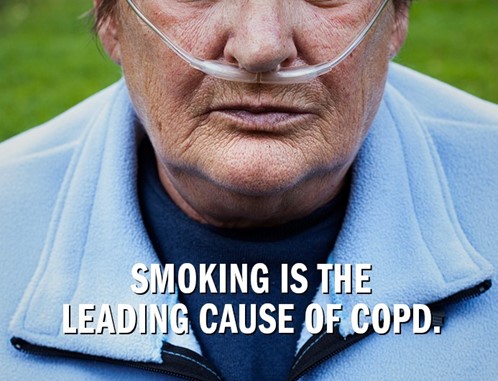
Smoking cessation is the cornerstone of treatment for chronic bronchitis, as continued smoking can worsen inflammation in the airways and accelerate the progression of the disease. In addition to smoking cessation, other treatments may include bronchodilators (such as albuterol) to help open the airways and improve breathing, postural chest drainage techniques to help clear mucus from the lungs, and antibiotics to treat bacterial infections.
While these treatments can help manage symptoms and prevent complications, they are not as effective as smoking cessation in halting the progression of chronic bronchitis. Therefore, it is important for individuals with chronic bronchitis to quit smoking as soon as possible to slow the disease process and improve their overall health.
Which factor is responsible for the hypertrophy of the myocardium associated with hypertension
Explanation
Hypertension, or high blood pressure, is a major risk factor for the development of left ventricular hypertrophy (LVH), which is characterized by thickening of the myocardium (heart muscle). LVH occurs in response to increased afterload (the resistance the heart has to pump against), which is a common feature of hypertension.
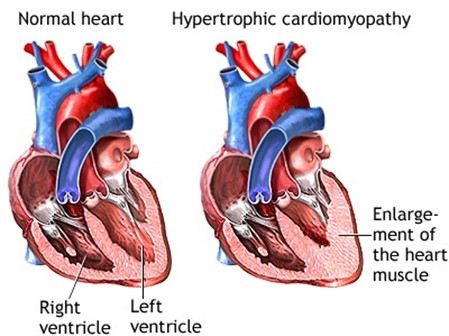
Angiotensin II, a hormone that is activated in response to hypertension, is a major mediator of LVH in this setting. Angiotensin II causes vasoconstriction (narrowing of blood vessels) and promotes the retention of salt and water, which increases blood volume and pressure. Additionally, angiotensin II stimulates the proliferation of cardiac myocytes (heart muscle cells) and the synthesis of extracellular matrix proteins, leading to hypertrophy and fibrosis of the myocardium.
Other factors that may contribute to LVH in hypertension include increased sympathetic nervous system activity, oxidative stress, and inflammation. However, angiotensin II is considered a key mediator of this process, and drugs that block the renin-angiotensin-aldosterone system (RAAS), such as angiotensinconverting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), are often used to treat hypertension and reduce the risk of LVH and other cardiovascular complications.
Which cardiac chamber has the thinnest wall and why?
Explanation
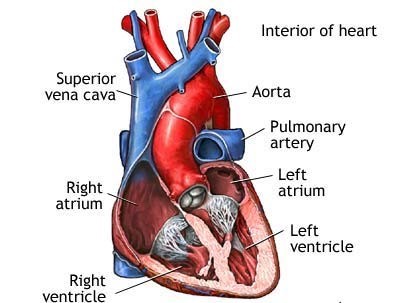
The walls of the atria are thin because they do not generate as much pressure as the ventricles, as their main function is to receive blood from the veins and pump it into the ventricles. The ventricles have thicker walls because they are responsible for generating the force necessary to pump blood out of the heart and into the systemic or pulmonary circulation.
Cystic fibrosis CF is caused by a
Explanation
Cystic fibrosis is a genetic disorder caused by mutations in the CFTR gene, which is inherited in an autosomal recessive manner. This means that a child must inherit two copies of the mutated gene (one from each parent) to develop the disorder. If only one parent carries a copy of the mutated gene, their children will not develop cystic fibrosis but may be carriers of the gene.
Complications of sustained hypertension include which of the following?
Explanation
Sustained hypertension can lead to several complications, including damage to the blood vessels in the retina (retinopathy), increased risk of stroke, and damage to the kidneys (renal disease). Other potential complications include heart disease, peripheral arterial disease, and cognitive impairment. It is important to manage hypertension through lifestyle modifications and medication to prevent these complications.
Patient was diagnosed with mitral stenosis. As a result the nurse realizes that the patient has incomplete emptying of the
Explanation
Mitral stenosis refers to a narrowing of the mitral valve, which is located between the left atrium and the left ventricle. This narrowing can cause incomplete emptying of blood from the left atrium into the left ventricle during diastole (relaxation phase) of the cardiac cycle. This can lead to increased pressure in the left atrium and pulmonary circulation, causing symptoms such as shortness of breath, fatigue, and pulmonary con
The nurse counts an adults heart beat at 110 beats per minute. The nurse describes this as
Explanation
Tachycardia refers to a heart rate that is faster than the normal range, which is typically considered to be between 60 and 100 beats per minute in adults. A heart rate of 110 beats per minute is above the normal range and is considered tachycardia.
Patient presents with dyspnea rapid, shallow breathing, inspiratory crackles, decreased lung compliance and hypoxemia. Tests reveal a fulminant form of respiratory failure characterized by acute lung inflammation and diffuse alveolocapillary injury. Which of the following is the most likely diagnosis the nurse will observe on the chart?
Explanation
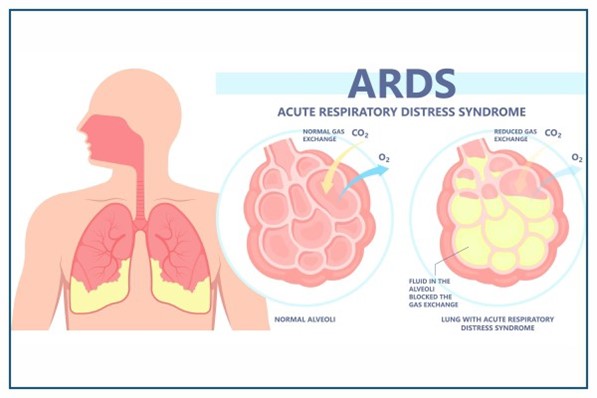
Acute respiratory distress syndrome (ARDS) is the most likely diagnosis based on the patient's symptoms and test results. ARDS is a serious condition that can develop in response to a variety of lung injuries, including pneumonia, sepsis, and trauma. The hallmark of ARDS is diffuse alveolocapillary injury, which leads to decreased lung compliance, hypoxemia, and respiratory distress. The symptoms of ARDS typically develop rapidly and include dyspnea, rapid, shallow breathing, inspiratory crackles, and hypoxemia. Treatment for ARDS typically involves supportive care, including oxygen therapy, mechanical ventilation, and treatment of the underlying cause of the lung injury.
Atherosclerosis causes an aneurysm by
Explanation
Atherosclerosis is a condition where plaque buildup occurs inside the arteries, which narrows the arterial lumen and limits blood flow. Aneurysms can occur as a result of atherosclerosis when the plaque formation weakens and damages the arterial wall, making it prone to bulging outwards or rupturing. This weakening of the vessel wall can cause it to lose its elasticity and strength, leading to the formation of an aneurysm. Therefore, the correct answer is C - eroding the vessel wall.
What term is used to identify when a cell is temporarily deprived of blood supply
Explanation
Ischemia refers to the temporary deprivation of blood supply to a particular tissue or organ, resulting in reduced oxygen and nutrient delivery to cells. This can lead to cellular injury and, if prolonged, irreversible damage. Infarction, on the other hand, refers to the death of tissue due to prolonged ischemia. Necrosis is a type of cell death that occurs when cells are damaged or injured and cannot survive. Inflammation is the body's response to tissue injury or infection, and can be a result of ischemia or necrosis.
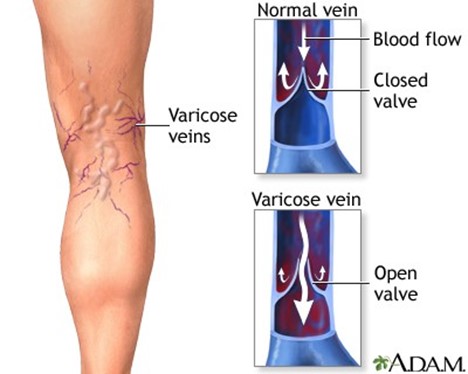
What changes in veins occur to create varicose veins
Explanation
Varicose veins occur when the valves within the veins, which normally prevent the backflow of blood, become damaged or weakened, allowing blood to pool and the veins to become enlarged and twisted. This can occur due to a variety of factors, including age, pregnancy, obesity, genetics, and prolonged periods of standing or sitting. An increase in hydrostatic pressure can contribute to the development of varicose veins, but it is not the primary cause.
A patient has a diagnosis of left ventricular failure. Which of the following signs and symptoms are associated with left ventricular failure?
Explanation
When the left ventricle is unable to pump blood effectively, blood backs up into the lungs, leading to pulmonary congestion and edema. This can cause symptoms such as shortness of breath, coughing, and wheezing. Decreased venous pressure and hyperoxygenation are not typically associated with left ventricular failure. Bradycardia may occur in some cases, but it is not a defining feature of left ventricular failure.
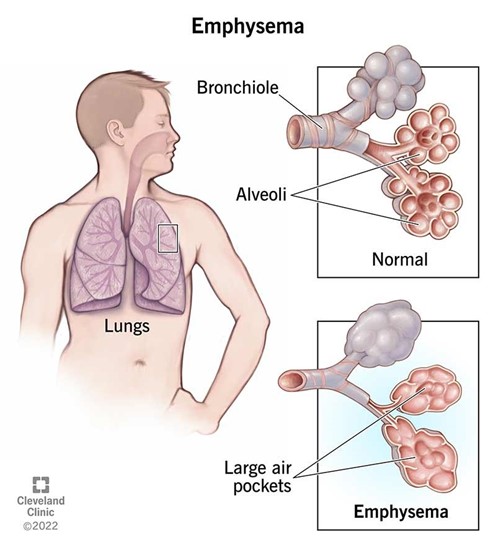
______ involves an abnormally enlarged gas exchange system and the destruction of alveolar walls
Explanation
Emphysema is a lung disease that involves damage to the alveoli (tiny air sacs in the lungs), causing them to become stretched out and lose their elasticity. This leads to an abnormally enlarged gas exchange system and the destruction of alveolar walls
Transudative effusion: An effusion is an abnormal buildup of fluid in a body cavity, such as the pleural cavity around the lungs. Transudative effusions occur when fluid leaks out of blood vessels due to changes in pressure or protein levels, rather than from inflammation or injury.
Exudate effusion: This type of effusion occurs when fluid leaks out of blood vessels due to inflammation or injury. The fluid contains high levels of protein and cellular debris, and may be caused by conditions such as pneumonia, cancer, or autoimmune disorders.
D. Abscess: An abscess is a localized collection of pus, usually caused by a bacterial infection. It can occur in various parts of the body, including the lungs.
An abscess in the lung can cause symptoms such as coughing, chest pain, and fever.
.
Chronic heart failure is associated with activation of the
Explanation
associated with chronic heart failure. Activation of the RAAS system occurs as a compensatory mechanism in response to decreased cardiac output and reduced renal perfusion. The renin-angiotensin-aldosterone system increases blood pressure, maintains blood volume and improves cardiac contractility in the short term, but in the long term it can lead to fluid retention, edema, and worsen cardiac function.
High attitudes may produce hypoxemia through
Explanation
At high altitudes, the air pressure is decreased, and there is less oxygen available in each breath. This leads to a decreased partial pressure of oxygen in the lungs, which can cause hypoxemia (low oxygen levels in the blood). Hyperventilation may initially help to increase oxygen delivery to the body, but it can also lead to respiratory alkalosis and decrease oxygen delivery to the tissues in the long run.
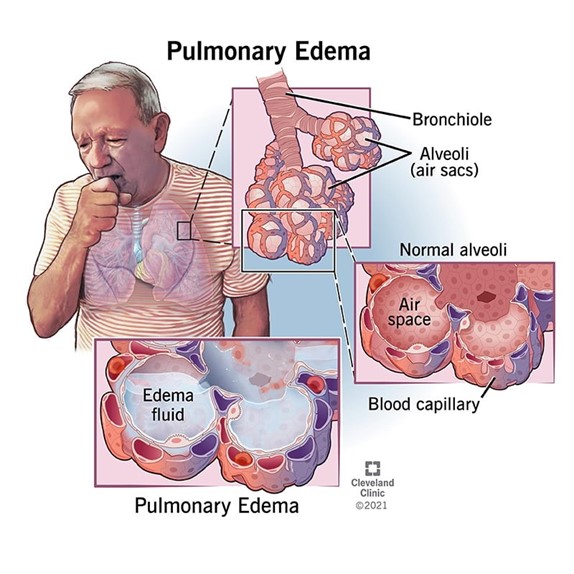
Continuous increases in left ventricular filling pressures result in which disorder
Explanation
Continuous increases in left ventricular filling pressures can lead to pulmonary edema, which is an accumulation of fluid in the lungs. Mitral regurgitation, mitral stenosis, and jugular vein distension are all conditions that can occur due to increased pressures in the left ventricle, but pulmonary edema is the most likely result of continuously increasing pressures.
Sign Up or Login to view all the 39 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

