Pediatrics Midterm V1 2023 Test 3
Total Questions : 75
Showing 25 questions, Sign in for moreA nurse is planning care for a 7-year-old child hospitalized with osteomyelitis. Which activities should the nurse plan to bring from the playroom for the child?
Explanation
The correct answer is choice E. Board games.
Choice A rationale:
Computer games might not be the best choice for a child with osteomyelitis. These games involve prolonged screen time and limited physical movement, which could potentially hinder the child's recovery.
Choice B rationale:
Paper and paints involve a level of physical activity that might not be suitable for a child with osteomyelitis. The child's movement might be restricted due to the condition, and activities that require fine motor skills might not be comfortable for them.
Choice C rationale:
Jack-in-the-box involves sudden surprises and might startle the child, which could be detrimental to their recovery. Children with osteomyelitis might be dealing with pain and discomfort, so it's important to avoid activities that could cause unnecessary distress.
Choice D rationale:
Stuffed animals might be a comforting option for the child. However, the child might also experience pain or discomfort when handling stuffed animals due to their condition. It's better to choose activities that don't involve physical contact that could potentially exacerbate the child's symptoms.
Choice E rationale:
Board games are a suitable choice for a child with osteomyelitis. They provide mental stimulation and entertainment without requiring excessive physical activity. Board games also promote social interaction if played with others, which is important for the child's emotional well-being during their hospital stay.

The nurse is providing education on tick removal. Which action would be incorrect?
Explanation
The correct answer is choice B. Grasp the tick by the body to remove.
Choice A rationale:
Cleansing the wound with soap and water is a correct action. This helps in preventing infection after tick removal. It's important to clean the area thoroughly to reduce the risk of any pathogens entering through the bite site.
Choice B rationale:
Grasping the tick by the body is incorrect. The proper way to remove a tick is to use fine-tipped tweezers and grasp it as close to the skin's surface as possible. Pull upward with steady, even pressure. Grasping the tick by the body could potentially cause the tick's mouthparts to break off and remain in the skin, increasing the risk of infection.
Choice C rationale:
Leaving the tick in place and seeking emergency medical treatment is incorrect. Ticks should be removed as soon as possible. Leaving a tick in place increases the risk of disease transmission. It's important to remove the tick properly to prevent potential complications.
Choice D rationale:
Avoiding touching the tick with bare hands is a correct action. Using fine-tipped tweezers is recommended for tick removal. Touching the tick with bare hands could expose you to any pathogens the tick might be carrying, increasing the risk of infection.
The nurse is evaluating a child who has been outside in the woods at camp. The child has multiple, small annular lesions without an indurated center on the arm. The nurse suspects Lyme disease.
Which stage of Lyme disease does the nurse believe that this child is exhibiting?
Explanation
The correct answer is choice B. First stage.
Choice A rationale:
There is no fourth stage of Lyme disease. Lyme disease typically progresses through three stages: early localized, early disseminated, and late disseminated. The symptoms mentioned in the question are more indicative of earlier stages of the disease.
Choice B rationale:
The child is likely exhibiting symptoms of the first stage of Lyme disease, known as early localized Lyme disease. This stage is characterized by the appearance of small annular (circular) lesions known as erythema migrans. These lesions are often red and have a clear center, resembling a "bull's-eye" pattern. This stage occurs within days to weeks after a tick bite and is usually accompanied by flu-like symptoms.
Choice C rationale:
There is no third stage of Lyme disease. The third stage is considered the late disseminated stage, which occurs months to years after the initial infection. It typically involves more severe symptoms, such as arthritis, neurological issues, and cardiac abnormalities.
Choice D rationale:
There is no second stage of Lyme disease. The second stage is the early disseminated stage, which occurs weeks to a few months after the tick bite. It involves the spread of the bacteria to other parts of the body, leading to symptoms such as multiple erythema migrans lesions, flu-like symptoms, fatigue, and muscle and joint pain.
A child is diagnosed with juvenile hypothyroidism. The nurse should expect to assess which symptoms associated with hypothyroidism?
Explanation
The correct answer is choice C. Sparse hair.
Choice A rationale:
Sleepiness is not a typical symptom of hypothyroidism. Hypothyroidism, a condition where the thyroid gland doesn't produce enough thyroid hormone, leads to a slower metabolism which can cause fatigue, but not necessarily sleepiness.
Choice B rationale:
Weight loss is not associated with hypothyroidism. In fact, weight gain is a common symptom due to the reduced metabolic rate caused by insufficient thyroid hormone levels.
Choice C rationale:
Sparse hair is a characteristic symptom of hypothyroidism. The thyroid hormones play a crucial role in the growth and maintenance of hair follicles. In hypothyroidism, hair can become brittle, thin, and sparse.

Choice D rationale:
Diarrhea is not a typical symptom of hypothyroidism. Constipation, on the other hand, is more commonly associated with this condition due to the slowed digestive processes caused by low thyroid hormone levels.
Choice E rationale:
Puffiness around the eyes is not typically associated with hypothyroidism. However, it is a symptom of another thyroid disorder known as Graves' disease, which is characterized by hyperthyroidism (overactive thyroid).
A child has come into the emergency department after a confirmed bite from a brown recluse. Which action can the nurse take to alleviate pain?
Explanation
The correct answers are choices B. Administer Benadryl, and D. Apply a cool compress.
Choice A rationale:
Placing an ace wrap on the bite is not recommended for a brown recluse spider bite. This action could potentially worsen the situation as it might trap venom in the area and increase the risk of necrosis.
Choice B rationale:
Administering Benadryl is a suitable action for alleviating pain and managing allergic reactions related to the bite. Benadryl (diphenhydramine) is an antihistamine that can help reduce itching and inflammation.
Choice C rationale:
Elevating the affected area might not provide significant pain relief for a brown recluse spider bite. Elevating is generally more effective for reducing swelling associated with injuries involving fluid accumulation, like sprains or strains.
Choice D rationale:
Applying a cool compress to the bite area can help alleviate pain and reduce inflammation. Cold therapy constricts blood vessels, which can reduce swelling and numb the area, providing relief.
A patient is taking acetaminophen (Tylenol) 325 mg, 2 tablets PO every 6 hours. How many grams is the patient receiving in 24 hours?
(Number Only, do not type in gram or g with your answer)
Explanation
The correct answer is 6 grams. To calculate the amount of acetaminophen (Tylenol) the patient is receiving in 24 hours, we can follow these steps: The patient is taking 2 tablets of acetaminophen 325 mg every 6 hours. 325 mg * 2 tablets = 650 mg every 6 hours. Since there are 4 sets of 6 hours in 24 hours (24 / 6 = 4), we multiply the dosage for one 6-hour period by 4 to find the daily dosage. 650 mg * 4 = 2600 mg (2.6 grams) in 24 hours.
So, the patient is receiving 2.6 grams of acetaminophen in 24 hours.
Exophthalmos may occur in children with what diagnosis?
Explanation
Choice A rationale:
Hypoparathyroidism is not associated with exophthalmos. Hypoparathyroidism is a condition where the parathyroid glands produce insufficient parathyroid hormone, leading to low calcium levels in the blood. This condition doesn't directly affect the thyroid gland or cause exophthalmos.
Choice B rationale:
Exophthalmos, also known as protruding or bulging eyes, is a classic symptom of hyperthyroidism. Hyperthyroidism is a condition where the thyroid gland produces excessive amounts of thyroid hormones. These elevated hormone levels can lead to a variety of symptoms, including increased metabolism, weight loss, nervousness, and protruding eyes due to inflammation of the eye muscles and tissues behind the eye.
Choice C rationale:
Hyperparathyroidism involves the overactivity of the parathyroid glands, leading to excessive production of parathyroid hormone (PTH) and elevated calcium levels in the blood. While elevated calcium levels can have various effects on the body, exophthalmos is not a typical manifestation of hyperparathyroidism. The condition is more commonly associated with bone and kidney issues.
Choice D rationale:
Hypothyroidism, the underproduction of thyroid hormones by the thyroid gland, is not linked to exophthalmos. Instead, hypothyroidism is known for causing symptoms such as fatigue, weight gain, cold intolerance, and slow heart rate. Exophthalmos is a characteristic sign of hyperthyroidism, not hypothyroidism.
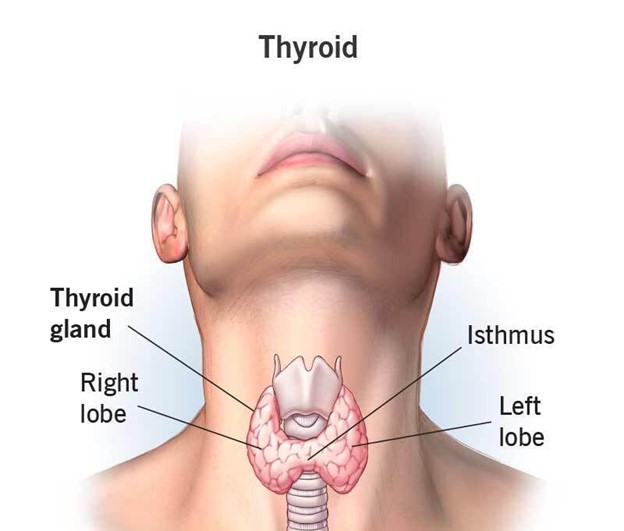
A goiter is an enlargement or hypertrophy of which gland?
Explanation
Choice A rationale:
A goiter refers to the enlargement or hypertrophy of the thyroid gland. This can occur due to various reasons, such as iodine deficiency, autoimmune disorders like Hashimoto's thyroiditis, or Graves' disease (which is associated with hyperthyroidism). The thyroid gland produces hormones that regulate metabolism and growth, and when it becomes enlarged, it can lead to visible swelling in the neck.
Choice B rationale:
The posterior pituitary gland is responsible for the release of hormones like vasopressin (antidiuretic hormone) and oxytocin. A goiter is not associated with the posterior pituitary gland. Issues with the posterior pituitary can lead to problems with water balance and uterine contractions, but not thyroid enlargement.
Choice C rationale:
The adrenal glands are responsible for producing hormones like cortisol and adrenaline. While adrenal disorders can lead to various hormonal imbalances, a goiter is not related to adrenal gland function. Adrenal issues might cause symptoms like fatigue, weight changes, and blood pressure irregularities.
Choice D rationale:
The anterior pituitary gland produces hormones that regulate the functions of other endocrine glands, including the thyroid gland. However, a goiter is not directly associated with the anterior pituitary. The anterior pituitary's malfunction can result in disorders like growth hormone deficiency or Cushing's disease, but not thyroid enlargement.
Calcium carbonate is given with meals to a child with chronic renal disease. The purpose of this is to achieve which desired result?
Explanation
Choice A rationale:
Calcium carbonate is often given with meals to individuals with chronic renal disease, especially those on dialysis. One of the primary purposes is to bind dietary phosphorus in the gastrointestinal tract. In chronic renal disease, the kidneys are less effective at filtering out excess phosphorus from the blood, leading to elevated phosphorus levels (hyperphosphatemia). Elevated phosphorus levels can contribute to bone and mineral disorders in these patients. Calcium carbonate forms insoluble calcium phosphate complexes with dietary phosphorus, preventing its absorption and facilitating its elimination from the body through the feces.
Choice B rationale:
While calcium carbonate can interact with fat-soluble vitamins like vitamin D, the primary reason for administering it to individuals with chronic renal disease is to manage phosphorus levels. Calcium carbonate can bind phosphorus and prevent its absorption, which is particularly important for patients with compromised kidney function.
Choice C rationale:
Stimulating appetite is not a primary purpose of administering calcium carbonate to children with chronic renal disease. The main focus is on managing phosphorus levels and preventing complications associated with hyperphosphatemia.
Choice D rationale:
Preventing vomiting is not a primary purpose of giving calcium carbonate to children with chronic renal disease. Calcium carbonate is typically used to manage phosphorus levels and complications related to hyperphosphatemia in this population.
The nurse is preparing an adolescent for discharge after a cardiac catheterization. Which statement by the adolescent would indicate the need for further teaching?
Explanation
The correct answer is choice B: "I have to stay on strict bed rest for 3 days."
Choice A rationale:
The statement "I should avoid tub baths but may shower" is correct. After a cardiac catheterization, the patient needs to keep the insertion site clean and dry to prevent infection. Showering is allowed, but tub baths should be avoided to minimize the risk of introducing water into the insertion site.
Choice B rationale:
The statement "I have to stay on strict bed rest for 3 days" is incorrect. Bed rest is not typically required after a cardiac catheterization. While the patient might need to lie flat for a few hours after the procedure to prevent bleeding and ensure hemostasis, strict bed rest for three days is unnecessary and could lead to complications like deep vein thrombosis (DVT) or deconditioning.
Choice C rationale:
The statement "I may attend school but should avoid exercise for several days" is correct. Attending school is generally acceptable after a cardiac catheterization, but exercise should be limited for several days to allow the insertion site to heal and to prevent complications like bleeding or hematoma formation.
Choice D rationale:
The statement "I should remove the pressure dressing the day after the procedure" is correct. Pressure dressings are typically removed by healthcare professionals after a specified period, which is usually around 24 hours after the procedure. Removing the dressing on their own the day after the procedure could lead to disruption of the wound and increase the risk of infection.
The diet of a child with nephrosis usually includes which requirement?
Explanation
The correct answer is choice C: "Salt restriction."
Choice A rationale:
The requirement of a high protein diet is not typically indicated for a child with nephrosis. Nephrosis, a condition characterized by excessive protein in the urine, indicates a need to reduce protein intake to alleviate kidney stress and proteinuria.
Choice B rationale:
A low fat diet is not a specific requirement for a child with nephrosis. The focus in nephrosis is primarily on protein and salt intake rather than fat content.
Choice C rationale:
Salt restriction is the correct requirement for a child with nephrosis. Nephrosis often leads to fluid retention and edema due to impaired kidney function. Restricting salt intake helps to reduce fluid retention and manage blood pressure.
Choice D rationale:
A high carbohydrate diet is not commonly prescribed for a child with nephrosis. While carbohydrates are a source of energy, they are not a primary consideration in managing nephrosis. The emphasis is more on protein and salt intake.
The nurse understands that hypospadias refers to what urinary anomaly?
Explanation
The correct answer is choice A: "Urethral opening along ventral surface of penis."
Choice A rationale:
The statement "Urethral opening along ventral surface of penis" is correct. Hypospadias is a congenital condition where the opening of the urethra is located on the underside of the penis rather than at the tip. This anomaly requires surgical correction.
Choice B rationale:
The statement "Urethral opening along dorsal surface of penis" is incorrect. This statement describes an anatomically incorrect condition. The opening of the urethra is not supposed to be along the dorsal surface of the penis.
Choice C rationale:
The statement "Absence of a urethral opening" is incorrect. This statement describes a more severe condition called "urethral agenesis" where the urethral opening is completely absent. Hypospadias is different and involves a misplaced urethral opening.
Choice D rationale:
The statement "Penis shorter than usual for age" is not related to hypospadias. Hypospadias primarily involves the location of the urethral opening and is unrelated to the length of the penis.
The nurse is admitting a child with rheumatic fever. Which therapeutic management should the nurse expect to implement?
Explanation
The correct answer is choice C: Administering penicillin.
Choice A rationale:
Imposing strict bed rest for 4 to 6 weeks. This choice is not the most appropriate therapeutic management for rheumatic fever. While rest is important during the acute phase, strict bed rest for 4 to 6 weeks is excessive and could lead to physical deconditioning and psychological distress for the child.
Choice B rationale:
Administering corticosteroids if chorea develops. This choice is relevant to the management of rheumatic fever but is not the primary treatment. Chorea is a movement disorder that can occur as a complication of rheumatic fever. Corticosteroids may be used to manage chorea symptoms, but they are not the mainstay of treatment for rheumatic fever itself.
Choice C rationale:
Administering penicillin. This is the correct choice. Penicillin is the mainstay of treatment for rheumatic fever. It helps eradicate the group A streptococcal infection that triggers the inflammatory response leading to rheumatic fever. Penicillin is essential to prevent further complications such as rheumatic heart disease.

Choice D rationale:
Avoiding salicylates (aspirin). This choice is also relevant to the management of rheumatic fever. Salicylates, including aspirin, are used to relieve symptoms and reduce inflammation. However, in children with acute rheumatic fever, salicylates are contraindicated due to the risk of developing Reye's syndrome, a serious condition that affects the brain and liver.
The nurse is caring for a school-age child with hyperthyroidism (Graves' disease). Which clinical manifestations should the nurse monitor that may indicate a thyroid storm? (Select all that apply.)
Explanation
The correct answers are choices A, C, and D: Tachycardia, Hyperthermia, and Vomiting.
Choice A rationale:
Tachycardia. Tachycardia, an abnormally fast heart rate, is a classic manifestation of thyroid storm. In this life-threatening condition, there is an excessive release of thyroid hormones, leading to increased metabolic rate and subsequent cardiovascular effects such as tachycardia.
Choice B rationale:
Constipation. This choice is incorrect for thyroid storm. Hyperthyroidism typically leads to increased bowel motility and can cause diarrhea rather than constipation.
Choice C rationale:
Hyperthermia. This is a correct choice. Thyroid storm is associated with severe hyperthermia due to the increased metabolic rate caused by excessive thyroid hormones. The body's temperature regulation is disrupted, leading to dangerously high body temperatures.
Choice D rationale:
Vomiting. This is a correct choice. Gastrointestinal symptoms, including vomiting and nausea, can occur in thyroid storm due to the heightened metabolic state. Thyroid storm affects various systems, including the gastrointestinal system, leading to symptoms like vomiting.
Choice E rationale:
Hypotension. This choice is incorrect for thyroid storm. Thyroid storm is more likely to cause hypertension rather than hypotension due to the increased cardiac output and sympathetic stimulation.
The nurse is caring for a 10-month-old infant diagnosed with respiratory syncytial virus (RSV) bronchiolitis. Which interventions should be included in the child's care? (Select all that apply.).
Explanation
The correct answers are choices A and E: Institute cluster care to encourage adequate rest and Place on noninvasive oxygen monitoring.
Choice A rationale:
Institute cluster care to encourage adequate rest. This is a correct choice. Cluster care involves grouping nursing interventions together to minimize disruptions to the child's rest. Adequate rest is crucial for the healing process in infants with respiratory syncytial virus (RSV) bronchiolitis.
Choice B rationale:
Administer cough syrup. This choice is incorrect for RSV bronchiolitis. Cough syrup is not recommended for infants with bronchiolitis. RSV primarily affects the lower respiratory tract and can cause airway inflammation, making cough syrup potentially ineffective and unnecessary.
Choice C rationale:
Administer antibiotics. This choice is incorrect for RSV bronchiolitis. RSV is a viral infection, and antibiotics are ineffective against viruses. Antibiotics should only be used when there is a bacterial infection or a clear indication.
Choice D rationale:
Encourage infant to drink 8 ounces of formula every 4 hours. This choice is not the best approach for managing RSV bronchiolitis. Infants with RSV may experience decreased appetite due to respiratory distress. Smaller, more frequent feedings are often recommended to prevent overfeeding and aspiration.
Choice E rationale:
Place on noninvasive oxygen monitoring. This is a correct choice. RSV bronchiolitis can cause respiratory distress and compromise oxygenation. Noninvasive oxygen monitoring helps assess the child's oxygen levels and aids in determining the need for supplemental oxygen therapy.
What is the initial goal for the treatment of secondary hypertension?
Explanation
The correct answer is choice C. Treating the underlying disease.
Choice A rationale:
Administration of digoxin. Administering digoxin is not the initial goal for the treatment of secondary hypertension. Digoxin is a medication commonly used to treat heart failure and certain arrhythmias, but it is not a primary intervention for hypertension. The rationale for this choice being incorrect lies in the fact that digoxin primarily affects the heart's contractility and is not a preferred option for managing high blood pressure.
Choice B rationale:
Weight control and diet. Weight control and dietary modifications are important aspects of managing hypertension, both primary and secondary. However, they are not the initial goal for the treatment of secondary hypertension. While these lifestyle modifications can contribute to blood pressure reduction, the primary focus in secondary hypertension is to identify and address the underlying condition causing the high blood pressure.
Choice C rationale:
Treating the underlying disease. Correct Answer. The initial goal for the treatment of secondary hypertension is to address the underlying disease or condition that is causing the elevated blood pressure. Unlike primary hypertension, which often lacks a specific underlying cause, secondary hypertension results from an identifiable condition such as kidney disease, hormonal disorders, or certain medications. Treating the root cause can lead to blood pressure normalization.
Choice D rationale:
Administration of β-adrenergic receptor blockers. Administering β-adrenergic receptor blockers is not typically the initial goal for the treatment of secondary hypertension. While these medications can lower blood pressure by blocking the effects of adrenaline and reducing heart rate, they are not the first-line approach for addressing the underlying cause of secondary hypertension.
What is an important nursing consideration when suctioning a young child who has had heart surgery?
Explanation
The correct answer is choice B. Administer supplemental oxygen before and after suctioning.
Choice A rationale:
Expect symptoms of respiratory distress when suctioning. While respiratory distress can occur during and after suctioning, it is not the main nursing consideration. The primary goal is to minimize any potential complications and ensure the child's safety during the procedure, which can be achieved by following appropriate guidelines.
Choice B rationale:
Administer supplemental oxygen before and after suctioning. Correct Answer. Administering supplemental oxygen before and after suctioning is crucial to maintain adequate oxygenation during and after the procedure. Suctioning can temporarily decrease oxygen levels and cause desaturation, especially in a child who has undergone heart surgery. Providing supplemental oxygen helps prevent hypoxia and supports respiratory function.
Choice C rationale:
Perform suctioning at least every hour. Frequent suctioning at least every hour is not a standard nursing practice, especially for a child who has had heart surgery. Suctioning should only be performed as needed based on the child's clinical condition, and excessive suctioning can irritate the airway and lead to complications.
Choice D rationale:
Suction for no longer than 30 seconds at a time. While limiting the duration of suctioning is important to prevent hypoxia and trauma to the airway, the specific duration of 30 seconds is not a universal rule. Suctioning should be performed for the shortest effective duration to minimize the risk of complications, but the optimal time can vary based on the child's condition and the type of suctioning being used.
A child is brought to the emergency department experiencing an anaphylactic reaction to a bee sting. While an airway is being established, what medication should the nurse prepare for immediate administration?
Explanation
The correct answer is choice B. Epinephrine.
Choice A rationale:
Diphenhydramine. Diphenhydramine is an antihistamine commonly used to relieve allergic symptoms such as itching, rash, and runny nose. While it can be part of the treatment for anaphylactic reactions, it is not the medication of choice for immediate administration in the case of a severe anaphylactic reaction like the one described in the scenario.
Choice B rationale:
Epinephrine. Correct Answer. In cases of severe anaphylactic reactions, epinephrine (adrenaline) is the medication of choice for immediate administration. Epinephrine acts rapidly to reverse life-threatening symptoms, such as airway constriction, low blood pressure, and hives. It works by dilating airways, increasing heart rate, and improving blood pressure.
Choice C rationale:
Dopamine. Dopamine is a medication used to increase blood pressure and cardiac output in certain critical situations. However, it is not the first-line treatment for anaphylactic reactions. Epinephrine's effects on airway and cardiovascular function make it the preferred choice in this context.
Choice D rationale:
Calcium chloride. Calcium chloride is not the appropriate medication for treating anaphylactic reactions. Its main medical uses include treating hypocalcemia (low blood calcium levels) and certain cardiac arrhythmias. It does not address the primary symptoms and physiological changes associated with anaphylaxis.
When providing education on Tinea capitis, what information should the nurse include?
Explanation
The correct answer is choice B: Lesions may extend to hairline or neck.
Choice A rationale:
Central clearing is not a prominent indicator of Tinea capitis. Tinea capitis is a fungal infection of the scalp and hair shafts, commonly caused by dermatophytes like Trichophyton species. The characteristic features include scaling, erythema, pustules, and hair loss. Unlike some other fungal infections, Tinea capitis does not typically have central clearing.
Choice B rationale:
Lesions extending to the hairline or neck is a correct aspect to include in education about Tinea capitis. The infection usually starts as small, scaly patches on the scalp and can progress to larger areas. It can extend to the hairline, neck, and even eyebrows and eyelashes. This is important information to convey to ensure proper recognition and timely treatment.
Choice C rationale:
Transmission of Tinea capitis mostly occurs from human-to-human rather than from dogs. While some animals can carry fungal infections that affect the skin, Tinea capitis is primarily spread through direct contact with an infected person or contaminated objects like combs, hats, and pillows.
Choice D rationale:
The appearance of Tinea capitis is not usually unilateral. This condition often presents with multiple, scattered areas of involvement on the scalp. It can cause varying degrees of inflammation, scaling, and hair loss in different areas, which may not follow a unilateral pattern.
What is a common side effect of corticosteroid therapy?
Explanation
Choice A rationale:
Increased appetite is a common side effect of corticosteroid therapy. Corticosteroids are known to affect various metabolic processes, and one of the effects is an increase in appetite. This can lead to weight gain, especially when the increased calorie intake is not balanced by physical activity.
Choice B rationale:
Fever is not a typical side effect of corticosteroid therapy. Corticosteroids are often used to reduce inflammation and suppress the immune response, which can help in managing conditions like autoimmune diseases, allergies, and inflammatory disorders. Fever is not a direct result of corticosteroid administration.
Choice C rationale:
Weight loss is not a common side effect of corticosteroid therapy. In fact, corticosteroids are more likely to cause weight gain due to their influence on appetite, metabolism, and fluid retention.
Choice D rationale:
Hypertension (high blood pressure) can indeed be a side effect of corticosteroid therapy. Corticosteroids can lead to sodium and water retention, which can contribute to increased blood pressure, particularly in individuals who are already at risk for hypertension. However, among the options provided, increased appetite is a more directly associated side effect of corticosteroid therapy.
What type of shock is characterized by a hypersensitivity reaction causing massive vasodilation and capillary leaks, which may occur with a drug or latex allergy?
Explanation
The correct answer is choice A: Anaphylactic shock.
Choice A rationale:
Anaphylactic shock is the correct answer. Anaphylactic shock is a severe and potentially life-threatening allergic reaction that causes massive vasodilation, capillary leakage, and bronchoconstriction. It can occur rapidly after exposure to an allergen such as certain foods, insect stings, medications, or latex. The release of histamine and other inflammatory mediators leads to systemic vasodilation and increased permeability of blood vessels, resulting in a sudden drop in blood pressure and compromised organ perfusion.
Choice B rationale:
Cardiogenic shock is characterized by inadequate cardiac output due to severe heart dysfunction. It is typically caused by conditions like myocardial infarction, heart failure, or other cardiac issues. While allergic reactions can potentially affect the cardiovascular system, the symptoms described in the question are more indicative of anaphylactic shock.
Choice C rationale:
Neurogenic shock results from disruption of sympathetic nervous system control over blood vessel tone, often due to spinal cord injury or severe emotional distress. This leads to widespread vasodilation and a sudden drop in blood pressure. While it can cause hemodynamic instability, it doesn't specifically involve the hypersensitivity reaction and capillary leaks associated with anaphylactic shock.
Choice D rationale:
Hypovolemic shock is caused by a significant loss of blood volume or bodily fluids, leading to decreased intravascular volume and subsequent inadequate tissue perfusion. This shock type is not directly related to a hypersensitivity reaction or capillary leakage caused by allergic responses. 2 / 2
What is a common sign of digoxin toxicity?
Explanation
The correct answer is Choice B: Tachycardia.
Choice A rationale:
Vomiting is not a common sign of digoxin toxicity. Digoxin is a medication commonly used to treat heart conditions, and its toxicity primarily affects the heart's electrical activity. Symptoms of digoxin toxicity usually manifest as cardiac arrhythmias and other cardiovascular issues rather than gastrointestinal symptoms like vomiting.
Choice B rationale:
Tachycardia is a common sign of digoxin toxicity. Digoxin can cause disturbances in the heart's electrical conduction system, leading to arrhythmias such as tachycardia. It can also cause atrioventricular (AV) block, which can result in bradycardia; however, tachycardia is more characteristic of digoxin toxicity.
Choice C rationale:
Bradypnea (slow breathing) is not a common sign of digoxin toxicity. While digoxin primarily affects the heart, it doesn't typically have a direct impact on respiratory function.
Choice D rationale:
Seizures are not a common sign of digoxin toxicity. Digoxin toxicity primarily affects the heart's electrical activity and can lead to arrhythmias, but it doesn't typically cause seizures.
What is a common clinical manifestation of juvenile hypothyroidism?
Explanation
The correct answer is Choice B: Dry skin.
Choice A rationale:
Diarrhea is not a common clinical manifestation of juvenile hypothyroidism. Hypothyroidism is characterized by an underactive thyroid gland, leading to a decrease in metabolic activity. Symptoms of hypothyroidism include fatigue, weight gain, cold intolerance, constipation, and dry skin, but not diarrhea.
Choice B rationale:
Dry skin is a common clinical manifestation of juvenile hypothyroidism. The decreased thyroid function results in a slower metabolic rate, which can lead to dry and coarse skin due to reduced oil production. This symptom is often seen in hypothyroid patients.
Choice C rationale:
Insomnia is not a common clinical manifestation of juvenile hypothyroidism. Hypothyroidism usually leads to fatigue and excessive sleepiness rather than insomnia.
Choice D rationale:
Accelerated growth is not a common clinical manifestation of juvenile hypothyroidism. In fact, the opposite is true. Hypothyroidism in children can lead to growth retardation due to the decreased metabolic rate and altered hormonal balance.
Therapeutic management of most children with Hirschsprung's disease is primarily
Explanation
The correct answer is Choice A: Surgical removal of the affected section of bowel.
Choice A rationale:
Surgical removal of the affected section of bowel is the primary therapeutic management for most children with Hirschsprung's disease. Hirschsprung's disease is a congenital condition where there is a lack of nerve cells in a segment of the colon, leading to obstruction and dilation of the bowel. Surgical resection of the affected segment and reconnection of healthy bowel portions is the standard treatment to alleviate the obstruction and restore normal bowel function.
Choice B rationale:
Daily enemas might be used in some cases to manage symptoms temporarily, but they are not the primary therapeutic management for Hirschsprung's disease. Surgery is the mainstay of treatment.
Choice C rationale:
Permanent colostomy might be considered if the affected portion of bowel is extensive and cannot be safely reconnected after resection, but it's not the primary option for most children with Hirschsprung's disease.
Choice D rationale:
A low-fiber diet is not a therapeutic management for Hirschsprung's disease. Surgical intervention is necessary to address the underlying cause of obstruction, and diet modifications alone wouldn't resolve the condition.
Instructions for decongestant nose drops should include what recommendation?
Explanation
The correct answer is choice A: Avoiding use for more than 3 days.
Choice A rationale:
Recommending avoiding the use of decongestant nose drops for more than 3 days is crucial due to the risk of rebound congestion. Decongestant nose drops work by constricting blood vessels in the nasal passages to alleviate congestion. Prolonged use can lead to a phenomenon known as rebound congestion, where the nasal passages become more congested once the medication wears off, causing the person to use the drops more frequently. This can result in a cycle of worsening congestion and overuse of the medication, which can be counterproductive and harmful. Limiting the use of decongestant nose drops to 3 days helps prevent this rebound effect and encourages the use of alternative treatments if congestion persists.
Choice B rationale:
Administering drops until nasal congestion subsides is not the recommended approach. Prolonged use of decongestant nose drops can lead to rebound congestion, as mentioned earlier. Using the drops until congestion subsides might extend their use beyond the safe period and increase the risk of adverse effects.
Choice C rationale:
Keeping drops to use again for nasal congestion is not advised. While it's important to follow the medication's storage instructions, relying on decongestant nose drops for recurring nasal congestion can lead to overuse and rebound congestion. This choice does not address the potential risks associated with prolonged use.
Choice D rationale:
Administering drops after feedings and at bedtime is not a standard recommendation for decongestant nose drops. The timing of administration is not a primary concern in the context of decongestant use. Instead, the focus should be on the duration of use and the potential for rebound congestion.
Sign Up or Login to view all the 75 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

