Pain Management During Labor > Maternal & Newborn
Exam Review
Pharmacologic Pain Management During Labor
Total Questions : 10
Showing 10 questions, Sign in for moreA nurse is caring for a client who is in labor and requests systemic analgesia.
Which of the following medications can the nurse administer intravenously to provide sedation, anxiolysis, and analgesia during labor?
Explanation
Meperidine is an opioid that can be administered intravenously to provide sedation, anxiolysis, and analgesia during labor.It provides pain relief that is superior to nitrous oxide but inferior to regional anesthesia.
A client who is in labor asks the nurse about the benefits and limitations of inhaled analgesia.
Which of the following statements should the nurse include in the teaching?
Explanation
inhaled analgesia, such as nitrous oxide, is self-administered by the client through a mask or mouthpiece.The client needs to coordinate the inhalation with the onset of contractions and may need assistance from a support person to hold the mask or mouthpiece.
A nurse is reviewing the medical record of a client who is in labor and has a history of asthma.
The nurse should identify that which of the following pharmacologic pain management methods is contraindicated for this client?
Explanation
Inhaled analgesia is contraindicated for this client because it can cause bronchospasm and hypoxia in patients with asthma.
Normal ranges for blood pressure are 90/60 to 120/80 mmHg, for fetal heart rate are 110 to 160 beats per minute, and for bladder function are urine output of at least 30 mL/hour.
A nurse is preparing to administer fentanyl to a client who is in labor and has severe pain.
Which of the following actions should the nurse take to prevent adverse effects on the fetus?
Explanation
Administer the medication immediately after a contraction.This is because fentanyl can cross the placenta and cause respiratory depression in the fetus, so it should be given when the placental blood flow is lowest, which is right after a contraction.
A nurse is caring for a client who is in labor and has received meperidine for pain relief.
Which of the following findings should alert the nurse to a possible adverse effect of the medication?
Explanation
This is a sign ofrespiratory depression, which is a possible adverse effect of meperidine.Meperidine is an opioid analgesic that can slow or stop breathing, and cause death in some cases.
A nurse is preparing to administer epidural anesthesia to a client in labor.
What is the minimum cervical dilation required before inserting the catheter into the epidural space?
Explanation
The correct answer is Choice B.
Choice A rationale: A cervical dilation of 2 cm is not sufficient for the insertion of an epidural catheter. The cervix needs to be dilated more to ensure that the catheter can be inserted without causing injury or discomfort to the patient. Furthermore, administering epidural anesthesia too early in labor can potentially slow down the labor process.
Choice B rationale: A cervical dilation of 4 cm is generally considered the minimum dilation required before inserting the catheter into the epidural space. At this stage, the labor is established and the risk of slowing down the labor process is minimal. The epidural space can be accessed safely and the catheter can be inserted without causing injury or discomfort to the patient.
Choice C rationale: While a cervical dilation of 6 cm is more than sufficient for the insertion of an epidural catheter, it is not necessary to wait until the cervix is dilated to this extent before administering epidural anesthesia. Waiting until the cervix is dilated to 6 cm could result in unnecessary pain and discomfort for the patient.
Choice D rationale: A cervical dilation of 8 cm is well into the active phase of labor and is often considered too late for the administration of epidural anesthesia. At this stage, the labor is progressing rapidly and there may not be enough time to administer the anesthesia and achieve adequate pain relief before the baby is born.
A nurse is caring for a client who received spinal anesthesia for a cesarean delivery.
The nurse should monitor the client for which of the following potential complications of spinal anesthesia?
Explanation
A potential complication of spinal anesthesia is postdural puncture headache (PDPH), which occurs when cerebrospinal fluid leaks through the puncture site and causes low pressure in the subarachnoid space.
This can result in a severe headache that worsens when sitting or standing and improves when lying down.PDPH usually occurs within 24 to 48 hours after the spinal anesthesia and can last for days or weeks.
A nurse is educating a client about the advantages of combined spinal-epidural (CSE) anesthesia over epidural or spinal anesthesia alone.
Which of the following statements by the client indicates understanding of the teaching?
Explanation
This statement indicates that the client understands the advantages of CSE anesthesia over epidural or spinal anesthesia alone.CSE anesthesia combines the rapid onset and reliable blockade of spinal anesthesia with the ability to extend and adjust the analgesia through epidural catheterization.This makes CSE anesthesia suitable for procedures that require timely, effective, and prolonged pain relief, such as labor and delivery, abdominal surgery, and lower extremity orthopedic surgery.
A nurse is assisting an anesthesiologist with performing dural puncture epidural (DPE) anesthesia for a client in labor.
What is the purpose of intentionally puncturing the dura mater with a needle in this technique?
Explanation
The purpose of intentionally puncturing the dura mater with a needle in this technique is to allow cerebrospinal fluid to leak into the epidural space and enhance the spread of local anesthetics.This technique is a modification of the combined spinal epidural technique, which involves injecting medication into both the epidural and the subarachnoid spaces.The dural puncture epidural technique aims to avoid the side effects of the combined spinal epidural technique, such as hypotension, pruritus, and urinary retention.
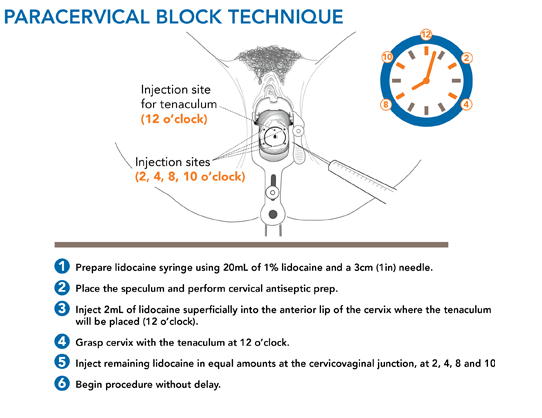
A nurse is planning to administer paracervical block to a client in labor.
Which of the following areas should the nurse inject local anesthetics into?
Explanation
The paracervical area at 3 o’clock and 9 o’clock positions.This is because a paracervical block is an anesthetic procedure in which a local anesthetic is injected into between two and six sites at a depth of 3–7 mm alongside the vaginal portion of the cervix in the vaginal fornices.The injection sites are usually at 10 o’clock, 8 o’clock, 2 and 4 o’clock positions, but for labor pain relief, the 3 o’clock and 9 o’clock positions are preferred.
Sign Up or Login to view all the 10 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

