PHARMACOLOGY 2
Total Questions : 35
Showing 25 questions, Sign in for moreA kidney transplant recipient stops immunosuppressive therapy three years after his surgery. Shortly after stopping therapy, he demonstrated clinical manifestations of kidney failure. Which type of reaction does this represent?
Explanation
A. Cushing's Syndrome: This is a condition caused by prolonged exposure to high levels of cortisol, a hormone produced by the adrenal glands. It is not related to kidney transplant or immunosuppressive therapy.
B. Hypersensitivity Reaction Type I: Also known as an immediate hypersensitivity reaction or an allergy, this type of reaction involves the immune system's exaggerated response to an allergen. Symptoms can range from mild to severe and occur quickly after exposure to the allergen. While allergies can cause various symptoms, they do not specifically represent rejection of a transplanted organ.
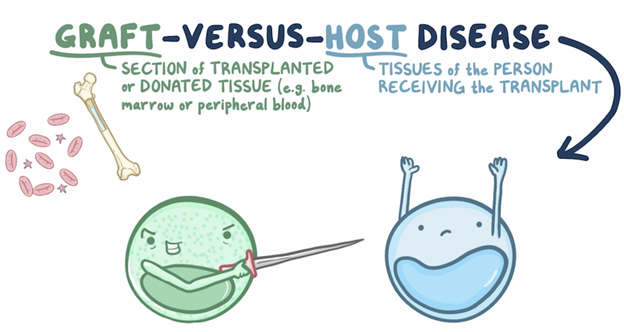
C. Chronic Graft Versus Host Rejection: This term is commonly associated with bone marrow or stem cell transplants. It occurs when immune cells from the donated tissue recognize the recipient's body as foreign and attack various organs or tissues. This process typically happens over a more extended period and is not directly related to the scenario described.
D. Acute Host Versus Graft Rejection: This occurs when the recipient's immune system recognizes the transplanted organ as foreign and launches an immune response against it. It can happen shortly after transplantation if the recipient's immune system is not adequately suppressed. In this case, stopping immunosuppressive therapy can trigger acute rejection, leading to the failure of the transplanted organ.
"My doctor said I have an autoimmune disease. What does that mean?" asks a client. How should the nurse respond?
Explanation
A. "You have developed urticaria in response to something in your environment."
This statement is incorrect. Urticaria refers to hives, a skin rash usually caused by an allergic reaction, infection, or stress. It's not necessarily indicative of an autoimmune disease.
B. "Your immune system is creating antibodies that are destroying your own cells."
This statement is correct. Autoimmune diseases involve the immune system mistakenly attacking the body's own cells and tissues, leading to various health issues.
C. "Your immune system is not able to create antibodies to help you fight infection."
This statement is incorrect. In autoimmune diseases, the immune system is overactive, producing antibodies that target the body's own cells, not that it can't create antibodies.
D. "You have developed an infection that is destroying your immune cells."
This statement is incorrect. Infections don't typically destroy immune cells; instead, infections often stimulate the immune system to respond and fight against invading pathogens.
Which immunoglobulin provides the most protection against Infection in a client, as it is the most abundant?
Explanation
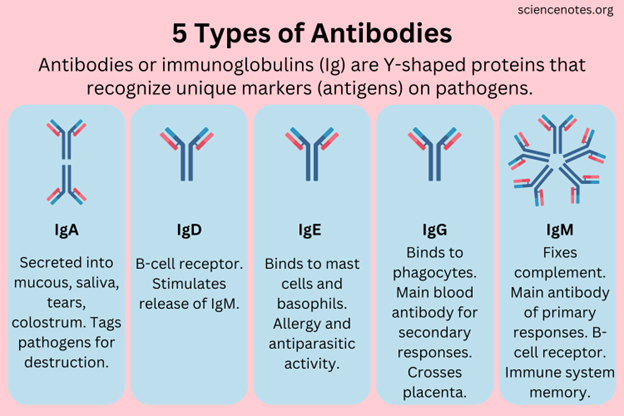
A. IgG: Immunoglobulin G (IgG) is the most abundant antibody in the bloodstream and represents about 75% of all the antibodies in the body. It provides long-term immunity because it can persist in the bloodstream for a long time. IgG antibodies are involved in secondary immune responses and are capable of crossing the placenta, providing passive immunity to newborns.
B. IgE: Immunoglobulin E (IgE) is associated mainly with allergic reactions. When the body is exposed to an allergen, it triggers the release of IgE, leading to the symptoms of an allergic response, such as sneezing or itching.
C. IgM: Immunoglobulin M (IgM) is the largest antibody and is usually the first antibody produced during an initial exposure to an antigen. It is particularly effective at agglutination (clumping together) of pathogens.
D. IgA: Immunoglobulin A (IgA) is found in high concentrations in mucous membranes, particularly those lining the respiratory passages and gastrointestinal tract. It provides localized defense against pathogens. IgA antibodies are also found in saliva, tears, and breast milk, providing immunity to infants.
Which one of the following types of immunoglobulins is involved in inflammatory and allergic responses?
Explanation
A. IgD: Immunoglobulin D (IgD) is found on the surface of B cells and serves as a receptor for antigen recognition during the immune response. Its exact function is not fully understood, but it plays a role in the activation of B cells.
B. IgE: Immunoglobulin E (IgE) is primarily associated with allergic responses and defense against parasitic infections. When an allergen enters the body, IgE antibodies trigger the release of histamine and other chemicals, leading to allergy symptoms. IgE is also involved in protecting against certain parasites.
C. IgG: Immunoglobulin G (IgG) is the most abundant immunoglobulin in the bloodstream. It provides long-term immunity by recognizing and neutralizing pathogens such as bacteria and viruses. IgG antibodies are involved in secondary immune responses and are transferred from mother to fetus, providing passive immunity.
D. IgM: Immunoglobulin M (IgM) is the first antibody produced during an initial immune response to an antigen. It is effective at agglutination (clumping) of pathogens. IgM antibodies are generally found in blood and lymph fluid and are the first line of defense during infections.
Both B and T cells are originally derived from cells of the:
Explanation
A. Gut-associated lymphoid tissue (GALT): GALT is a component of the mucosa-associated lymphoid tissue (MALT) and refers to the immune cells found in the gastrointestinal tract. These cells play a significant role in local immune responses in the gut.
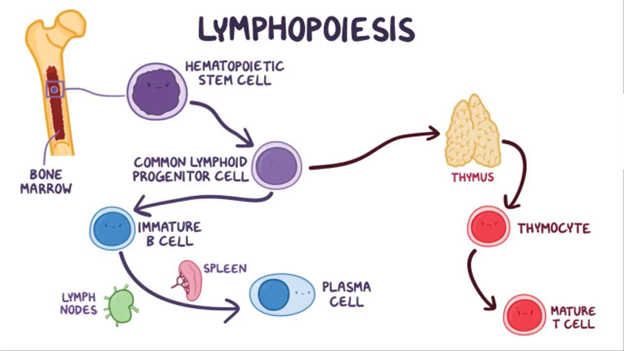
B. Bone marrow: The bone marrow is the primary site of blood cell production in the body. It contains stem cells that can differentiate into various blood cells, including B cells. B cells mature in the bone marrow.
C. Thymus: The thymus is an organ located near the heart and is crucial for the development of T cells. T cells mature in the thymus, where they learn to recognize self from non-self antigens.
D. Lymph nodes: Lymph nodes are small, bean-shaped structures that produce and store cells that help fight infection. While they are essential parts of the immune system, B and T cells are not originally derived from lymph nodes.
Your patient is on long-term prednisone therapy. This patient should have frequent follow-up office visits to assess for which of the following?
Explanation
A. Dermatitis and headaches: Prednisone use can sometimes cause skin issues, but dermatitis is not a common side effect. Headaches can also occur, but they are not specific to long-term prednisone therapy.
B. Heart failure and headaches: Prednisone does not directly cause heart failure. Headaches can occur but are not specific indicators of prednisone side effects.
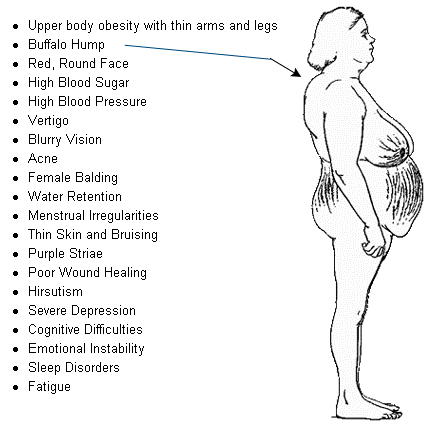
C. Hyperglycemia and osteoporosis: Prednisone can lead to elevated blood glucose levels (hyperglycemia) and increased bone loss (osteoporosis) when used long-term. Regular monitoring is essential to manage these potential side effects.
D. Weight loss and hypoglycemia: Prednisone can cause weight gain rather than weight loss. Hypoglycemia (low blood sugar) is not a common side effect of prednisone; it typically causes hyperglycemia (high blood sugar) instead.
A 65-year-old female is diagnosed with metastatic breast cancer. Which of the following cells would be produced in large quantities to eliminate the tumor cells?
Explanation
A. Neutrophils: Neutrophils are a type of white blood cell that plays a key role in the immune system's response to infections, particularly bacterial infections. They are not primarily involved in eliminating cancer cells.
B. Eosinophils: Eosinophils are another type of white blood cell. They are important in the immune response to parasites and are also involved in allergic reactions. While they have a role in the immune system, they are not the primary cells involved in eliminating cancer cells.
C. Platelets: Platelets, also known as thrombocytes, are not cells but rather small cell fragments. They are essential for blood clotting and do not directly participate in the immune response against cancer cells.
D. Macrophages: Macrophages are a type of white blood cell that are involved in the immune system's defense against cancer. They are phagocytes, which means they engulf and digest cellular debris, foreign substances, and cancer cells. Macrophages play a crucial role in the body's immune surveillance and response against cancer.
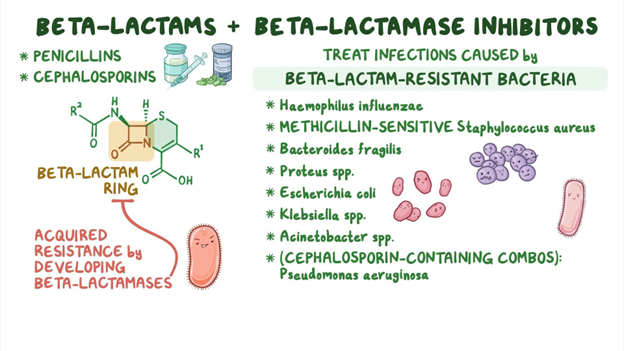
Penicillin has cross-sensitivity to which of the following drug classes?
Explanation
A. Aminoglycosides: Aminoglycosides are a different class of antibiotics. They do not have cross-sensitivity with penicillin. People who are allergic to penicillin can usually take aminoglycosides without a problem.
B. Erythromycins: Erythromycins are macrolide antibiotics. They are not related to penicillin structurally, so there is no cross-sensitivity between penicillin and erythromycins. People allergic to penicillin can generally take erythromycin without issues.
C. Quinolones: Quinolones, also known as fluoroquinolones, are a different class of antibiotics. They do not share a structural similarity with penicillin, so there is usually no cross-sensitivity between penicillin and quinolones. People allergic to penicillin can usually take quinolones without problems.
D. Cephalosporins: Cephalosporins are beta-lactam antibiotics, just like penicillins. They have a similar chemical structure to penicillins, which can lead to cross-sensitivity. Individuals who are allergic to penicillin might also have an allergic reaction to cephalosporins due to this structural resemblance. However, it's important to note that not all cephalosporins are the same, and the risk of cross-reactivity varies among different generations of cephalosporins. Healthcare providers need to assess the specific situation and choose an appropriate antibiotic if there is a known penicillin allergy.
Patients with aminoglycoside therapy should be monitored for:
Explanation
A. Ototoxicity and Nephrotoxicity:
Ototoxicity: Aminoglycosides can damage the inner ear structures, leading to hearing loss and balance issues.
Nephrotoxicity: These drugs can harm the kidneys, potentially causing acute kidney injury or chronic kidney disease. Monitoring kidney function is crucial to prevent renal damage.
B. Ototoxicity and Cardiotoxicity:
Ototoxicity: As mentioned above, aminoglycosides can damage the inner ear, affecting hearing and balance.
Cardiotoxicity: Aminoglycosides primarily affect the ears and kidneys; they do not directly target the heart. Cardiotoxicity is not a common side effect associated with aminoglycosides.
C. Hepatotoxicity and Nephrotoxicity:
Hepatotoxicity: This term refers to liver damage caused by drugs or toxins. Aminoglycosides are not known to cause liver problems; their primary concern is kidney damage.
Nephrotoxicity: As mentioned earlier, aminoglycosides can harm the kidneys, which is a well-known side effect.
D. Cardiotoxicity and Hepatotoxicity:
Cardiotoxicity: This term refers to the toxic effects on the heart, leading to various heart-related issues. Aminoglycosides do not primarily affect the heart; their main concerns are the ears (ototoxicity) and kidneys (nephrotoxicity).
Hepatotoxicity: Aminoglycosides are not typically associated with liver damage. They are primarily metabolized and excreted by the kidneys, which is why kidney monitoring is crucial during their use.
Your 25-year-old female patient has been prescribed ciprofloxacin (Cipro) for a respiratory infection. Patient teaching includes which of the following?
Explanation
A. Wear high-top shoes to avoid tendon rupture:
This statement is incorrect. Tendon rupture is a known side effect of fluoroquinolone antibiotics like ciprofloxacin, especially in certain populations. However, wearing high-top shoes does not prevent this. Patients should be educated about the signs of tendon pain, swelling, or inflammation and should be advised to stop the medication and contact their healthcare provider if they experience such symptoms.
B. Use a barrier method of birth control (condoms) during antibiotic use:
This statement is partially correct. Antibiotics like ciprofloxacin do not interfere with the efficacy of hormonal birth control methods like pills, patches, or injections. However, it's advisable to use a barrier method like condoms as an additional form of contraception while taking antibiotics. This is to prevent potential interactions and ensure maximum contraceptive effectiveness.
C. Do not use any bronchodilator inhalers while taking the drug:
This statement is incorrect. Ciprofloxacin does not interact negatively with bronchodilator inhalers. Patients can continue using their prescribed inhalers as directed by their healthcare provider, especially if they are being used for conditions like asthma or chronic obstructive pulmonary disease (COPD).
D. Stop the medication as soon as you feel better:
This statement is incorrect. It's crucial for patients to complete the entire course of antibiotics as prescribed, even if they start feeling better before the course is finished. Stopping antibiotics prematurely can lead to incomplete eradication of the infection, potentially allowing the bacteria to develop resistance and cause a recurrence of the illness.
The drug of choice for methicillin-resistant staphylococcus aureus (MRSA) is:
Explanation
A. Gentamicin: Gentamicin is an aminoglycoside antibiotic effective against many bacteria, but it's not the first choice for MRSA. Vancomycin or other alternatives are preferred due to the rising resistance of MRSA to gentamicin.
B. Nafcillin: Nafcillin is a penicillin antibiotic, often used for penicillin-sensitive staphylococcal infections. However, it is not effective against MRSA, which is resistant to many penicillin-based antibiotics.
C. Vancomycin: Vancomycin is a glycopeptide antibiotic used to treat a variety of bacterial infections, including MRSA. It works by inhibiting cell wall synthesis in bacteria, making it effective against Gram-positive bacteria that have developed resistance to other antibiotics like methicillin (which MRSA has).
D. Penicillin: Penicillin is a group of antibiotics that includes drugs like amoxicillin and ampicillin. MRSA is resistant to penicillin-based antibiotics, so they are not effective against MRSA infections.
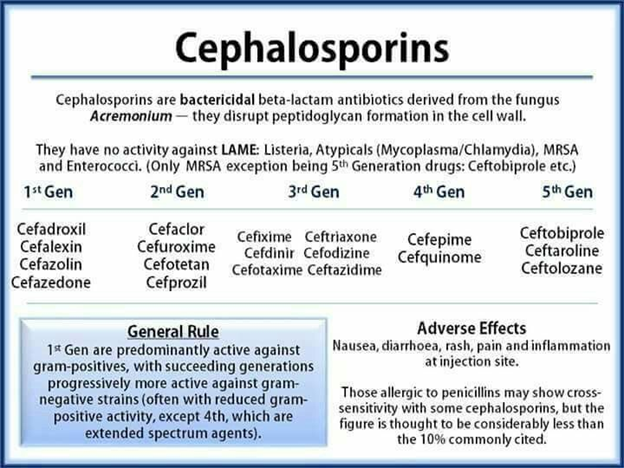
A drug that is a fifth-generation cephalosporin which is the first in its class effective against MRSA is:
Explanation
A. Ceftaroline (Teflaro) is a fifth-generation cephalosporin antibiotic that is effective against MRSA (Methicillin-Resistant Staphylococcus Aureus). It's the first cephalosporin in its class with this capability, making it a valuable choice in treating MRSA infections.
B. Cefepime (Maxipime) is a fourth-generation cephalosporin that does not have specific activity against MRSA.
C. Ceftriaxone (Rocephin) is a third-generation cephalosporin, effective against a wide range of bacteria, but not specifically targeted at MRSA.
D. Cephalexin (Keflex) is a first-generation cephalosporin, primarily effective against Gram-positive bacteria, but not effective against MRSA.
The nurse is reviewing her hospitalized client's medications and sees that he is on both a cephalosporin and an aminoglycoside. The nurse knows that this combination of antibiotics increases the client's risk for:
Explanation
A. Seizures: Some antibiotics, especially cephalosporins, can lower the seizure threshold, increasing the risk of seizures, especially in individuals prone to seizures or those with a history of epilepsy.
B. Nephrotoxicity: Both cephalosporins and aminoglycosides have the potential to harm the kidneys. When used together, their nephrotoxic effects can be additive, increasing the risk of kidney problems in patients.
C. Hearing Loss: Aminoglycosides, a class of antibiotics that includes drugs like gentamicin, are well-known for their potential to cause hearing loss, especially when used in high doses or for prolonged periods. This effect is due to their toxic impact on the hair cells in the inner ear.
D. Hepatotoxicity: Hepatotoxicity refers to liver damage caused by medications. Some antibiotics, including certain cephalosporins, can have hepatotoxic effects, potentially harming the liver. Monitoring liver function is important when these drugs are used.
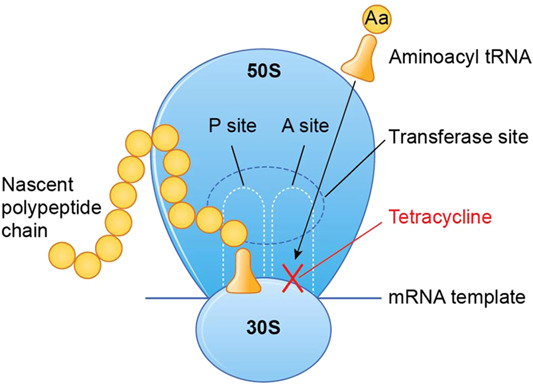
A nursing student asks the nursing instructor about the mechanism of the bacteriostatic action of tetracycline. Which explanation is correct?
Explanation
A. "Tetracycline inhibits protein synthesis."
Explanation: Tetracycline antibiotics interfere with bacterial protein synthesis by binding to the bacterial ribosomes. This binding prevents the attachment of transfer RNA (tRNA) to the messenger RNA (mRNA) complex, effectively inhibiting the production of proteins that are crucial for bacterial growth and replication.
B. "Tetracycline blocks RNA synthesis."
Explanation: This statement is incorrect. Tetracycline primarily affects protein synthesis, not RNA synthesis. It doesn't block the creation of RNA molecules in bacteria.
C. "Tetracycline degrades the bacterial cell wall."
Explanation: This statement is incorrect. Tetracycline antibiotics do not target bacterial cell walls. Agents like penicillins and cephalosporins are examples of antibiotics that disrupt bacterial cell walls.
D. "Tetracycline binds to magnesium ions."
Explanation: This statement is incorrect. Tetracycline does bind to certain metal ions, but it's not primarily through magnesium ions. The binding to bacterial ribosomes is a key mechanism of action for tetracyclines.
What is the difference between bactericidal drugs and bacteriostatic drugs?
Explanation
A. "Bactericidal and bacteriostatic are used interchangeably."
Explanation: This statement is incorrect. Bactericidal and bacteriostatic are two distinct categories of antibiotics with different mechanisms of action.
B. "Bactericidal drugs are directly lethal to bacteria, and bacteriostatic drugs work to slow bacterial growth but do not cause cell death."
Explanation: This statement is correct. Bactericidal drugs kill bacteria directly, leading to their death, while bacteriostatic drugs inhibit bacterial growth without causing immediate cell death.
C. "Bacteriostatic drugs are directly lethal to bacteria, and bactericidal drugs work to slow bacterial growth but do not cause cell death."
Explanation: This statement is incorrect. It is the opposite of the correct explanation. Bacteriostatic drugs do not directly kill bacteria, and bactericidal drugs do cause bacterial death.
D. "A bactericidal drug can cause death to the host, whereas a bacteriostatic drug only affects bacteria."
Explanation: This statement is not entirely accurate. While some bactericidal drugs can be more toxic to the host, it depends on the specific drug and its dosage. Bacteriostatic drugs, on the other hand, generally do not directly harm the host. The primary distinction between the two categories is their impact on bacterial growth and survival.
A patient has been ordered azithromycin [Zithromax] and asks the nurse why the medication does not have to be taken as often as other antibiotics that have previously been ordered. What is the nurse's best response?
Explanation
A. "This drug has a longer duration of action than some of the other antibiotics."
Explanation: Azithromycin, a macrolide antibiotic, has a longer half-life in the body compared to some other antibiotics. Half-life refers to the time it takes for half of the drug to be eliminated from the body. A longer half-life means the drug remains effective for a longer duration, allowing for less frequent dosing.
B. "This is a much more effective drug than what you received previously."
Explanation: While azithromycin is effective against a wide range of bacterial infections, it's not accurate to say it's universally more effective than other antibiotics. The choice of antibiotic depends on the specific type of infection and the susceptibility of the bacteria causing it. Effectiveness varies based on the context of use.
C. "I'll call the pharmacy and ask about the chemical makeup of the drug."
Explanation: While understanding the chemical makeup of drugs is important for healthcare professionals, it might not directly answer the patient's question about the dosing frequency. Explaining the drug's pharmacological properties, such as its duration of action, would provide a more relevant and understandable response to the patient's query.
D. "You'll need to ask your healthcare provider questions like that."
Explanation: This response does not provide the patient with the information they seek. Nurses are valuable resources for medication-related questions and should strive to provide accurate and understandable explanations to patients.
Which statement by a patient makes the nurse aware of a need for further education about drug resistance in antimicrobial therapy?
Explanation
A. "The antibiotic I have been taking doesn't work as well as it used to."
This statement shows awareness of decreased effectiveness, which can occur due to drug resistance. Bacteria can become resistant to antibiotics, leading to reduced efficacy of the medication over time.
B. "The bacteria in my body have become resilient."
This statement correctly attributes resistance to the bacteria. Resilience in this context means that bacteria have developed mechanisms to survive the effects of antibiotics, making the treatment less effective.
C. "Over time, an organism that had once been highly sensitive to an antibiotic may become less susceptible, or it may lose drug sensitivity entirely."
This statement accurately describes the concept of drug resistance. Bacteria can lose sensitivity to antibiotics, rendering the drugs ineffective against them.
D. "My body has become resistant to the antibiotic."
This statement is incorrect. It's the bacteria that develop resistance, not the patient's body. Patients don't become resistant to antibiotics; instead, bacteria evolve and adapt, making the drugs less effective against them.
A nurse is teaching a nursing student what is meant by "generations" of cephalosporins. Which statement by the student indicates an understanding of the teaching?
Explanation
A. "Cephalosporins are assigned to generations based on their relative costs to administer."
This statement is incorrect. The classification of cephalosporins into generations is based on their antimicrobial spectrum and activity against specific bacteria, not their cost.
B. "Later generations of cephalosporins have lower resistance to destruction by beta-lactamases."
This statement is not accurate. In fact, later generations of cephalosporins have increased resistance to destruction by beta-lactamases, which are enzymes produced by bacteria that can break down certain antibiotics.
C. "Cephalosporins have increased activity against gram-negative bacteria with each new generation."
This statement is correct. Cephalosporins are grouped into generations (first to fifth) based on their antibacterial spectrum. As the generations progress, there is an increase in activity against gram-negative bacteria, among other improvements in their spectrum.
D. "First-generation cephalosporins have better penetration of the cerebrospinal fluid."
This statement is generally true. First-generation cephalosporins have better penetration into the cerebrospinal fluid, making them useful for treating certain central nervous system infections.
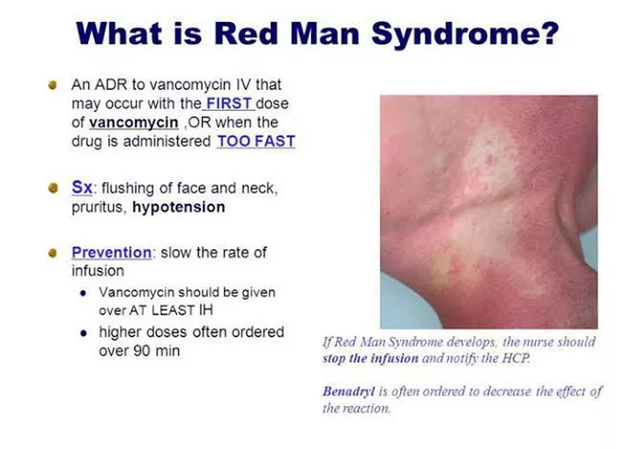
The nurse is caring for a patient who is receiving vancomycin (Vancocin). The nurse notes that the patient is experiencing flushing, rash, pruritus, and urticaria. The patient's heart rate is 120 beats per minute, and the blood pressure is 92/57 mm Hg. The nurse understands that these findings are consistent with:
Explanation
Allergic reaction: An allergic reaction can manifest in various ways, including rash, itching, and difficulty breathing. However, the specific symptoms described, along with the context of vancomycin administration, point to red man syndrome in this case.
Rhabdomyolysis: Rhabdomyolysis is a condition where damaged muscle tissue breaks down and releases a protein called myoglobin into the bloodstream. This can cause kidney damage, but the symptoms described do not align with rhabdomyolysis.
Stevens-Johnson syndrome: Stevens-Johnson syndrome is a severe skin reaction that can cause skin and mucous membranes to blister, peel, and can be life-threatening. While it can present with rash and other skin symptoms, the symptoms mentioned in the scenario are more characteristic of red man syndrome.
Red man syndrome: As mentioned earlier, red man syndrome is an allergic reaction to vancomycin characterized by flushing, rash, pruritus, and urticaria (hives), along with rapid heart rate and low blood pressure. It is specific to vancomycin and can be prevented or minimized by slowing down the infusion rate and administering antihistamines.
The nurse is caring for a patient on a medical-surgical unit who has a fever of unknown origin. The prescriber has ordered a broad-spectrum antibiotic. Which intervention is the priority?
Explanation
A. Obtaining all cultures before the antibiotic is administered: While obtaining cultures is important for identifying the specific pathogen causing the infection and guiding targeted antibiotic therapy, waiting for culture results can take time. During this time, the infection can progress. Therefore, it's generally recommended to initiate broad-spectrum antibiotics first and then adjust the treatment based on culture results.
B. Delaying administration of the antibiotic until the culture results are available: Delaying antibiotics until culture results are available can be risky, as it allows the infection to progress, potentially leading to sepsis or other severe complications.
C. Administering antipyretics as soon as possible: Administering antipyretics like acetaminophen or ibuprofen can help reduce fever and make the patient more comfortable. However, the primary intervention for a suspected infection is antibiotic therapy, as it targets the underlying cause of the fever.
D. Administering the antibiotic immediately: When dealing with a patient with a fever of unknown origin and a suspected infection, the priority is to start appropriate antibiotic therapy promptly. Delaying antibiotic administration can allow the infection to worsen, leading to serious complications.
The nurse who is working in a pediatric unit administers tetracycline [Sumycin] to a preschool-age child. What is a potential adverse effect of the medication for this child?
Explanation
A. Discoloration of teeth: Tetracycline antibiotics can bind with calcium ions in teeth, leading to the development of yellow-gray-brown stains. This effect is particularly significant in developing teeth in children below the age of 8 and can result in permanent discoloration.
B. Anabolic change: This term doesn't specifically relate to the side effects of tetracycline. "Anabolic" generally refers to processes in the body that build up complex molecules from simpler ones. There's no direct connection between tetracycline and anabolic changes.
C. Cartilage damage: Tetracyclines, especially in high doses or with prolonged use, have been associated with potential adverse effects on cartilage. This is more relevant in individuals whose bones and cartilage are still growing, such as children. It can interfere with skeletal development.
D. Suppression of growth: Long-term use of tetracycline in children can interfere with bone growth and development. It can suppress the growth of bones and affect overall height. This is a significant concern when considering the use of tetracycline in pediatric patients.
The nurse should teach a patient to observe which side effects when taking ampicillin.
Explanation
A. Reddened tongue and gums: This side effect is not typically associated with ampicillin. However, certain medications or medical conditions can cause changes in oral tissues, leading to redness in the tongue and gums.
B. Digit numbness and tingling: Ampicillin does not commonly cause numbness and tingling in the fingers and toes. These symptoms can be associated with neurological issues or circulatory problems.
C. Bruising and petechiae: These symptoms can indicate bleeding disorders or low platelet count and are not usually caused by ampicillin. It's essential to investigate further if a patient experiences unexplained bruising or petechiae.
D. Skin rash and loose stools: Skin rash is a known side effect of penicillin-type antibiotics, including ampicillin. Loose stools or diarrhea can also occur due to disruption of the gut flora caused by the antibiotic. Patients should be aware of these possibilities and report any severe or persistent symptoms to their healthcare provider.
Which of the following is an accurate description of a type-1 hypersensitivity reaction?
Explanation
A. Most type-1 reactions are allergic: This statement is accurate. Type-1 hypersensitivity reactions are typically associated with allergies. When a person is exposed to a specific allergen (like pollen or certain foods), their immune system overreacts, leading to various symptoms, from mild to severe.
B. It is mediated by IgA: This statement is incorrect. Type-1 hypersensitivity reactions are primarily mediated by immunoglobulin E (IgE) antibodies. When these antibodies bind to allergens, they trigger the release of histamine and other chemicals, causing allergic symptoms.
C. It never contributes to autoimmune diseases: This statement is incorrect. While type-1 hypersensitivity reactions are often associated with allergies, they are distinct from autoimmune diseases. In autoimmune diseases, the immune system mistakenly attacks the body's own cells and tissues, which is a different mechanism from hypersensitivity reactions.
D. Most occur against medications: This statement is not entirely accurate. While some type-1 hypersensitivity reactions can be triggered by medications (like penicillin), they can also be caused by various other allergens such as pollen, animal dander, insect venom, and certain foods. The prevalence of medication-induced type-1 reactions varies, and it's not accurate to say that most occur against medications.
While instructing a patient about antibiotic therapy, the nurse explains to the patient that bacterial resistance to antibiotics can occur what happens?
Explanation
A. Antibiotics are prescribed according to culture and sensitivity reports:
When antibiotics are prescribed based on specific tests like cultures and sensitivity reports, it ensures that the right antibiotic is chosen for the specific bacteria causing the infection. This practice helps in targeting the infection more effectively, reducing the risk of antibiotic resistance.
B. Patients stop taking an antibiotic after they feel better:
This scenario is problematic. When patients start feeling better, they might assume the infection is completely gone and stop taking antibiotics before the prescribed course is finished. This premature discontinuation can leave some bacteria alive, which may develop resistance to the antibiotic used. This practice is a significant contributor to antibiotic resistance.
C. Antibiotics are taken with ascorbic acid (vitamin C):
Ascorbic acid (vitamin C) doesn't have a significant impact on antibiotic resistance. It is not a factor contributing to antibiotic resistance.
D. Antibiotics are taken with water or juice:
Whether antibiotics are taken with water or juice doesn’t directly influence antibiotic resistance. Proper hydration is essential to support the body's overall health, but it doesn't impact the development of antibiotic resistance.
The nurse is setting up an intravenous infusion pump to administer a dose of vancomycin [Vancocin] to a patient. What is the fastest rate at which the drug may be infused?
Explanation
Vancomycin is often administered over at least 60 minutes to reduce the risk of infusion-related reactions, such as "Red Man Syndrome," which is characterized by flushing, rash, and itching. This reaction is caused by the rapid infusion of vancomycin, leading to the release of histamine.
Sign Up or Login to view all the 35 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

