PN Adult Medical Surgical 2020 - Exam 2
Total Questions : 91
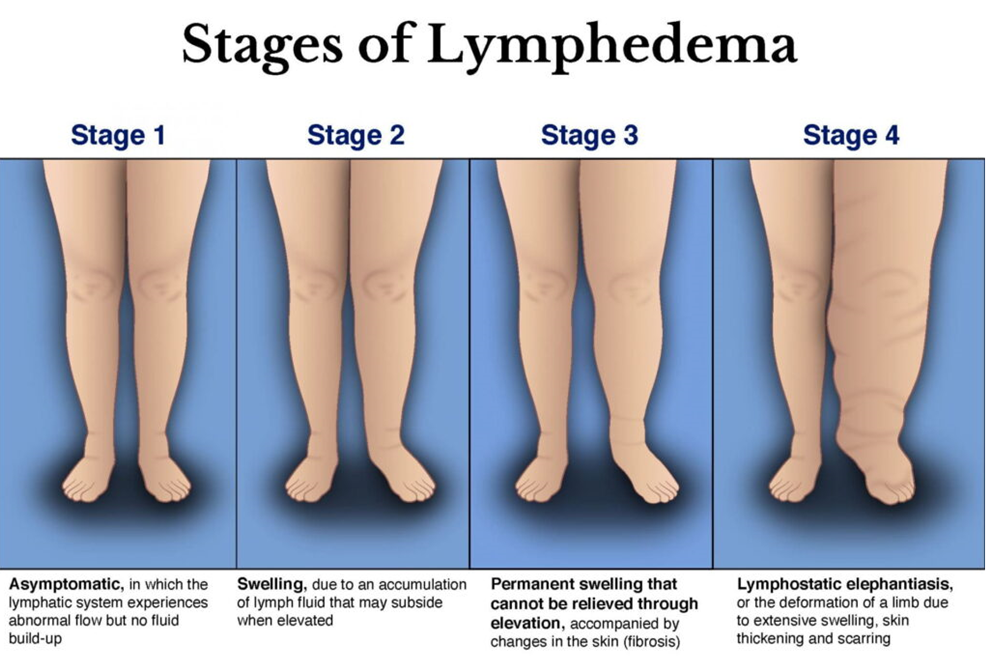
Showing 25 questions, Sign in for moreA nurse is caring for a client who is postoperative following a right radical mastectomy. Which of the following actions should the nurse take to prevent the development of lymphedema?
Explanation
Choice A reason: Keeping both arms below the level of the client's heart can increase venous pressure and fluid accumulation in the affected arm, which can lead to lymphedema.
Choice B reason: Using the client's left arm to obtain blood samples is a correct action to prevent lymphedema. The nurse should avoid any invasive procedures, such as blood draws, injections, or IV insertions, on the affected arm to reduce the risk of infection and injury.
Choice C reason: Obtaining blood pressure readings using the client's right arm is an incorrect action that can increase lymphatic fluid accumulation and impair circulation in the affected arm.
Choice D reason: Limiting range-of-motion exercises with the affected arm is an incorrect action that can decrease lymphatic drainage and increase swelling in the affected arm. The nurse should encourage the client to perform gentle exercises, such as squeezing a soft ball or raising and lowering the arm, to promote lymphatic flow and prevent stiffness.
Explanation
Choice A reason: Glucocorticoids are anti-inflammatory drugs that can increase blood glucose levels and worsen diabetes mellitus, which is a risk factor for stroke.
Choice B reason: HbA1c is a measure of average blood glucose levels over the past three months. A higher HbA1c level indicates poor glycemic control and increases the risk for stroke. The target HbA1c level for most people with diabetes mellitus is less than 7 percent.
Choice C reason: Having a high total cholesterol level is a risk factor for stroke, as it can lead to atherosclerosis and plaque formation in the blood vessels. The target total cholesterol level for most people is less than 200 mg/dL.
Choice D reason: Losing excess weight can lower blood pressure, improve blood glucose levels, and reduce inflammation, which are all beneficial for preventing stroke.
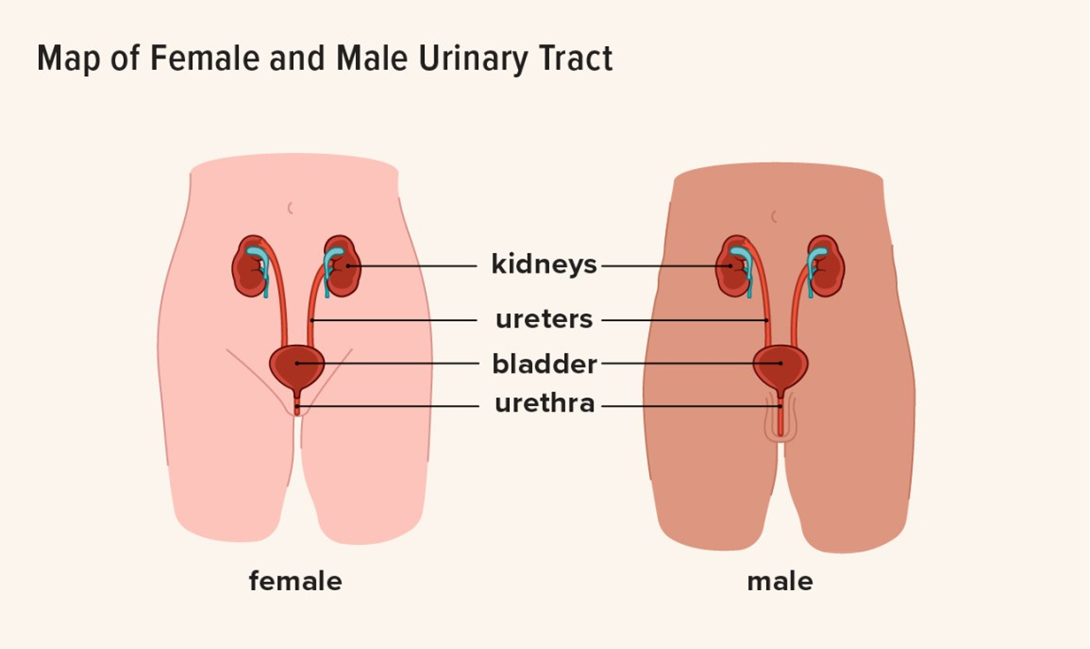
A nurse is collecting data on an older adult client. Which of the following findings should indicate to the nurse that the client has a bladder infection?
Explanation
Choice A reason: Changed mental status, such as confusion, agitation, or delirium, can be a sign of a bladder infection in older adults, as they may not have the typical symptoms of dysuria, frequency, or urgency.
Choice B reason: WBC count 9,000/mm³ is within the normal range of 4,500 to 11,000/mm³ and does not indicate an infection.
Choice C reason: Diminished reflexes are not related to a bladder infection and may be due to aging, neurological disorders, or medication side effects.
Choice D reason: Temperature 37.3°C (99.1°F) is slightly elevated but not indicative of a bladder infection. Older adults may have lower baseline temperatures and may not develop fever in response to an infection.
Explanation
Choice A reason: Cheese is a dairy product that contains protein and fat but little or no fiber.
Choice B reason: Eggs are an animal product that contains protein and fat but no fiber.
Choice C reason: Yogurt is a dairy product that contains protein and calcium but little or no fiber.
Choice D reason: Pears are a fruit that contains dietary fiber, which can help prevent constipation, lower cholesterol levels, and regulate blood sugar levels.
Explanation
Choice A reason: Isoniazid is an antitubercular drug that can cause urine to turn dark yellow or brown, not red-orange.
Choice B reason: Metoprolol is a beta-blocker that can cause urine to turn blue-green, not red-orange.
Choice C reason: Rifampin is an antitubercular drug that can cause urine to turn red-orange, as well as other body fluids such as saliva, sweat, and tears.
Choice D reason: Furosemide is a diuretic that can cause urine to become more concentrated and darker in color, but not red-orange.
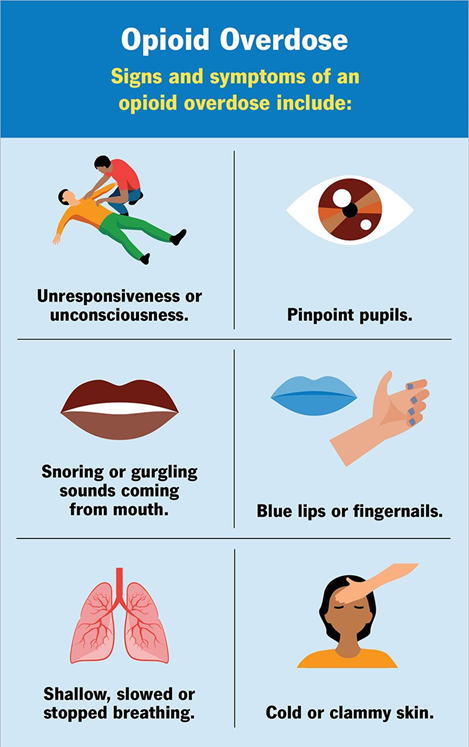
A nurse is collecting data from a client who is experiencing opioid toxicity. Which of the following findings should the nurse expect?
Explanation
Choice A reason: Pupillary dilation is not a sign of opioid toxicity, but rather of opioid withdrawal or stimulant overdose. Opioid toxicity causes pupillary constriction or miosis.
Choice B reason: Hypotension is a sign of opioid toxicity sign of opioid toxicity, as opioids can depress the central nervous system and reduce cardiac output and peripheral resistance.
Choice C reason: Chest pain is not a sign of opioid toxicity, but rather of cardiac ischemia or infarction, which can be caused by cocaine or other stimulants.
Choice D reason: Diaphoresis is not a sign of opioid toxicity, but rather of opioid withdrawal or hyperthermia, which can be caused by ecstasy or other stimulants.
Explanation
Choice A reason: Applying a motion sensor mat to the client's bed is an appropriate action to prevent wandering and alert the staff if the client tries to get out of bed.
Choice B reason: Moving the overbed table away from the bed is not an effective action to prevent wandering, as it does not restrict the client's mobility or provide any supervision.
Choice C reason: Raising all four side rails while the client is in bed is an inappropriate action that can increase the risk of injury or entrapment if the client attempts to climb over them.
Choice D reason: Leaving the television on in the client's room is not an effective action to prevent wandering, as it does not provide any stimulation or distraction for the client.
Explanation
Choice A reason: Replacing the unit when the drainage chamber is full is not an appropriate action, as it can disrupt the negative pressure and cause air leaks or infection. The nurse should empty the drainage chamber when it is half-full and record the amount.
Choice B reason: Pinning the tubing to the client's bed sheets is not an appropriate action, as it can cause kinks or occlusions in the tubing and impair drainage. The nurse should secure the tubing to the client's gown or chest wall with tape.
Choice C reason: Monitoring for at least 150 mL of drainage every hour is an appropriate action, as it can indicate excessive bleeding or fluid accumulation in the pleural space. The nurse should report any sudden increase or decrease in drainage to the provider.
Choice D reason: Clamping the tube for 30 min every 8 hr is not an appropriate action, as it can cause tension pneumothorax or fluid retention in the pleural space. The nurse should only clamp the tube briefly when changing the dressing or checking for air leaks.
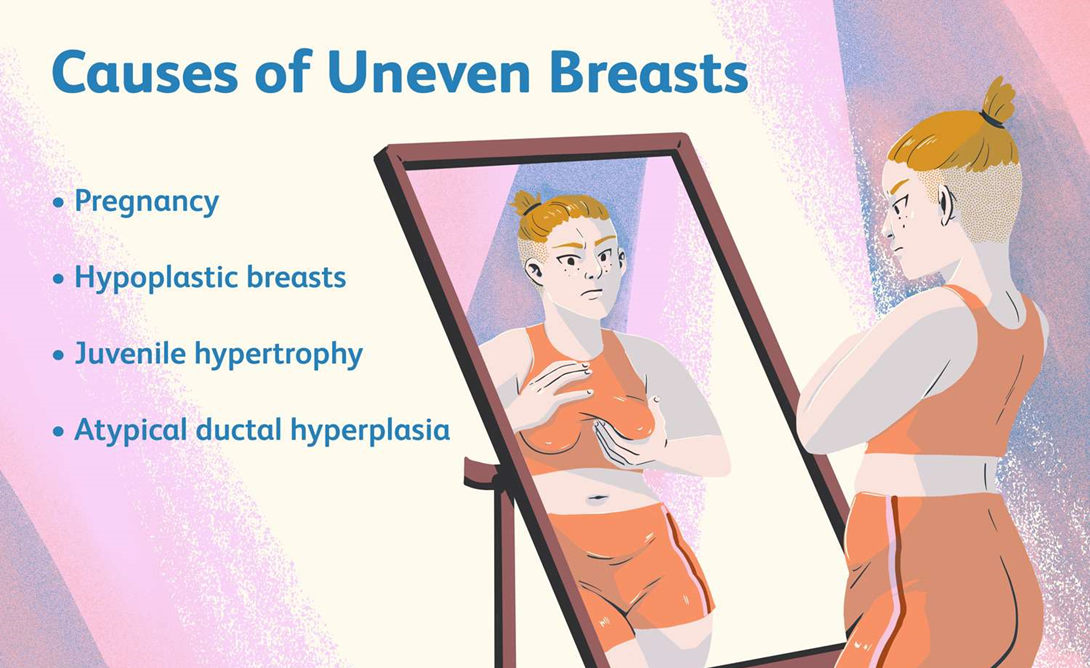
A nurse is reinforcing teaching with a client about breast self-examinations. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason: Performing breast exams every other month is not an adequate frequency, as it can delay the detection of any changes or abnormalities. The client should perform breast exams monthly, preferably a few days after their period ends.
Choice B reason: Having one breast larger than the other is a common variation and not a cause for concern, unless there is a sudden change in size or shape. The client should be aware of their normal breast appearance and report any changes to their provider.
Choice C reason: Performing breast exams the day their period begins is not an optimal time, as their breasts may be swollen, tender, or lumpy due to hormonal fluctuations. The client should perform breast exams when their breasts are not affected by their menstrual cycle, such as a week after their period ends.
Choice D reason: Having skin dimpling on their breasts is not a common variation and may indicate an underlying tumor that pulls on the connective tissue and causes puckering of the skin. The client should inspect their breasts for any changes in skin texture, such as dimpling, peau d'orange, or redness, and report them to their provider.
Explanation
Choice A reason: Taking ibuprofen or other nonsteroidal anti-inflammatory drugs (NSAIDs) can cause a false-positive result on a fecal occult blood screening test, as they can irritate the gastrointestinal mucosa and cause bleeding.
Choice B reason: Having a hemorrhoidectomy 1 year ago is unlikely to cause a false-positive result on a fecal occult blood screening test, as hemorrhoids are usually a source of bright red blood that can be seen with naked eye, not occult blood that requires chemical detection.
Choice C reason: Having a history of breast cancer is not related to a false-positive result on a fecal occult blood screening test, as breast cancer does not affect the gastrointestinal tract or cause bleeding in stool.
Choice D reason: Consuming citrus juice 3 days before the test is not likely to cause a false-positive result on a fecal occult blood screening test, as citrus juice does not contain any substances that can interfere with the chemical reaction of the test. However, consuming red meat, raw vegetables, vitamin C supplements, or iron supplements within 3 days before the test can cause false-negative results, as they can mask or degrade occult blood in stool.
Explanation
Choice A reason: Ammonia 55 mg/dL is within the normal range of 15 to 60 mg/dL and does not indicate any liver dysfunction or bleeding risk.
Choice B reason: Bilirubin 1.0 mg/dL is within the normal range of 0.3 to 1.2 mg/dL and does not indicate any liver damage or jaundice.
Choice C reason: Aspartate aminotransferase 34 units/L is within the normal range of 10 to 40 units/L and does not indicate any liver inflammation or injury.
Choice D reason: Platelets 60,000/mm³ is below the normal range of 150,000 to 450,000/mm³ and indicates thrombocytopenia, which is a low platelet count that can increase the risk of bleeding during or after the liver biopsy. The nurse should report this value to the provider and monitor the client for signs of bleeding, such as bruising, petechiae, hematuria, or melena.
Explanation
Choice A reason: Withholding the medication if the systolic blood pressure is less than 90 mm Hg is an appropriate action, as propranolol is a beta-blocker that can lower blood pressure and cause hypotension, which can impair tissue perfusion and cause dizziness, fainting, or shock.
Choice B reason: Requesting a dosage increase if the apical heart rate is less than 60/min is an inappropriate action, as propranolol can slow down the heart rate and cause bradycardia, which can lead to fatigue, weakness, or cardiac arrest. The nurse should monitor the apical pulse before administering propranolol and withhold it if it is less than 60/min.
Choice C reason: Informing the client to expect increased hair growth is an incorrect statement, as propranolol does not cause hypertrichosis or excessive hair growth. However, another beta-blocker, minoxidil, can cause this side effect.
Choice D reason: Administering the medication with an antacid is not an appropriate action, as antacids can interfere with the absorption of propranolol and reduce its effectiveness. The nurse should administer propranolol on an empty stomach or with food that does not contain antacids.
A nurse is reinforcing teaching about meal planning with a client who has hypertension. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason: Having a bologna sandwich is not a good choice for a client who has hypertension, as bologna is a processed meat that contains high amounts of sodium and saturated fat, which can raise blood pressure and cholesterol levels.
Choice B reason: Seasoning food with vinegar is a good choice for a client who has hypertension, as vinegar is a low-sodium condiment that can add flavor and acidity to food without increasing blood pressure.
Choice C reason: Seasoning food with ketchup is not a good choice for a client who has hypertension, as ketchup is a high-sodium condiment that can increase blood pressure and fluid retention.
Choice D reason: Having canned soup is not a good choice for a client who has hypertension, as canned soup is a high-sodium food that can increase blood pressure and fluid retention. The client should choose low-sodium or homemade soup instead.

Explanation
Choice A reason: Passing of flatus is not a reliable indicator of colostomy function, as it can occur even when there is an obstruction or ischemia in the bowel.
Choice B reason: Stoma is pinkish-red is a sign of a healthy and well-perfused colostomy, as it indicates that the blood supply to the bowel segment is adequate and there is no necrosis or infection.
Choice C reason: Tolerating a clear liquid diet is not a specific indicator of colostomy function, as it does not reflect the amount or consistency of the stool output.
Choice D reason: Absent bowel sounds are not a normal finding for a colostomy, as they can indicate a paralytic ileus or a bowel obstruction, which can cause complications such as distension, pain, or perforation.
Explanation
Choice A reason: Prone position is not appropriate for a paracentesis, as it can compress the abdominal organs and make it difficult to access the peritoneal cavity.
Choice B reason: Knees elevated position is not appropriate for a paracentesis, as it can increase the intra-abdominal pressure and reduce the amount of fluid that can be drained.
Choice C reason: Lithotomy position is not appropriate for a paracentesis, as it can expose the genital area and increase the risk of infection or injury.
Choice D reason: Leaning forward position is appropriate for a paracentesis, as it can shift the abdominal organs upward and allow more space for the needle insertion and fluid drainage.
Explanation
Choice A reason: Applying restraints to the client is not an appropriate action, as it can cause injury or suffocation to the client during a seizure. The nurse should protect the client from harm by removing any nearby objects and padding the side rails.
Choice B reason: Administering an IV bolus of lorazepam is an appropriate action, as lorazepam is an anticonvulsant drug that can stop or shorten the duration of a seizure by enhancing the inhibitory effects of gamma-aminobutyric acid (GABA) in the brain.
Choice C reason: Placing the client in the prone position is not an appropriate action, as it can obstruct the airway and cause respiratory distress or aspiration during a seizure. The nurse should place the client in the side-lying position to facilitate drainage of oral secretions and prevent tongue biting.
Choice D reason: Inserting a tongue blade into the client's mouth is not an appropriate action, as it can cause oral trauma or choking during a seizure. The nurse should never force anything into the client's mouth during a seizure and should allow them to breathe spontaneously.
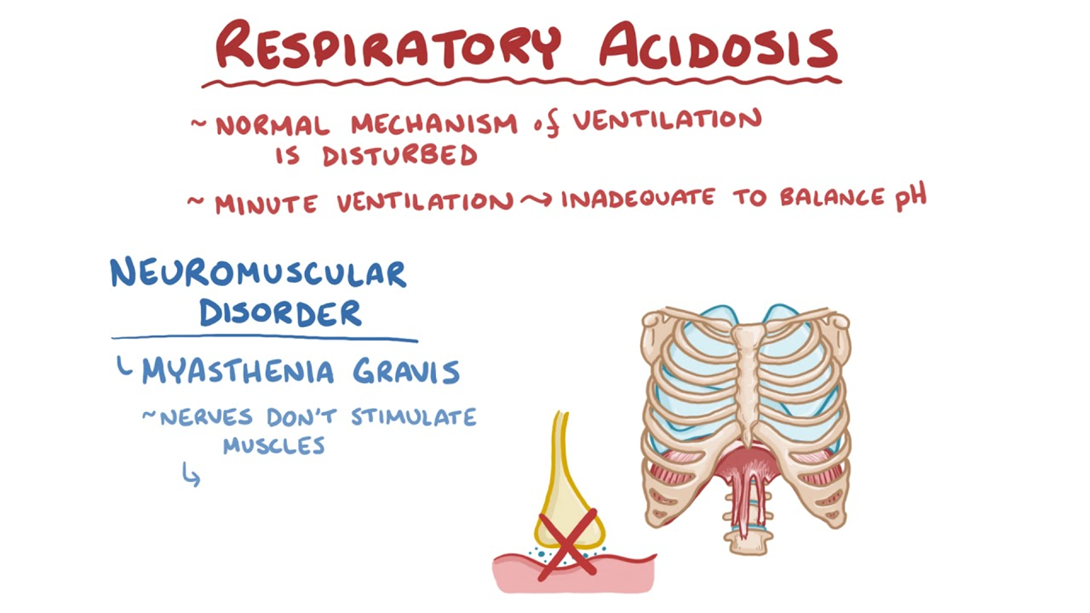
A nurse is reviewing the ABG values of a client who has pneumonia. Which of the following findings indicates the client is developing respiratory acidosis?
Explanation
Choice A reason: PaO2 85 mmHg is within the normal range of 80 to 100 mmHg and does not indicate any hypoxemia or oxygen deficiency.
Choice B reason: pH 7.47 is within the normal range of 7.35 to 7.45 and does not indicate any acid-base imbalance.
Choice C reason: HCO3 25 mEq/L is within the normal range of 22 to 26 mEq/L and does not indicate any metabolic disturbance.
Choice D reason: PaCO2 55 mmHg is above the normal range of 35 to 45 mmHg and indicates respiratory acidosis, which is a condition where the lungs cannot eliminate enough carbon dioxide and the blood becomes too acidic. This can be caused by pneumonia, which can impair gas exchange and ventilation.
Explanation
Choice A reason: Wiping the top of the feeding container with alcohol is not a priority action, as it is not essential for infection control or safety. The nurse should use a sterile technique when opening and handling the feeding container.
Choice B reason: Placing the head of the client's bed at a 30° angle or higher is a priority action, as it can prevent aspiration or regurgitation of the feeding solution into the lungs, which can cause pneumonia or respiratory distress.
Choice C reason: Rinsing the feeding bag with water once the feeding is complete is not a priority action, as it can be done after ensuring that the client has tolerated the feeding well and has no signs of complications.
Choice D reason: Documenting the client's response to the feeding is not a priority action, as it can be done after performing other interventions and assessments that are more urgent and important for the client's well-being.
Explanation
Choice A reason: 0.9% sodium chloride or normal saline is the only solution that should be administered with PRBCs, as it has an isotonic osmolarity and pH that are compatible with blood products and can prevent hemolysis or clotting.
Choice B reason: Dextrose 5% in water or D5W should not be administered with PRBCs, as it has a hypotonic osmolarity that can cause hemolysis or rupture of red blood cells due to osmotic pressure.
Choice C reason: Lactated Ringer's or LR should not be administered with PRBCs, as it contains calcium and lactate that can interfere with blood coagulation and cause clotting or embolism.
Choice D reason: Dextrose 5% in 0.45% sodium chloride or D5½NS should not be administered with PRBCs, as it has a hypotonic osmolarity that can cause hemolysis or rupture of red blood cells due to osmotic pressure.
A nurse is reinforcing teaching with a client who is taking oxybutynin. The nurse should tell the client that the medication will have which of the following effects?
Explanation
Choice A reason: Oxybutynin is an anticholinergic drug that relaxes the muscles of the bladder and reduces spasms, urgency, and frequency of urination. It is used to treat overactive bladder and urinary incontinence.
Choice B reason: Oxybutynin does not increase tissue perfusion in the lungs, as it has no effect on the respiratory system. It can actually cause dry mouth, nasal congestion, and blurred vision as side effects.
Choice C reason: Oxybutynin does not increase venous return to the heart, as it has no effect on the cardiovascular system. It can actually cause tachycardia, palpitations, and hypertension as side effects.
Choice D reason: Oxybutynin does not relax the muscles of the colon, as it has no effect on the gastrointestinal system. It can actually cause constipation, nausea, and abdominal pain as side effects.
A nurse is reviewing the laboratory data of a client who is 1 day postoperative following an abdominal hysterectomy. Which of the following findings should the nurse report to the provider?
Explanation
Choice A reason: WBC count 10,000/mm³ is within the normal range of 4,500 to 11,000/mm³ and does not indicate any infection or inflammation.
Choice B reason: BUN 20 mg/dL is within the normal range of 10 to 20 mg/dL and does not indicate any renal impairment or dehydration.
Choice C reason: Creatinine 2.3 mg/dL is above the normal range of 0.6 to 1.2 mg/dL and indicates renal dysfunction or damage, which can be caused by blood loss, hypotension, or nephrotoxic drugs during surgery. The nurse should report this value to the provider and monitor the client for signs of acute kidney injury, such as oliguria, edema, or electrolyte imbalances.

Choice D reason: Hematocrit 41% is within the normal range of 37% to 47% for females and does not indicate any anemia or polycythemia.
Explanation
Choice A reason: Filling the pad with sterile water is not necessary, as tap water can be used for an aquathermia pad without increasing the risk of infection or contamination.
Choice B reason: Using safety pins to secure the pad in place is not appropriate, as they can puncture or damage the pad and cause leakage or electric shock.
Choice C reason: Applying the pad for 45 min at a time is not recommended, as it can cause skin burns or tissue damage due to prolonged exposure to heat. The nurse should apply the pad for no more than 20 min at a time and check the skin frequently for signs of redness or blistering.
Choice D reason: Covering the pad prior to use is an important action, as it can prevent direct contact between the pad and the skin and reduce the risk of burns or irritation. The nurse should use a towel or a cloth to cover the pad before applying it to the affected area.
Explanation
Choice A reason: HbA1c or glycated hemoglobin is a measure of average blood glucose levels over the past 2 to 3 months. A lower HbA1c indicates better glycemic control and a lower risk of diabetes complications. The target HbA1c for most people with diabetes mellitus is less than 7%.
Choice B reason: HbA1c 12.5% is very high and indicates poor glycemic control and a high risk of diabetes complications, such as retinopathy, nephropathy, or neuropathy.
Choice C reason: Fasting blood glucose 100 mg/dL is within the normal range of 70 to 99 mg/dL and indicates normal glucose metabolism, but it does not reflect the long-term control of blood glucose levels over the past 3 months.
Choice D reason: Fasting blood glucose 70 mg/dL is at the lower end of the normal range and may indicate hypoglycemia or low blood glucose levels, which can cause symptoms such as sweating, trembling, hunger, or confusion.
Explanation
Choice A reason: Purchasing a stoma cap that can cover and conceal the ileostomy when not in use indicates that the client is in the acceptance stage of grieving, as it shows that they have adapted to their new condition and are able to resume their normal activities and social interactions.
Choice B reason: Having their partner empty their pouch for them every morning indicates that the client is in the denial stage of grieving, as it shows that they are avoiding or rejecting their new condition and are dependent on others for their care.
Choice C reason: Being embarrassed by the odor that comes from their ileostomy indicates that the client is in the depression stage of grieving, as it shows that they have low self-esteem and negative feelings about their new condition and its impact on their quality of life.
Choice D reason: Missing going to their church meetings because of their ostomy indicates that the client is in the anger stage of grieving, as it shows that they have resentment and frustration about their new condition and its interference with their previous routines and values.
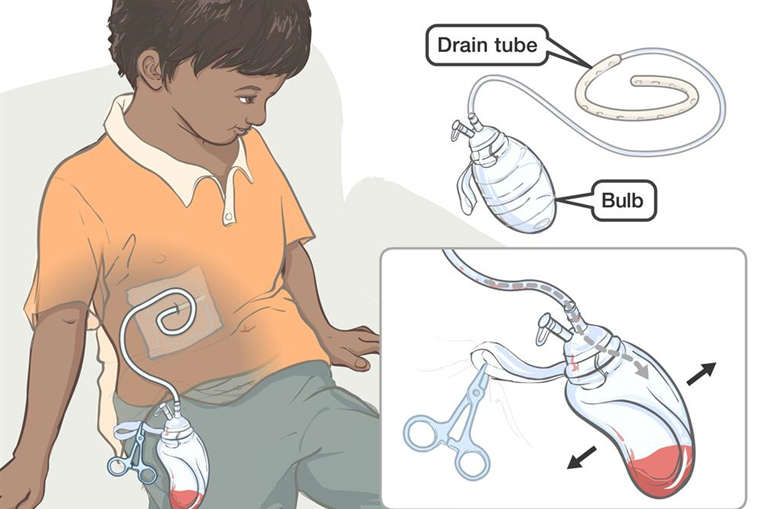
A nurse is caring for a client who is postoperative and has a Jackson-Pratt drain in place. Which of the following actions should the nurse take?
Explanation
Choice A reason: Maintaining the client on bed rest is not an appropriate action, as it can increase the risk of thromboembolism, infection, or atelectasis after surgery. The nurse should encourage early ambulation and exercise as tolerated by the client.
Choice B reason: Decreasing the client's fluid intake is not an appropriate action, as it can cause dehydration, constipation, or impaired wound healing after surgery. The nurse should encourage adequate hydration and nutrition to promote recovery and drainage.
Choice C reason: Applying cold compresses to the site is not an appropriate action, as it can cause vasoconstriction, inflammation, or pain at the site. The nurse should apply warm compresses to the site to facilitate drainage and reduce swelling.
Choice D reason: Placing the right leg in a dependent position is an appropriate action, as it can promote gravity-assisted drainage from the site and prevent fluid accumulation or infection. The nurse should place the drain below the level of the wound and secure it to prevent dislodgment or tension.
Sign Up or Login to view all the 91 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

