PN ati Maternal Newborn 2020
Total Questions : 47
Showing 25 questions, Sign in for moreA nurse is preparing to administer metronidazole 2 g PO. The amount available is 500 mg tablets. How many tablets should the nurse administer? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
To answer this question, the nurse needs to calculate the number of tablets required to give the prescribed dose of metronidazole. The formula for this is:
Number of tablets = (Prescribed dose) / (Available dose) Plugging in the values from the question, we get:
Number of tablets = (2 g) / (500 mg)
Since 1 g = 1000 mg, we can convert 2 g to 2000 mg and simplify the fraction: Number of tablets = (2000 mg) / (500 mg) = 4

A nurse is reviewing the results of a 1-hr glucose screening test for a client who is at 24 weeks of gestation. The client's glucose value is 130 mg/dL. Which of the following actions should the nurse take?
Explanation
A. Repeating the 1-hr glucose test may not provide enough information to confirm or rule out gestational diabetes.
B. Home glucose monitoring is not the standard approach for diagnosing gestational diabetes.
C. Waiting for a routine 1-month appointment delays further assessment and intervention.
D. Instructing the client to return for a 3-hr oral glucose tolerance test is the appropriate next step for a glucose value above the normal range.
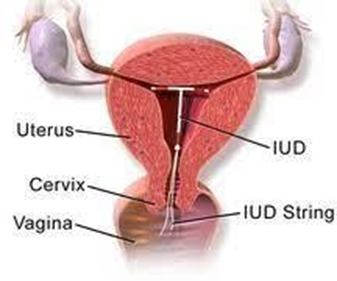
A nurse in a clinic is discussing contraceptive methods with a client. Which of the following methods should the nurse recommend as having the lowest failure rate?
Explanation
A. Intrauterine devices (IUDs) have one of the lowest failure rates among contraceptive methods.
B. Contraceptive sponges have a higher failure rate compared to IUDs.
C. Oral contraceptives, while effective with proper use, have a higher failure rate than IUDs.
D. Diaphragms have a higher failure rate compared to IUDs and may require precise use for optimal effectiveness.
A nurse is reinforcing teaching with a client about how to minimize nausea in the first trimester of pregnancy. Which of the following instructions should the nurse give to the client?
Explanation
A. Eating a slice of dry toast before getting out of bed can help alleviate morning sickness.
B. While staying hydrated is important, drinking water with meals may not specifically address nausea.
C. Limiting snacks between meals may not be as effective in preventing nausea.
D. Having a high-fat snack before going to bed may exacerbate nausea; a dry, bland snack is recommended.
A nurse on a postpartum unit is caring for a client who is breastfeeding and experiencing breast engorgement. Which of the following interventions should the nurse plan to implement to promote comfort for this client?
Explanation
A. Wearing a loose-fitting bra may provide some comfort, but it is not as effective as using ice packs.
B. Ice packs can help reduce inflammation and provide relief from breast engorgement.
C. Purified lanolin is often used for nipple care, not specifically for engorgement.
D. Avoiding a breast pump may exacerbate engorgement; expressing milk can help relieve discomfort.
A nurse is reinforcing teaching about perineal care to a client who is 2 hr postpartum and has an episiotomy and hemorrhoids. Which of the following statements by the client indicates understanding of the teaching?
Explanation
A. Applying heat packs may increase inflammation and should be avoided.
B. Numbing spray is typically used after cleansing, not before.
C. Prolonged sitz baths can exacerbate swelling; shorter durations are recommended.
D. Witch hazel pads can provide relief and help reduce inflammation after urination.
A nurse is assisting with a prenatal class discussion about newborn safety. Which of the following statements by a participant indicates an understanding of the teaching?
Explanation
A. Setting the hot water heater to 120 degrees Fahrenheit is recommended to prevent scalds.
B. Baby powder use is discouraged due to respiratory concerns.
C. Placing the baby's head on a cushion during sleep increases the risk of SIDS, as the baby can roll over or slide down and obstruct their airway.
D. Regularly replacing smoke detector batteries is a crucial safety practice.
A nurse is collecting data from a newborn who is 1 hr old and was born at 43 weeks of gestation. Which of the following findings should the nurse expect? (Select all that apply.)
Explanation
A. A baby born at 43 weeks is likely to have dry, cracked skin.
B. Vernix is typically present on the skin of a newborn, but it may be diminished after 43 weeks.
C. Hypotonia is low muscle tone or weakness, which can indicate a neurological problem or an infection.
D. Excessive lanugo is usually present in pre-term infants and diminished in post- term newborns.
E. Longer nails are common in post-term infants due to continued nail growth in utero.
A nurse in a clinic is reinforcing teaching about signs of effective breastfeeding with a client who has a 5-day-old newborn. Which of the following statements by the client demonstrates an understanding of the teaching?
Explanation
A. While diaper output is important, it may not specifically indicate effective breastfeeding.
B. Feeling the baby swallow during breastfeeding is a sign of effective milk transfer.
C. Bowel movement frequency can vary among infants; it's not the primary indicator of breastfeeding effectiveness.
D. Moderate tenderness may be normal, but pain or discomfort is not expected during effective breastfeeding.
A nurse working on a postpartum unit is collecting data from four clients. Which of the following findings should the nurse report to the provider?
Explanation
A. A reddened area on the calf may suggest a potential deep vein thrombosis (DVT) and requires prompt attention.
B. Painful uterine contractions during breastfeeding are a common postpartum experience and do not typically require immediate reporting.
C. A urinary output of 125 mL in 4 hr may require monitoring but doesn't warrant immediate reporting.
D. Changing a perineal pad every 2 hr is within the normal range and doesn't require urgent attention.
A nurse in a clinic is reinforcing teaching about signs of effective breastfeeding with a client who has a 5-day-old newborn. Which of the following statements by the client demonstrates an understanding of the teaching?
Explanation
A. While diaper output is important, it may not specifically indicate effective breastfeeding.
B. Feeling the baby swallow during breastfeeding is a sign of effective milk transfer.
C. Bowel movement frequency can vary among infants; it's not the primary indicator of breastfeeding effectiveness.
D. Moderate tenderness may be normal, but pain or discomfort is not expected during effective breastfeeding.
A nurse on a postpartum unit is caring for a client who delivered vaginally 24 hr ago. Which of the following should the nurse expect to find when collecting data?
Explanation
A. The uterine fundus should be palpated at or near the level of the umbilicus within the first 24 hours postpartum.
B. Frequent urges to urinate are common due to postpartum diuresis but are not the primary finding.
C. Colostrum, the first milk, is typically expressed from the breasts in the early postpartum period.
D. Lochia serosa is a normal finding, but the primary focus in this question is on colostrum expression.
A nurse is assisting with the care of a newborn whose mother has hepatitis B. Which of the following actions should the nurse plan to take when administering the hepatitis B vaccine?
Explanation
A. The hepatitis B vaccine is typically administered into the vastus lateralis muscle in infants.
B. Inserting the needle at a 45° angle is not specific to the hepatitis B vaccine administration.
C. Parental consent is required before administering any vaccine to a newborn.
D. The first dose of the hepatitis B vaccine is usually given shortly after birth, not at 24 hr after birth.
A nurse in a provider's office is collecting data from a client who is at 34 weeks of gestation and reports having a sudden gush of vaginal fluid. Which of the following manifestations is the priority?
Explanation
A. Elevated maternal temperature may indicate infection, but meconium-stained amniotic fluid takes precedence.
B. Amniotic fluid with meconium suggests fetal distress and requires prompt assessment but is not a priority compared to fetal bradycardia.
C. Foul-smelling vaginal discharge could indicate infection but is not as immediate a concern as meconium-stained fluid.
D. The priority manifestation is the fetal heart rate, which should be between 110 and 160/min.
A nurse is assisting with the care of a client who is in labor and has an epidural infusion for pain management. The client's blood pressure is 80/40 mm Hg. Which of the following actions should the nurse take?
Explanation
A. Methylergonovine is used for postpartum hemorrhage and is not indicated for low blood pressure in labor.
B. Emptying the bladder may be necessary, but a bolus of fluids is the priority in addressing hypotension.
C. A bolus of fluids helps increase blood pressure in the presence of epidural- induced hypotension.
D. Knee-chest position is not the primary intervention for hypotension related to epidural anesthesia.
A nurse is caring for a client who asks about the purpose of a Papanicolaou test. Which of the following responses should the nurse make?
Explanation
A. Papanicolaou (Pap) tests are not used for the removal of uterine fibroids.
B. Pap tests primarily focus on the detection of cervical abnormalities and cancer, not endometriosis.
C. The primary purpose of a Pap test is to screen for cervical cancer and detect abnormal cervical cells.
D. Pap tests are not used to determine ovulation status; they focus on cervical health.
A nurse is reinforcing teaching about laboratory testing with a client who is at 6 weeks of gestation. Which of the following statements should the nurse include?
Explanation
A. Screening for gestational diabetes typically occurs between 24 and 28 weeks of gestation.
B. Group B strep culture is usually performed around 36 weeks of gestation to determine the need for antibiotic prophylaxis during labor.
C. Routine clean catch urine specimens are not required every 2 months during pregnancy.
D. Maternal serum alpha-fetoprotein screening is typically performed around 16 to 18 weeks of gestation.
A nurse is collecting data from an adolescent who is postoperative following a cesarean birth and is receiving morphine for pain. Which of the following findings is the nurse's priority?
Explanation
A. Blood pressure within a normal range is not the priority in this scenario.
B. A respiratory rate of 11/min is concerning and may indicate opioid-induced respiratory depression, requiring immediate attention.
C. Urinary retention is a potential side effect of morphine but is not as immediately critical as respiratory depression.
D. Blurred vision may be a side effect of morphine but is not the priority in this situation.
A nurse is reinforcing teaching about home safety precautions with the guardian of a newborn. Which of the following instructions should the nurse include?
Explanation
A. Placing a small pillow under the newborn's head during naps increases the risk of sudden infant death syndrome (SIDS).
B. The water heater temperature should be set at 49° C (120° F) or lower to prevent scalds.
C. Washing the newborn's face with a warm, soapy washcloth is not a routine hygiene practice.
D. Soft bumper pads in the crib pose a suffocation risk and are not recommended.
A nurse is preparing to administer the hepatitis B vaccine to a newborn. Which of the following actions should the nurse take?
Explanation
A. A 3-inch needle is not necessary for administering the hepatitis B vaccine to a newborn.
B. The recommended dose of the hepatitis B vaccine for newborns is 0.5 mL.
C. A 20-gauge needle is appropriate for administering the vaccine.
D. The hepatitis B vaccine is typically administered into the vastus lateralis muscle, not the dorsal gluteal muscle.
A nurse in an antepartum clinic is reinforcing teaching with a client who is pregnant and has a new prescription for oral ferrous sulfate. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
A. Calcium in milk can interfere with iron absorption; it's not recommended to take iron with milk.
B. Taking iron with breakfast might result in reduced absorption due to the presence of other dietary components.
C. Taking iron with the midday meal can reduce its absorption and effectiveness.
D. Iron is better absorbed when taken with foods or drinks that contain vitamin C, such as orange juice.
A nurse is auscultating fetal heart tones with a Doppler device for a client who is at 12 weeks of gestation. Where should the nurse expect to auscultate the fetal heart tones?
Explanation
A. Auscultating fetal heart tones in the umbilical area is not the standard location.
B. Fetal heart tones are typically not audible below the liver border on the right abdomen at 12 weeks.
C. At 12 weeks of gestation, the uterus is still low in the pelvis and the fetal heart tones can be heard best in the suprapubic area, which is above the pubic bone and below the umbilicus.
D. Auscultating above the left iliac crest is not a standard location for fetal heart tones.
A nurse is caring for a client who is pregnant and has a vaginal culture that is positive for chlamydia. Which of the following medications should the nurse plan to administer?
Explanation
A. Tetracycline is not safe in pregnancy.
B. Metronidazole is used to treat bacterial vaginosis, not chlamydia.
C. Acyclovir is used for the treatment of herpes infections, not chlamydia.
D. Amoxicillin is safe and effective for treating chlamydia during pregnancy.
A nurse is assisting a provider with a pelvic examination of a client during her first prenatal visit. Which of the following actions should the nurse take?
Explanation
A. Emptying the bladder before a pelvic examination provides better access to pelvic structures.
B. Instructing the client to tighten pelvic muscles may interfere with the examination.
C. Sims' position is not typically used for routine pelvic examinations during pregnancy.
D. Encouraging rapid, shallow breaths is not necessary during a pelvic examination.
A nurse is collecting data from a client at a 6-week postpartum checkup. The client tells the nurse, "I am breastfeeding and would like to use a birth control pill." Which of the following statements should the nurse make?
Explanation
A. Breastfeeding does not guarantee contraception; additional birth control methods may be needed.
B. Birth control pills are not contraindicated but should preferably be progestin-only during lactation.
C. Progestin-only pills are preferred during lactation to avoid potential effects on breastfeeding.
D. There is no evidence supporting an increased risk of breast cancer with the use of birth control pills during breastfeeding.
Sign Up or Login to view all the 47 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

