PNU Adult Health II Spring 2023 Exam 2
Total Questions : 50
Showing 25 questions, Sign in for moreA nurse is caring for a client in an acute care mental health unit who was involuntarily admitted for 72 hr after attacking a neighbor. To keep the client in the hospital when the initial time to hold the client expires, which of the following must be determined?
Explanation
Whether the client is a danger to herself or others. When a client is involuntarily admitted to a mental health unit, they are held for an initial period of 72 hours for evaluation and treatment. Afterward, a determination must be made as to whether or not the client is still a danger to themselves or others to keep them in the hospital.
Choices A, C, and D do not address the primary concern of ongoing safety for the client and others.
For choice A, the client's financial status or their ability to pay for prescribed medications is not relevant to their safety or need for hospitalization.
For choice C, the client's ability to make arrangements to stay with someone is important for discharge planning but not for determining their need for ongoing hospitalization.
Finally, for choice D, whether the client is unwilling to accept treatment is important, but not the sole determining factor as to whether they are a danger to themselves or others.
A nurse in a community clinic is speaking to other nurses about risk factors for domestic violence. Which of the following statements by one of the other nurses indicates the need for further teaching?
Explanation
choice C, "I have heard that abusers think of themselves as important and have high self-esteem." This statement is incorrect and shows the nurse may need further education on the characteristics of an abuser. Abusers often lack self-esteem and feel powerless, using abuse as a way to gain control and confidence. Choices A, B, and D are all accurate statements and do not indicate the need for further education.
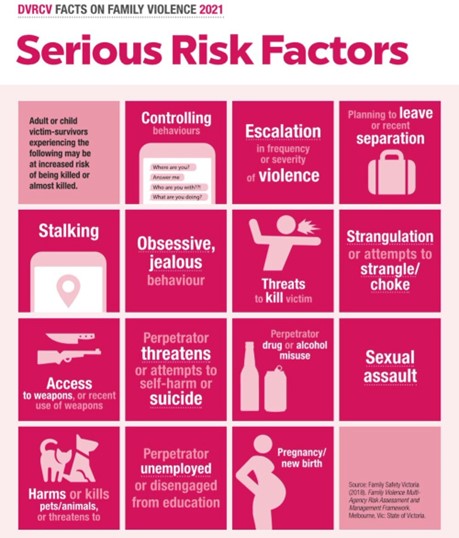
For choice A, abusers often isolate their partner to gain control over them. For choice B, abusers may lack social support and social skills, leading to violent behavior.
For choice D, abusers use intimidation tactics to maintain power in the relationship.
A nurse in an urgent care facility is caring for a client who has traumatic injuries following an assault. The client sits quietly and calmly tells the nurse, "I'm fine." The nurse should recognize the client's behavior as which of the following reactions?
Explanation
The client's behavior of stating "I'm fine" despite having traumatic injuries is an example of denial, a coping mechanism that involves denying that a problem or issue exists. Projection involves attributing one's own feelings to another person, displacement involves redirecting one's emotions onto a less threatening target, and undoing involves seeking to undo or forget past actions.
Choice A, projection, would involve the client attributing their own feelings to others.
Choice B, displacement, would involve the client redirecting their emotions onto someone or something else. Finally,
choice D, undoing, would involve the client attempting to forget or undo past actions.
A nurse facilitating a group therapy session is listening to clients discuss their coping strategies when feeling stressed. Which of the following statements indicates adaptive coping? (Select all that apply.)
Explanation
"I call a friend who makes me smile and laugh," and "I tense and release my muscles, starting with my feet." These are adaptive coping strategies that help to reduce stress and promote relaxation. Calling a friend who makes you smile and laugh, for example, can help to distract from negative thoughts and promote positive emotions. Tense and release exercises can help to reduce muscle tension and promote relaxation.
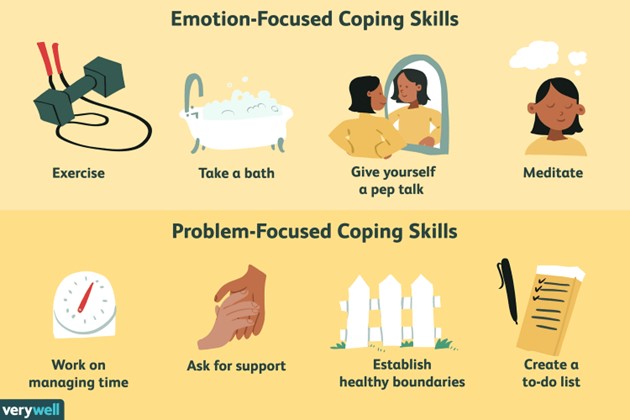
Choice A, "I sleep in in the mornings," is not an adaptive coping strategy because it doesn't address the source of stress and may actually lead to avoidance.
Choice B, "I isolate myself in my room for a few hours when things get overwhelming," is not adaptive because it promotes social withdrawal and avoidance.
Choice D, "I think about being on my favorite beach vacation," is not adaptive because it promotes avoidance and doesn't address the source of stress.
A nurse is helping a client relieve stress through cognitive reframing. Which of the following actions by the client demonstrates effective use of cognitive reframing?
Explanation
"The client learns to change negative thoughts into positive statements." This demonstrates the effective use of cognitive reframing, which involves changing negative thoughts into positive self-talk. This strategy can help to reduce stress and improve coping skills.
Choice A, "The client imagines being in a quiet, relaxing environment," is not an example of cognitive reframing, but rather an example of visualization, which can also be useful in reducing stress.
Choice B, "The client trains his mind to relax by using deep inner resources," is not an example of cognitive reframing, but rather an example of relaxation training.
Choice D, "The client learns the source of his stress by writing down daily events," is not an example of cognitive reframing, but rather an example of stress management through self-reflection.
A nurse on an inpatient unit is caring for a newly-admitted client who has anorexia nervosa. Which of the following actions should the nurse take? (Select all that apply.)
Explanation
"Stay with the client during meals and for 1 hr afterward," and "Monitor the client's weight daily after first voiding." These are important interventions for clients with anorexia nervosa, as they can help to prevent complications such as dehydration and electrolyte imbalances.
Choice B, "Give the client a weight gain goal of 4 to 5 lb per week," is not an appropriate intervention, as it can be overwhelming and may promote unhealthy weight gain.
Choice D, "Encourage the client to keep a diary of daily food intake," may be helpful for some clients, but is not a priority intervention.
Choice E, "Offer specific privileges for sustained weight gain," is not an appropriate intervention.
A nurse is discussing comorbidities associated with eating disorders with a newly licensed nurse. Which of the following comorbidities should the nurse include in the discussion? (Select all that apply.)
Explanation
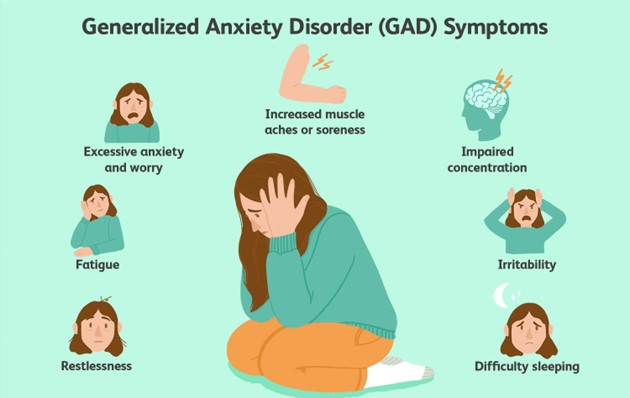
A nurse discussing comorbidities associated with eating disorders with a newly licensed nurse should include depression, anxiety, and obsessive-compulsive disorder (OCD) in the discussion. Clients who have eating disorders often have comorbid psychiatric conditions.
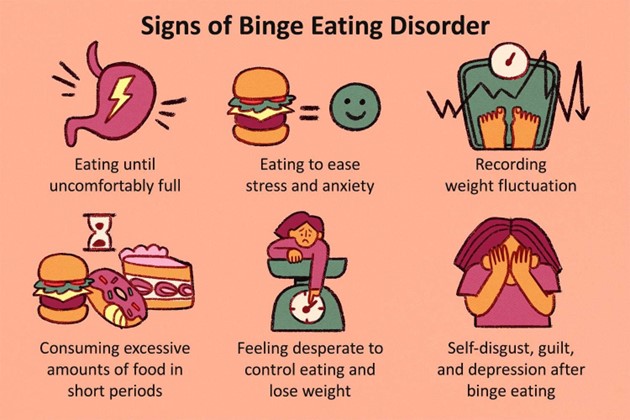
Depression and anxiety are two common conditions among clients with eating disorders. OCD is another condition that is often associated with eating disorders. Clients with OCD may have obsessive thoughts about food intake, weight, and body image. These clients may also engage in compulsive behaviors related to eating, such as calorie counting or food restriction. Options C and E are incorrect because breathing-related sleep disorders and schizophrenia are not typically associated with eating disorders.
An assistive personnel (AP) says to the nurse, "This client is incontinent of stool three or four times a day. I get angry because I think that the client might be doing it just to get attention." Which of the following responses by the nurse is therapeutic?
Explanation
When an assistive personnel expresses concerns or vents about client behaviors, a therapeutic response is necessary. Asking the AP to explain or to further describe his or her thoughts, feelings, or concerns will allow the AP to reflect on these issues and help clarify any misconceptions or misunderstandings. The nurse's response should be nonjudgmental, noncritical, and focused on the AP's perceptions and feelings.
Option A is confrontational and Option C is inappropriate because it suggests that the AP is not spending enough time with the client.
Option D shifts responsibility for managing the client's behavior to the nurse instead of helping the AP reflect on his or her perception of the situation.
A nurse is caring for a client who reports acute anxiety. Which of the following actions should the nurse take first?
Explanation
If a client reports acute anxiety, the nurse's first priority should be to remain with the client. The nurse should provide a safe, supportive environment for the client and help the client feel less anxious. This can be accomplished by staying with the client, listening attentively to the client, and offering reassurance and support. Options A and D are appropriate actions to take when caring for a client with anxiety, but they are not the first priority.
Option B may be an appropriate intervention when caring for a client with anxiety, but it is not the first priority.
A nurse is collecting data from a female client who has anorexia nervosa. Which of the following findings should the nurse expect?
Explanation
When collecting data from a female client who has anorexia nervosa, the nurse should expect a finding of low bone density.
Anorexia nervosa is an eating disorder characterized by self-starvation, distorted body image, and a fear of gaining weight. Clients with anorexia nervosa are at risk for severe malnutrition, which can lead to a variety of complications, including bone loss and osteoporosis.
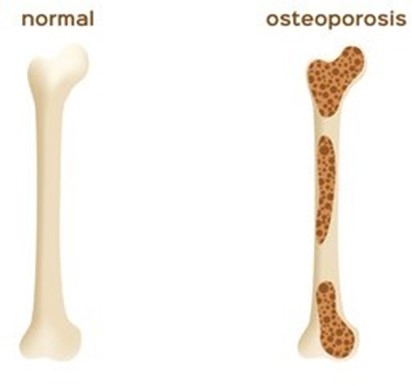
Options A, B, and C are incorrect findings in a client with anorexia nervosa. Decreased cholesterol levels may be an indication of malnutrition. Heavy monthly periods, or menstrual irregularities, may occur in clients with anorexia nervosa because of the hormonal changes that can result from severe weight loss. Elevated serum potassium levels are not a common finding in a client with anorexia nervosa.
A nurse is caring for a 20-year-old college student who has a 2-year history of bulimia nervosa. She tells the nurse, "I know my eating binges and vomiting are not normal, but I cannot do anything about them." Which of the following is a therapeutic response by the nurse?
Explanation
A therapeutic response to the client's statement would be to acknowledge that the client feels helpless about the behavior. The nurse should avoid judging or criticizing the client and instead focus on offering support and empathy.
Options A and B are not therapeutic because they are confrontational and may make the client defensive. Option C is a well-intentioned but empty statement that does not offer any practical support or guidance to the client.
A nurse in an addiction rehabilitation center is contributing to the plan of care for a newly admitted client who has an alcohol use disorder. Which of the following interventions is the nurse's priority?
Explanation
Accompany the client when ambulating. The nurse’s priority when caring for a client with alcohol use disorder and who is experiencing withdrawal symptoms is to prevent harm to the client. Physiologic manifestations of alcohol withdrawal syndrome include seizures, delirium tremens (DTs), and hallucinations. Therefore, ensuring the client’s safety is of the utmost importance. Accompanying the client when ambulating is the priority intervention as alcohol withdrawal may lead to ataxia, weakness, and dizziness which may lead to falls.
Choice A, placing the client in a private room, does not address the client’s physical needs.
Choice B, determining the client's level of disorientation, is something necessary to assess but not the priority.
Choice C, padding the side rails of the bed with towels, is not the priority intervention, and contributes little to the prevention of falls.
A nurse is caring for a client with whom he has developed a therapeutic relationship and who will be discharged later in the day. The client thanks the nurse for his help during the hospitalization. Which of the following responses should the nurse make?
Explanation
"I know you will do well living out in the community.". When a client expresses feelings of gratitude towards a nurse as they are about to be discharged, they are mostly affirming the therapeutic relationship between both parties. The nurse should acknowledge this affirmation clearly, warmly, and humbly, while encouraging the client's progress and independence. Choice D, "I know you will do well living out in the community" acknowledges the client's progress and offers encouragement.
Choice A, "Aren't you excited about being discharged today?" is a closed question that does not encourage the client's progress.
Choice B, "How do you feel about being discharged?" is not the best response because it is too broad.
Choice C, "I will send you a note in a few weeks" does not offer affirmation and encouragement to the client.
A nurse is caring for a client who has an alcohol use disorder and is experiencing withdrawal. Which of the following interventions is the nurse's priority?
Explanation
Prevent the client from harming herself or others. Withdrawal from alcohol can lead to autonomic hyperactivity and is most concerning when it involves seizures, deliriums tremens, and hallucinations which can be potentially life-threatening. Therefore, the nurse's priority when caring for a client experiencing alcohol withdrawal is to prevent harm to the client by implementing seizure precautions and monitoring the client's vital signs.
Choice A, identifying the use of defense mechanisms, is an important aspect of treatment but can be addressed later.
Choice C, supporting the client's coping skills, is not a priority intervention.
A nurse is discussing insomnia management techniques with a group of clients who have anxiety disorders. Which of the following techniques mentioned by a client requires further teaching?
Explanation
"I watch the television in my bedroom to help me sleep." This technique requires further teaching as watching TV before sleep is a poor sleep hygiene habit. Clients should be advised to keep TVs, mobile phones, and other electronic devices out of the bedroom, as electronic devices can be a source of stimulation and disrupt a sleep routine. Adequate sleep hygiene techniques include going to bed and waking up at the same time every day, avoiding caffeine, nicotine, and alcohol, and engaging in physical activity early in the day. Reading for a few minutes or engaging in some other relaxing activity can reduce difficulty falling back to sleep.
Option A: "If I wake up at night, I go to another room and read for 20 minutes" - This is a good sleep hygiene habit
Option B: "I eat my evening meal at least 3 hours before I go to bed" - This is a good sleep hygiene habit Option D: "I have stopped taking naps in the afternoon" - This is a good sleep hygiene habit Each of the other options helps with good sleep hygiene but C will not help.
A nurse is caring for a client following reported physical abuse. The client is quiet and withdrawn. Which of the following actions should the nurse take?
Explanation
"Be direct and honest when communicating with the client." Being direct and honest with the client about the situation is essential to build trust and promote open communication. Protecting client confidentiality and privacy is crucial for client safety and well-being. If the client feels comfortable in a safe and non-threatening environment, then they are more likely to open up and discuss their situation. Displaying disapproval or probing the client can make the situation worse and result in the client withdrawing further. Inviting a family member to be present during the nursing history is not appropriate given the sensitive and personal nature of the discussion.
Option A: "Display disapproval toward the perpetrator" - Not appropriate for the clinical setting
Option B: "Probe the client to offer a factual account of the abuse" May make the client withdraw more, not appropriate for the clinical setting
Option D: "Invite a family member to be present for the nursing history" - Not appropriate for the sensitive nature of the discussion Each of the other options is not appropriate given the sensitive nature of the conversation.
A nurse in an urgent care clinic is caring for a client who is using loud and rapid speech and continuously repeats, "I don't know why my wife left me." Which of the following levels of anxiety is the client experiencing?
Explanation
Moderate. According to the Mayo Clinic moderate anxiety is characterized by symptoms such as loud and rapid speech, difficulty concentrating, restlessness, and increased worry. The client's behavior matches these symptoms, indicating that they are experiencing moderate anxiety.
Choice B. Panic is incorrect because panic is a severe form of anxiety that involves symptoms such as chest pain, shortness of breath, trembling, and a sense of impending doom. The client does not exhibit these symptoms.
Choice C. Severe is incorrect because severe anxiety is marked by symptoms such as irrational fear, detachment from reality, hallucinations, and loss of control¹². The client does not show these symptoms.
Choice D. Mild is incorrect because mild anxiety is associated with symptoms such as nervousness, increased alertness, and slight discomfort¹². The client's symptoms are more intense than mild anxiety.
A nurse is caring for a client who witnessed her brother's homicide and has posttraumatic stress disorder (PTSD). Which of the following findings should the nurse expect?
Explanation
The client is easily startled by loud voices. Clients with posttraumatic stress disorder (PTSD) may exhibit hyperarousal symptoms, including exaggerated startle responses and hypervigilance. The client talking constantly about the traumatic experience is a possible finding in PTSD but not specific. The client is constantly drowsy and sleeping 11-12 hours daily is more associated with depression than PTSD. While the client may have satisfying personal relationships, it does not address the question of what finding to expect with PTSD, making choice C incorrect.
Reasons why the other choices are not answers:
Choice A, the client talking constantly about the traumatic experience, is a possible symptom of PTSD, but it is not specific to the disorder and may also indicate other disorders.
Choice B, the client being constantly drowsy and sleeping 11-12 hours daily, is more indicative of depression than PTSD and also does not address the question of finding expected with PTSD.
Choice C, the client reports satisfying personal relationships with family and close friends, does not address what finding is expected with PTSD, making it an incorrect answer.
Which statement by the client indicates an understanding of the information provided about sertraline?
Explanation
Sertraline is a medication used to treat depression and other mental health conditions that can cause unwanted side effects. Excessive sweating and muscle twitching are potential side effects that should be immediately reported to the healthcare provider. A dry cough is a common side effect of other medications and not specific to sertraline.
Decreasing sodium intake is not necessarily related to the medication, and harmless, temporary changes in the ability to taste and smell are not significant enough to warrant special mention.
 Choice B, "This medication can cause a dry cough," is a potential side effect of other medications and may cause confusion as to what medication the client is taking.
Choice B, "This medication can cause a dry cough," is a potential side effect of other medications and may cause confusion as to what medication the client is taking.
Choice C, "I need to decrease my sodium intake while on this medication," is not likely a statement related to sertraline but to other medications or medical conditions.
Choice D, "This medication can cause harmless, temporary changes to my ability to taste and smell," while accurate, is not the most critical information for the client to know about and may cause confusion as to what the client should report to the provider.
The nurse is collecting data from a client with obsessive-compulsive disorder (OCD). Which of the following findings should the nurse expect? (Select all that apply.)
Explanation
The client with OCD may experience difficulty relaxing and often feels tense, anxious, and irritable. They may engage in rule-conscious behavior and exhibit perfectionist tendencies, as well as experience compulsive behaviors. These behaviors may be time-consuming and interfere with daily activities.
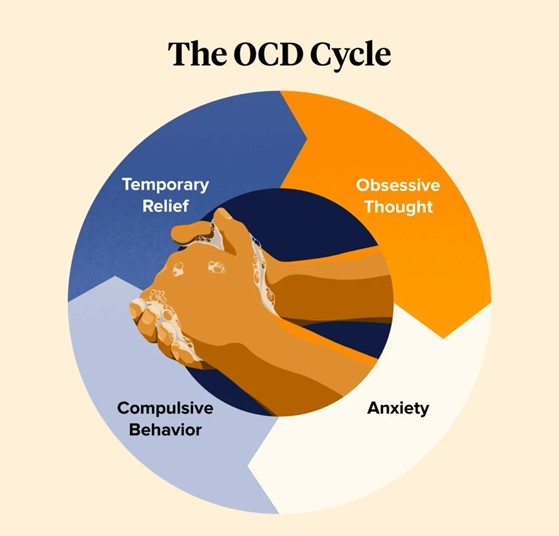
Option A is incorrect because irrational fear of certain objects is more indicative of a phobia than OCD.
Option C is incorrect because clients with OCD are usually aware of their compulsions and may even try to resist them.
Reasons why the other options are not correct answers:
Option A: Irrational fear of certain objects is more indicative of a phobia than OCD.
Option C: Clients with OCD are usually aware of their compulsions and may even try to resist them.
A nurse in a community clinic is caring for a 20-month-old toddler who has spiral fractures of the right ulna and radius. Which of the following findings should the nurse recognize as a potential indication of abuse?
Explanation
The parents report that the child injured herself by falling off the couch.
A spiral fracture is a type of broken bone that occurs when a twisting force is applied to the bone. It is often seen in cases of child abuse, where the abuser grabs and twists the child's arm or leg.
Choice A is not correct because bringing the child to the facility soon after the injury does not rule out abuse. The abuser may have done so to avoid suspicion or to prevent further complications.
Choice B is not correct because crying when the arm is examined is a normal reaction for a child who is in pain and scared. It does not indicate abuse or neglect.
Choice C is correct because it is unlikely that a fall from a couch would cause a spiral fracture of the ulna and radius. These bones are strong and require a lot of force to break. A fall from a couch would more likely cause a greenstick fracture, which is a partial break of the bone that occurs in children with flexible bones.
Choice D is not correct because a single injury does not exclude abuse. The child may have been abused before and healed without medical attention, or the abuser may have targeted only one part of the body. A single injury should still raise suspicion and prompt further investigation.
A nurse is discussing the reporting of child abuse with a newly licensed nurse. Which of the following statements by the newly licensed nurse indicates an understanding of the teaching?
Explanation
If suspicion of abuse exists then reporting is mandatory.
Choice A is incorrect because civil liability does not depend on whether the abuse can be proven or not, but on whether the report was made in good faith or not.
Choice B is incorrect because evidence of abuse does not need to be collected prior to reporting, but only reasonable suspicion of abuse.
Choice C is incorrect because reporting is not voluntary for healthcare workers, but mandatory by law.
Choice D is correct because if suspicion of abuse exists then reporting is mandatory for any person, agency, organization, or entity with direct knowledge of child abuse or neglect.
A nurse is caring for an older adult client who has dementia and is agitated. The client says, "I have to go home and see my mother." The nurse replies, "You miss your mother." Which of the following therapeutic techniques is the nurse using?
Explanation
Validation. Validation is a therapeutic technique that involves acknowledging and accepting the feelings and emotions of the person with dementia, even if they are not based on reality. Validation helps to reduce agitation and anxiety and promotes dignity and respect.
The other choices are not correct for the following reasons:
Remotivation is a technique that aims to stimulate the person's interest in the present and future, by providing factual information and encouraging participation in activities. Remotivation may not be appropriate for someone who is agitated and living in the past.
Orientation to reality is a technique that involves correcting the person's misperceptions and confusions, by providing factual information about time, place, and identity. Orientation to reality may increase agitation and frustration and may damage the person's self-esteem.
Guided imagery is a technique that involves using mental images to promote relaxation and well-being. Guided imagery may not be effective for someone who has difficulty with attention, concentration and memory.
A nurse is caring for a client who is experiencing opioid withdrawal. Which of the following medications should the nurse anticipate the provider to prescribe?
Explanation
Methadone. Methadone is a synthetic opioid that can help reduce the symptoms of opioid withdrawal and prevent relapse.
Methadone acts on the same receptors as other opioids, but it has a longer duration of action and a lower potential for abuse. Methadone is given in controlled doses as part of an opioid treatment program.
The other choices are not correct because:
Choice A. Risperidone is an antipsychotic medication that has no effect on opioid withdrawal.
Choice C. Lithium carbonate is a mood stabilizer that is used to treat bipolar disorder and has no effect on opioid withdrawal.
Choice D. Disulfiram is a medication that inhibits the metabolism of alcohol and causes unpleasant reactions when alcohol is consumed. It has no effect on opioid withdrawal.
A nurse is collecting data on an adolescent client who has attention deficit hyperactivity disorder (ADHD). Which of the following manifestations should the nurse expect to find?
Explanation
Difficulty maintaining sustained attention is a common manifestation of ADHD, according to the American Psychiatric Association and the CDC. This means that people with ADHD often have trouble focusing on tasks or activities for a long period of time, especially if they are boring or tedious.
The other choices are not manifestations of ADHD, but of other conditions or problems. Here are some reasons why:
Choice A: Difficulty using words in context is not a symptom of ADHD, but of a language disorder or a learning disability that affects communication skills.
Choice B: Difficulty performing self-grooming activities is not a symptom of ADHD, but of a physical disability, a mental health disorder, or a lack of motivation or self-care.
Choice C: Difficulty in acquiring reading skills is not a symptom of ADHD, but of dyslexia, which is a specific learning disability that affects reading and spelling.
Sign Up or Login to view all the 50 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

