Postpartum AMD Newborn Care
Total Questions : 41
Showing 25 questions, Sign in for moreThe nurse is conducting a prenatal class explaining the various activities that will occur within the first few hours after birth. The nurse determines the session is successful when the couples correctly choose which reason for the use of an antibiotic ointment.
Explanation
Prevent infection of the eyes from vaginal bacteria. This is because some newborns can be exposed to bacteria such as gonorrhea or chlamydia during delivery, which can cause a serious eye infection called gonococcal ophthalmia neonatorum (GON). Applying an antibiotic ointment such as erythromycin or ilotycin can prevent GON and other less severe eye infections by killing the bacteria.
Choice A is not correct because the umbilical cord does not need antibiotic ointment to prevent infection. It should be kept clean and dry until it falls off naturally.
Choice C is not correct because the tear ducts are not affected by vaginal bacteria. They are small tubes that drain tears from the eyes to the nose.
Choice D is not correct because the urethra is not a common site of infection for newborns. The urethra is the tube that carries urine from the bladder to the outside of the body.
A nurse is caring for a postpartum client who saturates a perineal pad in 10 minutes. Which of the following actions should the nurse take first?
Explanation
Massage the client’s fundus. This is because the most common cause of postpartum hemorrhage is uterine atony, which is the failure of the uterus to contract after delivery. Massaging the fundus can stimulate uterine contractions and reduce bleeding by compressing the blood vessels at the placental site.
Choice A is not correct because administering oxytocin is not the first action to take. Oxytocin is a medication that can also help the uterus contract, but it should be given after assessing the uterine tone and bleeding.
Choice B is not correct because observing for pooling of blood under the buttocks is not a priority action. It can help estimate the amount of blood loss, but it does not address the cause of bleeding or stop it.
Choice C is not correct because checking the client’s blood pressure is not the first action to take. Blood pressure can indicate hypovolemia due to blood loss, but it is not a sensitive indicator and may remain normal until a significant amount of blood is lost.
The nurse assesses a postpartum woman's perineum and notices that her lochial discharge is moderate in amount and red. The nurse would record this as what type of lochia?
Explanation
This is because lochia rubra is the first stage of lochia, the vaginal discharge after giving birth. It comprises blood, shreds of fetal membranes, decidua, vernix caseosa, lanugo, and membranes. It is red in color because of the large amount of blood it contains. It lasts 1 to 4 days after birth.
Choice A is not correct because lochia alba is the last stage of lochia. It is whitish or yellowish-white in color and contains fewer red blood cells and more leukocytes, epithelial cells, cholesterol, fat, mucus, and microorganisms. It lasts from the second through the third to sixth weeks after delivery.
Choice B is not correct because there is no such thing as lochia normal. Lochia has three stages: lochia rubra, lochia serosa and lochia alba.
Choice C is not correct because lochia serosa is the second stage of lochia. It is brownish or pink in color and contains serous exudate, erythrocytes, leukocytes, cervical mucus, and microorganisms. It lasts for 4 to 12 days after delivery.
What is the primary rationale for monitoring a new mother every 15 minutes for the first hour after delivery?
Explanation
To check for postpartum hemorrhage.
This is because postpartum hemorrhage is a serious and potentially life-threatening complication that can occur within 24 hours of birth or later. It is defined as a blood loss of more than 500 mL in a vaginal delivery or more than 1000 mL in a cesarean delivery. The most common cause of postpartum hemorrhage is uterine atony, which is the failure of the uterus to contract after delivery. Other causes include lacerations, retained placental fragments, coagulation disorders, and uterine rupture. Monitoring the vital signs, especially blood pressure, and pulse, can help detect signs of hypovolemia due to blood loss. Other signs include pale skin, cold and clammy extremities, delayed capillary refill, decreased urine output, and altered mental status.
Choice B is not correct because determining if the mother's milk is coming in is not the primary rationale for monitoring a new mother every 15 minutes for the first hour after delivery. Milk production usually begins around 48 to 72 hours after delivery and is influenced by hormonal changes, breastfeeding frequency, and maternal health. Although breastfeeding support is important for postpartum care, it is not a priority over checking for postpartum hemorrhage.
Choice C is not correct because monitoring the mother's blood pressure to note any elevations is not the primary rationale for monitoring a new mother every 15 minutes for the first hour after delivery. Elevated blood pressure can indicate gestational hypertension or preeclampsia, which are serious conditions that can affect postpartum women. However, these conditions are more likely to cause symptoms such as headache, blurred vision, epigastric pain, and proteinuria⁴.
Moreover, blood pressure may not be a sensitive indicator of blood loss and may remain normal until a significant amount of blood is lost¹.
Choice D is not correct because answering questions the new parents may have is not the primary rationale for monitoring a new mother every 15 minutes for the first hour after delivery. Although providing education and support to the new parents is an essential part of postpartum care, it is not a priority over checking for postpartum hemorrhage. The new parents may have questions about infant care, feeding, contraception, recovery, and other topics that can be addressed during the postpartum period.
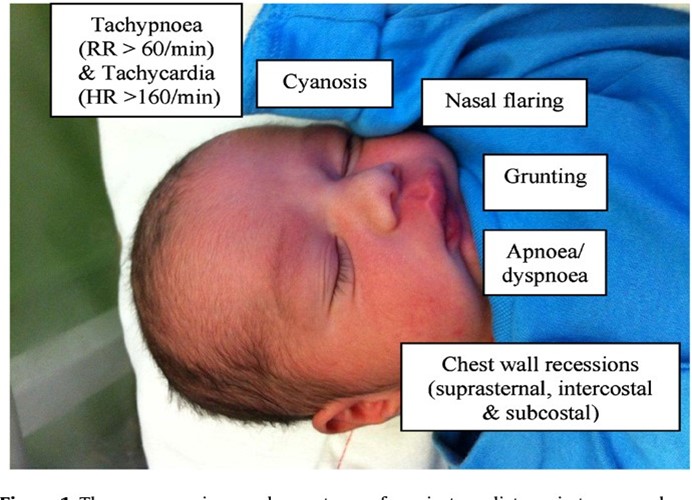
Shortly after delivery, a symptom of respiratory distress in the newborn that should be reported is:
Explanation
Sternal or chest retractions. This is because sternal or chest retractions are a sign of respiratory distress in newborns, which means they are having difficulty breathing. Chest retractions occur when the baby's chest pulls in with each breath, indicating that they are using extra muscles to breathe. This can be caused by various conditions that affect the lungs, such as respiratory distress syndrome (RDS), transient tachypnea of the newborn (TTN), meconium aspiration syndrome (MAS), pneumonia, or congenital heart defects.
 Choice A is not correct because mucus draining from the nose is not a symptom of respiratory distress in newborns. It is normal for newborns to have some mucus in their nose and mouth after birth, which can be cleared by suctioning or wiping.
Choice A is not correct because mucus draining from the nose is not a symptom of respiratory distress in newborns. It is normal for newborns to have some mucus in their nose and mouth after birth, which can be cleared by suctioning or wiping.
Mucus drainage does not interfere with breathing unless it is excessive or thick.
Choice B is not correct because cyanosis of the hands and feet is not a symptom of respiratory distress in newborns. It is normal for newborns to have bluish discoloration of their hands and feet, called acrocyanosis, for the first few days after birth. This is due to immature circulation and does not indicate a lack of oxygen. Cyanosis of the central parts of the body, such as the face, lips, and tongue, is more concerning and should be reported.
Choice C is not correct because irregular heart rate is not a symptom of respiratory distress in newborns. It is normal for newborns to have some variations in their heart rate, especially during sleep cycles. The normal heart rate range for newborns is 100 to 160 beats per minute. A heart rate that is too fast (tachycardia) or too slow (bradycardia) may indicate a problem with the heart or other organs³.
A nurse is collecting data from a newborn and notes a swollen area on the head that does not cross the suture line. The nurse should interpret this finding as which of the following?
Explanation
This is because cephalhematoma is a collection of blood under the scalp that does not cross the suture line. It is caused by trauma to the head during delivery, such as from vacuum extraction or forceps. It usually appears within a few hours or days after birth and resolves within weeks or months.


Choice B is not correct because nevus flammeus is a type of birthmark that is also known as port-wine stain. It is a flat, red, or purple patch of skin that can appear anywhere on the body, but often on the face. It is caused by abnormal blood vessels in the skin and does not go away over time³.
Choice C is not correct because the molding is the temporary change in the shape of the head due to pressure during delivery. It does not cause swelling or bruising and usually resolves within a few days.
Choice D is not correct because caput succedaneum is a type of swelling that affects the scalp and crosses the suture line. It is caused by fluid accumulation under the scalp due to pressure during delivery. It usually appears at birth and goes away within a few days.
A nurse is reviewing the medical record of a client who experienced a vaginal birth 2 hr ago. The nurse should identify which of the following findings places the client at risk for a postpartum hemorrhage.
Explanation
Precipitous birth
This is because precipitous birth, which is defined as a labor that lasts less than three hours from the onset of contractions to delivery, is a risk factor for postpartum hemorrhage. This is because the uterus may not contract well after a rapid delivery, leading to uterine atony and bleeding. Other risk factors for postpartum hemorrhage include uterine overdistension, oxytocin use, placental abruption, placenta previa, infection, coagulation disorders, and previous history of postpartum hemorrhage.
Choice A is not correct because gestational hypertension is not a risk factor for postpartum hemorrhage. It is a condition that causes high blood pressure during pregnancy and can lead to complications such as preeclampsia, eclampsia, and placental abruption³.
Choice B is not correct because small for gestational age newborn is not a risk factor for postpartum hemorrhage. It is a condition that indicates that the baby's growth was restricted in the womb and weighs less than 90% of other babies of the same gestational age. It can be caused by maternal factors, placental factors, or fetal factors⁴.
Choice C is not correct because a two-vessel umbilical cord is not a risk factor for postpartum hemorrhage. It is a condition that occurs when the umbilical cord has only one artery and one vein instead of the normal two arteries and one vein. It can be associated with congenital anomalies, intrauterine growth restriction, and stillbirth.
A nurse is assisting with the care of a newborn following a vaginal delivery. Which of the following actions should the nurse perform first?
Explanation
Clear the respiratory tract. This is because clearing the respiratory tract is the first step in the initial care of a newborn following vaginal delivery. The respiratory tract includes the nose, mouth, and lungs.
Clearing the respiratory tract helps the baby breathe more easily and prevents aspiration of amniotic fluid, blood, or mucus. The nurse can use a bulb syringe or a suction device to gently remove any fluid from the baby's nose and mouth.

Choice B is not correct because drying the infant off and covering the head is not the first action to take. Drying and covering the infant helps prevent heat loss and hypothermia, which are important for newborn care. However, this should be done after clearing the respiratory tract.
Choice C is not correct because stimulating the infant to cry is not the first action to take. Stimulating the infant to cry can help expand the lungs and improve oxygenation, which is also important for newborn care. However, this should be done after clearing the respiratory tract.
Choice D is not correct because clamping the umbilical cord is not the first action to take. Clamping and cutting the umbilical cord separates the baby from the placenta, which is no longer needed after birth. However, this should be done after clearing the respiratory tract.
A woman had a vaginal delivery two days ago and is preparing for discharge. To help prevent postpartum complications, the nurse plans to teach the woman to report any:
Explanation
Fever. This is because fever is a sign of infection, which is a common and potentially serious postpartum complication. Infection can affect various parts of the body, such as the uterus (endometritis), the bladder (cystitis), the breast (mastitis), the wound (wound infection), or the blood (sepsis). Infection can cause symptoms such as fever, chills, pain, foul-smelling discharge, redness, swelling, or warmth at the site of infection.
Choice A is not correct because the change in lochia from red to white is not a sign of postpartum complication. Lochia is the vaginal discharge that occurs after childbirth. It changes color and amount over time, from red to pink to brown to yellow to white. This is a normal process of healing and does not indicate a problem unless the lochia is foul-smelling, heavy, or contains large clots³.
Choice B is not correct because fatigue and irritability are not signs of postpartum complications. Fatigue and irritability are common feelings after childbirth due to hormonal changes, sleep deprivation, physical recovery, and emotional adjustment. They do not necessarily indicate a problem unless they are severe or persistent and interfere with daily functioning or bonding with the baby.
Choice D is not correct because contractions are not signs of postpartum complication. Contractions are normal after childbirth and help the uterus shrink back to its pre-pregnancy size. They are usually mild and subside within a few days. They may be more intense during breastfeeding due to the release of oxytocin, which stimulates uterine contractions.
Following delivery, the nurse's assessment reveals a soft, boggy uterus located above the level of the umbilicus. The appropriate intervention is:
Explanation
Massage the fundus. This is because massaging the fundus (the upper part of the uterus) can help the uterus contract and prevent excessive bleeding after delivery. A soft, boggy uterus indicates uterine atony, which is a failure of the uterus to contract sufficiently after childbirth.
Uterine atony is the most common cause of postpartum hemorrhage, which can be life-threatening if not treated promptly¹².
Choice B is not correct because initiating measures that encourage voiding is not the appropriate intervention for a soft, boggy uterus. A full bladder can interfere with uterine contractions and cause bleeding, so it is important to empty the bladder after delivery. However, this should be done after massaging the fundus.
Choice C is not correct because positioning the patient flat is not the appropriate intervention for a soft, boggy uterus. Positioning the patient flat can increase blood loss and reduce venous return. The patient should be positioned with the head slightly elevated and the legs flexed to improve blood circulation and prevent shock³.
Choice D is not correct because notifying the doctor is not the first intervention for a soft, boggy uterus. Notifying the doctor is important if bleeding persists or worsens despite massaging the fundus. The doctor may order medications or other treatments to stop the bleeding and prevent complications¹.
A nurse is collecting data from a client who delivered 2 hours ago. The client has moderate lochia rubra, temperature within normal limits, breasts soft, fundus firm, slightly deviated to the right, pulse rate 88/min, respiratory rate 18/min.
Which of the following actions should the nurse perform?
Explanation
ask the client to empty her bladder. A full bladder can cause the uterus to be displaced and lead to excessive bleeding. The moderate lochia rubra, normal temperature, soft breasts, firm fundus, slightly deviated to the right, pulse rate of 88/min, and respiratory rate of 18/min are all normal findings.
Choice A is not correct because the client's milk will come in regardless of nursing frequency.
Choice B is not correct because the client's temperature is within normal limits.
Choice D is not correct because there is no indication of an increase in IV fluids.
To protect newborns from infection while in the nursery, the nurse plans to:
Explanation
Wash hands before touching each baby. This is because hand hygiene is the most effective way to prevent infection transmission in the nursery. Hand hygiene should be performed before and after every patient contact, as well as before and after wearing gloves or handling equipment. Hand hygiene can be done by washing hands with soap and water or using alcohol-based hand rubs.
Choice A is not correct because adjusting room temperature between 75°F and 80°F is not a measure to protect newborns from infection. The room temperature should be maintained within a comfortable range for newborns, but it does not affect infection risk.
Choice B is not correct because wearing a disposable gown when giving infant care is not a measure to protect newborns from infection. Disposable gowns are part of contact precautions, which are used for patients with known or suspected infections that can be transmitted by direct or indirect contact. They are not necessary for routine infant care.
Choice C is not correct because keeping the newborn dressed warmly is not a measure to protect newborns from infection. Keeping the newborn dressed warmly can help prevent heat loss and hypothermia, but it does not affect infection risk.
When a newborn takes its first breath, what physical changes occur in the heart to increase oxygenation of the body?
Explanation
The foramen ovale closes, preventing blood exchange from right to left in the heart. This is because the foramen ovale is a fetal shunt that allows blood to bypass the lungs and flow from the right atrium to the left atrium. After birth, when the baby starts to breathe air, the lungs expand and the pulmonary resistance decreases. This causes an increase in blood flow and pressure in the left atrium, which pushes the foramen ovale closed. This prevents blood from mixing between the right and left sides of the heart and allows oxygenated blood to circulate to the body¹².
Choice A is not correct because the ductus arteriosus does not expand to allow more blood to enter the lungs. The ductus arteriosus is another fetal shunt that
connects the pulmonary artery to the aorta. It allows blood to bypass the lungs and flow from the right ventricle to the aorta. After birth, when the baby starts to breathe air, the oxygen concentration in the blood increases and causes the ductus arteriosus to constrict and close. This increases blood flow to the lungs and decreases blood flow to the aorta.
Choice C is not correct because the umbilical vein that carried oxygenated blood in utero does not become the ascending aorta entering the right atrium. The umbilical vein is a fetal vessel that carries oxygenated blood from the placenta to the fetus. It connects to either the portal vein or the ductus venosus, which then drains into the inferior vena cava. After birth, when the umbilical cord is clamped and cut, the umbilical vein collapses and becomes a fibrous cord called ligamentum teres hepatis.
Choice D is not correct because the ductus venosus does not shunt oxygenated aortic blood to the lungs. The ductus venosus is another fetal vessel that connects the umbilical vein to the inferior vena cava. It allows some of the oxygenated blood from the placenta to bypass the liver and enter directly into the systemic circulation. After birth, when the umbilical cord is clamped and cut, the ductus venosus closes and becomes a fibrous cord called ligamentum venosum.
A new mother of a newborn girl calls the clinic in a panic, concerned about the blood-tinged soiled diaper. What is the best response from the nurse?
Explanation
This can be from the sudden withdrawal of your hormones. It's not a cause for alarm. This is because newborn female babies may have a little bloody vaginal discharge in their diaper due to the withdrawal of maternal hormones after delivery. This usually stops as the hormones return to normal levels¹².
Choice B is wrong because the baby does not need an appointment for this condition.
Choice C is wrong because the mother does not need to watch her baby for this condition.
Choice D is wrong because the blood is not related to cleaning her perineal area.
A nurse is caring for a newborn shortly after birth and places the newborn under a radiant warmer. Which of the following potential complications does this action help to prevent?
Explanation
This action helps to prevent cold stress. This is because cold stress is a condition where the newborn's core temperature drops below 36.5°C and they use energy and oxygen to generate warmth. This can lead to hypoglycemia, metabolic acidosis, hypoxia, and an increased risk of infection.
Placing the newborn under a radiant warmer provides thermal stability and prevents heat loss by radiation.
Choice B is wrong because thermogenesis is the process of heat production, not a complication.
Choice C is wrong because shivering is a mechanism of heat production in adults, not in newborns.
Choice D is wrong because brown fat production is a normal feature of newborns that helps them generate heat by lipolysis.
Here is an image of a newborn under a radiant warmer.

When planning the care for a client during the first 24 hours postpartum, the nurse expects to monitor the client's pulse and blood pressure frequently based on the understanding that the client is at risk for which condition?
Explanation
Hemorrhage. This is because postpartum hemorrhage (PPH) is severe bleeding and loss of blood after childbirth that can lead to death. The most common cause of PPH is the uterus not contracting properly after delivery. The nurse needs to monitor the client’s pulse and blood pressure frequently to detect signs of shock and blood loss.
Choice A is wrong because thromboembolism is a blood clot that blocks a blood vessel, not a complication of bleeding.
Choice B is wrong because cervical laceration is a tear in the cervix that can cause bleeding, but it is not a common cause of PPH.
Choice C is wrong because hemorrhoids are swollen veins in the anus or rectum that can cause bleeding, but they are not a common cause of PPH.

A nurse is collecting data from a client who is 12 hr postpartum. Which of the following findings should the nurse expect?
Explanation
Fundus firm, at the level of the umbilicus. This is because the normal postpartum uterine fundus location should be around the belly button (umbilicus) one hour after delivery and then decrease by 1 cm per 24 hours. A firm fundus indicates that the uterus is contracting well and preventing bleeding.

Choice A is wrong because a soft fundus indicates uterine atony, which is a risk factor for hemorrhage.
Choice C is wrong because the fundus should not be above the umbilicus 12 hours after delivery.
Choice D is wrong because a fundus to the right of the umbilicus indicates a full bladder, which can displace the uterus and cause bleeding.
During a postpartum assessment, a woman reports that her right calf is painful. The nurse observes edema and redness along the saphenous vein in the right lower leg. Based on this finding, the nurse explains that the probable treatment will involve:
Explanation
Anticoagulants for 6 weeks. This is because the client’s symptoms suggest that she has deep vein thrombosis (DVT), which is a blood clot in a deep vein of the leg. DVT is a serious condition that can lead to pulmonary embolism, which is a blockage of a blood vessel in the lungs. The treatment for DVT involves anticoagulants, which are drugs that prevent blood clots from growing or forming new ones. The duration of anticoagulant therapy depends on the risk factors and severity of DVT, but it is usually at least 6 weeks.
Choice A is wrong because gentle massage of the affected leg can dislodge the clot and cause a pulmonary embolism.
Choice C is wrong because passive leg exercises can increase blood flow and worsen pain and swelling.
Choice D is wrong because the application of ice to the affected leg can reduce inflammation but does not treat the underlying clot.
The 1-day postpartum patient shows a temperature elevation, cough, and slight shortness of breath on exertion. Based on these symptoms, the nurse should:
Explanation
Notify the physician of a possible pulmonary embolism. This is because the client's symptoms suggest that she has a pulmonary embolism, which is a blockage of a blood vessel in the lungs often caused by blood clots that travel from the legs. Pulmonary embolism is a life-threateningcondition that requires immediate medical attention. The client may also have chest pain, coughing up blood, dizziness, or fainting.

Choice A is wrong because postpartum mucous membrane congestion does not cause fever, cough, or shortness of breath.
Choice B is wrong because an upper respiratory infection does not cause edema and redness along the saphenous vein.
Choice D is wrong because an antipyretic remedy does not treat the underlying cause of the fever and may mask the severity of the condition.
Five days after a spontaneous vaginal delivery, a woman comes to the emergency room because she has a fever and persistent cramping. The nurse recognizes that the cause of these signs and symptoms may be:
Explanation
Endometritis. This is because the client's symptoms suggest that she has endometritis, which is an infection of the lining of the uterus. Endometritis is a common postpartum complication that can occur after vaginal or cesarean delivery. The client may also have foul-smelling vaginal discharge, chills, and fatigue.
Choice B is wrong because cystitis is an infection of the bladder that causes pain or burning during urination, not cramping.
Choice C is wrong because dehydration does not cause fever or persistent cramping.
Choice D is wrong because hypovolemic shock is a condition of low blood volume that causes low blood pressure, rapid pulse, and pale skin, not fever or cramping.
A nurse is updating the plan of care for a newborn who is undergoing phototherapy. Which of the following actions should the nurse include in the plan?
Explanation
Encourage the newborn to breastfeed every 2 hr. This is because breastfeeding helps the newborn to excrete bilirubin through stool and urine. Breastfeeding also prevents dehydration, which can worsen jaundice. The nurse should also monitor the newborn’s weight, hydration status, and bilirubin levels during phototherapy.
Choice A is wrong because monitoring the newborn’s blood glucose level hourly is not necessary for phototherapy.
Choice B is wrong because applying lotion to the newborn’s skin twice per day can interfere with the effectiveness of phototherapy and increase the risk of skin irritation.
Choice D is wrong because maintaining the newborn in a prone position can increase the risk of sudden infant death syndrome (SIDS) and limit the exposure of skin to light.
To prevent possible retinopathy in a preterm infant requiring oxygen therapy, the nurse will:
Explanation
Administer low concentrations of oxygen. Retinopathy of prematurity (ROP) is a disease of retinal vascular and capillary proliferation affecting premature infants undergoing oxygen therapy. Oxygen treatment results in pathologic growth of vessels in the developing retina that may lead to permanent damage to the retina as well as retinal detachment and macular folds. Administering low concentrations of oxygen can help prevent ROP by reducing the oxygen-induced vasoconstriction and vascular endothelial growth factor (VEGF) expression.
Choice A is not correct because keeping the infant's eyes covered at all times does not prevent ROP. In fact, it may increase the risk of infection or injury to the eyes.
Choice B is not correct because positioning with the head slightly lower than the body does not prevent ROP. It may increase the intracranial pressure and affect the cerebral blood flow.
Choice D is not correct because monitoring arterial oxygen levels with a pulse oximeter does not prevent ROP. It is a useful tool to guide oxygen therapy, but it does not directly affect retinal vascular development.
Which finding would alert the nurse to suspect that a newborn is experiencing respiratory distress?
Explanation
Asymmetrical chest movement is a sign of respiratory distress in the newborn, as it indicates unequal lung expansion or airway obstruction. A respiratory rate of 50 breaths/minute (choice B) is normal for a newborn, as is acrocyanosis (choice C), which is a bluish discoloration of the hands and feet due to immature peripheral circulation. Short periods of apnea (less than 15 seconds) (choice D) are also common and benign in newborns unless they are associated with bradycardia or cyanosis.
Choice B is not correct because a respiratory rate of 50 breaths/minute is within the normal range for a newborn.
Choice C is not correct because acrocyanosis is a normal finding in newborns and does not indicate respiratory distress.
Choice D is not correct because short periods of apnea (less than 15 seconds) are normal in newborns and do not indicate respiratory distress.
The nurse is caring for a new mother and newborn in a rooming-in unit and watches the mother put the infant in the bed, lying on her side, propped up with a pillow. The nurse should point out that this position can increase the risk of which situation?
Explanation
Sudden infant death syndrome (SIDS) is the sudden and unexplained death of an infant under one year of age. SIDS is more likely to occur when infants sleep on their stomachs or sides, or when they are propped up with pillows or other soft bedding. These positions can interfere with the infant's breathing and increase the risk of suffocation or overheating .
Choice A is incorrect because gastroesophageal reflux (GER) is a common condition in infants that causes them to spit up frequently after feeding. GER does not increase the risk of SIDS and can be managed by feeding smaller amounts, burping the infant often, and keeping them upright for a while after feeding.
Choice C is incorrect because apnea episodes are brief pauses in breathing that occur normally in infants, especially during sleep. Apnea episodes do not increase the risk of SIDS and usually resolve by six months of age.
Choice D is incorrect because sleeping for short intervals is normal for newborns, who need to feed frequently during the day and night. Sleeping for short intervals does not increase the risk of SIDS and will gradually change as the infant grows older.
Within three days of birth, a newborn has developed a yellowish tinge that extends from the face to mid-chest is lethargic, and has to be awakened to feed. Which condition does the nurse suspect this infant is manifesting?
Explanation
Pathologic jaundice. This type of jaundice occurs within the first 24 hours of birth and is caused by an underlying health condition, such as blood type incompatibility, infection, or liver problems. It can lead to serious complications, such as brain damage, if not treated promptly. Pathologic jaundice requires medical attention and often involves phototherapy or blood transfusion to lower the bilirubin levels in the baby's blood.
Choice A is not correct because physiologic jaundice is a normal and harmless condition that affects most newborns. It usually appears between the second and fourth day after birth and resolves by the second week. It is caused by the immature liver's inability to process bilirubin efficiently.
Choice C is not correct because breast milk jaundice is a rare condition that affects some breastfed babies. It usually appears after the first week of life and lasts up to a month or longer. It is caused by a substance in breast milk that interferes with the liver's ability to eliminate bilirubin.
Sign Up or Login to view all the 41 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

