RN ADULT MEDICAL SURGICAL 2019 WITH NGN Updated 2024
Total Questions : 66
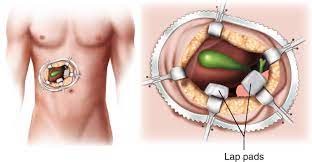
Showing 25 questions, Sign in for moreA nurse is planning care for a client who is 1 day postoperative following an open cholecystectomy. Which of the following interventions should the nurse include in the plan of care?
Explanation
Choice Areason:
Placing pillows under the client's knees might be useful for comfort, but it doesn't directly address the risk of DVT.
Choice Breason:
Discouraging leg exercises while in bed is not recommended because it can lead to decreased circulation and an increased risk of blood clot formation.
Choice C reason:
Applying compression stockings to the lower extremities is recommendable. After an open cholecystectomy surgery, the client is at risk for developing deep vein thrombosis (DVT) due to reduced mobility and surgical trauma. Applying compression stockings to the lower extremities can help improve blood circulation and reduce the risk of blood clot formation.
Choice D reason:
Avoiding the use of anticoagulants is not recommendable, if prescribed by the healthcare provider, could be detrimental in preventing postoperative complications like DVT. Anticoagulants are often used to prevent clot formation in high-risk surgical patients.
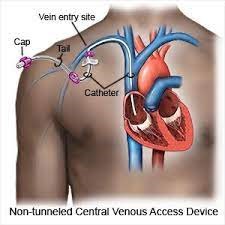
A nurse is preparing to assist with the insertion of a non-tunneled central venous catheter for a client who is malnourished. Which of the following actions should the nurse plan to take?
Explanation
Choice A reason:
Confirming the correct position of the line by obtaining a blood sample is appropriate. Inserting a central venous catheter is a procedure that involves placing a catheter into a large vein, typically in the neck, chest, or groin. Confirming the correct placement is crucial to prevent complications such as pneumothorax (lung collapse) or catheter misplacement.
Choice B reason:
Instructing the client to cough as the catheter is inserted is not a standard practice during central venous catheter insertion and could lead to unnecessary complications.
Choice C reason:
Placing the head of the client's bed lower than the foot (Trendelenburg position) is not a standard practice during central venous catheter insertion and would not be helpful for this procedure.
Choice D reason:
Cleansing the site with hydrogen peroxide is not the recommended method for central venous catheter insertion. Typically, a sterile technique and appropriate antiseptic solution are used to reduce the risk of infection.
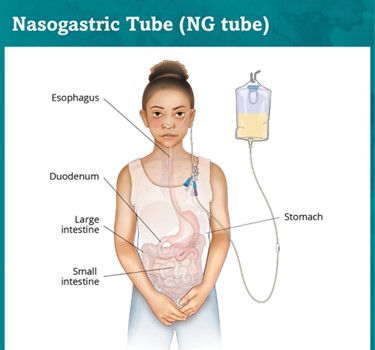
A PACU nurse is monitoring the drainage from a client's NG tube following abdominal surgery. Which of the following findings in the first postoperative hour should the nurse report to the provider?
Explanation
Choice A reason:
75 mL of greenish-yellow drainage should not be reported. This could be stomach contents or bile, which can be expected after surgery and might not be alarming.
Choice B reason:
150 mL of serosanguineous drainage should not be reported. Serosanguineous drainage is a mix of clear and slightly bloody fluid, which can be expected after surgery and may not be alarming.
Choice C reason:
100 mL of red drainage should be reported. After abdominal surgery, the drainage from an NG (nasogastric) tube is monitored to assess the client's condition and the status of their gastrointestinal system. Red drainage could indicate bleeding, which is a significant concern after surgery. The nurse should report this finding to the provider for further evaluation and intervention.
Choice D reason:
200 mL of brown drainage should not be reported. Brown drainage could also be indicative of old blood or digestive fluids, which might be expected after surgery and may not be alarming.
A nurse is caring for a client who arrives at the emergency department and reports vomiting and diarrhea for the past 3 days. The client's serum potassium level is 2.8 mEq/L. Which of the following interventions should the nurse implement first?
Explanation
Choice A reason:
Listening to the client's bowel sounds should not be implemented. It is important for assessing the gastrointestinal status, but the priority in this situation is to address the potential cardiac complications of hypokalaemia.
Choice B reason:
Initiating cardiac monitoring for the client should be implemented. A serum potassium level of 2.8 mEq/L is significantly low (normal range is typically around 3.5-5.0 mEq/L). Low potassium levels, known as hypokalaemia, can lead to serious cardiac arrhythmias and other complications. Therefore, the nurse should prioritize cardiac monitoring to assess for any potential changes or abnormalities in the client's heart rhythm due to the low potassium levels.
Choice C reason:
Checking the client's hand grasps should not be implemented. It is a test for muscle strength and can be indicative of hypokalaemia, but initiating cardiac monitoring is more critical at this point.
Choice D reason:
Administering an IV potassium drip may be necessary, but initiating cardiac monitoring takes precedence as the first action to ensure the client's heart rhythm is stable before addressing the potassium imbalance.
A nurse is providing discharge teaching to a client following a modified left radical mastectomy with a breast expander. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason:
"will keep my left arm flexed at the elbow as much as possible": This statement is incorrect because after a mastectomy, it's important to promote full range of motion in the affected arm to prevent complications like contractures and lymphedema.
Choice B reason:
“will have to wait 2 months before additional saline can be added to my breast expander" This is the correct statement. Following a modified radical mastectomy with a breast expander, additional saline is often added gradually to the expander to stretch the skin and muscle for reconstruction. The waiting period between saline additions allows for healing and proper tissue expansion. This statement indicates that the client understands the postoperative care and timeline.
Choice C reason:
"should expect less than 25 ml of secretions per day in the drainage devices": This statement is not accurate because the drainage amount can vary, and 25 ml per day might not be an accurate estimate.
Choice D reason:
"will perform strength-building arm exercises using a 15-pound weight": This statement is not appropriate, especially shortly after surgery. Gradual and gentle strength-building exercises are recommended, and using a 15-pound weight could be too strenuous and potentially harmful.
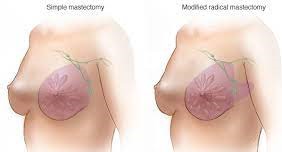
A nurse is providing discharge teaching to a client following a modified left mastectomy. Which statements by the client indicate an understanding of the teaching?
Explanation
Choice A reason:
"will keep my left arm flexed at the elbow as much as possible": This statement is incorrect because after a mastectomy, it's important to promote full range of motion in the affected arm to prevent complications like contractures and lymphedema.
Choice B reason:
“will have to wait 2 months before additional saline can be added to my breast expander" This is the correct statement. Following a modified radical mastectomy with a breast expander, additional saline is often added gradually to the expander to stretch the skin and muscle for reconstruction. The waiting period between saline additions allows for healing and proper tissue expansion. This statement indicates that the client understands the postoperative care and timeline.
Choice C reason:
"should expect less than 25 ml of secretions per day in the drainage devices": This statement is not accurate because the drainage amount can vary, and 25 ml per day might not be an accurate estimate.
Choice D reason:
"will perform strength-building arm exercises using a 15-pound weight": This statement is not appropriate, especially shortly after surgery. Gradual and gentle strength-building exercises are recommended, and using a 15-pound weight could be too strenuous and potentially harmful.
A nurse is caring for a client in diabetic ketoacidosis (DKA). Which of the following is the priority intervention by the nurse?
Explanation
Choice A reason:
Initiating a continuous IV insulin infusion is the first priority. The priority intervention for a client in diabetic ketoacidosis (DKA) is to normalize blood glucose levels and reverse the ketoacidosis. Initiating a continuous IV insulin infusion is essential to rapidly lower the elevated blood glucose levels and counteract the metabolic acidosis associated with DKA.
Choice B reason:
Beginning a bicarbonate continuous IV infusion is generally not the priority in DKA management. While metabolic acidosis is a concern in DKA, insulin therapy and fluid resuscitation are typically the initial focus of treatment.
Choice C reason:
Checking potassium levels is important since potassium imbalances are common in DKA. However, while this is important, it is not the first priority. It's important to ensure that insulin therapy has been initiated before addressing potassium levels.
Choice D reason:
Administering 0.9% sodium chloride (normal saline) is a crucial part of DKA treatment but it is not the first priority as it helps correct dehydration and electrolyte imbalances. However, starting insulin therapy to address the underlying metabolic issue takes precedence.
A nurse is caring for a client in diabetic ketoacidosis (DKA). Which of the following is the priority intervention by the nurse?
Explanation
Choice A reason:
Initiating a continuous IV insulin infusion is the first priority. The priority intervention for a client in diabetic ketoacidosis (DKA) is to normalize blood glucose levels and reverse the ketoacidosis. Initiating a continuous IV insulin infusion is essential to rapidly lower the elevated blood glucose levels and counteract the metabolic acidosis associated with DKA.
Choice B reason:
Beginning a bicarbonate continuous IV infusion is generally not the priority in DKA management. While metabolic acidosis is a concern in DKA, insulin therapy and fluid resuscitation are typically the initial focus of treatment.
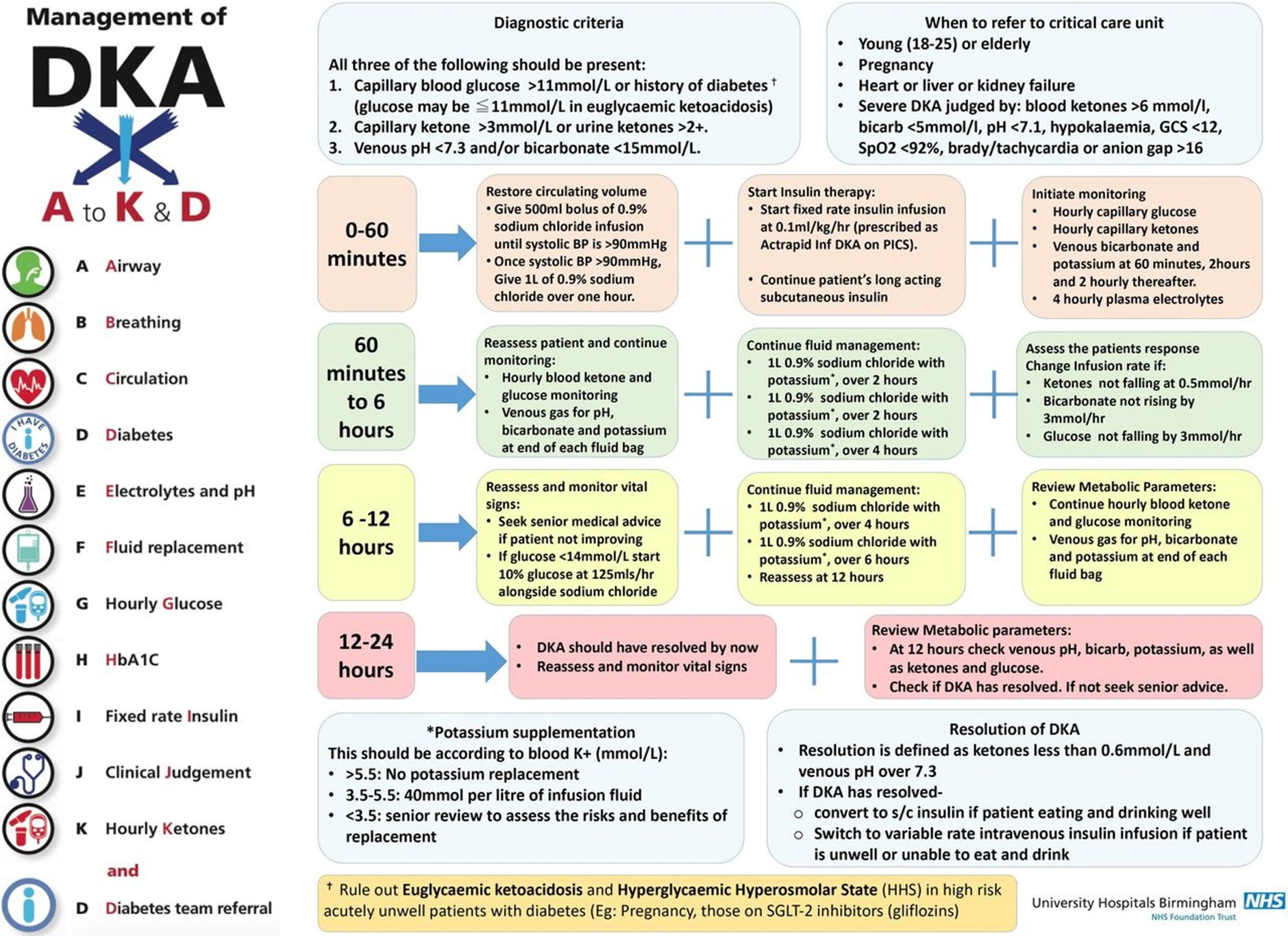
Choice C reason:
Checking potassium levels is important since potassium imbalances are common in DKA. However, while this is important, it is not the first priority. It's important to ensure that insulin therapy has been initiated before addressing potassium levels.
Choice D reason:
Administering 0.9% sodium chloride (normal saline) is a crucial part of DKA treatment but it is not the first priority as it helps correct dehydration and electrolyte imbalances. However, starting insulin therapy to address the underlying metabolic issue takes precedence.
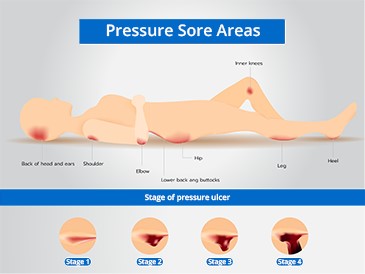
A nurse is assessing a client who has a pressure ulcer. Which of the following findings should the nurse expect as an indication the wound is healing?
Explanation
Choice A reason:
Wound tissue firm to palpation is a false expectation. While firmness can be an indicator of healing in some wounds, it's not a reliable indicator on its own. The appearance and characteristics of the tissue, including granulation tissue, are more significant indicators of healing.
Choice B reason:
Dry brown eschar is a false expectation. Brown eschar is often necrotic tissue that needs to be removed for the wound to heal. Its presence typically suggests a lack of healing progress.
Choice C reason:
Dark red granulation tissue is the correct expectation because it is a sign of healing in a pressure ulcer. Granulation tissue is the new tissue that forms during the healing process, and the dark red color indicates that the tissue is well-vascularized and receiving adequate blood supply, which is essential for healing.
Choice D reason:
Light yellow exudate is a false expectation. Light yellow exudate is often indicative of infection or non-healing wounds. While some exudate is normal in the healing process, its color alone doesn't necessarily indicate healing.
A nurse is assessing a client who has a pressure ulcer. Which of the following findings should the nurse expect as an indication the wound is healing?
Explanation
Choice A reason:
Wound tissue firm to palpation is a false expectation. While firmness can be an indicator of healing in some wounds, it's not a reliable indicator on its own. The appearance and characteristics of the tissue, including granulation tissue, are more significant indicators of healing.
Choice B reason:
Dry brown eschar is a false expectation. Brown eschar is often necrotic tissue that needs to be removed for the wound to heal. Its presence typically suggests a lack of healing progress.
Choice C reason:
Dark red granulation tissue is the correct expectation because it is a sign of healing in a pressure ulcer. Granulation tissue is the new tissue that forms during the healing process, and the dark red color indicates that the tissue is well-vascularized and receiving adequate blood supply, which is essential for healing.
Dark red granulation tissue is a positive sign of wound healing. It indicates that new blood vessels are forming and that the wound is progressing toward the later stages of healing. Granulation tissue is crucial for wound repair and serves as the foundation for new tissue growth.
Choice D reason:
Light yellow exudate is a false expectation. Light yellow exudate is often indicative of infection or non-healing wounds. While some exudate is normal in the healing process, its colour alone doesn't necessarily indicate healing.
A nurse is providing instructions about foot care for a client who has peripheral arterial disease. The nurse should identify that which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A reason:
"use my heating pad on a low setting to keep my feet warm". This statement is incorrect. Using a heating pad, especially on a low setting, is not recommended for individuals with PAD. It can lead to burns or skin damage due to reduced sensation in the feet.
Choice B reason:
"rest in my recliner with my feet elevated for about an hour every afternoon" This statement is incorrect. While elevating the feet can help with blood circulation, it's important to avoid prolonged periods of inactivity. Regular physical activity is important for improving circulation.
Choice C reason:
"soak my feet in hot water before trimming my toenails". This statement is incorrect. Soaking feet in hot water can cause burns or damage to the skin for individuals with reduced sensation due to PAD. Trimming toenails should be done carefully and without soaking to prevent injury and infection.
Choice D reason:
"apply a lubricating lotion to the cracked areas on the soles of my feet every morning “This statement is correct. Clients with peripheral arterial disease (PAD) are at risk of reduced blood circulation to the extremities, including the feet. Proper foot care is crucial to prevent complications such as non-healing wounds or infections. Applying a lubricating lotion to cracked areas can help keep the skin moisturized and prevent further complications.

A nurse is caring for a client who arrives at the emergency department and reports vomiting and diarrhea for the past 3 days. The client's serum potassium level is 2.8 mEq/L. Which of the following interventions should the nurse implement first?
Explanation
Choice A reason:
Listening to the client's bowel sounds should not be implemented. While assessing bowel sounds is important, it is not the highest priority in this situation. The client's low serum potassium level indicates the potential for serious cardiac arrhythmias, so actions related to monitoring and addressing this electrolyte imbalance are more critical.
Choice B reason:
Initiate cardiac monitoring for the client is the correct answer. A serum potassium level of 2.8 mEq/L is significantly low and can lead to life-threatening cardiac arrhythmias. Initiating cardiac monitoring is crucial to assess the client's heart rhythm and ensure that any potential abnormalities are identified promptly.
Choice C reason:
Check the client's hand grasps should not be implemented. Assessing the client's hand grasps can provide information about muscle strength, but it is not the immediate priority when the client has a critically low potassium level.
Choice D reason:
Administer an IV potassium drip should not be implemented. Administering IV potassium is important for correcting the potassium imbalance, but the priority is to assess and monitor the client's cardiac status first. Rapid administration of potassium can lead to cardiac arrhythmias, so it's important to ensure the heart's stability through cardiac monitoring before administering potassium.
A nurse is caring for a client who is experiencing an acute asthma attack. Which of the following should the nurse identify as a contributing factor to the client's manifestations?
Explanation
Choice A reason:
Inability to exhale retained carbon dioxide is incorrect. This is not the primary contributing factor to an acute asthma attack. Asthma attacks are primarily characterized by airway inflammation and bronchoconstriction, leading to difficulties in inhaling and exhaling.
Choice B reason:
Acute loss of alveolar elasticity is correct. During an acute asthma attack, bronchoconstriction occurs, leading to a narrowing of the airways. This narrowing results in increased resistance to airflow, difficulty exhaling, and decreased alveolar elasticity. The smooth muscles surrounding the bronchioles contract, contributing to the narrowing of the airways and leading to the characteristic symptoms of wheezing, shortness of breath, and difficulty breathing.
Choice C reason:
Decreased responsiveness of airways to allergens is incorrect. In asthma, the airways can become hypersensitive to allergens, which leads to increased responsiveness rather than decreased responsiveness.
Choice D reason:
Suppressed bronchiolar inflammatory response is incorrect. In asthma, the airways experience an exaggerated inflammatory response, leading to swelling, mucus production, and bronchoconstriction. This response is not suppressed but rather overactive during an asthma attack.
A nurse is reviewing the medical record of a client who is 1-day post- operative following an appendectomy. Which of the following findings should the nurse report to the provider?
Explanation
Choice A reason:
WBC count 8,400/mm3 is not appropriate. This white blood cell count is within the normal range and is not a cause for concern.
Choice B reason:
Serosanguineous exudate noted on dressing change is not appropriate. Serosanguineous drainage is a normal finding in the early stages of wound healing and is expected after surgery.
Choice C reason:
Reports pain of 4 on a scale from 0 to 10 when coughing is not appropriate. A pain level of 4 out of 10 with coughing is a common and expected finding following an appendectomy. It's important for the nurse to assess and manage pain, but this is not an urgent concern.
Choice D reason:
Haemoglobin 10 mg/dL is appropriate. Haemoglobin level of 10 mg/dL indicates a low level of haemoglobin, which might suggest anaemia or blood loss. Reporting this finding to the provider is important as it could indicate a need for further evaluation or intervention.

A nurse is caring for a client who has been receiving total parenteral nutrition (TPN) for 1 week. For which of the following findings should the nurse notify the provider?
Explanation
Choice A reason:
Calcium level 11.5 mg/dL is not appropriate. While the calcium level is above the normal range (8.5-10.5 mg/dL), it is not significantly elevated. The nurse should monitor this level and notify the provider if there is a trend of increasing levels.
Choice B reason
Serum albumin level 3.9 g/dL is not appropriate. This level is within a reasonable range for serum albumin. It might be an indicator of nutritional status, but it's not an urgent concern.
Choice C reason:
Output 200 ml, more than intake over the past 12 hr is appropriate. In a client receiving total parenteral nutrition (TPN), it's important to maintain fluid balance and avoid excessive fluid losses. An output significantly exceeding intake can indicate potential issues with fluid and electrolyte balance or the TPN administration. The nurse should notify the provider about this finding for further assessment and intervention.
Choice D reason:
Fasting blood glucose level 105 mg/dL is not appropriate: A fasting blood glucose level of 105 mg/dL is slightly elevated, but it's not a critically high value. The nurse should monitor blood glucose levels and collaborate with the healthcare team to manage blood glucose appropriately.
A nurse is preparing to discharge a client who has a halo device and is reviewing new prescriptions from the provider. The nurse should clarify which of the following prescriptions with the provider?
Explanation
Choice A reason:
May operate a motor vehicle when no longer taking analgesics is appropriate. This option could still potentially be a concern. While the patient might not be taking analgesics, the halo device's restrictions on neck movement could still impact their ability to safely operate a motor vehicle. So, this option might still need clarification with the provider.
Choice B reason:
Increase Intake of fibre-rich foods. This option is not related to the use of a halo device. Increasing fibber intake is generally a positive dietary recommendation, and it doesn't directly pertain to the halo device or the patient's discharge instructions.
Choice C reason:
May place a small pillow under the head when sleeping. This option is incorrect because using a small pillow under the head when sleeping is a common practice for patients with halo devices. It helps to maintain proper alignment and reduce discomfort while sleeping.
Choice D reason:
Take tub baths instead of showers. This option is incorrect because taking tub baths instead of showers is a common recommendation for patients with halo devices. The halo device must be kept dry to prevent complications. Showering might increase the risk of water seeping into the halo vest, whereas taking a tub bath could help in maintaining dryness around the device.
A nurse is caring for a client who is 6 hr. postoperative following application of an external fixator for a tibial fracture. Which of the following actions should the nurse take?
Explanation
Choice A reason:
Palpating the dorsalis pedis pulse is the appropriate option. Checking the dorsalis pedis pulse is crucial to assess the perfusion and circulation to the affected extremity. This is an important nursing action to monitor the patient's vascular status and ensure that there is adequate blood flow to the extremity distal to the fixator. A decrease or absence of the dorsalis pedis pulse could indicate potential circulation issues and require immediate attention.
Choice B reason:
Adjusting the clamps on the fixator frame is incorrect. The nurse should not adjust the clamps without specific orders from the healthcare provider. The external fixator is typically secured according to the surgeon's specifications, and any adjustments should be made under the guidance of the surgical team.
Choice C reason:
Wrapping sterile gauze on the sharp point of the pins is incorrect. The sharp pins used in an external fixator are an integral part of the device and are placed to stabilize the fracture. They should not be covered with sterile gauze, as this could interfere with their function and increase the risk of infection.
Choice D reason:
Maintaining the affected extremity in a dependent position is incorrect. Keeping the affected extremity in a dependent position (lower than the heart) can increase swelling and impair circulation. After surgery and fixation, it's often recommended to elevate the extremity to reduce swelling and promote proper circulation.

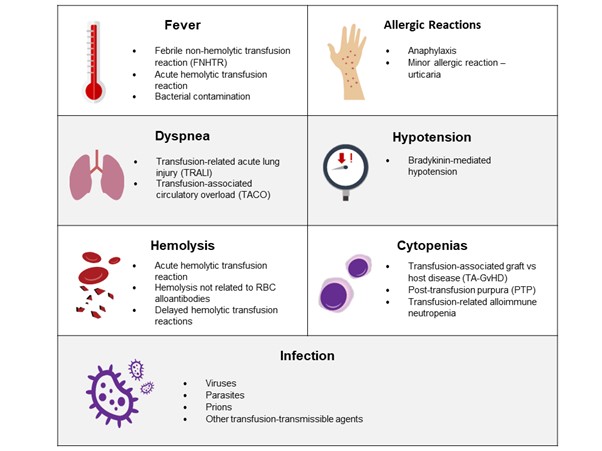
A nurse is administering packed RBCs to a client. The client reports chills, lower back pain, and nausea 10 min after the infusion begins. Which of the following actions should the nurse take first?
Explanation
Choice A reason:
Checking the client's vital signs is not appropriate. Checking vital signs is important to assess the severity of the reaction and monitor the client's overall condition.
Choice B reason:
Stopping the infusion is appropriate. Stopping the infusion is crucial to prevent further administration of the blood product that might be causing the adverse reaction. Once the infusion is stopped, the nurse can assess the client's condition more thoroughly and determine the appropriate steps to take next.
Choice C reason:
Collecting a urine sample is not appropriate. While urine sample collection may be important to assess for hemolysis (breakdown of red blood cells), it's not the first action to take. Stopping the infusion and assessing the client's vital signs are more immediate priorities.
Choice D reason:
Administering oxygen to the client is not appropriate. Providing oxygen might be necessary if the client is experiencing respiratory distress, but it's not the first action to take. Stopping the infusion and assessing the situation before providing additional interventions.
A nurse is caring for a client following a below-the-knee amputation. The client states. "My life is over." Which of the following responses should the nurse make?
Explanation
Choice A reason:
"You are upset. We can talk about this later." This response acknowledges the client's feelings, but it doesn't actively engage in addressing the client's concerns. It might also give the impression that the nurse is avoiding the conversation.
Choice B reason:
"Why do you think your life is over?" This response shows empathy and encourages the client to share their thoughts and feelings. It provides an opening for a meaningful conversation and allows the nurse to better understand the client's perspective. This approach demonstrates active listening and a willingness to support the client emotionally.
Choice C reason:
"Would you like to meet with another client who is an amputee?" While connecting the client with another amputee might offer valuable perspective and support, it's important to address the client's immediate concerns and emotions first. This response doesn't directly address the client's statement about feeling that their life is over.
Choice D reason:
"Most people can adjust following this surgery."
While this response provides a general statement of reassurance, it may not fully acknowledge the client's emotions and concerns. It's important to validate the client's feelings and provide an opportunity for them to express themselves before offering reassurance.

A nurse is reviewing laboratory results for four clients who are scheduled for surgery. Which of the following laboratory values should the nurse report to the surgeon?
Explanation
Choice A reason:
Hct 42% is not appropriate. This haematocrit value is within the normal range (usually around 36-46% for females and 38-50% for males).
Choice B reason:
WBC count 8,000/mm3 is not appropriate. This white blood cell count is within the normal range (typically around 4,500 to 11,000/mm3).
Choice C reason:
INR of 1.6 An INR (International Normalized Ratio) of 1.6 indicates that the client's blood clotting time is prolonged, which means that they might have a decreased ability to form blood clots. This could pose a significant risk during surgery, as proper blood clotting is important to prevent excessive bleeding. The surgeon needs to be aware of this result to determine if any adjustments to the surgical plan or preoperative medications are necessary to ensure the client's safety.
Choice D reason:
Platelets 95,000/mm3 is not appropriate This platelet count is slightly lower than the normal range (typically around 150,000 to 450,000/mm3), but it might not be low enough to be immediately concerning, especially if the client doesn't have a history of bleeding disorders. However, it's still important for the surgical team to be aware of this value.
A home health nurse is providing care to an older adult client during the winter. During an in-home visit, the nurse notes that the thermostat is set to 12.8° C (55° F). The client tells the nurse, "I keep the heat set low because I can't afford to pay the bill." Which of the following actions should the nurse take?
Explanation
Recommending staying at a local shelter might not be appropriate unless the client's health is in immediate danger due to the low temperature. It's better to explore other options first.
Choice B reason:
Contacting the client's family members about their financial status might not be necessary or respectful of the client's privacy without their consent.
Choice C reason:
Contact the local Department of Health and Human Services for the client. Contacting the local Department of Health and Human Services can help ensure that appropriate resources and assistance are provided to the client. They may have programs or services available to assist individuals who are struggling to afford heating during the winter. This action addresses the immediate concern of the client's health and the living environment.
Choice D reason:
Providing information about the dangers of hypothermia is important, but the client's current situation of living in a cold environment should be addressed first. The nurse can provide this information along with appropriate resources to help the client.
A home health nurse is providing care to an older adult client during the winter. During an in-home visit, the nurse notes that the thermostat is set to 12.8° C (55° F). The client tells the nurse. "I keep the heat set low because I can't afford to pay the bill." Which of the following actions should the nurse take?
Explanation
Choice A reason:
Recommending staying at a local shelter might not be appropriate unless the client's health is in immediate danger due to the low temperature. It's better to explore other options first.
Choice B reason:
Contacting the client's family members about their financial status might not be necessary or respectful of the client's privacy without their consent.
Choice C reason:
Contact the local Department of Health and Human Services for the client. Contacting the local Department of Health and Human Services can help ensure that appropriate resources and assistance are provided to the client. They may have programs or services available to assist individuals who are struggling to afford heating during the winter. This action addresses the immediate concern of the client's health and the living environment.
Choice D reason:
Providing information about the dangers of hypothermia is important, but the client's current situation of living in a cold environment should be addressed first. The nurse can provide this information along with appropriate resources to help the client.
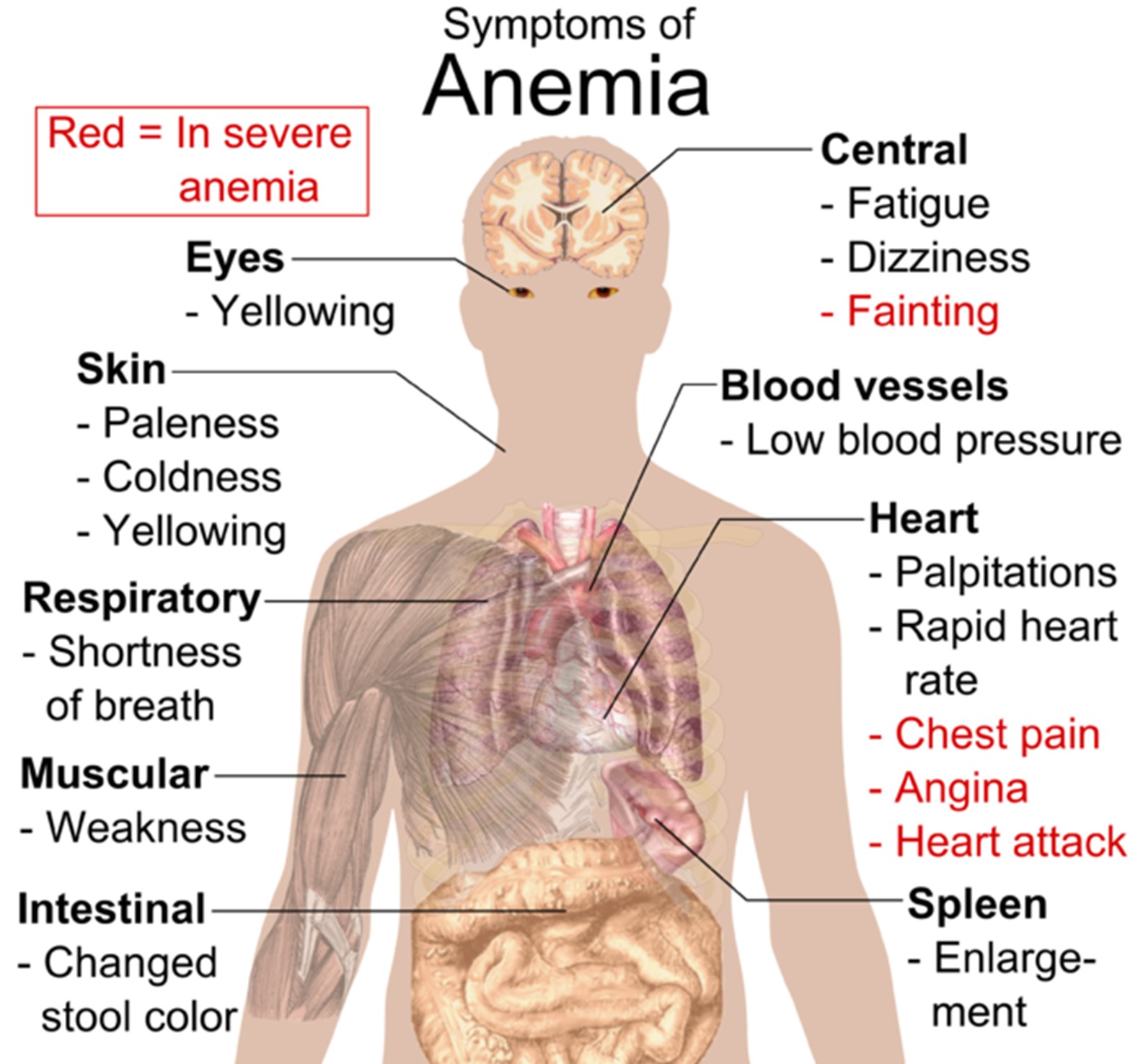
A nurse is caring for a client who has anemia. Which of the following assessment findings should the nurse anticipate with the client's condition?
Explanation
Choice A reason:
Bradycardia is incorrect. Bradycardia refers to a slow heart rate, and while anaemia can lead to an increased heart rate (tachycardia) as the body tries to compensate for the decreased oxygen levels, it is not typically associated with bradycardia.
Choice B reason:
Headache Anaemia is a condition characterized by a decreased number of red blood cells or a decrease in the amount of haemoglobin in the blood, leading to reduced oxygen-carrying capacity. This can result in decreased oxygen delivery to various tissues and organs, including the brain. As a result, clients with anaemia often experience symptoms such as fatigue, weakness, and headaches.
Choice C reason:
Flushed skin colour - Anaemia is more likely to cause paleness of the skin (pallor) due to the decreased haemoglobin levels, rather than flushed skin colour.
Choice D reason:
Heat intolerance - Heat intolerance is not a typical symptom of anaemia. It might be seen in conditions affecting the thyroid or related to hormonal imbalances, but it is not directly related to anaemia.
A nurse is checking a client's ventilator settings. The nurse should understand that positive end-expiratory pressure has which of the following purposes?
Explanation
Choice A Reason:
To prevent alveolar collapse is the correct answer. Positive end-expiratory pressure (PEEP) is used in mechanical ventilation to prevent alveolar collapse during expiration. Alveolar collapse, also known as atelectasis, can occur when the alveoli (air sacs in the lungs) collapse and don't fully re-inflate during the breathing cycle. This can lead to impaired gas exchange and decreased lung compliance. By applying positive pressure to the airways at the end of expiration, PEEP helps keep the alveoli open and improves oxygenation by maintaining lung volume.
Choice B Reason:
Positive airway pressure during inspiration is typically provided by the inspiratory pressure support, not by PEEP.
Choice C Reason:
Tidal volume refers to the amount of air moved into and out of the lungs with each breath. It is not the purpose of PEEP.
Choice D Reason:
Controlling the rate of ventilations is usually achieved by adjusting the ventilator settings for respiratory rate, not by using PEEP.
A nurse in an emergency department is preparing a client for emergency surgery. The client's blood alcohol level is 180 mg/dL. Which of the following actions is the nurse's priority?
Explanation
Choice A reason:
Obtaining consent for surgery is the correct answer. Obtaining informed consent for surgery is a critical and ethical step to ensure the client's rights are respected and that necessary medical interventions can be performed. However, in cases where the client is unable to provide consent due to their level of intoxication, the nurse should follow established protocols for obtaining consent from a legal guardian or
Choice B reason:
Insert an NG tube is incorrect. Inserting a nasogastric (NG) tube might be a necessary step in preparing a client for surgery in certain cases, but it is not the top priority in this situation. Obtaining consent for surgery takes precedence.
Choice C reason:
Applying ant embolic stockings is incorrect. Applying ant embolic stockings, also known as compression stockings, is an important measure to prevent blood clots (deep vein thrombosis) during and after surgery. However, obtaining consent for surgery is more urgent in an emergency situation.
Choice D reason:
Inserting an indwelling urinary catheter is incorrect. Inserting a urinary catheter might be necessary to monitor the client's urinary output during surgery, but obtaining consent for surgery is the priority action.
Sign Up or Login to view all the 66 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

