RN ATI Medsurg
Total Questions : 35
Showing 25 questions, Sign in for moreA nurse is caring for a client who is 1 day postoperative following a thyroidectomy and reports severe muscle spasms of the lower extremities. Which of the following actions should the nurse take?

Explanation
A. Checking the pedal pulses is important for assessing circulation, but it may not directly address the cause of the muscle spasms. In this case, addressing the electrolyte imbalance is a higher priority.
B. Requesting a relaxant might provide temporary relief for muscle spasms, but it does not address the potential underlying cause. It's important to identify and treat the root issue.
C. Correct. Severe muscle spasms in a client post-thyroidectomy could indicate hypocalcemia, as the parathyroid glands, which regulate calcium levels, can be affected during the surgery. Verifying the most recent calcium level will help determine if this is the cause.
D. Administering an oral potassium supplement addresses a different electrolyte imbalance (hypokalemia), which is not typically associated with muscle spasms following a thyroidectomy. Calcium levels are more relevant in this context.
A nurse is caring for an adolescent client who has a long history of diabetes mellitus and is being admitted to the emergency department confused, flushed, and with an acetone odor on the breath. Diabetic ketoacidosis is suspected. The nurse should anticipate using which of the following types of insulin to treat this client?

Explanation
A. NPH insulin: NPH insulin, also known as Neutral Protamine Hagedorn, is an intermediate acting insulin. It has a slower onset of action and a longer duration compared to regular insulin. It is not the best choice for treating diabetic ketoacidosis (DKA) because it does not act quickly enough to lower dangerously high blood glucose levels in this acute situation.
B. Insulin glargine: Insulin glargine is a long-acting basal insulin. It has a slow, steady release and provides a consistent level of insulin over an extended period. Like NPH insulin, it is not suitable for rapidly lowering blood glucose levels in a DKA emergency.
C. Insulin detemir: Insulin detemir is another long-acting basal insulin similar to glargine. It has a slow onset and provides a sustained release of insulin. It is not the first-line choice for treating DKA due to its slower action.
D. Regular Insulin: Regular insulin, also known as short-acting or fast-acting insulin, has a rapid onset of action. When administered intravenously, it can quickly lower blood glucose levels. This makes it the preferred choice for treating diabetic ketoacidosis (DKA) where prompt action is essential to correct the severe hyperglycemia and associated metabolic imbalances.
A nurse is caring for a client who has chronic hypothyroidism. For which of the following conditions should the nurse monitor?
Explanation
A. Photophobia is not typically associated with hypothyroidism. It can be a symptom of conditions affecting the eyes, such as certain infections or ocular disorders.
B. Exophthalmos is a protrusion of the eyeballs and is a characteristic symptom of hyperthyroidism (overactive thyroid), not hypothyroidism (underactive thyroid).
C. Correct. Lethargy is a common symptom of hypothyroidism. It is characterized by extreme tiredness, sluggishness, and lack of energy.
D. Goiter is an enlargement of the thyroid gland and can occur in both hyperthyroidism and hypothyroidism. However, it is not a direct symptom; it is a physical finding that can be associated with thyroid disorders.
A nurse is assessing a client who has hypoparathyroidism. Which of the following findings should the nurse expect?
Explanation
A. Flaccid muscles are associated with conditions like hypokalemia, not hypoparathyroidism. In hypoparathyroidism, there is a deficiency of parathyroid hormone (PTH), which leads to low calcium levels and can result in muscle spasms and tetany, not flaccid muscles.
B. While anorexia can occur in clients with various health conditions, it is not a specific finding associated with hypoparathyroidism.
C. Correct. Hypoparathyroidism is characterized by low levels of parathyroid hormone (PTH), which leads to low calcium levels in the blood. This can cause symptoms such as numbness, tingling, and muscle cramps, especially in the extremities.
D. A positive Chvostek's sign is associated with hypocalcemia, which can be caused by hypoparathyroidism. Therefore, a negative Chvostek's sign would not be an expected finding in a client with hypoparathyroidism.
A patient is scheduled for surgery to remove a tumor of the anterior pituitary. Which hormone should the nurse expect to be affected by this surgery? Select all that apply.
Explanation
A. Thyroid stimulating hormone (TSH): The anterior pituitary gland secretes TSH, which regulates the thyroid gland's function. Surgery on the anterior pituitary can potentially disrupt the production and regulation of TSH.
B. Prolactin: The anterior pituitary gland also produces prolactin. Surgery on the anterior pituitary can affect prolactin production.
C. Oxytocin: Oxytocin is produced by the posterior pituitary, not the anterior pituitary. Surgery on the anterior pituitary would not directly impact oxytocin production.
D. Gonadotropin hormones: These include follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which are important for reproductive function. The anteriorpituitary secretes these hormones, so surgery on the anterior pituitary can impact their production.
E. Adrenocorticotropic hormone (ACTH): ACTH is essential for the stimulation of cortisol release from the adrenal glands. The production of ACTH is regulated by the anterior pituitary, so surgery in this area can affect ACTH levels.
A nurse is assessing a client who has thyrotoxicosis after taking too high of a level of levothyroxine. Which of the following manifestations should the nurse expect?
Explanation
A. Drowsiness is not a typical manifestation of thyrotoxicosis. Instead, individuals with thyrotoxicosis often experience restlessness and anxiety due to excessive thyroid hormone levels.
B. Dry skin is more commonly associated with hypothyroidism (insufficient thyroid hormone levels), rather than thyrotoxicosis (excessive thyroid hormone levels).
C. Bradycardia (slower than normal heart rate) is a symptom of hypothyroidism, not thyrotoxicosis. In thyrotoxicosis, tachycardia (an abnormally rapid heart rate) is a common finding.
D. Correct. Heat intolerance is a classic symptom of thyrotoxicosis. Excessive thyroid hormone levels can lead to an increased metabolic rate, making individuals more sensitive to heat.
A nurse is assessing a client who is admitted with hyperthyroidism. The client reports a weight loss of 5.4 kg (12 lb) in the last 2 months, increased appetite, increased perspiration, fatigue, menstrual irregularity, and restlessness. Which of the following actions should the nurse take to prevent a thyroid crisis?
Explanation
A. Administering aspirin for hyperthermia is not a standard intervention for hyperthyroidism. Hyperthermia can occur in severe cases of hyperthyroidism, but the primary intervention is to address the underlying thyroid dysfunction and provide supportive care.
B. Keeping the client NPO (nothing by mouth) is not directly related to preventing a thyroid crisis in hyperthyroidism. It may be necessary for certain pre-operative preparations or if the client is undergoing specific procedures, but it does not address the prevention of a thyroid crisis.
C. While monitoring for signs of hypocalcemia is important in some cases of thyroid dysfunction, it is not the primary action to prevent a thyroid crisis. In hyperthyroidism, the focus is on managing excessive thyroid hormone levels.
D. Correct. Providing a quiet, low-stimulus environment is a crucial nursing intervention for clients with hyperthyroidism. They can be highly sensitive to external stimuli due to their increased metabolic rate. A calm environment helps reduce stress and the risk of exacerbating symptoms, potentially preventing a thyroid crisis.
The primary health-care provider prescribes a cough syrup 0.4 g every 4 hours. The dosage strength of the syrup is 100 mg/5 mL. The medication bottle contains a measuring spoon that measures in teaspoons and tablespoons. How many teaspoons will the nurse instruct the client to take?
Explanation
One gram is equal to 1000 milligrams, and one teaspoon is equal to 5 milliliters. Therefore, the nurse can use the following formula:
0.4 g x 1000 mg/g x 5 mL/100 mg x 1 tsp/5 mL = 2 tsp
The nurse will instruct the client to take two teaspoons of cough syrup every four hours as prescribed by the primary health-care provider.
A nurse is preparing a teaching session about reducing the risk of complications of diabetes mellitus. Which of the following information should the nurse plan to include in the teaching? (Select all that apply.)
Explanation
A. Incorrect. Sustaining hyperglycemia is not a recommended approach. In fact, it is crucial to maintain blood glucose levels within a target range to prevent complications associated with diabetes.
B. Correct. Maintaining optimal blood pressure is important for preventing kidney damage, which is a common complication of diabetes. High blood pressure can exacerbate kidney problems in individuals with diabetes.
C. Correct. Reducing cholesterol and saturated fat intake is important for managing cardiovascular risk factors associated with diabetes. Elevated cholesterol levels are a risk factor for heart disease, which is more prevalent in individuals with diabetes.
D. Correct. Enrolling in a smoking cessation program is essential. Smoking increases the risk of cardiovascular disease, which is already elevated in individuals with diabetes. Quitting smoking is a crucial step in reducing this risk.
E. Correct. Increasing physical activity is an important component of diabetes management. Regular exercise helps improve insulin sensitivity, maintain a healthy weight, and reduce the risk of cardiovascular complications.
The primary healthcare provider prescribes a cough syrup of 0.4 g every 4 hours. The dosage strength of the syrup is 100 mg/5 mL. The medication bottle contains a measuring spoon that measures in teaspoons and tablespoons. How many teaspoons will the nurse instruct the client to take?
Explanation
One gram is equal to 1000 milligrams, one milliliter is equal to 0.2 teaspoons, and one teaspoon is equal to 5 milliliters. Using these conversion factors, the nurse can perform the following steps:
- Multiply the prescribed amount of cough syrup by 1000 to get the equivalent in milligrams: 0.4 g x 1000 = 400 mg
- Divide the equivalent in milligrams by the dosage strength of the syrup to get the equivalent in milliliters: 400 mg / 100 mg/5 mL = 20 mL
- Multiply the equivalent in milliliters by 0.2 to get the equivalent in teaspoons: 20 mL x 0.2 = 4 teaspoons
Therefore, the nurse will instruct the client to take 4 teaspoons of cough syrup every 4 hours.
A nurse is planning care for a client who is postoperative following a thyroidectomy. Which of the following interventions should the nurse include in the plan?
Explanation
A. Placing the head of the client's bed in the flat position is contraindicated after a thyroidectomy due to the risk of compromising the airway and causing respiratory distress. The head of the bed should be elevated to semi-Fowler's position to promote comfort and reduce swelling.
B. Correct. Instructing the client to deep breathe every 4 hours is important for preventing respiratory complications and maintaining lung function after surgery. This helps prevent atelectasis and pneumonia.
C. Hyperextending the client's neck is contraindicated after a thyroidectomy, as it can put tension on the suture line and potentially cause bleeding or damage to the surgical site. The neck should be maintained in a neutral or slightly flexed position.
D. Checking the client's voice every 2 hours is not a necessary intervention. While assessing vocal cord function is important, checking it this frequently may cause unnecessary disruption to the client's rest and recovery. It is generally assessed less frequently unless there are specific concerns about vocal cord function.
Propylthiouracil (PTU) is prescribed for a client with Graves' disease. The nurse should teach the client to immediately report which of the following?
Explanation
A. Correct. Propylthiouracil (PTU) is an antithyroid medication used to treat hyperthyroidism, including Graves' disease. It can sometimes cause agranulocytosis, a condition characterized by a severe reduction in white blood cells, which can lead to symptoms like a sore throat and fever. These symptoms should be reported immediately.
B. Constipation is not a common side effect of propylthiouracil. If it occurs, it is usually not an urgent concern, and can often be managed with dietary and lifestyle changes.
C. Increased urine output is not typically associated with propylthiouracil. It is more likely to be seen with diuretic medications or conditions like diabetes.
D. Painful, excessive menstruation is not a direct side effect of propylthiouracil. However, hormonal changes related to hyperthyroidism can affect menstrual patterns. If the client is experiencing significant changes in menstrual bleeding, it should be reported to the healthcare provider, but it may not be considered an immediate emergency.
A nurse in an emergency department is caring for a client who has diabetic ketoacidosis (DKA) and a blood glucose level of 925 mg/dL. The nurse should anticipate which of the following prescriptions from the provider?
Explanation
A. Glucocorticoid medications are not the primary treatment for diabetic ketoacidosis (DKA). They may be used in specific situations, but they are not the first-line treatment.
B. Oral hypoglycemic medications are not appropriate for a client with DKA. DKA is a serious condition that requires prompt treatment with insulin and intravenous fluids.
C. Dextrose 5% in 0.45% sodium chloride is not the initial treatment for DKA. This solution contains dextrose, which would raise the blood glucose levels, but it does not provide the necessary insulin to address the underlying issue of insulin deficiency.
D. Correct. The initial treatment for DKA involves administering intravenous fluids, typically with 0.9% sodium chloride (normal saline). This helps to restore blood volume, correct electrolyte imbalances, and gradually lower the high blood glucose levels. Insulin is also administered concurrently to address the underlying insulin deficiency.
The nurse is reviewing a teaching tool created for insulin therapy Which statement on the tool should be corrected? Select all that apply.
Explanation
A. NPH insulin may be mixed with pens. This statement is correct. NPH insulin can be mixed with other insulins, and it is available in pens for ease of administration.
B. Insulin detemir is administered once or twice daily, not necessarily with meals. Detemir is a long-acting insulin and can be taken once or twice daily, depending on the individual's specific treatment plan. It does not need to be strictly timed with meals.
C. Insulin glargine is a long-acting insulin and is generally not used as a first-line treatment for gestational diabetes. Short-acting insulins are typically recommended. Gestational diabetes is usually managed with short-acting insulins (like regular insulin) due to their faster onset and shorter duration of action. Long-acting insulins like glargine are not typically used in this context.
D. Regular insulin can be administered intravenously. This is a correct statement. Regular insulin can indeed be given intravenously in a hospital setting for precise control of blood glucose levels.
E. Lispro is a rapid-acting insulin. This statement is accurate. Lispro is a rapid-acting insulin analog used to control high blood sugar levels during and after meals. It has a fast onset of action.
The client with type 1 diabetes mellitus is prescribed to take NPH (Humulin N) insulin at 5 PM each day. The client should be instructed that the greatest risk of hypoglycemia will occur about what time?
Explanation
1 AM while sleeping: NPH insulin, like Humulin N, typically reaches its peak effectiveness about 4-12 hours after administration. Since the client takes it at 5 PM, the time of greatest risk for hypoglycemia is around 1 AM when the insulin's effects are at their peak. This is a critical period for monitoring blood glucose levels.
B. 8 PM shortly after dinner: By 8 PM, the NPH insulin's effectiveness is not at its peak. It's been about 3 hours since administration, and the insulin is still working to lower blood glucose levels. This time frame is not associated with the highest risk of hypoglycemia.
C. 6 PM shortly after dinner: At 6 PM, it's been only about an hour since the client took the NPH insulin. The insulin is just beginning to take effect, and the risk of hypoglycemia is not as high as it would be later in the night.
D. 11:00 AM, shortly before lunch: By 11:00 AM, the effects of the NPH insulin from the previous evening have largely worn off. This time frame is not associated with a high risk of hypoglycemia related to the evening dose of NPH insulin.
A nurse is caring for a client who is 1 day postoperative following a transsphenoidal hypophysectomy. While assessing the client, the nurse notes a large area of clear drainage seeping from the nasal packing. Which of the following should be the nurse's initial action?
Explanation
A. Obtaining a culture of the drainage may be necessary, but the immediate concern is to determine if the drainage is cerebrospinal fluid (CSF) or another type of fluid. Checking for glucose content is a rapid way to differentiate CSF from other fluids.
B. Correct. Clear drainage from the nose post-transsphenoidal hypophysectomy may indicate a CSF leak, which is a potential complication. Checking the drainage for glucose can help differentiate CSF from other fluids, as CSF contains glucose. If the drainage tests positive for glucose, it indicates the presence of CSF.
C. Documenting the amount of drainage is important, but determining the nature of the drainage (CSF or other fluid) takes precedence in this situation.
D. Notifying the client's provider is important, but the nurse should gather information about the drainage first by checking for glucose content. This information will be crucial for the healthcare provider to make decisions about further interventions
A nurse is reviewing guidelines to prevent DKA during periods of illness with a client who has type 1 diabetes mellitus. Which of the following instructions should the nurse include in the teaching?
Explanation
A. Incorrect. Withholding insulin during illness is not recommended. Clients with type 1 diabetes should continue to take their prescribed insulin even when they are ill. Insulin is necessary to regulate blood glucose levels, and illness can increase the body's demand for insulin.
B. Incorrect. Drinking calorie-free liquids is important to prevent dehydration during illness, but specific fluid amounts should be individualized based on the client's needs and healthcare provider's recommendations. The given volume is not a universally applicable guideline.
C. Incorrect. Testing blood glucose levels every 8 hours may not be frequent enough during illness. Blood glucose should be monitored more frequently to closely track changes in response to illness and adjust insulin doses accordingly.
D. Correct. Checking urine for ketones when blood glucose levels exceed 240 mg/dL is an important guideline during illness. Elevated blood glucose levels can lead to the production of ketones, and checking for ketones in the urine helps identify the early signs of diabetic ketoacidosis (DKA). If ketones are present, the client should follow a specific plan of action as outlined by their healthcare provider, which may include adjusting insulin doses or seeking medical attention.
A nurse is preparing to administer furosemide 40 mg IV. Available is furosemide 10 mg/1 mL. How many ml should the nurse administer per dose?
Explanation
Dose (mg) / Concentration (mg/mL) = Volume (mL)
Plugging in the given values, we get:
40 mg / 10 mg/mL = 4 Ml
Therefore, the nurse should administer 4 mL of furosemide per dose.
A nurse is caring for a client who is 1 day postoperative following a subtotal thyroidectomy. The client reports a tingling sensation in the hands, the soles of the feet, and around the lips. For which of the following findings should the nurse assess the client?
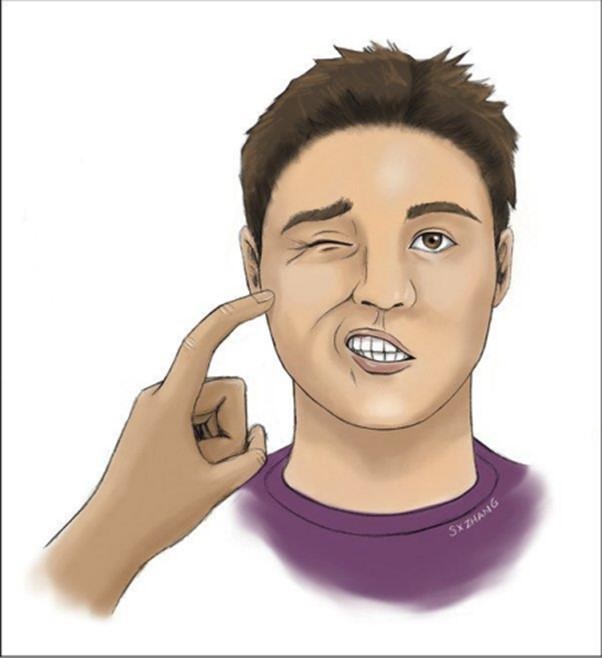
Explanation
A. Correct. Chvostek's sign is a clinical sign of hypocalcemia. It is elicited by tapping on the facial nerve, just anterior to the ear, and observing for facial twitching or spasm.
B. Incorrect. Kernig's sign is a test for assessing meningitis and involves flexing the hip and knee at 90-degree angles and then extending the knee. This test is not relevant to the client's reported symptoms.
C. Incorrect. Brudzinski's sign is another test for assessing meningitis. It involves flexing the neck forward and observing for involuntary flexion of the hips and knees. This test is not relevant to the client's reported symptoms.
D. Incorrect. Babinski's sign is used to assess upper motor neuron lesions. It involves stimulating the sole of the foot, and in a positive response, the big toe extends upward. This test is not relevant to the client's reported symptoms.
At 8 a.m. the nurse is reviewing patient assignments and notes one of the patients has a current blood glucose of 264. Breakfast is routinely served at 8:30. The following orders are noted in the chart. What action should the nurse take? Accucheck before meals and at bedtime with sliding scale insulin aspart SQ: Glucose 0-150 Administer 0 units; 151-200 Administer 2 units; 201-250 Administer 4 units: 251-300 Administer 6 units: 301-350 Administer 8 units; 351- 400 Administer 10 units; >400 Notify physician.
Explanation
A. This option corresponds to the blood glucose range of 151-200. However, the patient's current blood glucose level is 264, which falls into the range of 251-300. Therefore, administering 2 units would not be appropriate in this case.
B. The patient's current blood glucose level is 264, which falls into the range of 251-300. According to the sliding scale insulin aspart orders, for this range, 6 units should be administered. This option aligns with the patient's blood glucose level and the prescribed protocol.
C. This option corresponds to the blood glucose range of 351-400. The patient's blood glucose level of 264 does not fall into this range, so administering 10 units would be excessive and potentially lead to hypoglycemia.
D. This option corresponds to the blood glucose range of 201-250. The patient's current blood glucose level is 264, which falls into the range of 251-300. Therefore, administering 4 units would not be sufficient to address the elevated blood glucose level.
When preparing to provide morning medications, the nurse would give levothyroxine (Synthroid) ordered daily in which of the following ways?
Explanation
A. This option is not ideal for levothyroxine (Synthroid) because it should be taken on an empty stomach for optimal absorption. Taking it with food, especially a meal like breakfast, can interfere with its absorption.
B. This is the correct option. Levothyroxine should be taken in the morning, at least 30 minutes before breakfast, or any other medications. Taking it on an empty stomach ensures the best absorption of the medication.
C. Taking levothyroxine in the evening is not recommended. It should be taken in the morning to coincide with the body's natural circadian rhythm and to avoid potential interactions with food or other medications.
D. While it's important to take levothyroxine in the morning before breakfast, it is not necessary to take it without any other medications. It can be taken alongside other daily medications as long as there are no interactions that would affect its absorption.
A nurse is assessing a client who has hypothyroidism. The nurse should expect which of the following findings?
Explanation
A. Incorrect. Palpitations, which are rapid or irregular heartbeats, are more commonly associated with hyperthyroidism, where there is an excess of thyroid hormones.
B. Incorrect. Diaphoresis, or excessive sweating, is not typically associated with hypothyroidism.
C. Incorrect. Exophthalmos, or bulging of the eyes, is a characteristic finding in hyperthyroidism (specifically Graves' disease) and is not typically seen in hypothyroidism.
D. Correct. Weight gain is a common finding in hypothyroidism. The slowing down of metabolic processes due to insufficient thyroid hormones can lead to an increase in body weight.
The nurse is assessing an older patient with type 2 diabetes mellitus. What age-related endocrine change should the nurse expect in this patient?
Explanation
A. Incorrect. Aging is associated with a decrease in insulin production and a reduction in the speed of insulin release, not an increase.
B. Incorrect. Intolerance of fatty foods is not typically an age-related endocrine change. It may be related to other factors such as digestive issues.
C. Correct. Decreased sensitivity to insulin is a common age-related endocrine change, particularly in individuals with type 2 diabetes mellitus.
D. Incorrect. Lower and prolonged blood glucose levels are not an expected age-related endocrine change. Instead, insulin resistance tends to result in elevated blood glucose levels.
When preparing to provide morning medications, the nurse would give levothyroxine (Synthroid) ordered daily in which of the following ways?
Explanation
A. Incorrect. Taking levothyroxine with breakfast may reduce its absorption due to food interference.
B. Correct. Levothyroxine should be taken in the morning on an empty stomach, at least 30 minutes before any other medications or food, to ensure optimal absorption.
C. Incorrect. Taking levothyroxine in the evening with a snack is not recommended. It should be taken on an empty stomach for best results.
D. Incorrect. Taking levothyroxine in the morning before breakfast is advised, but it should also be done on an empty stomach. Additionally, there's no need to avoid other medications if they do not interfere with its absorption.
A client is being discharged after having a thyroidectomy. Which discharge instructions are appropriate for this client? Select all that apply.
Explanation
A. Take thyroid replacement medication, as ordered. This is crucial for individuals who have undergone a thyroidectomy, as they will likely need thyroid hormone replacement therapy to maintain normal thyroid function.
B. Watch for changes in body functioning, such as lethargy, restlessness, sensitivity to cold, and dry skin. Report them to the physician.
These symptoms could indicate potential issues with thyroid hormone levels and should be reported to the physician for further evaluation.
C. Recognize the signs of dehydration. This is important for overall health and can be especially relevant post-surgery. Dehydration can exacerbate other issues and slow down the healing process.
D. Carry injectable dexamethasone at all times. This is not a standard discharge instruction after a thyroidectomy. Dexamethasone may be prescribed for specific situations, but it is not a routine medication for all patients post-thyroidectomy.
E. Report any signs and symptoms of hypoglycemia. This is important because thyroidectomy can affect blood sugar levels. Monitoring for signs of hypoglycemia is crucial for the client's well-being.
Sign Up or Login to view all the 35 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

