RN Community Health 2019 - Exam 2 Updated 2024
Total Questions : 52
Showing 25 questions, Sign in for moreA nurse is providing teaching to a licensed nurse about case management. The nurse should include that which of the following is the responsibility of the case manager?
Explanation
Case management is a collaborative process that involves assessing, planning, implementing, coordinating, monitoring, and evaluating the options and services required to meet the patient's health needs. The case manager is responsible for evaluating the patient's needs and developing a care plan that meets those needs. The case manager works closely with the patient, their family, and the healthcare team to ensure that the care plan is being followed and adjusted as necessary.
Teaching a smoking cessation support group, performing employee risk assessments, and familiarizing with OSHA Standards in the workplace are not responsibilities of the case manager. These tasks are typically performed by other healthcare professionals such as nurses, occupational health nurses, or environmental health and safety professionals.
A nurse is developing health promotion strategies for older adult clients at an assisted living facility. Which of the following strategies is the best to include?
Explanation
Regular exercise is an essential component of health promotion for older adults. Exercise helps to maintain and improve physical function, mobility, and independence, reduces the risk of falls, and helps to prevent chronic conditions such as diabetes, cardiovascular disease, and osteoporosis. Exercise also has mental health benefits, such as reducing depression and anxiety.
Scheduling annual dental examinations for the clients (A) is important but is not the best health promotion strategy for older adults at an assisted living facility. While dental health is important, exercise is a more comprehensive strategy that addresses multiple aspects of health.
Providing the clients with a low-fat diet (B) is also important for health promotion, but it is not as effective as exercise in promoting physical and mental health.
Immunizing the clients against influenza (D) is important to prevent infection, but it is not a health promotion strategy that addresses overall health and wellbeing.
A nurse in an antepartum clinic is reviewing the medical records of four clients. Which of the following infectious conditions should the nurse report to the Centres for Disease Control and Prevention?
Explanation
Gonorrhoea is a sexually transmited infection (STI) that is reportable to the Centers for Disease Control and Prevention (CDC) in the United States. Reporting of cases of gonorrhoea helps public health officials monitor the spread of the disease and implement measures to prevent its transmission.
Genital herpes simplex virus (A), bacterial vaginosis (C), and human papillomavirus (D) are also STIs, but they are not reportable to the CDC. However, it is still important for healthcare providers to diagnose and treat these conditions appropriately to prevent complications and reduce the risk of transmission.
A school nurse is planning primary prevention activities for the school year. Which of the following actions should the nurse plan to take?
Explanation
Primary prevention activities aim to prevent the onset of disease or injury. Monitoring the immunization status of students is a primary prevention activity because it helps to prevent the spread of infectious diseases that can cause serious illness and even death. By monitoring the immunization status of students, the school nurse can ensure that students are up-to-date on their vaccinations and can provide education and resources to parents and guardians who may have questions or concerns about immunizations.
Providing referrals for students who have asthma (A) and providing first aid for injured students (B) are both important activities that the school nurse should be prepared to do, but they are not primary prevention activities. These activities are considered secondary prevention because they aim to identify and treat health problems early before they become more severe.
Scheduling hearing screenings for each grade level (D) is a tertiary prevention activity because it aims to prevent complications and disability resulting from existing hearing problems.

A home health nurse is providing teaching to the guardian of a child who has leukemia about methods to prevent complications. Which following statement by the guardian indicates an understanding of the teaching?
Explanation
Children with leukemia are at increased risk for infection and other complications due to their weakened immune system. One potential complication is oral mucositis, which can cause painful sores in the mouth and throat. Inspecting the child's mouth for sores once a week is a preventive measure that can help identify this complication early and allow for prompt treatment.
Taking the child's rectal temperature daily (A) is not a necessary preventive measure for a child with leukemia unless directed by the healthcare provider.
Riding a bicycle (B) can be a healthy activity for a child with leukemia but it does not prevent complications.
Getting a measles, mumps, and rubella vaccine (D) is important for preventing these specific infectious diseases but it is not directly related to preventing complications in a child with leukemia. The vaccine may also not be recommended for a child with leukemia, depending on their treatment plan and medical history.

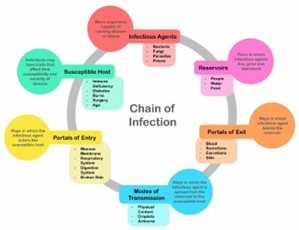
A nurse is caring for a patient who has the hepatitis A virus. Which of the following reservoirs should the nurse identify for this infection?
Explanation
Hepatitis A is primarily transmited through the fecal-oral route, meaning that the virus is present in the stool of infected individuals and can be spread through contaminated food, water, or surfaces. Therefore, the reservoir for hepatitis A is the gastrointestinal tract of infected individuals, specifically their feces.
Blood (A) is not a reservoir for hepatitis A, as the virus is not typically present in the blood.
The genitourinary tract (C) and skin (D) are also not reservoirs for hepatitis A, as the virus is not typically present in these areas.

A nurse in an extended care facility enters the room of a client and notices a fire in the trash can. Which of the following actions is the nurse's priority?
Explanation
According to the fire safety guidelines for hospitals, the nurse’s priority in this situation is to move the client to another location. This is because the client’s safety and well-being are the most important considerations in a fire emergency. The nurse should move the client to a safe area away from the fire, preferably behind a fire door or in another fire compartment. The nurse should also close the door of the room where the fire is to prevent the spread of smoke and flames.
The nurse should then activate the alarm to alert other staff and the fire department. The nurse should also use a fire extinguisher to attempt to extinguish the fire, if it is safe and feasible to do so. However, the nurse should not put themselves or the client at risk by trying to fight the fire. The nurse should follow the RACE acronym for fire response: Rescue, Alarm, Contain, and Extinguish.
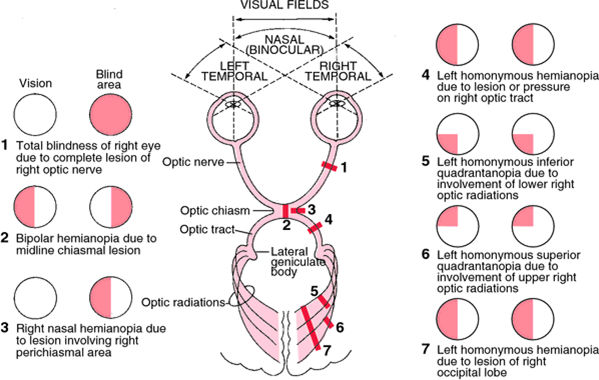
A home health nurse is performing an eye assessment for an older adult client. Which of the following findings is the priority for the nurse to report to the provider?
Explanation
Hemianopsia is a visual field defect in which there is a loss of vision in half of the visual field of one or both eyes. It is a serious finding that can significantly impact a person's ability to perform daily activities and can indicate a neurological problem. The nurse should report this finding to the provider immediately to ensure prompt evaluation and management.
Conjunctivitis (A) is an inflammation of the conjunctiva and is not typically an urgent finding, although it may require treatment depending on the underlying cause.
Decreased near vision (B) is a common finding in older adults and can often be addressed with corrective lenses or other interventions. While it should be noted and addressed, it is not a priority finding that requires immediate reporting to the provider.
Increased sensitivity to glare (C) is also a common finding in older adults and can be addressed with interventions such as sunglasses or tinted lenses. While it should be noted and addressed, it is not a priority finding that requires immediate reporting to the provider.
A community health nurse is working with a task force to decrease community violence. Which of the following planned interventions should the nurse identify as a primary prevention strategy?
Explanation
Primary prevention focuses on preventing a problem before it occurs by promoting health and wellness. Providing parenting classes for local parents can help them develop skills to manage their children's behavior effectively, which can reduce the risk of violence in the community.
While the other options are important interventions to address violence, they are considered secondary or tertiary prevention strategies, as they aim to prevent violence from recurring or manage its consequences.
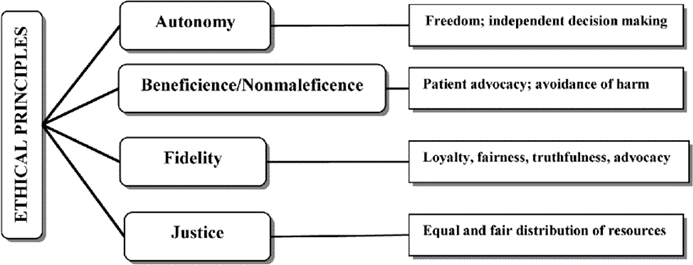
A nurse is caring for a client who asks, "Can I decide not to continue with chemotherapy?" The nurse responds, "This is your choice, and I'll support whatever decision you make."
The nurse's response is an example of which of the following ethical principles?
Explanation
The nurse's response demonstrates respect for the client's autonomy, which is the principle of respecting the client's right to make decisions about their own healthcare. The nurse acknowledges the client's right to make a decision and offers support for whatever decision the client makes. Beneficence is the principle of doing good for the client, while nonmaleficence is the principle of avoiding harm. Veracity is the principle of telling the truth to the client, which is not necessarily demonstrated in this scenario.
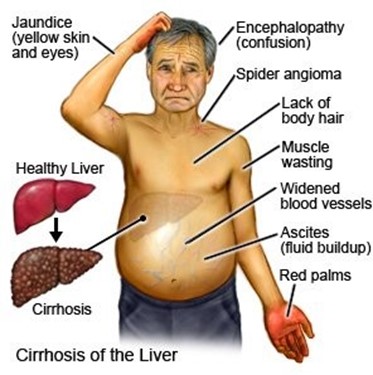
A case manager is completing discharge planning for a client who has alcohol use disorder and cirrhosis of the liver. Which of the following actions should the case manager take first?
Explanation
The first priority in discharge planning for this client should be to arrange for a home health nurse to visit the client following discharge to monitor the client's health and provide support. The client's condition is complex and requires ongoing monitoring and support to prevent relapse and ensure safety.
Providing the client with information on self-help groups and determining home safety measures are also important components of the discharge plan, but they should come after ensuring that the client has the necessary support in place. Contacting a social worker to assist with managing finances is not a priority at this time.
A home health nurse is assessing a client who has AIDS. Which of the following responses by the client indicates a risk for suicide?
Explanation
The client's statement that they are afraid of experiencing pain near the end of life may indicate a risk for suicide, as it suggests that the client may be considering suicide as a way to avoid the anticipated pain. The other statements do not necessarily indicate a risk for suicide.
Statement a) may indicate a desire to maintain autonomy and control over their healthcare decisions.
Statement b) may indicate a hopeful attitude, which can be a protective factor against suicide.
Statement d) may indicate a reliance on social support, which can also be a protective factor against suicide.
A community health nurse is teaching a group of parents about manifestations of alcohol withdrawal. Which of the following manifestations should the nurse include in the teaching?
Explanation
Alcohol withdrawal can cause a range of symptoms, including anxiety, tremors, hallucinations, and seizures. Seizures are a potentially serious complication of alcohol withdrawal that can occur within the first 24-48 hours after a person stops drinking. Hyperglycemia, or high blood sugar, is not typically associated with alcohol withdrawal. Hypotension, or low blood pressure, can occur in severe cases of alcohol withdrawal, but it is not a primary manifestation. Somnolence, or drowsiness, may be present in some cases of alcohol withdrawal, but it is not a primary manifestation and is not typically a cause for concern.

A nurse working in an assisted care facility is developing a disaster plan. Which of the following is the first action the nurse should take?
Explanation
When developing a disaster plan, the first action the nurse should take is to determine potential environmental health hazards that could affect the facility and its residents. This involves assessing the facility's location and surrounding area for potential hazards, such as floods, fires, earthquakes, or chemical spills.
Once potential hazards have been identified, the nurse can then develop appropriate response strategies specific to the needs of the residents and the facility.
Identifying materials needed for staff and resident education, developing response strategies specific to older adults, and verifying dates of the annual community-wide mass casualty drill are all important steps in disaster planning, but they should come after potential environmental health hazards have been identified.
A nurse educator is teaching a group of newly licensed nurses about maintaining client confidentiality according to HIPAA regulations. Which of the following statements by a newly licensed nurse indicates an understanding of the teaching?
Explanation
This statement is accurate because clients have the right to access their medical records under HIPAA regulations.
Option A is incorrect because HIPAA rules are federal regulations that are applicable to all states.
Option C is incorrect because sharing computer passwords with anyone, including managers, can compromise patient privacy and is a violation of HIPAA regulations.
Option D is incorrect because posting a client's diagnosis on a communication board inside the client's room can breach the client's confidentiality.

A nurse at a rural clinic is interviewing a family who has different cultural beliefs than the nurse. The family reports seeing a folk healer. Which of the following statements should the nurse make?
Explanation
This statement is open-ended and allows the family to discuss their beliefs and values related to their health and healing. It also allows the nurse to gain a better understanding of the family's cultural practices and provide culturally sensitive care.
Option A is incorrect because it is judgmental and can negatively impact the therapeutic relationship between the nurse and the family.
Option B is incorrect because it is dismissive of the family's beliefs and values and does not show respect for their cultural practices.
Option C is incorrect because it does not address the family's current health care needs or their beliefs about healing.
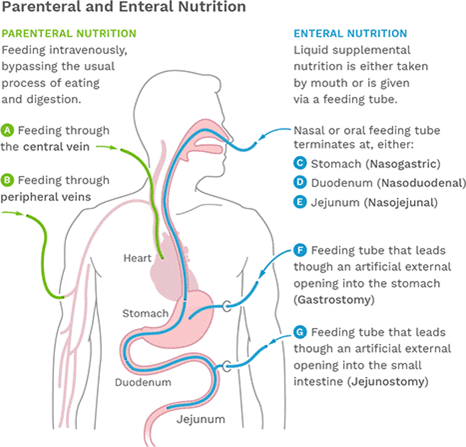
A home health nurse is caring for a client who has terminal cancer and no longer wants to receive enteral tube feedings. Which of the following actions should the nurse take?
Explanation
This action is appropriate because it allows the client to document their end-of-life wishes and ensure that they are honored.
Option A is incorrect because requesting the facility chaplain to visit the client is not directly related to the client's current health care needs.
Option C is incorrect because completing an against medical advice form is not appropriate in this situation, as the client has the right to refuse medical treatments, including enteral tube feedings.
Option D is incorrect because asking the client to sign an informed consent form is not necessary in this situation, as the client is not receiving a specific medical treatment that requires informed consent.
A nurse is providing teaching to a 50-year-old female client. Which of the following statements should the nurse include in the teaching?
Explanation
This statement is appropriate because it is a recommended preventive health measure for women in this age group to detect any potential eye problems early on.
Option A is incorrect because the American Diabetes Association recommends that individuals over the age of 45 should have their fasting blood glucose level checked every 3 years, not every 6 years.
Option C is incorrect because the United States Preventive Services Task Force does not recommend routine hearing screening in adults who do not have any symptoms of hearing loss.
Option D is incorrect because the American Cancer Society recommends that individuals over the age of 50 should have a screening colonoscopy every 10 years or a fecal occult blood test every year, not every other year until the age of 74.
A public health nurse is developing protocols to use in emergency shelters following a disaster. Which of the following interventions should the nurse include as a secondary prevention strategy for clients who survive a disaster?
Explanation
This is an important strategy to help individuals who have been displaced by a disaster to get back to their homes and communities as soon as possible.
Option A may be a helpful strategy for providing a sense of normalcy and structure for shelter residents, but it is not a secondary prevention strategy.
Option B may be important for identifying individuals who may need further support or resources, but it is also not a secondary prevention strategy.
Option D may be important for disseminating information to the public, but it is not a secondary prevention strategy.
A nurse manager at a clinic is reviewing the preventative services offered to clients. Which of the following activities should the nurse identify as a secondary prevention activity?
Explanation
The nurse should identify option C, "Refer a client who is recovering from a substance use disorder to a social service program," as a secondary prevention activity. This intervention focuses on early identification and intervention to prevent further harm or complications related to substance use disorder.
Option A is a primary prevention activity, as it focuses on preventing the development of complications through early intervention and education.
Option B is a tertiary prevention activity, as it focuses on reducing the impact of a disease or injury that has already occurred.
Option D is also a tertiary prevention activity, as it focuses on reducing the impact of a disease that has already occurred.
A nurse is working with a community health care team to devise strategies for preventing violence in the community.
Which of the following interventions is an example of tertiary prevention?
Explanation
The nurse should identify option B, "Developing resources for victims of abuse," as an example of tertiary prevention. This intervention focuses on reducing the impact of a disease or injury that has already occurred. In this case, the focus is on providing support and resources for victims of abuse to help them recover from the effects of the violence.
Option A is a primary prevention activity, as it focuses on preventing the development of complications through early intervention and education.
Option C is a combination of primary and secondary prevention, as it focuses on preventing violence from occurring and addressing it early if it does occur.
Option D is a secondary prevention activity, as it focuses on early identification and intervention to prevent further harm or complications related to intimate partner abuse.

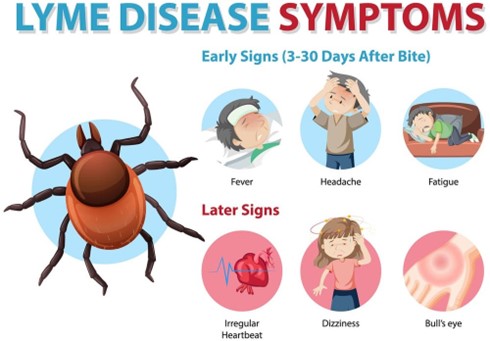
A nurse working in an infectious disease clinic is caring for a client who has a new diagnosis of Lyme disease.
Which of the following agencies is responsible for voluntarily reporting cases of this disease to the Centers for Disease Control and Prevention?
Explanation
State health departments are responsible for monitoring and reporting communicable diseases within their respective states to the Centers for Disease Control and Prevention. Lyme disease is a nationally notifiable disease, which means that cases must be reported to the Centers for Disease Control and Prevention by the state health department.
A home health nurse is discussing electrical hazards with a client. Which of the following statements should the nurse include?
Explanation
Extension cords are designed for temporary use and should not be used as a permanent solution for providing power to appliances and other electrical devices. Instead, clients should use outlets that are conveniently located near their appliances. Overuse of extension cords can create tripping hazards and increase the risk of electrical fires. It is also important for clients to avoid running cords under carpets or rugs, as this can cause the cords to overheat and increase the risk of electrical fires.
Finally, clients should be advised to unplug appliances by gripping the plug and pulling it out of the outlet, rather than pulling on the cord.
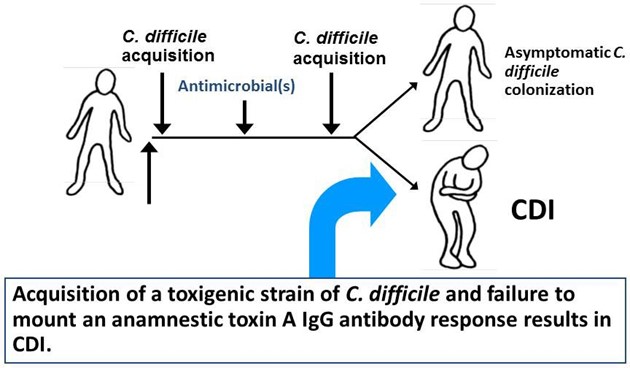
A home health nurse is caring for a client who has a Clostridium difficile infection. Which of the following actions should the nurse take?
Explanation
Clostridium difficile is a highly contagious bacterium that can survive on surfaces for long periods of time. Cleaning the bathroom with a diluted bleach solution is an effective way to kill the bacteria and prevent its spread. The nurse should also instruct the client to wash their hands frequently with soap and water, as alcohol-based hand sanitizers are not effective against Clostridium difficile.
It is not necessary for the client to wear a surgical mask when away from home, as the bacteria is primarily spread through contact with contaminated surfaces. The use of probiotics may be beneficial in restoring the balance of gut bacteria in some cases, but there is limited evidence to support its use in preventing or treating Clostridium difficile infections.
An occupational health nurse is completing a walk-through of a factory to identify workers at risk for injury.
Which of the following workers should the nurse identify as being at risk?
Explanation
Bending at the waist to lift heavy objects can increase the risk of back injury, even when wearing a back brace. The nurse should advise this worker to bend at the knees and keep the back straight when lifting heavy objects. The worker who is standing with a wide base of support when pulling a cart toward himself is using proper body mechanics, which helps reduce the risk of injury.
The worker who is 7-weeks postoperative following rotator cuff surgery and is labeling boxes should avoid lifting heavy objects or performing tasks that require excessive use of the affected arm. The worker who is standing in place for extended periods and rests one foot on a box may experience fatigue or discomfort, but is not necessarily at an increased risk for injury.
Sign Up or Login to view all the 52 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

