RN > Exit Exams
Exam Review
RN Hesi Exit
Total Questions : 150
Showing 10 questions, Sign in for moreExplanation
Nursing Interventions for Client Starting Clonazepam:
The following nursing interventions are appropriate for the client starting clonazepam 0.25 mg PO every 12 hours:
a. Screen for orthostatic hypotension:
Rationale:
- Clonazepam,like other benzodiazepines,can cause central nervous system (CNS) depression,which can lead to hypotension,particularly orthostatic hypotension.This occurs when blood pressure drops suddenly upon standing due to impaired autonomic nervous system regulation.
- Screening for orthostatic hypotension involves measuring the client's blood pressure and heart rate while lying down and then again after standing for 3 minutes.A significant drop in blood pressure (systolic decrease of 20 mmHg or diastolic decrease of 10 mmHg) or increase in heart rate (over 20 beats per minute) indicates orthostatic hypotension.
- Monitoring for orthostatic hypotension is crucial to prevent falls and other complications,especially in older adults or those with pre-existing cardiovascular conditions.
b. Provide oral care at least twice a day:
Rationale:
- Clonazepam can cause dry mouth as a side effect,which can increase the risk of cavities,gum disease,and oral infections.
- Regular oral care helps to remove plaque and bacteria,promoting oral hygiene and preventing complications.Providing oral care at least twice a day,especially before bedtime and upon waking,is essential.
d. Assess mental status regularly:
Rationale:
- Clonazepam,while indicated for anxiety and insomnia,can paradoxically cause agitation,confusion,and even hallucinations in some individuals,particularly older adults or those with pre-existing psychiatric conditions.
- Regular assessment of mental status helps to identify any adverse behavioral or cognitive changes early on.This includes monitoring for anxiety,depression,suicidal ideation,confusion,disorientation,hallucinations,and changes in sleep patterns.
e. Assist the client to the bathroom:
Rationale:
- Clonazepam can cause drowsiness and dizziness,which can increase the risk of falls,especially in older adults or those with impaired mobility.
- Assisting the client to the bathroom and providing support during toileting activities helps to prevent falls and injuries.
Choices not included:
c. Monitor calcium levels:
- There is no specific indication for monitoring calcium levels with clonazepam use.
f. Have an opioid agonist at the bedside:
- Clonazepam is not indicated for pain management and does not interact significantly with opioid analgesics.Therefore,having an opioid agonist readily available is not a necessary intervention for clonazepam initiation.
Additional Considerations:
- Educate the client about the potential side effects of clonazepam,including drowsiness,dizziness,dry mouth,and cognitive changes.
- Advise the client to avoid alcohol and other CNS depressants while taking clonazepam,as this can increase the risk of sedation and respiratory depression.
- Instruct the client to take clonazepam exactly as prescribed and not to stop taking it abruptly,as this can lead to withdrawal symptoms.
- Monitor the client's sleep patterns and adjust the medication schedule if necessary.
Patient Data
What other treatments might be helpful for this client? Select all that apply.
Explanation
A) Incorrect - Phototherapy, often used to treat conditions like seasonal affective disorder (SAD) or certain skin conditions, involves exposure to specific wavelengths of light. It is not typically used as a treatment for distressing thoughts and memories related to trauma, as described in the client's situation.
B) Incorrect - Lithium is primarily used to treat bipolar disorder and is not a first-line treatment for trauma-related symptoms or acute stress disorder. The client's symptoms are more indicative of trauma-related distress, which would be addressed through psychotherapeutic approaches like cognitive behavioral therapy (CBT).
C) Incorrect - "Consciousness-raising" is not a recognized treatment intervention in this context.
It's important to focus on evidence-based therapeutic approaches for trauma-related symptoms, such as psychotherapy and support services.
D) Correct - Cognitive behavioral therapy (CBT) is Given the client's distressing thoughts and memories, CBT is a highly effective psychotherapy approach. It focuses on identifying and modifying negative thought patterns and behaviors associated with trauma. CBT can help the client develop healthier coping strategies.
E) Correct - Animal-assisted therapy involves interacting with trained animals to improve emotional well-being. Since the client expresses feeling unhappy and having difficulty coping, animal therapy can provide comfort, reduce stress, and promote a sense of companionship.
F) Incorrect - Electroconvulsive therapy (ECT) is a treatment primarily used for severe cases of depression or certain psychiatric conditions that are unresponsive to other treatments. It involves inducing controlled seizures to affect brain chemistry. ECT is not a first-line treatment for the client's distressing thoughts and memories following a traumatic event.
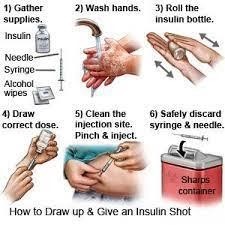
A client with a history of type 1 diabetes mellitus (DM) and asthma is readmitted to the unit for the third time in two months with a current fasting blood sugar (FBS) is 325 mg/dL (18 mmol/L). The client describes to the nurse of not understanding why the blood glucose level continues to be out of control. Which intervention(s) should the nurse implement? (Select all that apply.)
Reference Range
Blood Glucose [74 to 106 mg/dL (4.1 to 5.9 mmol/L)]
Explanation
A) Correct - Demonstrating the technique used to monitor blood glucose levels is crucial.
Incorrect technique can lead to inaccurate readings, impacting insulin dosing decisions and blood sugar control.
B) Correct - Some asthma medications, like corticosteroids, can elevate blood glucose levels.
Evaluating the client's asthma medications is essential as they can contribute to fluctuations in blood sugar levels.
C) Incorrect- Asking the client if they want a different manufacturer's glucose monitoring device is not helpful, because it does not address the underlying causes of the poor glycemic control. The client may also perceive this as a lack of confidence in their ability to manage their diabetes or as a criticism of their choice of device. The nurse should focus on educating the client on how to use their current device correctly and consistently, rather than suggesting a change that may not be necessary or feasible.
D) Correct - Understanding the client's daily routine helps identify factors influencing blood glucose control, such as meal timing, activity level, and stress. This information aids in creating a personalized diabetes management plan.
E) Correct - Ensuring the client uses a new insulin needle for each administration is important for preventing infection and complications. Reusing needles can affect injection site health and insulin absorption.
A client who weighs 65 kg receives a prescription for lorazepam 44 mcg/kg intravenously to be administered 20 minutes before a scheduled procedure. The medication is available in 2 mg/mL vial. How many mL should the nurse administer? (Enter numerical value only. If rounding is required, round to the nearest tenth.)
Explanation
Calculate the total dosage required: 44 mcg/kg * 65 kg = 2860 mcg. Convert mcg to mg: 2860 mcg ÷ 1000 = 2.86 mg.
Divide by concentration: 2.86 mg ÷ 2 mg/mL = 1.43 mL.
Considering the vial contains 2 mg/mL, the nurse should administer around 1.43 mL, which can be rounded to 1.4 mL.
A client with leukemia who is receiving myelosuppressive chemotherapy has a platelet count of 25,000/mm3 (25 x 109/L). Which intervention is most important for the nurse to include in this client's plan of care?
Reference Range:
Platelet Count [150,000 to 400,000/mm3 (156 400 x 109/L)]
Explanation
A) Correct- With a significantly low platelet count, the risk of bleeding is elevated. Assessing urine and stool for occult (hidden) blood is important to detect any signs of internal bleeding that may not be immediately apparent. A low platelet count increases the risk of spontaneous bleeding, which can be life-threatening if undetected.
B) Incorrect- This choice is related to neutropenia, not thrombocytopenia. Neutropenia, or low neutrophil count, increases the risk of infection, which is why monitoring temperature frequently is important.
C) Incorrect- Monitoring for signs of activity intolerance is not directly related to the low platelet count. The primary concern with thrombocytopenia is the risk of bleeding, not generalized activity intolerance.
D) Incorrect- Requiring visitors to wear respiratory masks is not relevant to the client's current condition of low platelet count. This action is related to infection control and protection from respiratory infections.
An infant who weighs 22 pounds receives a prescription for amoxicillin 20 mg/kg/day by mouth in divided doses every 8 hours. The bottle is labeled, "Amoxicillin for Oral Suspension, USP 250 mg per 5 mL." How many mL should the nurse administer with each dose? (Enter numerical value only. If rounding is necessary, round to the nearest tenth.)
Explanation
1. Convert the infant's weight from pounds to kilograms. We can use the conversion factor 1 kg
= 2.2 lb. So, 22 lb x (1 kg / 2.2 lb) = 10 kg.
2. Calculate the total daily dose of amoxicillin for the infant. We can use the formula D = d x W, where D is the total daily dose, d is the dose per kg per day, and W is the weight in kg. So, D = 20 mg x 10 kg = 200 mg.
3. Calculate the single dose of amoxicillin for the infant. We can divide the total daily dose by the number of doses per day. Since the prescription is for every 8 hours, there are 3 doses per day. So, 200 mg / 3 = 66.67 mg.
4. Calculate the volume of amoxicillin suspension for the single dose. We can use the ratio of the concentration of the suspension, which is 250 mg per 5 mL. So, 66.67 mg x (5 mL / 250 mg) =
1.33 mL.
5. Round the volume to the nearest tenth= 1.3 mL
An older client is taken to the clinic by the spouse, who appears extremely worried. The spouse reports to the nurse that the client started to not make any sense and asked to visit a brother who has been dead for many years. Which action(s) should the nurse take? (Select all that apply.)
Explanation
The correct answer/s is Choice/s A, C, and E.
Choice A rationale: Obtaining the client’s tympanic temperature measurement is a crucial step. The client’s confusion and disorientation could be symptoms of an infection, such as a urinary tract infection or pneumonia. Infections in older adults can often present with atypical symptoms, including changes in mental status. Therefore, checking the client’s temperature can help identify if the client has a fever, which is a common sign of an infection.
Choice B rationale: While it’s always important to be aware of a client’s allergies, especially when administering medications, it doesn’t directly address the immediate concern of the client’s altered mental status. Therefore, it’s not the most appropriate action to take in response to the situation described.
Choice C rationale: Asking if the client is experiencing any pain with urination is relevant because urinary tract infections (UTIs) are common in older adults and can cause confusion and other changes in mental status. Pain during urination is a common symptom of a UTI.
Choice D rationale: Encouraging the intake of high protein foods is generally a good recommendation for older adults to maintain their strength and energy levels. However, it’s not directly related to the client’s current symptoms of confusion and disorientation.
Choice E rationale: Determining if the client has recently experienced a fall is important. Falls in older adults can lead to injuries, such as a head injury, which can cause confusion and other changes in mental status. Additionally, some medications used to treat pain after a fall can also contribute to confusion.
The nurse is triaging several children as they present to the emergency room after a school bus accident. Which child requires the most immediate intervention by the nurse?
Explanation
A. A 12-year-old reporting neck, arm, and lower back discomfort:
- This child is reporting discomfort, which is concerning, but it doesn't indicate an immediate life-threatening condition. However, a thorough assessment is needed to rule out any serious injuries, especially to the spine.
B. An 8-year-old with a full leg air splint for a possible broken tibia:
- While a possible broken tibia requires attention, it is not as immediately critical as symptoms such as projectile vomiting. Splinting can help stabilize the limb, but it is not an emergency that requires immediate attention compared to potential neurological issues.
C. A 6-year-old with multiple superficial lacerations of all extremities:
- Superficial lacerations, although they require care, are generally not immediately life-threatening. The child needs appropriate wound care and assessment for any deeper injuries, but this can be addressed in a timely manner without immediate urgency.
D. An 11-year-old with a headache, nausea, and projectile vomiting:
- This is the most concerning presentation among the options. Headache, nausea, and projectile vomiting could be indicative of a severe head injury, and these neurological symptoms require urgent evaluation to assess for conditions such as a concussion, intracranial bleed, or increased intracranial pressure.
When the parents of a 6-year-old boy with a brain tumor are told that his condition is terminal, the mother shouts at the father, "This is your fault! It never would have happened if we had sought treatment sooner!" Which intervention is best for the nurse to implement?
Explanation
The best intervention for the nurse to implement in this scenario isd. Explain to the parents that anger is a common response to grief. This answer is based on the following rationale:
- Anger is one of the stages of grief that people may experience when they face a loss or a threat of loss12.It is a normal and healthy emotion that helps people cope with their pain and frustration3.
- Explaining to the parents that anger is a common response to grief can help them understand their own feelings and reactions, as well as those of their spouse.It can also help them avoid blaming themselves or each other for something that is not their fault4.
- The nurse should also provide the parents with empathy, support, and resources to help them cope with their grief and loss, such as individual counseling, support groups, or spiritual care124.
- The other options are not the best interventions for the nurse to implement because:
- a. Refer the parents to the chaplain to provide grief counseling. This option may be helpful for some parents who have religious or spiritual beliefs, but it may not be appropriate for others who do not share the same faith or worldview.The nurse should respect the parents’ preferences and values and not impose their own beliefs on them4.
- b. Tell the parents that blaming each other will not change the situation. This option may sound harsh and insensitive to the parents who are in emotional distress.It may also make them feel guilty or defensive, which can worsen their relationship and their coping ability4.
- c. Assure the parents that a terminal diagnosis is inevitable. This option may be factual, but it may not be helpful or comforting to the parents who are grieving.It may also make them feel hopeless or helpless, which can affect their mental and physical health
When the nurse enters the room of a male client who was admitted for a fractured femur, his cardiac monitor displays a normal sinus rhythm (NSR), but he has no spontaneous respirations and his carotid pulse is not palpable. Which intervention should the nurse implement?
Explanation
A) Incorrect- Observing for swelling at the fracture site is important for assessing the client's musculoskeletal condition, but it is not the priority intervention in this situation. The absence of spontaneous respirations and palpable carotid pulse indicates cardiac arrest, and immediate intervention is needed.
B) Incorrect- Analyzing the cardiac rhythm in another lead is not the first priority when the client is in cardiac arrest. Cardiopulmonary resuscitation (CPR) should be initiated immediately to restore circulation.
C) Incorrect- Obtaining a 12-lead electrocardiogram is not the initial intervention in a client in cardiac arrest. CPR and defibrillation (if indicated) are the immediate actions to provide circulation and oxygenation to the vital organs.
D) Correct- The absence of spontaneous respirations and palpable carotid pulse indicates cardiac arrest. In this situation, immediate initiation of cardiopulmonary resuscitation (CPR) is critical to provide circulation and oxygenation to the vital organs. Chest compressions are the initial step to address cardiac arrest and ensure blood flow to the body.
Sign Up or Login to view all the 150 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

