Rn Hesi Mental Health
Total Questions : 38
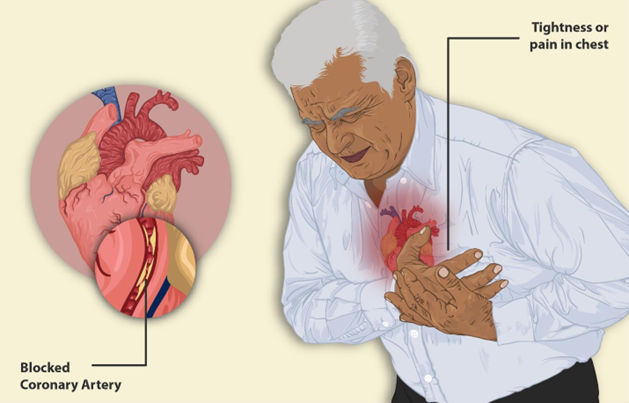
Showing 25 questions, Sign in for moreThe nurse is developing a plan of care for an older client with hypertension who reports chest pain on exertion. Which outcome should the nurse include in the plan of care for this client?
Explanation
Choice A rationale:
Weekly monitoring of blood pressure and symptoms is important but does not address the specific issue of chest pain on exertion.
Choice B rationale:
Encouraging daily walking is generally a good recommendation for overall health but does not address the immediate concern of chest pain.
Choice C rationale:
Taking up to 4 nitroglycerine tablets for chest pain may provide temporary relief, but this should be done under the guidance of a healthcare provider and is not a long-term outcome.
Choice D rationale:
Recording episodes of angina and self-management for one week is a specific and appropriate outcome to monitor the client's chest pain and response to interventions.
During a routine assessment at an outpatient clinic, the nurse notes that a client has abdominal obesity and a high waist-hip ratio, with a body mass index of 32 kg/m2.
Which action(s) should the nurse take in response to these findings? (Select all that apply.)
Explanation
Choice A rationale:
Measuring blood pressure in both arms can help assess for potential hypertension, which is a common concern in individuals with abdominal obesity and a high waist-hip ratio.
Choice B rationale:
Screening for a family history of diabetes mellitus is important because individuals with abdominal obesity are at increased risk for type 2 diabetes.
Choice C rationale:
Immediate transport to a medical facility is not indicated based solely on the findings of abdominal obesity, high waist-hip ratio, and elevated BMI. These findings may indicate an increased risk for certain health conditions, but they do not necessitate emergency transport.
Choice D rationale:
Restricting fluids and elevating feet is not a standard intervention based solely on the findings described. This action would be more relevant in specific medical situations, such as managing edema.
Choice E rationale:
Discussing the importance of a regular exercise program is appropriate because it can help address obesity and its associated health risks, including diabetes and hypertension.
Patient Data
History and Physical Laboratory Results
Flow Sheet
Laboratory Test
Result
Glucose
75 mg/dL (4.2 mmol/L)
Reference Range
74 to 106 mg/dim (4.1 to 5.9 mmol/L)
Click to highlight the assessment findings that require Immediate follow-up by the nurse.
The client is a 68-year-old with a history of diabetes, hypertension (HTN), coronary artery disease (CAD), and was recently diagnosed with end-stage renal disease (ERSD). She has been placed on hemodialysis three times a week for one month.
She presents to the emergency department (ED) with fatigue, generalized weakness, muscle cramps, tingling sensation in her arms and legs, and lightheadedness following 3 days of illness during which her husband reports she has complained of nausea and had a poor appetite and was not able to go for her scheduled dialysis 2
Initial vital signs: BP 146/82 mmHg, HR 114 bpm, RR 18 bpm, SpO, 98% on room air, temperature 98.2 °F (36.8 °C) orally.
Explanation
The assessment findings that require immediate follow-up by the nurse are muscle cramps, tingling sensation in arms and legs, and lightheadedness. These are signs of electrolyte imbalance, which can be caused by missed dialysis sessions, dehydration, or infection. Electrolyte imbalance can lead to serious complications such as cardiac arrhythmias, seizures, or coma. The nurse should monitor the client's vital signs, neurological status, and cardiac rhythm, and notify the physician for further orders. The nurse should also assess the client's fluid status, hydration, and nutritional intake, and provide education on the importance of adhering to the dialysis schedule and dietary restrictions.
A client is admitted to the mental health unit and sits in the corner of the day room. When the nurse begins the admission assessment interview, the client is guarded, suspicious, and resists talking.
Which action should the nurse implement?
Explanation
Choice A rationale:
Postponing the interview until the next day may not be necessary and could delay necessary assessment and care.
Choice B rationale:
Documenting the client's paranoid behavior is important but should be done after the nurse attempts to engage with the client.
Choice C rationale:
Attempting to ask the client simple questions is a non-threatening approach that allows the nurse to start the assessment and establish some rapport. It respects the client's need for space while initiating communication.
Choice D rationale:
Asking another nurse to talk with the client may be an option later if the client remains uncooperative, but the nurse should first attempt to engage with the client directly.
A young adult client with a recent diagnosis of bipolar disorder takes lithium carbonate daily. The client informed the school nurse of the desire to live away from home to attend college after graduating in one month. Which information is most important for the nurse to provide the client and his family?
Explanation
Choice A rationale:
While it's important for the client to be aware of the signs and symptoms of their illness, medication monitoring is a more immediate concern.
Choice B rationale:
Participating in therapy can be beneficial, but it's not the most critical information to provide in this context.
Choice C rationale:
Living away from home is possible for many individuals with bipolar disorder, but medication management is a higher priority.
Choice D rationale:
Routine monitoring of serum lithium levels is crucial to ensure therapeutic levels and prevent lithium toxicity in individuals taking lithium carbonate for bipolar disorder.
A preschool-aged girl tells the school nurse that her hair hurts. The nurse finds that the child's hair has been arranged to cover several small bald spots. Which finding indicates to the nurse that the hair loss is not disease-related?
Explanation
Choice A Rationale:
Ecchymotic blood accumulations (bruises) are indicative of possible trauma or injury to the scalp. In this case, it suggests that the hair loss is likely due to physical manipulation (such as pulling or arranging the hair to cover bald spots) rather than a medical condition.
Choice B rationale:
This choice suggests that evidence of patches of lost hair would be indicative of non-disease-related hair loss. However, this is not necessarily true. Medical conditions, such as alopecia areata, can also cause patchy hair loss without physical trauma. Therefore, it is not a definitive indicator that hair loss is not disease-related.
Choice C rationale:
Episodic complaints of pruritus (itching) could be associated with various scalp conditions, including those that lead to hair loss. Itching alone does not rule out disease-related hair loss. In fact, some medical conditions can cause both itching and hair loss.
Choice D rationale:
Erythema (redness) of localized lesions may suggest inflammation but does not necessarily indicate non-disease-related hair loss. Medical conditions can also cause localized inflammation and hair loss.
A client with depression does not want to communicate with friends, uses television watching as a means of escaping responsibilities, and describes the inability to handle personal circumstances. Which coping strategy should the nurse include in the plan of care?
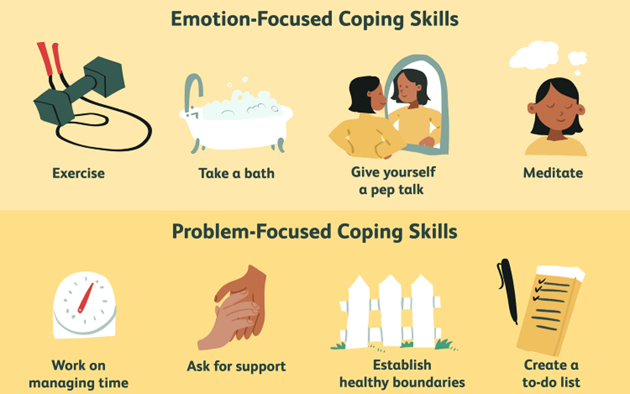
Explanation
Choice A Rationale:
While emotional expression and ventilation can be therapeutic, it may not be the most appropriate coping strategy for someone with depression who may already be overwhelmed by negative emotions. Ventilating emotions without a structured approach might not provide the desired relief and can even exacerbate feelings of distress.
Choice B Rationale:
This choice may not be suitable for someone with depression because it could lead to further neglect of their own needs and contribute to feelings of guilt or exhaustion.
Choice C Rationale:
While relaxation techniques can be helpful, reducing the effort to solve problems may not be the most effective strategy for individuals with depression. Avoidance of problems can perpetuate feelings of helplessness and hopelessness.
Choice D Rationale:
For a client with depression who is struggling with handling personal circumstances, focusing on small achievable tasks can be a helpful coping strategy. Breaking down larger problems into manageable steps can reduce feelings of overwhelm and gradually improve the client's sense of accomplishment and self-efficacy.
Prior to initiating a treatment regimen with the antidepressant sertraline, it is most important for the nurse to obtain which information?
Explanation
Choice A rationale:
It is crucial to obtain information about any history of heart disease before starting an antidepressant-like sertraline because certain antidepressants can have effects on the heart's electrical conduction system. Sertraline, in particular, may be associated with QT interval prolongation, and individuals with a history of heart disease may be at higher risk. Assessing this history helps the nurse make informed decisions about the client's treatment and potential risks.
Choice B rationale:
While a familial history of mental illness is important to consider, it is not the most critical information to obtain before starting sertraline. The primary concern with sertraline is its potential impact on the heart's electrical conduction system, making option A (heart disease history) more relevant.
Choice C rationale:
Current weight is essential to monitor during treatment with sertraline as it can impact dosing, but it is not the most critical piece of information to obtain before starting the medication.
Choice D rationale:
Medication history is important but not the most critical information in this context. Assessing any history of heart disease (Option A) takes precedence due to the specific cardiovascular risks associated with sertraline.
The nurse is assessing a client who reports using cocaine several times in the past week. Which observations should the nurse expect on assessment?
Explanation
Choice A rationale:
Cocaine is a stimulant and typically leads to increased heart rate (tachycardia) and respiratory rate (tachypnea). Bradycardia (slow heart rate) and bradypnea (slow respiratory rate) would be atypical findings with cocaine use.
Choice B rationale:
Cocaine is a stimulant drug that typically produces effects such as increased heart rate, increased blood pressure, stimulation, euphoria, and dilated pupils. These physiological and psychological effects are common when someone has used cocaine.
Choice C rationale:
While cocaine use can cause hallucinations and paranoia during intoxication or withdrawal, these symptoms are not typically the primary manifestations. The most common initial effects are stimulation and increased alertness.
Hallucinations and delusions may occur with substance use, but they are not the most expected or specific findings for cocaine use.
Choice D rationale:
Cocaine use is associated with increased energy, euphoria, and heightened arousal. Lethargy and depression are more likely during the comedown phase or withdrawal from cocaine, rather than immediately after use.
Patient Data
Laboratory Results
Flow Sheet
The nurse is reviewing the history and physical.
Choose the most likely options for the information missing from the statement below by selecting from the list of options provided.
Based on the client's subjective and objectives data, the nurse recognizes that she is having signs and symptoms of a_______
Explanation
Choice A rationale:
Sinus tachycardia is not a cause, but a consequence of hyperkalemia.
Choice B rationale:
The client has a history of diabetes, hypertension, coronary artery disease, and end-stage renal disease, which are all risk factors for developing hyperkalemia (high levels of potassium in the blood). She also missed her scheduled dialysis session, which could have caused a buildup of potassium in her blood. Some of the signs and symptoms of hyperkalemia include fatigue, weakness, muscle cramps, tingling sensation in arms and legs, and cardiac arrhythmias such as sinus tachycardia (a fast heart rate). The other options are not consistent with the client's data or condition.
Choice C rationale:
Hypermagnesemia can also cause muscle weakness and cardiac arrhythmias, but they are less likely in this scenario since magnesium is not affected by dialysis
Choice D rationale:
Hypokalemia can also cause muscle weakness and cardiac arrhythmias, but they is less likely in this scenario since potassium is usually elevated in ESRD.
Patient Data
The nurse is reviewing the physician's orders.
Which of the following physician's orders requires priority attention from the nurse?
Select all that apply.
Explanation
Choice A rationale:
This order is useful to evaluate the client's electrolyte levels, renal function, and acid-base balance, as she has ERSD and missed her dialysis session. She may have hyperkalemia, metabolic acidosis, or uremia, which can affect her cardiac and neurological status.
Choice B rationale:
This order is helpful to assess the client's cardiac structure and function, as she has a history of CAD and HTN and may have developed heart failure or valvular disease.
Choice C rationale:
This order is beneficial to rule out any intra-abdominal causes of the client's nausea and poor appetite, such as infection, obstruction, or bleeding.
Choice D rationale:
This order is necessary to identify any possible source of infection or sepsis, as the client has been ill for 3 days and has a history of diabetes, which can impair her immune system.
Choice E rationale:
This order is important to assess the client's cardiac and pulmonary status, as she has a history of CAD and is presenting with chest discomfort and lightheadedness, which could indicate a cardiac event or pulmonary edema.
Choice F rationale:
This order is essential to monitor the client's heart rate and rhythm, as she has a history of CAD and HTN and is at risk for arrhythmias, ischemia, and infarction.
Choice G rationale:
This order is important to evaluate the client's hematological status, as she has ERSD and may have anemia, leukocytosis, or thrombocytopenia.
Choice H rationale:
This order is crucial to obtain a baseline of the client's cardiac electrical activity and to detect any signs of acute coronary syndrome, such as ST-segment elevation or depression, T wave inversion, or Q waves.
Patient Data
History and Physical
The client is a 68-year-old with a history of diabetes, hypertension (HTN), coronary artery disease (CAD), and was recently diagnosed with end-stage renal disease (ERSD). She has been placed on hemodialysis three times a week for one month. She presents to the emergency department (ED) with fatigue, generalized weakness, muscle cramps, tingling sensation in arms and legs, and lightheadedness following 3 days of illness during which her husband reports she has complained of nausea and had a poor
appetite and not able to go for her scheduled dialysis 2
Initial vital signs: BP 146/82 mmHg, HR 114 bpm, RR 18 bpm, SpO, 98% on room air, temperature 98.2 °F (36.8 °C) orally.
Nurses' Notes Laboratory Results Imaging Studies
Chest X-ray: no acute disease
CT of Abdomen: no acute disease Flow Sheet
The nurse determines the plan of care.
For each action, click to indicate whether they would be included or not included in the plan of care for the client.
Each row must have only one response option selected.
Actions
Explanation
Choice A rationale:
This is included because the client has a history of cardiovascular issues (hypertension, coronary artery disease), and the symptoms presented (fatigue, muscle cramps, tingling sensation, lightheadedness) could be related to cardiac concerns. Monitoring cardiac status helps assess for any cardiac-related issues.
Choice B rationale:
This is essential because the client's recent illness and missed dialysis sessions may have contributed to her symptoms. Ensuring the client understands the importance of compliance with hemodialysis is crucial for her overall well-being.
Choice C rationale:
Monitoring vital signs, including blood pressure, heart rate, and respiratory rate, is a fundamental aspect of assessing the client's current condition and response to treatment.
Choice D rationale:
A comprehensive head-to-toe assessment helps identify any physical signs or symptoms that may be contributing to the client's complaints and guides further evaluation and interventions.
Choice E rationale:
Given the client's history of cardiovascular disease and the complaints of chest discomfort, monitoring the heart rhythm is essential to assess for any arrhythmias or irregularities.
Choice F rationale:
Monitoring fluid intake and output is crucial, especially in clients with end-stage renal disease, as imbalances in fluid and electrolytes can exacerbate symptoms and lead to complications.
Choice G rationale:
The client's complaints of muscle cramps and tingling sensations in the arms and legs indicate potential neuromuscular involvement. Monitoring neuromuscular status helps assess these symptoms.
Choice H rationale:
There is no indication in the provided information that an immediate transfer to a telemetry unit is necessary. The client's vital signs, including heart rate and oxygen saturation, are stable at the moment. Further assessment and interventions can be carried out on the current unit before considering a transfer.
Choice I rationale:
Given the client's history of end-stage renal disease and the symptoms presented, educating her to avoid a high-potassium diet is important. High potassium levels can lead to symptoms like muscle cramps and tingling sensations, which the client is experiencing.
Patient Data
On further assessment, the client reports that her doctor A had recently started her on Lisinopril for blood pressure control but it "doesn't seem to help". She then complained of some chest discomfort. The client is moved to an ED room, and another set of vital signs is performed. Physician notified and orders received.
ECG monitor shows a slight peaked T-wave.
What treatments should the nurse anticipate for the client at this time? Select all that apply.
Explanation
Choice A rationale:
This is not a priority action for the nurse at this time. The nurse should first implement the ordered treatments for hyperkalemia and stabilize the client's condition before calling and giving a report to the receiving unit.
Choice B rationale:
Loop diuretics are medications that increase urine output and can lower potassium levels in mild cases of hyperkalemia. However, they are contraindicated in patients with ERSD who have oliguria or anuria (reduced or absent urine production). Loop diuretics can worsen renal function and fluid overload in these patients.
Choice C rationale:
Scheduling the client for hemodialysis is crucial, especially if the client has missed a scheduled dialysis session. Hemodialysis can help manage electrolyte imbalances and fluid overload.
Choice D rationale:
Checking the blood glucose level is important, especially in a client with a history of diabetes. Maintaining glycemic control is essential for overall health.
Choice E rationale:
Drawing a repeat potassium level is necessary to monitor the client's electrolyte status, especially given the ECG changes.
Choice F rationale:
Holding Lisinopril, an ACE inhibitor, is appropriate in this context, considering the client's elevated blood pressure and potential renal issues. It should be done under the guidance of the healthcare provider.
Choice G rationale:
Administering insulin, dextrose, and calcium gluconate can help manage hyperkalemia, which may be indicated by the ECG changes. Repeating the 12-lead EKG is important to assess the response to treatment and any changes in cardiac rhythm.
Patient Data
History and Physical Laboratory Results
The client is a 68-year-old with a history of diabetes, hypertension (HTN), coronary artery disease (CAD), and was recently diagnosed with end-stage renal disease (ERSD). She has been placed on hemodialysis three times a week for one month. She presents to the emergency department (ED) with fatigue, generalized weakness, muscle cramps, tingling sensation in her arms and legs, and lightheadedness following 3 days of Illness during which her husband reports she has complained of nausea and had a poor appetite and not able to go for her scheduled dialysis 2
On further assessment, the client reports that her doctor had recently started her on Lisinopril for blood pressure control but it "doesn't seem to help". She then complained of some chest discomfort. The client is moved to an ED room and another set of vital signs is performed. Physician notified and orders received.
Laboratory Test
Glucose Result
75 mg/dL (4.2 mmol/L)
Reference Range
74 to 106 mg/dL (4.1 to 5.9 mmol/L)
Nurses' Notes
Flow Sheet Orders
Imaging Studies
12 lead EKG
. CBC
Basic metabolic panel
. Chest X-ray
. Place on a continuous cardiac monitor
. CT scan of abdomen Blood cultures times 2 sets
- Echocardiogram
Initial vital signs: BP 146/82 mm Hg, heart rate 114 beats/minute, respiratory rate 18 breaths/minute, Spo, 98% on room air, temperature 98.2 °F (36.8 °C) orally.
Vital signs: BP 156/88 mm Hg, heart rate 116 beats/minute, respiratory rate 22 breaths/minute, Spo2 98% on room air, temperature 98.0 °F (36.7 °C) orally.
The client has been in IMU unit for 3 days and the physician plans to discharge her home today.
For each assessment finding, click to indicate whether the actions taken were effective or ineffective.
Each row must have only one response option selected.
Client Findings
Explanation
Choice A rationale:
This finding suggests that the client may not be fully disclosing her symptoms or may not be aware of their significance. It should be investigated further.
Choice B rationale:
The blood pressure and heart rate are within an acceptable range, indicating that the client's blood pressure is relatively stable.
Choice C rationale:
A potassium level of 3.6 mEq/L falls within the reference range, indicating that the client's potassium level is within normal limits.
Choice D rationale:
The client's commitment to attending dialysis appointments is a positive sign, as regular dialysis is crucial for managing end-stage renal disease.
Choice E rationale:
If the client recognizes the need to resume her Lisinopril for blood pressure control, it indicates her understanding of the medication's importance in managing her hypertension.
Choice F rationale:
The client's willingness to incorporate nutrient-rich foods like dark green vegetables and potatoes into her diet is a positive sign for improving her nutritional status, which can be beneficial for her overall health. However, dietary changes should be discussed with her healthcare provider to ensure they are appropriate for her condition.
The nurse is teaching a client with cancer about skincare for the portal site receiving external beam radiation. Which client action regarding skin care indicates a need for further teaching?

Explanation
Choice A rationale:
Applying prescribed lotions to the radiation site is generally a recommended part of skin care during radiation therapy, as it helps keep the skin moisturized and reduces irritation.
Choice B rationale:
Washing the radiation site with antibacterial soap and water is not recommended. Clients undergoing radiation therapy are typically advised to use gentle, mild soaps and to avoid scrubbing or using harsh cleansers on the treated area. Antibacterial soap may be too harsh and could lead to skin irritation.
Choice C rationale:
Wearing clothing to cover the radiation site is a good practice to protect the area from sun exposure and potential irritation.
Choice D rationale:
Drying the area with patting motions after taking a shower is the correct way to dry the radiation site, as it minimizes friction and reduces the risk of skin damage.
The nurse is providing dietary instructions for a client who is being discharged after passing a calcium oxalate renal stone. Which food should the nurse instruct the client to avoid?
Explanation
Choice A rationale:
Sweet potatoes are not typically high in oxalates and are generally considered safe to consume in moderation for individuals with calcium oxalate renal stones.
Choice B rationale:
Spinach is high in oxalates, which can contribute to the formation of calcium oxalate renal stones. Therefore, the client should be instructed to avoid spinach and foods high in oxalates.
Choice C rationale:
Bananas are generally low in oxalates and are not likely to be a significant contributor to the formation of calcium oxalate renal stones. They are safe for most individuals to consume.
Choice D rationale:
Fish is generally not high in oxalates and is not a major concern for individuals with calcium oxalate renal stones. However, it's essential to maintain an overall balanced diet and stay hydrated to prevent stone formation.
A client with benign prostatic hyperplasia (BPH) is preparing for discharge following a transurethral needle ablation (TUNA). Which information should the nurse include in the discharge instructions?
Explanation
Choice A rationale:
Using an incentive spirometer is not directly related to the post-TUNA discharge instructions for a client with BPH. Incentive spirometry is typically used to improve lung function and prevent respiratory complications.
Choice B rationale:
Monitoring the urinary stream for a decrease in output may be important, but it is a general instruction that may not be specific to the TUNA procedure. The primary focus after TUNA is often on monitoring for complications related to the procedure.
Choice C rationale:
Reporting when hematuria (blood in the urine) becomes pink-tinged is important. While some degree of hematuria is expected after TUNA, a change in color to pink or any other concerning changes should be reported to the healthcare provider as it could indicate complications.
Choice D rationale:
There is typically no need to restrict physical activities after a TUNA procedure. In fact, healthcare providers often encourage patients to resume normal activities gradually unless otherwise instructed due to specific complications.
Patient Data
History and Physical
What nursing interventions are appropriate for the client starting clonazepam? Select all that apply.
Explanation
Choice A rationale:
Clonazepam is not typically associated with a significant risk of causing urinary retention or frequent bathroom needs. There's no immediate need for bathroom assistance related to clonazepam use.
Choice B rationale:
Clonazepam is a medication that affects the central nervous system and can influence mental status. Regular assessment helps monitor for any changes or adverse effects.
Choice C rationale:
Clonazepam is administered orally, and it's important to ensure the client's oral health and comfort, especially since dry mouth can be a side effect.
Choice D rationale:
Clonazepam can cause drowsiness and potential changes in blood pressure, which could lead to orthostatic hypotension. Screening for this condition helps ensure the client's safety when changing positions.
Choice E rationale:
Clonazepam does not typically affect calcium levels. Monitoring calcium levels is not a standard nursing intervention when starting clonazepam.
Choice F rationale:
Clonazepam is not an opioid, and it does not require having an opioid agonist at the bedside. This intervention is not relevant to clonazepam use.
Patient Data
History and Physical
The client is in the hospital after her house collapsed during a hurricane. She has been in the intensive care unit for 2 weeks and moved today to the surgical floor to continue monitoring her respiratory function and to complete intravenous antibiotic administration. Nurses Notes
Orders 0900
Orders
Pain assessment completed. The client's pain is 2/10. The client requests sleeping medication for the night. She states that she has horrible thoughts and memories about the house collapsing all the time and that it is keeping her from falling asleep. She states, "I used to be so happy before all of this happened. Now I can't seem to get out of this funk I am in." The client would also prefer to be in a quieter area of the unit as she is currently by the nurses' station and hears talking and alarms constantly.
1115
. Start clonazepam 0.25 mg every 12 hours
For each client statement, click to highlight the statement(s) below that require follow-up teaching by the nurse.
Explanation
Choice A rationale:
This reflects a potential misunderstanding about the diagnosis and may contribute to stigma. The nurse should provide education and clarify that having acute stress disorder or similar responses to trauma does not mean the client is "crazy."
Choice B rationale:
This statement reflects a positive attitude toward therapy and self-improvement. There is no immediate need for follow-up teaching in this statement, as it aligns with the potential benefits of therapy for coping with trauma.
Choice C rationale:
This indicates the client's interest in holistic approaches, which is positive. However, the nurse should provide information and guidance on the use of such approaches in conjunction with other treatments.
Choice D rationale:
This suggests that the client may believe her response is typical. The nurse should provide education about the variability in individual responses to stress and trauma.
Choice E rationale:
This statement shows an understanding of the relationship between acute stress disorder (ASD) and post-traumatic stress disorder (PTSD). While it's true that having ASD can increase the risk of developing PTSD, this statement does not require immediate follow-up teaching. However, the client should receive ongoing education about managing and preventing PTSD
Choice F rationale:
This raises concerns about the client's expectations regarding the duration of medication. The nurse should provide information about the intended duration of medication and the importance of ongoing assessment and follow-up with healthcare providers.
The nurse is using the CAGE questionnaire as a screening tool for a client who is seeking help because his wife said he had a drinking problem. Which information should the nurse explore in-depth with the client based on this screening tool?
Explanation
Choice A rationale:
This option includes various factors but does not directly align with the CAGE questions.
Choice B rationale:
While it mentions liver enzyme and gastrointestinal complaints, it does not specifically address the CAGE questions about efforts to cut down, annoyance with questions, guilt, or using alcohol as an "Eye-opener."
Choice C rationale:
The CAGE questionnaire is designed to assess for alcohol misuse or dependency. The responses in choice C ("Efforts to cut down," "annoyance with questions," "guilt," and "drinking as an 'Eye-opener'") are the key elements of the CAGE questionnaire that indicate potential issues with alcohol use. These responses should be explored further to assess the client's relationship with alcohol and the impact it may have on their life.
Choice D rationale:
This option mentions minimizing drinking and missing family events but does not cover all the key elements of the CAGE questionnaire.
An adolescent client is admitted to the postoperative unit following open reduction of a fractured femur which occurred when the client fell down the stairs at a party. The nurse notices needle marks on the client's arms. Which assessment findings should the nurse document related to suspected narcotic withdrawal?
Explanation
Choice A rationale:
Vomiting, seizures, and loss of consciousness are more severe symptoms that are not typically associated with narcotic withdrawal but could indicate other medical issues.
Choice B rationale:
Agitation, sweating, and abdominal cramps are indicative of narcotic withdrawal. These symptoms are commonly associated with opioid withdrawal, especially when there are needle marks on the client's arms, which may suggest a history of opioid use. Opioid withdrawal symptoms can include restlessness, sweating, and gastrointestinal discomfort, such as abdominal cramps. Therefore, these findings should be documented and reported for further assessment and appropriate intervention related to narcotic withdrawal.
Choice C rationale:
Depression, fatigue, and dizziness are not specific to narcotic withdrawal and could be related to various conditions.
Choice D rationale:
Hypotension, shallow respirations, and dilated pupils may suggest opioid overdose rather than withdrawal.
A female client with bulimia is admitted to the mental health unit after she disclosed to a friend that she purges after meals. Which intervention should the nurse implement first?
Explanation
Choice A rationale:
Providing a supportive, structured environment for meals is an important aspect of the overall care plan for individuals with bulimia. However, it should not be the first intervention when a client is admitted with potential physical complications. Addressing the client's physical condition and safety is the initial priority.
Choice B rationale:
This is the correct initial intervention. Bulimia can lead to severe medical complications, including electrolyte imbalances, which can be life-threatening. Assessing the client's weight, vital signs, and electrolyte levels is crucial to determine the severity of physical issues and guide appropriate medical interventions.
Choice C rationale:
Discussing alternative strategies for binging and purging is an important aspect of treatment for bulimia, but it should follow the initial assessment of the client's physical condition. Addressing the client's medical needs takes precedence over discussing alternatives.
Choice D rationale:
While monitoring the client for possible vomiting is important in the care of individuals with bulimia, it should not be the first intervention when the client is admitted. Assessing the client's physical status and addressing potential medical complications should come before monitoring for specific behaviors.
The nurse is caring for a client who is experiencing extreme sadness after the passing of a companion of 30 years. The client describes not being able to think of other things and finds it difficult to control emotions. Which action should the nurse take first?
Explanation
Choice A rationale:
Exploring changes in life that have occurred after the loss is the first action the nurse should take. This allows the nurse to assess the client's grief, identify specific stressors, and understand how the loss is impacting the client's daily life and emotional well-being. It provides valuable information for tailoring further interventions and support.
Choice B rationale:
Suggesting the need for a psychiatric consultation may be premature as the nurse should first assess the client's grief and coping mechanisms. Referral for psychiatric consultation should be considered if the client's emotional distress is severe, persistent, or significantly impacting their functioning.
Choice C rationale:
Offering a referral to pastoral counseling may be appropriate for some clients, but it should not be the first action. The nurse should assess the client's needs and preferences before making such a referral.
Choice D rationale:
Encouraging attendance at a local support group can be beneficial, but it should not be the initial step. The nurse should first assess the client's current emotional state and needs to determine the most appropriate interventions.
A client is admitted to the hospital with suicidal ideation. When completing the health history and admission assessment interview, which client comment is most important for the nurse to document?
Explanation
Choice A rationale:
This statement expresses the client's emotional state but does not provide information about immediate access to lethal means.
Choice B rationale:
This comment is the most crucial to document because it indicates the client's access to potentially lethal means, which is a significant risk factor for committing suicide.
Choice C rationale:
This statement provides information about a source of support in the client's life but does not indicate immediate access to lethal methods.
Choice D rationale:
This statement provides information about the frequency of panic attacks but does not indicate immediate access to lethal means.
The nurse notes that a client with a history of self-mutilation has increased body tension and is pacing in the hallway. Which nursing intervention is most important at this time?
Explanation
Choice A rationale:
While completing a thorough room search to remove potential self-harming objects is important, it should follow the immediate need for monitoring and intervention.
Choice B rationale:
Providing time alone in the client's room may not be appropriate when the client is exhibiting signs of distress and increased risk.
Choice C rationale:
Closely monitoring the client and having staff intervene as needed (Choice C) is the most important intervention in this situation. Clients with a history of self-mutilation who display signs of increased tension and agitation may be at higher risk for engaging in self-harming behaviors. Close observation and intervention can help prevent self-harm and ensure the client's safety.
Choice D rationale:
Giving firm, consistent expectations is important in the overall care plan but may not be effective in acute situations where immediate monitoring and intervention are required.
Sign Up or Login to view all the 38 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

