RN HESI OB/pediatrics
Total Questions : 44
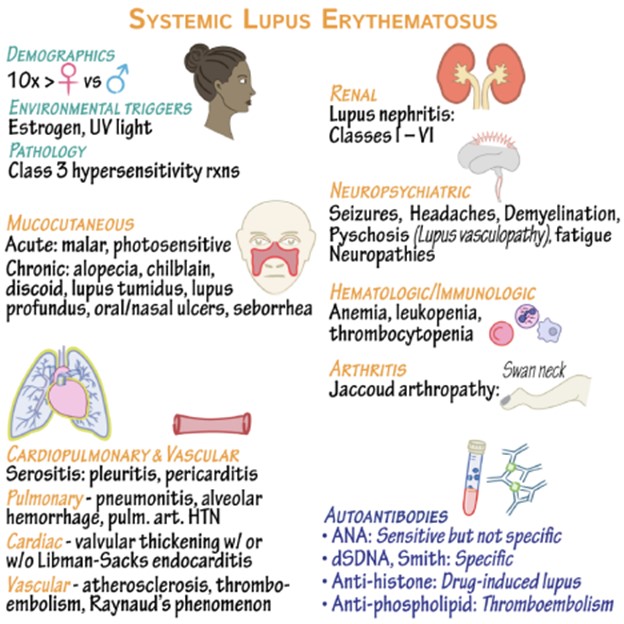
Showing 25 questions, Sign in for moreThe nurse caring for a client with systemic lupus erythematosus (SLE) would include which information in teaching about triggers that can result in an exacerbation of the disease?
Explanation
Excessive exposure to UV light, such as sunlight or tanning beds, is a known trigger for SLE exacerbations. It is important for individuals with SLE to protect their skin from the sun by wearing protective clothing, using sunscreen, and avoiding direct sunlight during peak hours. Having a family history of SLE increases the risk of developing the disease. While it is not a trigger in itself, it is an important piece of information for the client to be aware of, as it may indicate a genetic predisposition to the condition.
Acetaminophen is a commonly used over-the-counter pain reliever. While it can help manage pain associated with SLE, it is not typically considered a trigger for exacerbations. Menopause, which marks the end of a woman's reproductive years, does not directly trigger SLE exacerbations. However, hormonal changes during menopause can potentially affect disease activity in some individuals. It is important for the client to discuss any changes or concerns with their healthcare provider to manage their symptoms effectively.
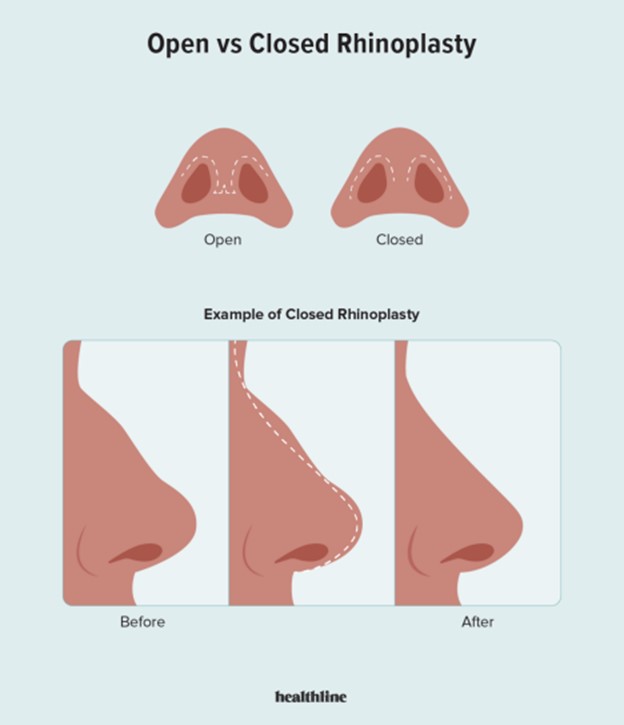
A patient, age 23, underwent a rhinoplasty 6 hours ago. After administering his pain medication, the nurse notes that he is swallowing frequently. What is the most likely cause of the swallowing?
Explanation
Rhinoplasty is a surgical procedure performed on the nose, and it often involves the placement of nasal packing to control bleeding, support the nasal structures, and promote healing. Nasal packing can cause mouth breathing and oral dryness, which can lead to increased swallowing as the patient tries to alleviate the discomfort.
While bleeding posterior to the nasal packing is a potential complication of rhinoplasty, it typically presents with other symptoms such as active bleeding, nasal discharge, or changes in vital signs. Without additional information or signs of active bleeding, it is less likely to be the cause of the patient's frequent swallowing in this scenario.
An adverse reaction to the analgesic is possible, but it would typically present with other symptoms such as allergic reactions (rash, swelling, difficulty breathing) or gastrointestinal symptoms (nausea, vomiting). In the absence of these symptoms, an adverse reaction to the analgesic is less likely.
Lastly, a normal response to the analgesic and surgery would not typically manifest as frequent swallowing. While pain medication can cause side effects, such as drowsiness or nausea, increased swallowing is not a common response.
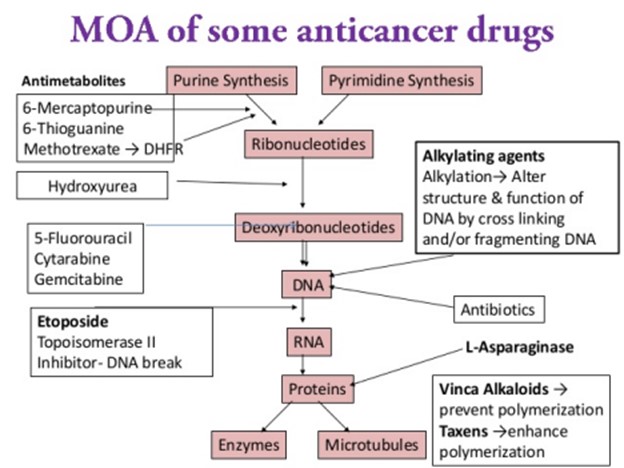
A 58-year-old man is going to have chemotherapy for lung cancer. He asks the nurse how the chemotherapeutic drugs will work.The most accurate explanation the nurse can give is which of the following?
Explanation
Chemotherapy is a treatment modality used to target and destroy rapidly dividing cells, including cancer cells. It works by interfering with the cell division process, which is a characteristic of cancer cells. However, it is important to note that chemotherapy drugs can also affect normal, healthy cells in the body that undergo rapid division, such as cells in the bone marrow, hair follicles, and gastrointestinal lining. This is why chemotherapy can be associated with side effects like bone marrow suppression, hair loss, and gastrointestinal disturbances. While the molecular structure of DNA can be altered by certain chemotherapeutic drugs, this explanation is not comprehensive enough to encompass the overall mechanism of action of chemotherapy.
The statement that "cancer cells are susceptible to drug toxins" is partially true, as cancer cells are generally more vulnerable to the cytotoxic effects of chemotherapy drugs compared to normal cells.
Chemotherapy aims to disrupt the division and growth of cancer cells rather than promoting their division.
A patient with a gastric outlet obstruction has been treated with NG decompression. After the first 24 hours, the patient develops nausea and increased upper abdominal bowel sounds. What is the best action by the nurse?
Explanation
The development of nausea and increased upper abdominal bowel sounds after 24 hours of NG decompression in a patient with gastric outlet obstruction raises concerns for possible complications or changes in the patient's condition. Assessing the patient's vital signs, including blood pressure, heart rate, respiratory rate, and oxygen saturation, can provide important information about their circulatory status and overall stability.
While checking the patency of the NG tube is important, it is not the best immediate action in this situation. The nurse should first assess the patient's vital signs to ensure their stability before proceeding with further interventions.
Placing the patient in a recumbent position (lying down) or encouraging deep breathing and conscious relaxation may not address the underlying issue and could potentially exacerbate the symptoms. It is essential to assess the patient's vital signs and circulatory status to determine the appropriate course of action.
A client with systemic lupus erythematosus (SLE) is receiving nonsteroidal anti- inflammatory drug (NSAID) therapy. Which side effect of NSAID therapy should the nurse immediately report to the health care provider?
Explanation
Pancytopenia refers to a decrease in all three major blood cell types: red blood cells (anemia), white blood cells (leukopenia), and platelets (thrombocytopenia). It is a potentially serious side effect that can lead to increased susceptibility to infections, anemia-related symptoms (fatigue, weakness), and an increased risk of bleeding. Prompt reporting is necessary for further
evaluation and appropriate management.
While melena (dark, tarry stools) is a concerning side effect, it typically indicates gastrointestinal bleeding, which should also be reported promptly but may not require immediate action unless the bleeding is severe or accompanied by other symptoms.
Decreased vision can be a side effect of certain medications, including NSAIDs, but it does not usually require immediate reporting unless it is severe or rapidly progressive. Hyperglycemia (high blood sugar) can occur with NSAID therapy, especially in individuals with preexisting diabetes or impaired glucose tolerance. While it should be monitored and managed appropriately, it does not typically require immediate reporting unless it is extremely high or associated with other concerning symptoms.
The nurse determines that teaching for the patient with peptic ulcer disease has been effective when the patient makes which statement?
Explanation
Effective teaching for a patient with peptic ulcer disease focuses on promoting understanding and adherence to the treatment plan, as well as addressing lifestyle modifications that can help manage the condition. Stress reduction is an important aspect of ulcer management, as stress
can exacerbate symptoms and delay healing. If the patient acknowledges learning relaxation strategies that decrease their stress, it indicates that they have grasped the concept and are likely to implement it in their daily life.
It is crucial for the patient to understand that any potential side effects should be reported to the healthcare provider, who will then determine the appropriate course of action. Abruptly stopping medications without medical guidance can have adverse consequences. While pain relief is an important goal, the treatment for peptic ulcer disease typically involves addressing the underlying cause, such as Helicobacter pylori infection or reducing stomach acid production. The patient should follow the treatment regimen as prescribed by the healthcare provider, even if they experience pain relief, to ensure proper healing and prevent ulcer recurrence.
Different antacids have different formulations and ingredients, and they may vary in terms of effectiveness and duration of action. It is important for the patient to consult with their healthcare provider or pharmacist to determine which antacid is most suitable for their specific needs.
The nurse is caring for a patient with COPD. Which intervention could be delegated to unlicensed assistive personnel (UAP)?
Explanation
Assisting the patient to get out of bed is a task that can be safely delegated to UAP, as long as the patient's mobility and transfer status allow for assistance without the need for specialized nursing skills. UAPs are trained to provide basic patient care, including assisting with activities of daily living, under the supervision and direction of licensed healthcare professionals.
Teaching the patient to purse lip breath requires knowledge and understanding of the technique, as well as the ability to assess the patient's response and provide feedback. This is best done by a licensed healthcare professional, such as a nurse or respiratory therapist. Auscultating breath sounds every 4 hours requires the ability to correctly use a stethoscope and interpret the findings. This task falls within the scope of practice of a nurse or respiratory therapist who has received appropriate training.
Planning patient activities to minimize exertion requires knowledge of the patient's condition, limitations, and goals. It involves assessment, evaluation, and coordination of care, which are typically performed by licensed healthcare professionals.
Which medication should the nurse anticipate being used first in the emergency department for relief of severe respiratory distress related to asthma?
Explanation
Albuterol is a short-acting beta-agonist bronchodilator that provides rapid relief of bronchospasm and helps to alleviate the symptoms of respiratory distress in asthma. It acts quickly to relax the smooth muscles in the airways, improving airflow and relieving wheezing, coughing, and shortness of breath. In an acute asthma exacerbation, albuterol is often the first-line medication used to provide immediate relief and improve respiratory function. Prednisone is an oral corticosteroid that has anti-inflammatory effects and is commonly used in the treatment of asthma. However, it is typically administered orally and takes time to exert its effects. In the emergency department setting, the focus is on providing immediate relief of symptoms, and oral medications like prednisone may not have an immediate effect. Ipratropium is an anticholinergic bronchodilator that can be administered via inhalation. While it is effective in relieving bronchospasm, it is generally used as an adjunct to albuterol and not typically the first-line medication for severe respiratory distress in asthma. Fluticasone is an inhaled corticosteroid that has anti-inflammatory effects and is used for long-term management and control of asthma. It is not appropriate for immediate relief of severe respiratory distress and is not typically used as a first-line medication in the emergency department.
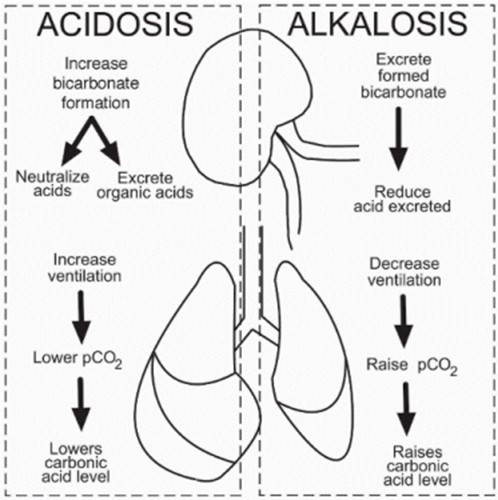
Colleen, a 19 year old Freshman, was drinking alcohol at a frat party. She stupors, falls and hits her head on the ground. Her friend Julie dials "911" because Colleen is now unconscious, depressed ventilation (shallow and slow respirations), rapid heart rate, and is profusely bleeding from both ears. Which primary acid-base imbalance is Colleen at risk for if medical attention is not provided?
Explanation
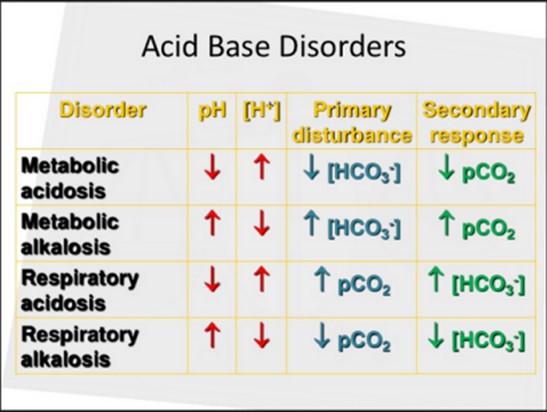
Respiratory acidosis is a primary acid-base imbalance that occurs when there is an excess of carbon dioxide (CO2) in the body due to impaired ventilation or inadequate removal of CO2 from the lungs. In this case, Colleen's depressed ventilation, indicated by shallow and slow respirations, can lead to inadequate elimination of CO2 from her body. The excessive CO2 levels can result in an accumulation of carbonic acid (H2CO3) in the blood, leading to an increase in acidity and a decrease in pH.
The profuse bleeding from both ears indicates a potential head injury, which can lead to decreased neurological function and impaired control over the respiratory center in the brain. This can further contribute to depressed ventilation and the development of respiratory acidosis. Metabolic acidosis, characterized by a decrease in bicarbonate (HCO3-) levels or an increase in non-carbonic acids in the blood, is not the primary acid-base imbalance in this case since the scenario does not provide information indicating a primary metabolic disorder. Respiratory alkalosis, characterized by decreased levels of CO2 in the blood, leading to increased pH and alkalinity, is not the primary acid-base imbalance in this case. The depressed ventilation and associated increase in CO2 levels indicate the opposite, respiratory acidosis. Metabolic alkalosis, characterized by an increase in bicarbonate levels or a decrease in non-carbonic acids, is not the primary acid-base imbalance in this case as the scenario does not provide information indicating a primary metabolic disorder.
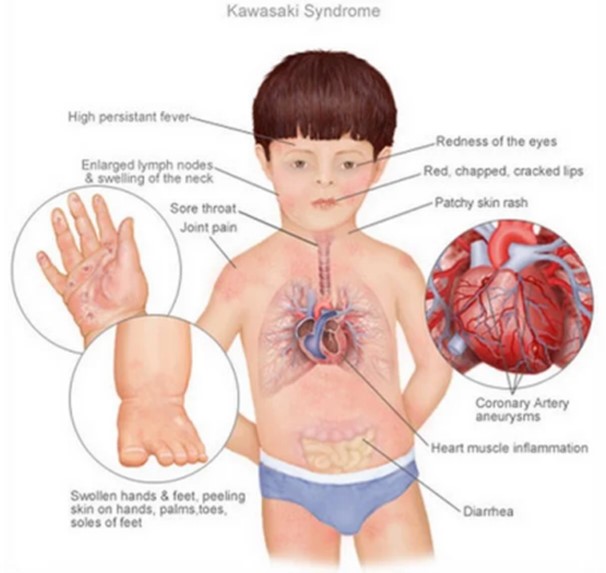
A child diagnosed with Kawasaki disease is brought to the clinic. The mother reports that her child is irritable, refuses to eat, and has skin peeling on both hands and feet. Which intervention should the nurse instruct the mother to implement first?
Explanation
Kawasaki disease is an inflammatory condition that primarily affects children, causing symptoms such as fever, rash, conjunctivitis, swollen lymph nodes, and changes in the hands and feet, including skin peeling. It is important to create a calm and quiet environment for the child to minimize stimulation and discomfort.
Placing the child in a quiet environment helps reduce irritability and allows the child to rest. It also helps prevent further stress and agitation, which can exacerbate the symptoms of
Kawasaki disease. Providing a quiet space can promote comfort and improve the child's overall well-being.
Applying lotion to the hands and feet may be beneficial for soothing any dry or peeling skin, but it is not the priority intervention. Creating a quiet environment to address the child's irritability and discomfort takes precedence.
Encouraging the parents to rest when possible and making a list of foods that the child likes are important aspects of care, but they are not the immediate interventions to address the child's current symptoms of irritability, refusal to eat, and skin peeling. These interventions can be addressed after providing a quiet environment and ensuring the child's comfort.
Mrs. Kalen is a 70 year old female who has arrived into the ER due to persistent vomiting for two days now. She appears to be lethargic and weak and has myalgia. She is noted to have dry mucus membranes and her capillary refill takes >4 seconds. She is diagnosed as having gastroenteritis and dehydration. Measurement of arterial blood gas shows pH 7.5, PaO2 85 mm Hg, PaCO2 40 mm Hg, and HCO3 34 mmol/L. What would you interpret the acid-base disorder to be?
Explanation
The pH value of 7.5 indicates alkalosis, as it is above the normal range of 7.35-7.45. The elevated bicarbonate (HCO3-) level of 34 mmol/L suggests metabolic alkalosis, as it is higher than the normal range of 22-28 mmol/L. The PaCO2 level of 40 mm Hg falls within the normal range of 35-45 mm Hg.
In this case, the primary disturbance is metabolic alkalosis, which is likely caused by vomiting leading to excessive loss of gastric acid (hydrogen ions) and chloride ions from the stomach. This loss of acid and chloride results in an imbalance of electrolytes and an increase in bicarbonate levels, leading to metabolic alkalosis.
The arterial blood gas results do not indicate any compensation. Compensation occurs when the body attempts to restore the pH balance by adjusting the respiratory or metabolic systems. In this case, there is no compensation observed because the PaCO2 level is within the normal range and not significantly altered.
Mrs. Kalen is a 70-year-old female who has arrived at the ER due to persistent vomiting for two days now. She appears to be lethargic and weak and has myalgia. She is noted to have dry mucus membranes and her capillary refill takes >4 seconds. She is diagnosed as having gastroenteritis and dehydration. Measurement of arterial blood gas shows pH 7.5, PaO2 85 mm Hg, PaCO2 40 mm Hg, and HCO3 34 mmol/L. Based on the acid-base interruption from Mrs. Kalen, what can the nurse anticipate the treatment will be for correcting this imbalance?
Explanation
Mrs. Kalen is diagnosed with gastroenteritis and dehydration, and the arterial blood gas results indicate metabolic alkalosis (elevated pH and HCO3-). This suggests that there is an excessive loss of gastric acid and chloride ions from vomiting, leading to an imbalance of electrolytes and an increase in bicarbonate levels.
To correct the imbalance and treat dehydration, the primary intervention is fluid replacement. Administration of IV 0.9 Saline Solution, also known as normal saline, is commonly used for fluid resuscitation and rehydration. This isotonic solution helps restore fluid balance and electrolyte levels in the body.
Administration of antiemetics may help control vomiting, but the primary treatment focus in this case is fluid and electrolyte replacement to correct dehydration and the associated metabolic alkalosis.
Administration of diuretics, which increase urine output, would not be appropriate in this case as the patient is already experiencing dehydration.
Electrolyte replacement may be necessary if there are specific electrolyte imbalances identified, but the primary treatment is fluid replacement with IV saline solution.
Having the patient go home and rest without addressing the underlying dehydration and metabolic alkalosis would not be appropriate as it can lead to further complications.
Mrs. Kalen is a 70 year old female who has arrived into the ER due to persistent vomiting for two days now. She appears to be lethargic and weak and has myalgia. She is noted to have dry mucus membranes and her capillary refill takes >4 seconds. She is diagnosed as having gastroenteritis and dehydration. Measurement of arterial blood gas shows pH 7.5, PaO2 85 mm Hg, PaCO2 40 mm Hg, and HCO3 34 mmol/L. What would you interpret the acid-base disorder to be?
Explanation
The pH value of 7.5 indicates alkalosis, as it is above the normal range of 7.35-7.45. The elevated bicarbonate (HCO3-) level of 34 mmol/L suggests metabolic alkalosis, as it is higher than the normal range of 22-28 mmol/L. The PaCO2 level of 40 mm Hg falls within the normal range of 35-45 mm Hg.
In this case, the primary disturbance is metabolic alkalosis, which is likely caused by the persistent vomiting leading to excessive loss of gastric acid (hydrogen ions) and chloride ions from the stomach. This loss of acid and chloride results in an imbalance of electrolytes and an increase in bicarbonate levels, leading to metabolic alkalosis.
Since there is no significant deviation from the normal range in the PaCO2 level, the respiratory system has not effectively compensated for the metabolic alkalosis. Therefore, it is considered uncompensated.
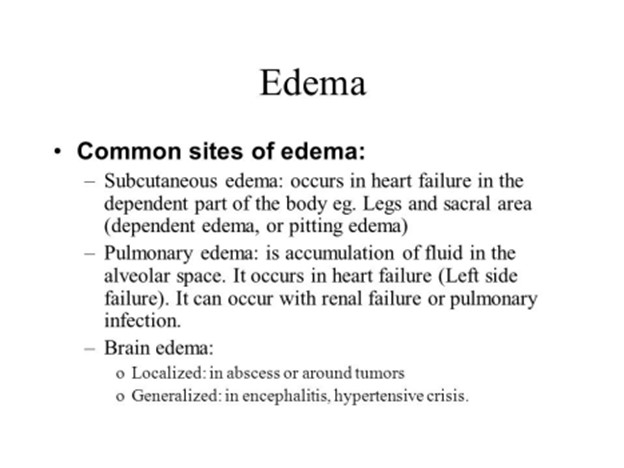
The patient who is confined to bed in the supine position has gained 5 lbs. in the last 48 hours. In which area does the nurse assess skin turgor for accurate determination of dependent edema?
Explanation
Dependent edema refers to the accumulation of fluid in the dependent parts of the body, which are areas that are most affected by gravity when a person is in a supine or sitting position for an extended period. The sacrum, which is the triangular bone at the base of the spine, is one such dependent area. It is prone to developing edema when there is increased fluid retention in the body, as seen in the patient's weight gain.
To assess for dependent edema accurately, the nurse can gently press the skin over the sacral area with their fingers and observe the skin turgor or the return of the skin to its normal position after releasing the pressure. If there is edema, the skin may have reduced elasticity and take longer to return to its normal position (poor skin turgor).
While edema can occur in other dependent areas such as the feet, ankles, and lower legs, assessing skin turgor in these areas may not provide an accurate determination of dependent edema as they are located further away from the sacrum and may be influenced by other factors.
A client is suffering from osteoarthritis in the knees and the nurse is providing care. The nurse is assessing the client's pain level and pain tolerance. Based on the nurse's understanding of pain, the nurse knows that a client's pain tolerance is most likely relieved by which of the following?
Explanation
Pain tolerance refers to the maximum level of pain that an individual can tolerate without significant distress. It is influenced by various factors, including psychological and emotional factors. While emotions such as anger, boredom, and introversion can have an impact on a person's pain perception and experience, sleep plays a significant role in pain tolerance. During sleep, the body is in a state of rest and relaxation, allowing for decreased sensory input and potentially reducing pain perception. Sleep provides an opportunity for the body to repair and heal, which can contribute to improved pain tolerance. Additionally, sleep promotes the release of endogenous opioids, which are natural pain-relieving substances produced by the body.
Which nursing documentation demonstrates the integration of patient-centered care?
Explanation
Patient-centered care involves actively involving the patient in their care and considering their preferences, values, and goals. By discussing dietary preferences with the client, the nurse is demonstrating a patient-centered approach. This documentation indicates that the nurse took the time to engage in a conversation with the client to understand their dietary preferences,
which can help tailor the care plan to meet the client's individual needs and preferences. "Steady gait observed when ambulating" focuses on the nurse's observation and assessment but does not specifically involve the patient's preferences or goals.
"Social worker paged for consultation" indicates collaboration with another healthcare professional but does not necessarily reflect the patient's active involvement or preferences. "Nursing literature reviewed for best practice approaches" highlights evidence-based practice but does not directly involve the patient's preferences or engagement in decision-making.
An older adult is admitted to the hospital. The patient's height is 5 feet, 6 Inches (1.68M), and weigh 250 lb. (113.3kg). The nurse calculates the patient's current body mass index (BMI) as: (Round your answer to the nearest whole number.)
Explanation
To calculate the patient's body mass index (BMI), we need to divide the weight (in kilograms) by the square of the height (in meters). Let's convert the height and weight measurements to the appropriate units and perform the calculation:
Height: 5 feet, 6 inches = 5 + (6/12) = 5.5 feet = 1.6764 meters (rounded to four decimal places) Weight: 250 lb. = 113.3 kg
BMI = Weight (kg) / (Height (m))^2
BMI = 113.3 kg / (1.6764 m)^2
BMI ≈ 40.0
Based on the diagnosis of Dehydration, select which IV solution will be ordered to treat waiting this patient.
Explanation
0.9% Sodium chloride is a balanced isotonic solution that closely resembles the electrolyte composition of the extracellular fluid. It is commonly used to treat dehydration because it helps restore fluid volume and electrolyte balance in the body.
5% dextrose in Lactated Ringers: This solution is typically used for fluid and electrolyte replacement in patients who have significant fluid losses or imbalances, but it may not be the best choice for dehydration alone.
0.45% sodium chloride: This solution, also known as half-normal saline, has a lower concentration of sodium chloride and is often used for patients who require hypotonic fluids. It may not provide enough electrolyte replacement for a dehydrated patient. 3% Normal Saline: This solution has a higher concentration of sodium chloride and is typically used for specific indications, such as severe hyponatremia or in critical care settings. It is not the first-line choice for treating dehydration.
A patient, age 23, underwent a rhinoplasty 6 hours ago. After administering his pain medication, the nurse notes that he is swallowing frequently. What is the most likely cause of the swallowing?
Explanation
After rhinoplasty, nasal packing is often used to control bleeding and provide support to the nasal structures. Nasal packing can cause oral dryness, as it obstructs the normal airflow through the nasal passages, leading to mouth breathing. Mouth breathing, in turn, can cause dryness of the oral mucosa and throat, resulting in the sensation of dryness and the need to swallow frequently.
While bleeding is a possible complication after rhinoplasty, the patient's symptom of frequent swallowing is more indicative of oral dryness rather than bleeding.
Although adverse reactions to analgesics can occur, frequent swallowing is not a common symptom associated with analgesic adverse reactions. Other signs such as rash, difficulty breathing, or changes in vital signs would be more typical in case of an adverse reaction. Swallowing can be a normal response to surgery, but in this scenario, the most likely cause is the oral dryness caused by the nasal packing rather than a direct response to the analgesic.
The nurse is caring for a 48-year-old-client admitted with complaints of fatigue and hemoptysis, but no other significant medical history. Social history includes smoking 1 pack/day x 20 years and occasional alcohol use. He denies taking any medication. The Mantoux test placed 72 hours earlier reveals an indurated area of 4 cm. Which action will the nurse plan to include in the care for this client?
Explanation
The client's complaint of hemoptysis (coughing up blood) and a positive Mantoux test (4 cm induration) suggest the possibility of tuberculosis (TB) infection. TB is an airborne infectious disease, and placing the client in airborne isolation is necessary to prevent the spread of the infection to others.
Antibiotics may be used to treat tuberculosis, but the initial step would be to isolate the client and confirm the diagnosis before starting specific treatment.
A CT scan may be ordered to further evaluate the client's condition, but it is not the immediate action required in this case. Isolation and confirmation of the diagnosis take priority. While the client may require oxygen therapy based on their respiratory symptoms, it is not the primary action to take at this stage. Isolation and further evaluation are necessary before initiating specific treatments.
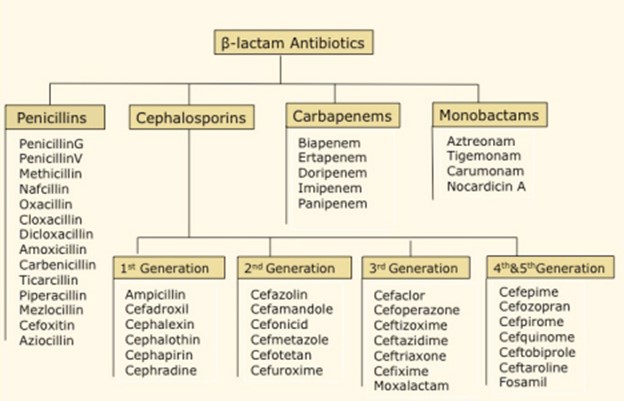
Cephalosporins are similar to another group of beta-lactam antibiotics called the?
Explanation
Cephalosporins are similar to another group of beta-lactam antibiotics called the Penicillins. Both cephalosporins and penicillins belong to the beta-lactam class of antibiotics, which share a similar structure and mechanism of action. They inhibit bacterial cell wall synthesis by binding to specific proteins called penicillin-binding proteins (PBPs), leading to bacterial cell death. This shared mechanism of action makes cephalosporins and penicillins similar in their antibacterial effects.
On the other hand, macrolides, fluoroquinolones, and aminoglycosides are different classes of antibiotics with distinct structures and mechanisms of action. They work through different mechanisms to inhibit bacterial growth and have different spectrums of activity compared to beta-lactam antibiotics like cephalosporins and penicillins.
The nurse receives an order to draw a peak level on a patient prescribed Gentamicin via Intravenous (IV) infusion. When is the best time for the nurse to draw this peak level?
Explanation
Gentamicin is an antibiotic that is usually administered via IV infusion. The peak level is the highest concentration of the medication in the bloodstream, and it is important to monitor it to ensure therapeutic levels are achieved without reaching toxic levels.
Drawing the peak level 30 minutes after the infusion is complete allows enough time for the medication to distribute throughout the body and reach its peak concentration. This timing provides an accurate representation of the highest drug concentration in the bloodstream. 30 minutes before starting the infusion: Drawing the peak level before starting the infusion would not accurately reflect the peak concentration of the medication in the bloodstream. Immediately before the next dose of Gentamicin: Drawing the peak level immediately before the next dose would not provide an accurate assessment of the highest drug concentration, as the levels would have started to decrease due to elimination.
1 hour after infusion is complete: Waiting for 1 hour after the infusion is complete may result in missing the actual peak concentration of the medication in the bloodstream, as it may have already started to decline.
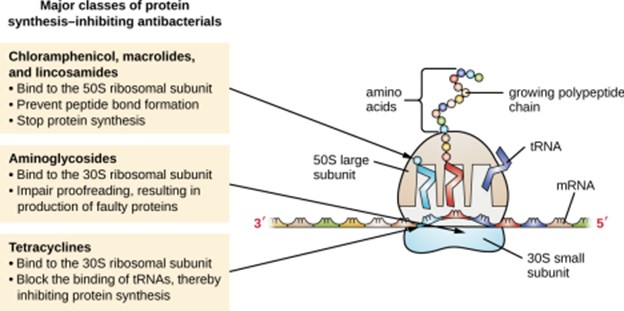
Fill-in-the-blank: Aminoglycosides work by binding to the _______ which prevents______
Explanation
Aminoglycosides work by binding to the 30S subunit; this binding interferes with the bacterial ribosome's ability to synthesize proteins. By inhibiting protein synthesis, aminoglycosides disrupt bacterial growth and can lead to bacterial cell death.
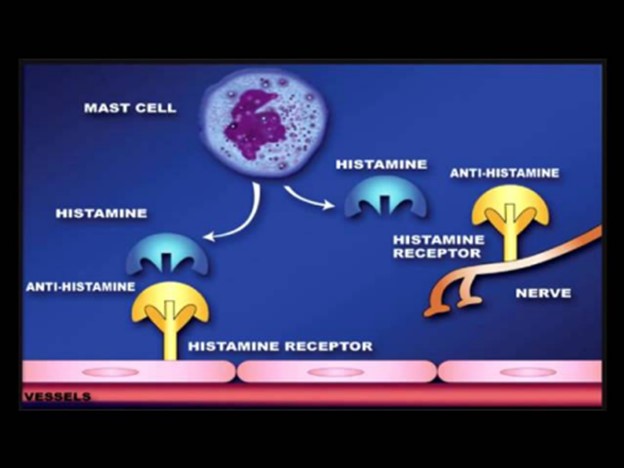
A nursing instructor is teaching a group of nursing students about antihistamines. Which statement by a student indicates an understanding of the mechanism of action of the antihistamines?
Explanation
Antihistamines primarily work by blocking the H1 receptors, which are the receptors responsible for mediating the actions of histamine in the body. By blocking these receptors, antihistamines prevent or reduce the effects of histamine, such as itching, sneezing, runny nose, and watery eyes. This is the main mechanism by which antihistamines provide their therapeutic effects. "Antihistamines block release of histamine from mast cells and basophils." This statement is incorrect. Antihistamines do not block the release of histamine; instead, they block the histamine receptors to prevent the effects of histamine.
"H1 antagonists can bind to H1 receptors, H2 receptors, and muscarinic receptors." This statement is incorrect. H1 antagonists, or H1 receptor blockers, specifically bind to H1 receptors and do not have significant affinity for H2 receptors or muscarinic receptors. "First-generation antihistamines are more selective than second-generation antihistamines." This statement is incorrect. First-generation antihistamines are generally less selective and can have more sedating and anticholinergic effects compared to second-generation antihistamines, which are designed to be more selective for H1 receptors and have reduced sedative properties.
Celecoxib is what class of drug?
Explanation
Nonsteroidal anti-inflammatory drugs (NSAIDs) are a class of medications commonly used to relieve pain, reduce inflammation, and lower fever. They work by inhibiting the production of prostaglandins, which are substances in the body that play a role in pain and inflammation. Celecoxib specifically belongs to the subclass of NSAIDs known as selective COX-2 inhibitors, which target the enzyme cyclooxygenase-2 (COX-2). By selectively inhibiting COX-2, celecoxib helps to reduce inflammation and pain while potentially minimizing the gastrointestinal side effects associated with traditional non-selective NSAIDs.
Sign Up or Login to view all the 44 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

