RN HESI Pharmacology Exam
Total Questions : 31
Showing 25 questions, Sign in for moreA female client with mild depression reports to the nurse recently starting St. John's wort. Which information provided by the client requires further instruction?
Explanation
Choice A reason: Hard candy can be used for a dry mouth, which is a common side effect of St. John's wort.
Choice B reason: Another form of contraception is needed, because St. John's wort can reduce the effectiveness of oral contraceptives and increase the risk of unplanned pregnancy. This information requires further instruction from the nurse.

Choice C reason: Insomnia may occur while taking the medication, which is another possible side effect of St. John's wort. The client should be advised to take the medication in the morning or afternoon, and avoid caffeine and alcohol.
Choice D reason: Sensitivity to the sun can develop, which is a rare but serious side effect of St. John's wort. The client should be instructed to wear sunscreen and protective clothing when exposed to sunlight.
A client who is taking an oral dose of a tetracycline reports gastrointestinal (GI) upset. Which snack should the nurse instruct the client to take with the tetracycline?
Explanation
Choice A reason: Cheese and crackers are not a good snack to take with tetracycline, because cheese contains calcium, which can interfere with the absorption of tetracycline and reduce its effectiveness.
Choice B reason: Toasted wheat bread and jelly are a suitable snack to take with tetracycline, because they do not contain any dairy products or iron, which can also affect the absorption of tetracycline. Toasted bread may also help to settle the stomach and prevent nausea.

Choice C reason: Fruit-flavored yogurt is not a good snack to take with tetracycline, because yogurt is a dairy product that contains calcium, which can interfere with the absorption of tetracycline and reduce its effectiveness.
Choice D reason: Cold cereal with skim milk is not a good snack to take with tetracycline, because skim milk is a dairy product that contains calcium, which can interfere with the absorption of tetracycline and reduce its effectiveness.
To prevent deep vein thromboses following knee replacement surgery, an adult male client is receiving daily subcutaneous enoxaparin. Which laboratory result requires immediate action by the nurse?
Reference Range:
Hematocrit [42% to 52% (0.42 to 0.52 volume fraction)]
Platelets [150,000 to 400,000/mm² (150 to 400 × 10^9/L)]
Creatinine [0.5 to 1.1 mg/dL (44 to 97 μmol/L)]
Blood Urea Nitrogen (BUN) [10 to 20 mg/dL (3.6 to 7.1 mmol/L)]
Explanation
Choice A reason: Platelet count of 100,000/mm³ (100 x 10^9/L) is below the normal range and indicates thrombocytopenia, which is a decrease in the number of platelets in the blood. Thrombocytopenia can increase the risk of bleeding and bruising, and can be a serious adverse effect of enoxaparin. This laboratory result requires immediate action by the nurse, such as notifying the prescriber, monitoring for signs of bleeding, and withholding the next dose of enoxaparin.
Choice B reason: Hematocrit 45% (0.45 volume fraction) is within the normal range and does not indicate any problem with the client's red blood cells or oxygen-carrying capacity.
Choice C reason: Blood urea nitrogen (BUN) 20 mg/dL (7.1 mmol/L) is within the normal range and does not indicate any problem with the client's kidney function or hydration status.
Choice D reason: Serum creatinine 1.0 mg/dL (88.4 μmol/L) is within the normal range and does not indicate any problem with the client's kidney function or muscle metabolism.
Explanation
Choice A reason: Increased anxiety and nervousness have been reported by some people taking feverfew, but this is not a common or serious side effect. It may be related to individual sensitivity or dosage.
Choice B reason: Feverfew may interact with aspirin or non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, which are commonly used for pain relief. Feverfew and these drugs can both inhibit platelet aggregation and increase the risk of bleeding. This information is most important for the nurse to include in a teaching plan for this client, especially if they are taking any of these medications or have a history of bleeding disorders.
Choice C reason: Those with allergies to chamomile, ragweed, or yarrow should not take feverfew, because they may have a cross-reactivity and experience an allergic reaction to feverfew. This information is important for the nurse to include in a teaching plan for this client, but it is not as critical as choice B.
Choice D reason: Abdominal pain, gas, nausea, vomiting, and diarrhea can occur when taking feverfew, but these are usually mild and transient side effects that do not require medical attention. They may be reduced by taking feverfew with food or water.
A client is receiving orlistat as part of a weight management program. Which ongoing assessment should be included in the plan of care to determine the effectiveness of the medication?
Explanation
Choice A reason: Depression screening is not directly related to the effectiveness of orlistat, which is a medication that blocks the absorption of fat from the diet and helps to reduce weight. Depression screening may be important for the overall mental health of the client, but it is not an ongoing assessment for orlistat.
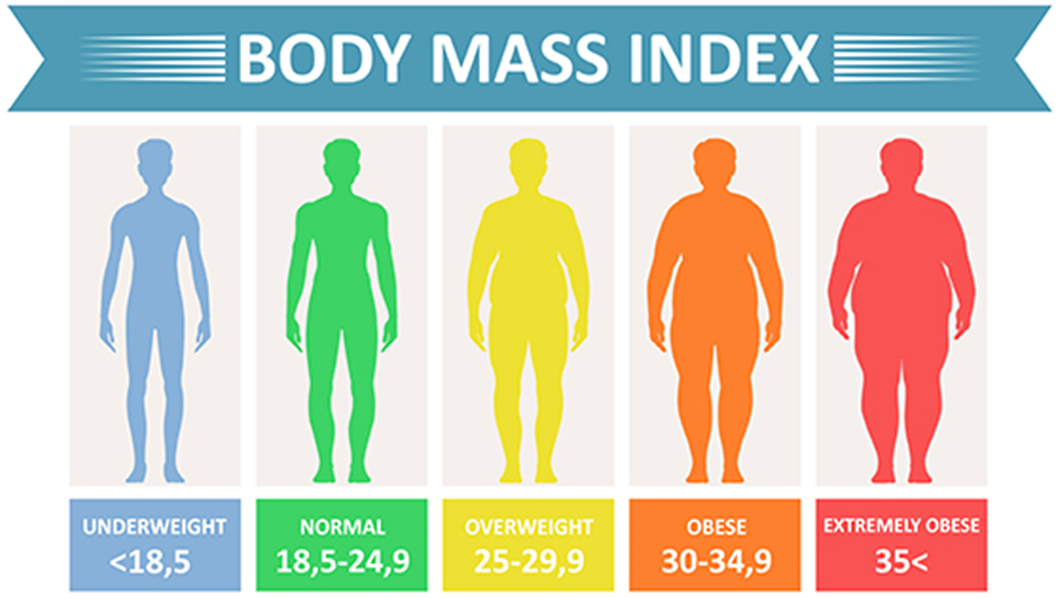
Choice B reason: Body mass index (BMI) is a measure of body fat based on height and weight, and it is used to assess the risk of obesity-related health problems. BMI is an ongoing assessment for orlistat, because it can indicate the progress and outcome of the weight management program. The goal of orlistat therapy is to achieve and maintain a healthy BMI.
Choice C reason: Daily calorie count is not an ongoing assessment for orlistat, because it does not reflect the amount of fat absorbed by the body. Orlistat works by blocking the action of lipase, an enzyme that breaks down fat in the intestine. Therefore, even if the client consumes a high-calorie diet, orlistat can prevent some of the fat from being absorbed and reduce weight. However, daily calorie count may be useful for monitoring the overall nutritional intake and energy balance of the client.
Choice D reason: Serum protein levels are not an ongoing assessment for orlistat, because they are not affected by the medication. Orlistat only blocks the absorption of fat, not protein or carbohydrates. Serum protein levels may be important for evaluating the nutritional status and organ function of the client, but they are not an indicator of orlistat effectiveness.
Explanation
Choice A reason: Beef tips with gravy are not a dietary choice that should be avoided by a client taking phenelzine, which is a monoamine oxidase inhibitor (MAOI) that treats depression. Beef tips with gravy do not contain tyramine, which is a substance that can interact with MAOIs and cause a hypertensive crisis.
Choice B reason: Deep-fried shrimp are not a dietary choice that should be avoided by a client taking phenelzine, which is a monoamine oxidase inhibitor (MAOI) that treats depression. Deep-fried shrimp do not contain tyramine, which is a substance that can interact with MAOIs and cause a hypertensive crisis.
Choice C reason: Pepperoni pizza is a dietary choice that should be avoided by a client taking phenelzine, which is a monoamine oxidase inhibitor (MAOI) that treats depression. Pepperoni pizza contains tyramine, which is a substance that can interact with MAOIs and cause a hypertensive crisis. Tyramine is found in aged, fermented, cured, smoked, or pickled foods, such as cheese, salami, sauerkraut, soy sauce, beer, and wine.
Choice D reason: Pan-seared catfish is not a dietary choice that should be avoided by a client taking phenelzine, which is a monoamine oxidase inhibitor (MAOI) that treats depression. Pan-seared catfish does not contain tyramine, which is a substance that can interact with MAOIs and cause a hypertensive crisis.
Which assessment finding requires nursing intervention prior to the administration of a prescribed dose of digoxin to an adult?
Explanation
Choice A reason: Apical pulse rate of 50 beats/minute requires nursing intervention prior to the administration of digoxin, which is a medication that slows down and strengthens the heartbeat. Digoxin can cause bradycardia, which is a slow heart rate below 60 beats/minute. Bradycardia can lead to inadequate blood flow and oxygen delivery to the body. The nurse should withhold the dose of digoxin and notify the prescriber if the apical pulse rate is below 60 beats/minute.
Choice B reason: Irregular apical pulse rhythm does not require nursing intervention prior to the administration of digoxin, which is a medication that treats arrhythmias, which are irregular heart rhythms. Digoxin can correct or prevent some types of arrhythmias, such as atrial fibrillation or flutter. The nurse should monitor the apical pulse rhythm and report any changes to the prescriber, but it is not a reason to withhold the dose of digoxin.
Choice C reason: Presence of a systolic heart murmur does not require nursing intervention prior to the administration of digoxin, which is a medication that improves the pumping function of the heart. A systolic heart murmur is a sound that occurs when the heart contracts and blood flows through a narrow or leaky valve. Digoxin can reduce the symptoms of heart failure, such as shortness of breath, fatigue, and edema, which may be associated with a systolic heart murmur. The nurse should document the presence and characteristics of the heart murmur, but it is not a reason to withhold the dose of digoxin.
Choice D reason: Apical pulse heard best at the pulmonic site does not require nursing intervention prior to the administration of digoxin, which is a medication that affects the electrical activity and contractility of the heart. The apical pulse is the heartbeat heard at the apex of the heart, which is located at the fifth intercostal space on the left midclavicular line. The pulmonic site is located at the second intercostal space on the left sternal border, where the sound of blood flow through the pulmonary valve can be heard. The nurse should listen to the apical pulse at the correct location, but it is not a reason to withhold the dose of digoxin.
A client with multiple sclerosis starts a new prescription, baclofen, to control muscle spasticity. Three days later, the client calls the clinic nurse and reports feeling fatigued and dizzy. Which instruction should the nurse provide?
Explanation
Choice A reason: Increasing intake of fluids and high protein foods is not an instruction that the nurse should provide to the client who is taking baclofen, which is a medication that relaxes skeletal muscles and reduces spasticity. Fluids and high protein foods do not affect the action or side effects of baclofen.
Choice B reason: Stopping taking the medication immediately is not an instruction that the nurse should provide to the client who is taking baclofen, which is a medication that should be tapered off gradually under medical supervision. Abrupt withdrawal of baclofen can cause serious complications, such as seizures, hallucinations, and increased spasticity.
Choice C reason: Obtaining transportation to the emergency department is not an instruction that the nurse should provide to the client who is taking baclofen, which is a medication that can cause mild and transient side effects, such as fatigue and dizziness. These side effects are not life-threatening and usually subside as the body adjusts to the medication.
Choice D reason: Avoiding hazardous activities until symptoms subside is an instruction that the nurse should provide to the client who is taking baclofen, which is a medication that can impair the ability to drive, operate machinery, or perform other tasks that require alertness and coordination. The client should be advised to exercise caution and avoid activities that could result in injury until they are no longer experiencing fatigue and dizziness.

Explanation
Choice A reason: Expectorating bronchial secretions is not an assessment information that indicates that the antitussive medication benzonatate is effective. Benzonatate is a medication that suppresses the cough reflex by numbing the throat and lungs. It does not loosen or thin the mucus in the airways, which would facilitate expectoration.
Choice B reason: Reports reduced nasal discharge is not an assessment information that indicates that the antitussive medication benzonatate is effective. Benzonatate is a medication that suppresses the cough reflex by numbing the throat and lungs. It does not affect the production or drainage of nasal secretions, which are caused by inflammation and infection in the upper respiratory tract.
Choice C reason: Able to sleep through the night is not an assessment information that indicates that the antitussive medication benzonatate is effective. Benzonatate is a medication that suppresses the cough reflex by numbing the throat and lungs. It does not have any sedative or hypnotic effects, which would promote sleep. However, by reducing coughing, benzonatate may indirectly improve the quality of sleep for the client.
Choice D reason: Denies having coughing spells is an assessment information that indicates that the antitussive medication benzonatate is effective. Benzonatate is a medication that suppresses the cough reflex by numbing the throat and lungs. It reduces the frequency and intensity of coughing, which can relieve discomfort and irritation for the client.
Explanation
Choice A reason: Eliminating use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, is an instruction that the nurse should provide to the client who is taking lithium carbonate, which is a medication that stabilizes mood and prevents manic episodes. NSAIDs can increase the blood levels of lithium and cause toxicity, which can manifest as nausea, vomiting, tremors, confusion, or seizures.
Choice B reason: Monitoring blood glucose levels daily is not an instruction that the nurse should provide to the client who is taking lithium carbonate, which is a medication that does not affect the blood sugar levels or the risk of diabetes. Blood glucose levels may be important for the general health of the client, but they are not related to lithium therapy.
Choice C reason: Notifying healthcare provider prior to dental procedures is not an instruction that the nurse should provide to the client who is taking lithium carbonate, which is a medication that does not interact with local anesthetics or antibiotics that may be used during dental procedures. However, the client should inform the dentist about their medical history and medications, as a precaution.
Choice D reason: Avoiding consuming all foods that contain iodine is not an instruction that the nurse should provide to the client who is taking lithium carbonate, which is a medication that does not interfere with the thyroid function or the metabolism of iodine. Iodine is an essential nutrient that is found in many foods, such as seafood, dairy products, eggs, and iodized salt. Avoiding iodine can cause deficiency and lead to goiter or hypothyroidism.
A client with bipolar disorder admitted with severe depression and suicidal ideation receives a prescription for lithium carbonate. Which instruction should the nurse provide to the client?
Explanation
Choice A reason: Eliminating use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, is an instruction that the nurse should provide to the client who is taking lithium carbonate, which is a medication that stabilizes mood and prevents manic episodes. NSAIDs can increase the blood levels of lithium and cause toxicity, which can manifest as nausea, vomiting, tremors, confusion, or seizures.
Choice B reason: Monitoring blood glucose levels daily is not an instruction that the nurse should provide to the client who is taking lithium carbonate, which is a medication that does not affect the blood sugar levels or the risk of diabetes. Blood glucose levels may be important for the general health of the client, but they are not related to lithium therapy.
Choice C reason: Notifying healthcare provider prior to dental procedures is not an instruction that the nurse should provide to the client who is taking lithium carbonate, which is a medication that does not interact with local anesthetics or antibiotics that may be used during dental procedures. However, the client should inform the dentist about their medical history and medications, as a precaution.
Choice D reason: Avoiding consuming all foods that contain iodine is not an instruction that the nurse should provide to the client who is taking lithium carbonate, which is a medication that does not interfere with the thyroid function or the metabolism of iodine. Iodine is an essential nutrient that is found in many foods, such as seafood, dairy products, eggs, and iodized salt. Avoiding iodine can cause deficiency and lead to goiter or hypothyroidism.

Explanation
Choice A reason: Using a Snellen chart to assess visual acuity is not a direct measure of the effectiveness of pilocarpine, which is used to lower intraocular pressure by constricting the pupil and increasing aqueous humor outflow. Visual acuity may be affected by other factors, such as refractive errors, cataracts, or macular degeneration.
Choice B reason: Checking the amount of drainage from each eye is not a relevant action for evaluating the effectiveness of pilocarpine, which does not affect tear production or drainage. Excessive or abnormal eye drainage may indicate an infection, allergy, or injury.
Choice C reason: Palpating the eyelids for decreased swelling is not a useful action for evaluating the effectiveness of pilocarpine, which does not cause or reduce eyelid swelling. Eyelid swelling may be caused by inflammation, infection, allergy, or trauma.
Choice D reason: Reviewing eye pressure measurements is the correct action for evaluating the effectiveness of pilocarpine, which is used to lower intraocular pressure in patients with open-angle glaucoma. High intraocular pressure can damage the optic nerve and cause vision loss. Pilocarpine reduces intraocular pressure by constricting the pupil and increasing aqueous humor outflow.
Explanation
Choice A reason: Trouble sleeping is not a relevant information for administering pyridostigmine, which is a cholinesterase inhibitor that improves muscle strength and function in patients with myasthenia gravis. Trouble sleeping may be caused by other factors, such as stress, pain, or medication side effects.
Choice B reason: Difficulty with urination is not a pertinent information for administering pyridostigmine, which does not affect urinary function or bladder control. Difficulty with urination may indicate a urinary tract infection, prostate enlargement, or kidney stones.
Choice C reason: Unexplained weight loss is not a significant information for administering pyridostigmine, which does not affect metabolism or appetite. Unexplained weight loss may be a sign of an underlying condition, such as hyperthyroidism, diabetes, or cancer.
Choice D reason: Recent oral intake is the correct information for administering pyridostigmine, which should be taken on an empty stomach or before meals to enhance its absorption and effectiveness. Pyridostigmine can also help prevent or reduce dysphagia (difficulty swallowing), which is a common symptom of myasthenia gravis.
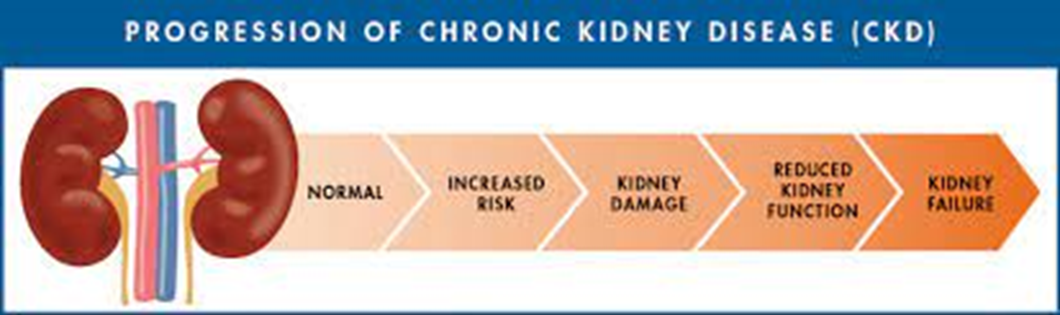
The nurse is administering sevelamer during lunch to a client with chronic kidney disease (CKD). The client asks the nurse to bring the medication later. The nurse should describe which action of sevelamer as an explanation for taking it with meals?
Explanation
Choice A reason: Promoting stomach emptying and preventing gastric reflux is not a relevant action of sevelamer, which is a phosphate binder that lowers serum phosphate levels in patients with CKD. Gastric reflux may be caused by other factors, such as hiatal hernia, obesity, or spicy foods.
Choice B reason: Buffering hydrochloric acid and preventing gastric erosion is not a pertinent action of sevelamer, which does not affect gastric acidity or mucosal integrity. Gastric erosion may be caused by other factors, such as NSAIDs, alcohol, or Helicobacter pylori infection.
Choice C reason: Preventing indigestion associated with ingestion of spicy foods is not a significant action of sevelamer, which does not affect digestion or food tolerance. Indigestion may be caused by other factors, such as overeating, stress, or gallstones.
Choice D reason: Binding with phosphorus in foods and preventing absorption is the correct action of sevelamer, which should be taken with meals to reduce the amount of phosphorus that enters the bloodstream from the diet. High serum phosphate levels can cause bone loss, calcification of soft tissues, and secondary hyperparathyroidism in patients with CKD.
Explanation
Choice A reason: Sleeping soundly through the night is the desired outcome of administering zolpidem, which is a sedative-hypnotic that induces sleep by enhancing the activity of GABA, an inhibitory neurotransmitter. Zolpidem is used to treat insomnia, especially difficulty falling asleep.
Choice B reason: Decreasing episodes of incontinence is not a relevant outcome of administering zolpidem, which does not affect urinary function or bladder control. Incontinence may be caused by other factors, such as aging, prostate problems, or urinary tract infections.
Choice C reason: Improving ability to concentrate is not a pertinent outcome of administering zolpidem, which does not affect cognitive function or attention span. Zolpidem may actually impair memory and cause daytime drowsiness or confusion in some patients.
Choice D reason: Exhibiting fewer emotional outbursts is not a significant outcome of administering zolpidem, which does not affect mood or behavior. Zolpidem may actually cause paradoxical reactions, such as agitation, aggression, or hallucinations in some patients.
: [Zolpidem (Oral Route)]
: [Insomnia]
: [Urinary Incontinence]
: [Concentration Problems]
The nurse is teaching a client with type 1 diabetes mellitus (DM) about the onset, peak, and duration of a new prescription for glargine insulin. If the insulin is administered at 0800, when is the client most likely to experience hypoglycemia?
Explanation
Choice A reason: Midmorning is not a likely time for experiencing hypoglycemia after administering glargine insulin at 0800, because glargine insulin has a slow onset of action (about 1 hour) and does not have a pronounced peak effect. Glargine insulin is a long-acting insulin that provides a steady level of insulin throughout the day and night.
Choice B reason: No peak occurs is the correct answer for when hypoglycemia is most likely to occur after administering glargine insulin at 0800, because glargine insulin does not have a pronounced peak effect that could cause a sudden drop in blood glucose levels. Glargine insulin is a long-acting insulin that provides a steady level of insulin throughout the day and night.
Choice C reason: Midafternoon is not a likely time for experiencing hypoglycemia after administering glargine insulin at 0800, because glargine insulin has a long duration of action (about 24 hours) and does not have a pronounced peak effect. Glargine insulin is a long-acting insulin that provides a steady level of insulin throughout the day and night.
Choice D reason: Shortly after midnight is not a likely time for experiencing hypoglycemia after administering glargine insulin at 0800, because glargine insulin has a long duration of action (about 24 hours) and does not have a pronounced peak effect. Glargine insulin is a long-acting insulin that provides a steady level of insulin throughout the day and night.

Explanation
Choice A reason: Promoting stomach emptying and preventing gastric reflux is not a relevant action of sevelamer, which is a phosphate binder that lowers serum phosphate levels in patients with CKD. Gastric reflux may be caused by other factors, such as hiatal hernia, obesity, or spicy foods.
Choice B reason: Buffering hydrochloric acid and preventing gastric erosion is not a pertinent action of sevelamer, which does not affect gastric acidity or mucosal integrity. Gastric erosion may be caused by other factors, such as NSAIDs, alcohol, or Helicobacter pylori infection.
Choice C reason: Preventing indigestion associated with ingestion of spicy foods is not a significant action of sevelamer, which does not affect digestion or food tolerance. Indigestion may be caused by other factors, such as overeating, stress, or gallstones.
Choice D reason: Binding with phosphorus in foods and preventing absorption is the correct action of sevelamer, which should be taken with meals to reduce the amount of phosphorus that enters the bloodstream from the diet. High serum phosphate levels can cause bone loss, calcification of soft tissues, and secondary hyperparathyroidism in patients with CKD.
Patient Data
History and Physical
The client is a 42-year-old female who had a right above-the-knee amputation for osteomyelitis. The client has a drain in place and a surgical dressing that will need to be changed by the surgeon on post-op day 1.
Orders:
- Admit to the surgical floor
- Clear liquid diet, advance as tolerated
- Continuous cardiorespiratory monitoring
- Morphine 1 mg/hr intravenously
- Alert surgeon to signs of bleeding or infection in the surgical site
The nurse is discussing the client's pain management with a student nurse. Choose the most likely options for the information missing from the statement(s) by selecting from the lists of options provided.
Morphine is a(n) ______(a)_____ and it activates ______(b)________ receptors and is used to relieve _________(c)_________.
Choices a: a. Agonist-antagonist opiod b. Andogenous opiod c. Pure opioid antagonist d. Local anesthetic
Choice B: a. Mu b. Kappa c. Delta d. NMDA e. GABA
Choice C: a. Mild pain b. Moderate pain c. Severe pain d. Neuropathic pain e. Inflammatory pain
Explanation
The correct answer is:
Morphine is a(n) **pure opioid antagonist** and it activates **mu** receptors and is used to relieve **severe pain**.
Choice area A
Choice A reason:
A pure opioid antagonist is a drug that blocks the effects of opioids by binding to their receptors without activating them. Morphine is not a pure opioid antagonist, but a pure opioid agonist, which means it binds to and activates opioid receptors, producing analgesia and other effects. Therefore, choice A is incorrect.
Choice B reason:
An endogenous opioid is a naturally occurring substance in the body that binds to and activates opioid receptors, such as endorphins and enkephalins. Morphine is not an endogenous opioid, but an exogenous opioid, which means it is derived from an external source, such as the opium poppy. Therefore, choice B is incorrect.
Choice C reason:
A pure opioid antagonist is the correct term for morphine, as explained above. Therefore, choice C is correct.
Choice D reason:
A local anesthetic is a drug that blocks the transmission of nerve impulses in a specific area of the body, causing numbness and loss of sensation. Morphine is not a local anesthetic, but a systemic analgesic, which means it affects the whole body and reduces the perception of pain. Therefore, choice D is incorrect.
Choice area B
Choice A reason:
Mu receptors are one of the three types of opioid receptors in the body, along with kappa and delta receptors. Mu receptors are responsible for most of the analgesic and euphoric effects of opioids, as well as respiratory depression and physical dependence. Morphine has a high affinity for mu receptors and activates them strongly. Therefore, choice A is correct.
Choice B reason:
Kappa receptors are another type of opioid receptors in the body. Kappa receptors mediate some analgesic effects of opioids, as well as dysphoria, sedation, and miosis. Morphine has a low affinity for kappa receptors and activates them weakly. Therefore, choice B is incorrect.
Choice C reason:
Delta receptors are the third type of opioid receptors in the body. Delta receptors modulate some analgesic effects of opioids, as well as emotional responses and memory. Morphine has a low affinity for delta receptors and activates them weakly. Therefore, choice C is incorrect.
Choice D reason:
NMDA receptors are not opioid receptors, but glutamate receptors that are involved in synaptic plasticity, learning, memory, and pain modulation. Some drugs that act on NMDA receptors, such as ketamine and dextromethorphan, have analgesic properties, especially for neuropathic pain. Morphine does not act on NMDA receptors. Therefore, choice D is incorrect.
Choice E reason:
GABA receptors are not opioid receptors, but gamma-aminobutyric acid receptors that are involved in inhibitory neurotransmission in the central nervous system. Some drugs that act on GABA receptors, such as benzodiazepines and barbiturates, have sedative, anxiolytic, anticonvulsant, and muscle relaxant properties. Morphine does not act on GABA receptors. Therefore, choice E is incorrect.
Choice area C
Choice A reason:
Mild pain is pain that is easily tolerated and does not interfere with normal activities or sleep. Mild pain can usually be managed with non-opioid analgesics, such as acetaminophen or ibuprofen. Morphine is not used to relieve mild pain, as it is too potent and has more side effects and risks than non-opioid analgesics. Therefore, choice A is incorrect.
Choice B reason:
Moderate pain is pain that causes discomfort and affects normal activities or sleep to some extent. Moderate pain can usually be managed with combination analgesics, such as codeine or hydrocodone with acetaminophen or ibuprofen. Morphine can be used to relieve moderate pain in some cases, but it is not the first-line option, as it may be more effective and safer to use lower doses of opioids with non-opioid analgesics. Therefore, choice B is incorrect.
Choice C reason:
Severe pain is pain that causes significant distress and impairs normal activities or sleep to a great extent. Severe pain usually requires strong opioids, such as morphine or fentanyl, to achieve adequate relief. Morphine is commonly used to relieve severe pain in various settings, such as post-operative pain, cancer pain, or acute myocardial infarction. Therefore, choice C is correct.
Choice D reason:
Neuropathic pain is pain that results from damage or dysfunction of the nervous system, such as diabetic neuropathy or post-herpetic neuralgia. Neuropathic pain often responds poorly to conventional analgesics, including opioids. Morphine can be used to relieve neuropathic pain in some cases, but it may not be very effective or require higher doses than for nociceptive pain (pain that results from tissue damage or inflammation). Therefore, choice D is incorrect.
Choice E reason:
Inflammatory pain is pain that results from tissue damage or inflammation, such as arthritis or appendicitis. Inflammatory pain often responds well to non-opioid analgesics, especially NSAIDs, which have anti-inflammatory properties. Morphine can be used to relieve inflammatory pain in some cases, but it may not be necessary or optimal to use opioids for this type of pain, as they do not have anti-inflammatory effects and may cause more side effects and risks than non-opioid analgesics. Therefore, choice E is incorrect.
Patient Data
History and Physical
The client is a 42-year-old female who had a right above-the-knee amputation for osteomyelitis. The client has a drain in place and a surgical dressing that will need to be changed by the surgeon on post-op day 1.
Nurses Notes
1400: Started continuous morphine in the left antecubital vein peripheral intravenous line. No redness, edema, or bleeding noted at the site.
Orders:
- Admit to the surgical floor
- Clear liquid diet, advance as tolerated
- Continuous cardiorespiratory monitoring
- Morphine 1 mg/hr intravenously
- Alert surgeon to signs of bleeding or infection in the surgical site
What actions should the nurse take to ensure safety during morphine administration? Select all that apply.
Explanation
Choice A reason:
Taking an initial respiratory rate is a necessary action to ensure safety during morphine administration, as morphine can cause respiratory depression, which is a potentially life-threatening side effect. The nurse should monitor the client's respiratory rate and oxygen saturation regularly and report any signs of respiratory distress or hypoxia to the physician. Therefore, choice A is correct.
Choice B reason:
Performing a 12-lead electrocardiogram is not a necessary action to ensure safety during morphine administration, as morphine does not have a significant effect on the cardiac rhythm or conduction. The nurse should monitor the client's heart rate and blood pressure regularly and report any signs of bradycardia, hypotension, or chest pain to the physician. Therefore, choice B is incorrect.
Choice C reason:
Suctioning the client to clear the airway is not a necessary action to ensure safety during morphine administration, as morphine does not cause excessive secretions or bronchospasm that would obstruct the airway. The nurse should assess the client's level of consciousness and gag reflex regularly and report any signs of sedation, confusion, or aspiration to the physician. Therefore, choice C is incorrect.
Choice D reason:
Having a manual resuscitation bag at the bedside is a necessary action to ensure safety during morphine administration, as morphine can cause respiratory depression that may require emergency intervention. The nurse should be prepared to administer oxygen and naloxone (an opioid antagonist) as ordered and perform rescue breathing or cardiopulmonary resuscitation if needed. Therefore, choice D is correct.
Choice E reason:
Asking the client about other medications she takes is a necessary action to ensure safety during morphine administration, as morphine can interact with other drugs that may enhance or reduce its effects or cause adverse reactions. The nurse should review the client's medication history and current medications and report any potential drug interactions or contraindications to the physician. Therefore, choice E is correct.
Choice F reason:
Restraining the client with soft restraints is not a necessary action to ensure safety during morphine administration, as morphine does not cause agitation or delirium that would warrant physical restraint. The nurse should provide a safe and comfortable environment for the client and report any signs of anxiety, hallucinations, or psychosis to the physician. Therefore, choice F is incorrect.
Patient Data
History and Physical
The client is a 42-year-old female who had a right above-the-knee amputation for osteomyelitis. The client has a drain in place and a surgical dressing that will need to be changed by the surgeon on post-op day 1.
Nurses Notes
1400: Started continuous morphine in the left antecubital vein peripheral intravenous line. No redness, edema, or bleeding noted at the site. Vital signs are heart rate 77 bpm, blood pressure 118/74 mmHg, respiratory rate 16 breaths/min.
Orders:
- Admit to the surgical floor
- Clear liquid diet, advance as tolerated
- Continuous cardiorespiratory monitoring
- Morphine 1 mg/hr intravenously
- Alert surgeon to signs of bleeding or infection in the surgical site
What other medications would the nurse expect the surgeon to prescribe along with morphine? Select all that apply.
Explanation
Choice A reason:
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that has analgesic, anti-inflammatory, and antipyretic effects. Ibuprofen can be prescribed along with morphine to enhance the pain relief and reduce the inflammation caused by the surgery. Ibuprofen can also reduce the opioid requirement and the risk of opioid-related side effects, such as nausea, constipation, and respiratory depression. Therefore, choice A is correct.
Choice B reason:
Propofol is a short-acting intravenous anesthetic agent that induces and maintains anesthesia and sedation. Propofol is not prescribed along with morphine for post-operative pain management, as it is not an analgesic and has a high risk of hypotension, bradycardia, and respiratory depression. Propofol is only used in controlled settings, such as the operating room or the intensive care unit, under close monitoring and supervision. Therefore, choice B is incorrect.
Choice C reason:
Methadone is a long-acting synthetic opioid that has analgesic and opioid substitution effects. Methadone is not prescribed along with morphine for post-operative pain management, as it is not indicated for acute pain and has a high risk of accumulation, overdose, and addiction. Methadone is mainly used for chronic pain or opioid dependence treatment, under strict regulation and monitoring. Therefore, choice C is incorrect.
Choice D reason:
Senna is a stimulant laxative that increases the intestinal motility and promotes bowel movements. Senna can be prescribed along with morphine to prevent or treat constipation, which is a common side effect of opioids. Senna can improve the comfort and quality of life of the client who is receiving opioid therapy. Therefore, choice D is correct.
Choice E reason:
Docusate sodium is a stool softener that increases the water content and softness of the stool. Docusate sodium can be prescribed along with morphine to prevent or treat constipation, which is a common side effect of opioids. Docusate sodium can improve the comfort and quality of life of the client who is receiving opioid therapy. Therefore, choice E is correct.
Choice F reason:
Naloxone is an opioid antagonist that reverses the effects of opioids by displacing them from their receptors. Naloxone is not prescribed along with morphine for post-operative pain management, as it would counteract the analgesic effect of morphine and cause withdrawal symptoms. Naloxone is only used in emergency situations, such as opioid overdose or respiratory depression, as a rescue medication. Therefore, choice F is incorrect.
Patient Data
History and Physical
The client is a 42-year-old female who had a right above-the-knee amputation for osteomyelitis. The client has a drain in place and a surgical dressing that will need to be changed by the surgeon on post-op day 1.
Nurses Notes
1400: Started continuous morphine in the left antecubital vein peripheral intravenous line. No redness, edema, or bleeding noted at the site. Vital signs are heart rate 77 bpm, blood pressure 118/74 mmHg, respiratory rate 16 breaths/min.
Orders:
- Admit to the surgical floor
- Clear liquid diet, advance as tolerated
- Continuous cardiorespiratory monitoring
- Morphine 1 mg/hr intravenously
- Alert surgeon to signs of bleeding or infection in the surgical site
1500:
- Docusate sodium 240 mg orally every am
- Naloxone 2 mg intravenously as needed for respiratory depression
- Ibuprofen 600 mg orally every 6 hours
The charge nurse places a fall precautions sign on the client's door. What side effects of morphine could contribute to this client's fall risk? Select all that apply.
Explanation
Choice A reason:
Seizures are not a common side effect of morphine, and they are unlikely to contribute to this client's fall risk. Seizures can occur in rare cases of morphine overdose, hypersensitivity, or withdrawal, but they are not expected in a client who is receiving a continuous and monitored dose of morphine. Therefore, choice A is incorrect.
Choice B reason:
Nausea is a common side effect of morphine, and it can contribute to this client's fall risk. Nausea can cause the client to feel dizzy, weak, or unsteady, and it can also impair the client's appetite and hydration status. Nausea can also trigger vomiting, which can increase the risk of aspiration or dehydration. Therefore, choice B is correct.
Choice C reason:
Orthostatic hypotension is a common side effect of morphine, and it can contribute to this client's fall risk. Orthostatic hypotension is a sudden drop in blood pressure that occurs when the client changes position from lying to sitting or standing. Orthostatic hypotension can cause the client to feel faint, dizzy, or lightheaded, and it can also increase the risk of syncope (loss of consciousness) or cardiac arrhythmias. Therefore, choice C is correct.
Choice D reason:
Sedation is a common side effect of morphine, and it can contribute to this client's fall risk. Sedation can cause the client to feel sleepy, drowsy, or confused, and it can also impair the client's alertness and coordination. Sedation can also reduce the client's ability to respond to stimuli or alarms, and it can increase the risk of respiratory depression or coma. Therefore, choice D is correct.
Choice E reason:
Euphoria is a common side effect of morphine, and it can contribute to this client's fall risk. Euphoria is a feeling of intense happiness or well-being that is induced by the activation of opioid receptors in the brain. Euphoria can cause the client to feel overconfident, impulsive, or reckless, and it can also impair the client's judgment and perception of reality. Euphoria can also increase the risk of psychological dependence or addiction. Therefore, choice E is correct.
Choice F reason:
Itching is a common side effect of morphine, and it can contribute to this client's fall risk. Itching is caused by the release of histamine from mast cells in response to the stimulation of opioid receptors in the skin. Itching can cause the client to scratch excessively, which can damage the skin and increase the risk of infection. Itching can also distract the client from other sensations or warnings, and it can reduce the client's comfort and quality of life. Therefore, choice F is correct.
Choice G reason:
Urinary retention is a common side effect of morphine, and it can contribute to this client's fall risk. Urinary retention is the inability to empty the bladder completely or voluntarily due to the inhibition of bladder contraction by opioid receptors in the urinary tract. Urinary retention can cause the client to feel pain, discomfort, or urgency in the lower abdomen, and it can also increase the risk of urinary tract infection or kidney damage. Urinary retention can also prompt the client to attempt to get out of bed without assistance or supervision, which can increase the risk of falling. Therefore, choice G is correct.
Patient Data
History and Physical
The client is a 42-year-old female who had a right above-the-knee amputation for osteomyelitis. The client has a drain in place and a surgical dressing that will need to be changed by the surgeon on post-op day 1.
Nurses Notes
1400: Started continuous morphine in the left antecubital vein peripheral intravenous line. No redness, edema, or bleeding noted at the site. Vital signs: heart rate 77 bpm, blood pressure 118/74 mmHg, respiratory rate 16.
1800: Vital signs: heart rate 79 bpm, blood pressure 114/78 mmHg, respiratory rate 14.
1900: Responded to an alarm in the room. The client is not responsive. Her respiratory rate is 5 bpm. Her heart rate is 92 bpm. Her pupils are pinpoint.
Orders:
- Admit to the surgical floor
- Clear liquid diet, advance as tolerated
- Continuous cardiorespiratory monitoring
- Morphine 1 mg/hr intravenously
- Alert surgeon to signs of bleeding or infection in the surgical site
- Docusate sodium 240 mg orally every am
- Naloxone 2 mg intravenously as needed for respiratory depression
- Ibuprofen 600 mg orally every 6 hours
What should the nurse do immediately? Select all that apply.
Explanation
Choice A: Printing an electrocardiogram strip is not a priority in this situation. The client is not responsive and has a low respiratory rate, which indicates a possible overdose of morphine. The nurse should focus on reversing the effects of the opioid and maintaining the client's airway and circulation.
Choice B: Providing rescue breaths with a manual ventilation bag is a correct and urgent action. It can supply oxygen to the client until naloxone takes effect and restore normal breathing.
Choice C: Giving naloxone 2 mg intravenously is a correct and urgent action. Naloxone is an opioid antagonist that can block the effects of morphine and reverse respiratory depression.
Choice D: This can help increase the patient’s oxygen levels, which may be low due to the decreased respiratory rate.
Choice E: Performing chest compressions is not a correct or urgent action. It is only indicated if the client has no pulse or signs of life. It can also cause harm if the client has a heartbeat.
Choice F: Calling for rapid response is a correct and urgent action. Rapid response is a team of health care professionals that can assist in emergency situations and provide advanced care.
Patient Data
History and Physical
The client is a 42-year-old female who had a right above-the-knee amputation for osteomyelitis. The client has a drain in place and a surgical dressing that will need to be changed by the surgeon on post-op day 1.
Nurses Notes
1400: Started continuous morphine in the left antecubital vein peripheral intravenous line. No redness, edema, or bleeding noted at the site.
Vital signs: heart rate 77 bpm, blood pressure 118/74 mmHg, respiratory rate 16.
1800: Vital signs: heart rate 79 bpm, blood pressure 114/78, respiratory rate 14 bpm.
1900: Responded to an alarm in the room. The client is not responsive. Her respiratory rate is 5 bpm. Her heart rate is 92 bpm. Her pupils are pinpoint.
Orders:
- Admit to the surgical floor
- Clear liquid diet, advance as tolerated
- Continuous cardiorespiratory monitoring
- Morphine 1 mg/hr intravenously
- Alert surgeon to signs of bleeding or infection in the surgical site
1500:
- Docusate sodium 240 mg orally every am
- Naloxone 2 mg intravenously as needed for respiratory depression
- Ibuprofen 600 mg orally every 6 hours
For each statement, click to indicate whether the statements by the student nurse indicate understanding or no understanding of naloxone.
Explanation
Choice A reason: This statement indicates understanding of naloxone. Naloxone is an opioid antagonist that can reverse the effects of opioid overdose, such as respiratory depression, sedation, and hypotension. Naloxone can be administered by different routes, depending on the availability and urgency of the situation. Intravenous, intramuscular, and subcutaneous routes are all acceptable ways to give naloxone.
Choice B reason: This statement also indicates understanding of naloxone. Naloxone works best on pure agonist opioids, such as morphine, heroin, and fentanyl. These opioids bind to the same receptors as naloxone, but naloxone has a higher affinity and can displace them. Naloxone is less effective on partial agonist or mixed agonist-antagonist opioids, such as buprenorphine and pentazocine. These opioids have lower intrinsic activity or antagonize some receptors, making them less susceptible to naloxone.
Choice C reason: This statement indicates no understanding of naloxone. Naloxone is not a harmless drug that can be given repeatedly without consequences. Naloxone has a short half-life of about 30 to 90 minutes, which means it can wear off before the opioid does. This can cause the patient to relapse into respiratory depression and require repeated doses of naloxone. However, giving too many doses of naloxone can also cause adverse effects, such as agitation, hypertension, tachycardia, pulmonary edema, and seizures. Therefore, naloxone should be given cautiously and titrated to the minimum effective dose to reverse respiratory depression.
Choice D reason: This statement indicates no understanding of naloxone. Naloxone will affect the client's level of pain by blocking the analgesic effects of opioids. This can cause the patient to experience acute pain and distress, especially if they have a chronic pain condition or a surgical wound. Naloxone should not be used to treat opioid-induced sedation or pruritus without respiratory depression, as this will unnecessarily expose the patient to pain and suffering.
Choice E reason: This statement indicates no understanding of naloxone. When given IV, naloxone starts working immediately, but it does not last several hours. As mentioned earlier, naloxone has a short half-life and can be eliminated from the body quickly. The duration of action of naloxone depends on the dose, route, and frequency of administration, as well as the type, dose, and route of the opioid involved. Generally, naloxone lasts for about 30 to 90 minutes when given IV, which may not be enough to counteract the longer-lasting effects of some opioids. Therefore, continuous monitoring and repeated doses of naloxone may be needed until the opioid is cleared from the system.
Patient Data
History and Physical
The client is a 75-year-old female who was admitted to the preop area to prepare for pacemaker insertion. She states that she needs this procedure because her heart rate has been very low, she feels tired all the time, and she has fainted once due to low heart rate. She has a history of worsening symptomatic bradycardia and atrial fibrillation controlled by medication. She has been off anticoagulants for four days to prepare for the procedure.
Nurses' Notes
0700: Labs were drawn and completed during a preadmission visit. After changing clothes and settling into bed, she was placed on continuous monitoring. Admission process was completed.
0800: A PIV was started in her right antecubital with a 20-gauge intracath. IVF of NS was started at 50 mL/hr. The cardiac surgeon came to see the client and answer her questions about the procedure.
0830: The client reports no known allergies. Vancomycin 1 gram in 250 mL NS was started at 125 mL/hr as endocarditis prophylaxis.
0840: The client was awaiting transfer to OR. Vancomycin was infusing at 125 mL/hr.
0845: The client says, "I don't feel well." Assessment reveals dizziness, headache, burning sensation on extremities, and red color on face and extremities. Blood pressure is 108/46 mmHg. Vancomycin infusion was stopped. The surgeon was notified.
0850: The client has flushing and redness over her entire body with hives developing. She complains of feeling hot and nauseous. Cool cloths were applied to her face and extremities. She is restless in bed. IVF of NS is running.
Orders:
1140
- Diphenhydramine 25 mg IV now
- Methylprednisolone 100 mg IV now
The nurse is implementing the plan of care.
For each body system, select to specify the potential nursing intervention that would be appropriate for the care of the client. Each body system may support more than one potential nursing intervention. Each category must have at least one response option selected.
Explanation
Body System: Respiratory
The correct choice is A
Choice A: Assess lung sounds This is the correct choice because the client may have developed an allergic reaction to vancomycin, which can cause bronchospasm and wheezing. Assessing lung sounds can help the nurse monitor the client’s respiratory status and intervene if needed.
Choice B: Provide a calm environment This is not the correct choice because providing a calm environment is not specific to the respiratory system. It may help the client feel more comfortable, but it does not address the potential respiratory complications of an allergic reaction.
Choice C: Pain medication This is not the correct choice because pain medication is not related to the respiratory system. The client did not report any pain, and pain medication may have adverse effects on the respiratory system, such as respiratory depression.
Choice D: Chest x-ray This is not the correct choice because a chest x-ray is not indicated for the client at this time. A chest x-ray is a diagnostic test that can show abnormalities in the lungs, such as pneumonia or pleural effusion. However, the client’s symptoms are more likely caused by an allergic reaction, which would not be visible on a chest x-ray.
Body System: Cardiovascular
The correct answer is A, B, and C. Here are the explanations for each choice:
Choice A: Monitor vital signs continuously. This is a correct and appropriate nursing intervention for the cardiovascular system. The client may have hypotension, tachycardia, or arrhythmias due to anaphylaxis or the effects of medications. Continuous monitoring can help detect any changes and guide interventions accordingly .
Choice B: Provide warmth. This is also a correct and appropriate nursing intervention for the cardiovascular system. The client may lose heat due to vasodilation, sweating, or exposure during the procedure. Providing warmth can help prevent hypothermia and shivering, which can increase oxygen demand and worsen cardiac function. Providing warmth can also improve comfort and reduce anxiety .
Choice C: Defibrillator at bedside. This is another correct and appropriate nursing intervention for the cardiovascular system. The client is at risk of cardiac arrest due to anaphylaxis, bradycardia, or pacemaker malfunction. Having a defibrillator at bedside can facilitate prompt resuscitation if needed.
Choice D: ECHO. This is an incorrect and inappropriate nursing intervention for the cardiovascular system. ECHO is a diagnostic test that uses ultrasound waves to create images of the heart and its structures. It can help evaluate the client’s cardiac function, valve function, and presence of any complications such as pericardial effusion or tamponade. However, this is not a priority intervention for the client who is experiencing an anaphylactic reaction and needs immediate treatment to stabilize her condition. ECHO can be done later after the client recovers from the acute episode.
Body System: Immunological
The correct answer is **A and D**.
- Choice A: Administer antihistamine. This is a correct and appropriate nursing intervention for the immunological system. The client is having an anaphylactic reaction to vancomycin, which is a type of hypersensitivity reaction mediated by IgE antibodies. Antihistamines, such as diphenhydramine, can block the effects of histamine, which is a major mediator of allergic inflammation and symptoms. Antihistamines can help reduce itching, hives, flushing, and bronchoconstriction¹².
- Choice B: IV fluids. This is an incorrect and inappropriate nursing intervention for the immunological system. IV fluids are not directly related to the immune response or the allergic reaction. IV fluids are mainly used to maintain hydration, electrolyte balance, and blood pressure. However, IV fluids may be indicated for the client as part of the cardiovascular or renal system interventions³.
- Choice C: Assess rash. This is an incorrect and inappropriate nursing intervention for the immunological system. Assessing rash is not a specific intervention for the immune response or the allergic reaction. Assessing rash is part of the general assessment of the client's skin condition, which may reflect other factors such as infection, inflammation, or drug toxicity. However, assessing rash may be helpful to monitor the severity and progression of the allergic reaction and the effectiveness of the treatment⁴.
- Choice D: Administer steroid. This is a correct and appropriate nursing intervention for the immunological system. The client is having an anaphylactic reaction to vancomycin, which is a type of hypersensitivity reaction mediated by IgE antibodies. Steroids, such as methylprednisolone, can suppress the immune system and reduce the production of inflammatory mediators, such as cytokines and prostaglandins. Steroids can help decrease swelling, inflammation, and tissue damage¹².
A client receives a new prescription for somatropin. Which information provided by the client indicates a need for further education by the nurse?
Explanation
Choice A reason: Storing unused vials at room temperature is incorrect information that indicates a need for further education by the nurse, because somatropin is a growth hormone that should be stored in the refrigerator (2°C to 8°C) until use. Exposure to heat or light can degrade the medication and reduce its effectiveness.
Choice B reason: Rotating injection sites to minimize discomfort is correct information that does not indicate a need for further education by the nurse, because somatropin is administered subcutaneously and repeated injections at the same site can cause skin irritation, bruising, or infection.
Choice C reason: Discarding the medication if the solution is cloudy is correct information that does not indicate a need for further education by the nurse, because somatropin is a clear and colorless solution that should not be used if it appears cloudy, discolored, or contains particles. This may indicate contamination or degradation of the medication.
Choice D reason: Administering the medication subcutaneously is correct information that does not indicate a need for further education by the nurse, because somatropin is a growth hormone that is given by subcutaneous injection using a syringe or a pen device. Subcutaneous injection allows for better absorption and bioavailability of the medication.
Sign Up or Login to view all the 31 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

