RN MATERNAL HEALTH 2019
Total Questions : 13
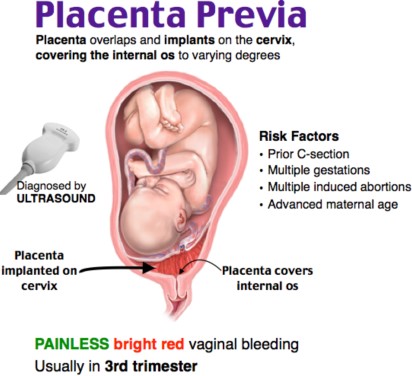
Showing 13 questions, Sign in for moreA nurse is caring for a client who has a placenta previa. Which of the following findings should the nurse expect?
Explanation
A. Uterine hypertonicity is more often associated with conditions like uterine tachysystole during labor.
B. Painless, vaginal bleeding
Placenta previa is a condition where the placenta partially or completely covers the cervix. The hallmark sign is painless vaginal bleeding, typically occurring in the second or third trimester of pregnancy. This bleeding can be severe and life-threatening and requires immediate medical attention.
C. A firm, rigid abdomen might be seen in cases of uterine rupture, but it's not a characteristic finding in placenta previa.
D. A persistent headache is not a direct symptom of placenta previa but could be related to other pregnancy complications like preeclampsia.
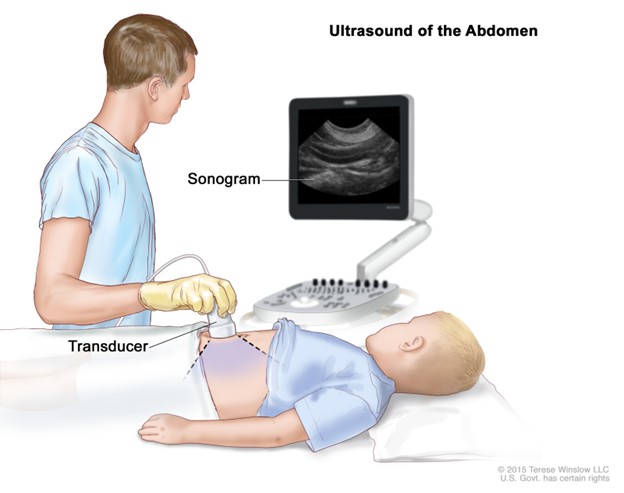
A nurse is providing teaching to a client who is primigravid and is scheduled to have an abdominal ultrasound. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
A. "I won't apply perfumed lotion to my abdomen before the test."
- This statement is incorrect. Applying perfumed lotion to the abdomen is not recommended before an ultrasound, as it can interfere with the ultrasound gel's ability to make good contact with the skin. However, the client didn't choose this statement.
B. "I need to take a stool softener the night before the test."
- This statement is incorrect. Taking a stool softener is not necessary for an abdominal ultrasound. Stool softeners are usually used to relieve constipation or prepare for certain types of gastrointestinal procedures, not for abdominal ultrasounds.
C. "I can't have anything to eat after midnight."
- This statement is incorrect. Fasting after midnight is typically required for procedures that involve anesthesia or sedation, but it's not necessary for an abdominal ultrasound. You can usually eat normally before this type of ultrasound.
D. "I will drink water before the test until my bladder feels full."
- This statement is correct. Drinking water to fill the bladder before the test is often part of the preparation for an abdominal ultrasound. A full bladder can help provide better images of the pelvic organs. This is the statement that indicates an understanding of the teaching.
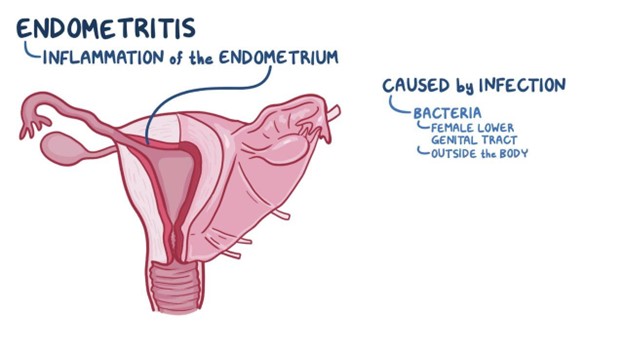
A nurse is assessing a client who is 6 hr postpartum and has endometritis. Which of the following findings should the nurse expect?
Explanation
A. Scant lochia: Endometritis can cause increased lochia (vaginal discharge) that may be foul-smelling.
B. WBC count 9,000/mm3: An elevated white blood cell (WBC) count is usually seen in cases of infection, so this finding doesn't rule out endometritis.
C. Uterine tenderness: Endometritis is an infection of the uterine lining, which often results in uterine tenderness or pain.
D. Temperature 37.4°C (99.3°F): Although a slightly elevated temperature might be seen in endometritis, a higher fever is more common.
A nurse is caring for a client who is at 30 weeks of gestation. The nurse should plan to Immunize the client with which of the following vaccines? (Select all that apply.)
Explanation
A. Tdap (Tetanus, Diphtheria, Pertussis) Vaccine: Tdap is usually recommended for pregnant individuals between 27 and 36 weeks of gestation during each pregnancy. This vaccine provides protection against pertussis (whooping cough) for both the pregnant person and the newborn.
B. Varicella (Chickenpox) Vaccine: If a pregnant person is not immune to chickenpox, they should receive the varicella vaccine after giving birth, as it is a live vaccine and generally not recommended during pregnancy.
C. Human Papillomavirus (HPV) Vaccine: HPV vaccines are not routinely given during pregnancy. The vaccine is typically recommended for eligible individuals before pregnancy or after childbirth.
D. Measles, Mumps, and Rubella (MMR) Vaccine: If a pregnant person is not immune to measles, mumps, and rubella, they should receive the MMR vaccine after giving birth, as it is a live vaccine and generally not recommended during pregnancy.
E. Inactivated Influenza (Flu) Vaccine: It is generally recommended that pregnant individuals receive the inactivated influenza vaccine during flu season, regardless of their gestational age. This helps protect both the pregnant person and their newborn from influenza-related complications.
A nurse is caring for a client who is receiving oxytocin to induce labor. The nurse should discontinue the oxytocin if which of the following occurs?
Explanation
A. "Moderate variability of the fetal heart rate" is a reassuring sign, indicating that the fetus is tolerating labor well. It does not warrant discontinuing oxytocin.
B. "Nonrepetitive early decelerations" are also a reassuring sign and are typically not an indication to discontinue oxytocin. Early decelerations are typically benign and related to head compression during contractions.
C. "Six contractions in 10 min" may be within the acceptable range for uterine activity during labor. However, it's important to assess the duration and intensity of these contractions as well.
D. "Contractions last 60 seconds" on their own may not be an indication to discontinue oxytocin. The nurse should also assess the frequency and intensity of contractions to determine if they are causing uterine hyperstimulation. Uterine Hyperstimulation Occurs: Uterine hyperstimulation is defined by an excessive frequency, duration, or intensity of contractions. Generally, contractions that occur more frequently than 5 contractions in 10 minutes (one every 2 minutes) or contractions that last longer than 60-90 seconds can be concerning.
A nurse is assessing a client who is 6 hr postpartum and has endometritis. Which of the following findings should the nurse expect?
Explanation
A. Scant lochia: Endometritis can cause increased lochia (vaginal discharge) that may be foul-smelling.
B. WBC count 9,000/mm3: An elevated white blood cell (WBC) count is usually seen in cases of infection, so this finding doesn't rule out endometritis.
C. Uterine tenderness: Endometritis is an infection of the uterine lining, which often results in uterine tenderness or pain.
D. Temperature 37.4°C (99.3°F): Although a slightly elevated temperature might be seen in endometritis, a higher fever is more common.
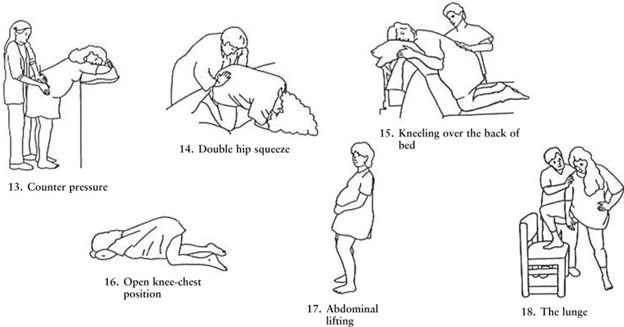
A nurse is teaching a client and her partner about the technique of counterpressure during labor. Which of the following statements by the nurse is appropriate?
Explanation
A. "Your partner will apply upward pressure on your lower abdomen between contractions" is not the correct technique for counterpressure. Counterpressure is specifically applied to the lower back.
B. "Your partner will apply steady pressure with a tennis ball to your lower back." Counterpressure, often referred to as "sacral pressure," is a technique used during labor to alleviate lower back pain and discomfort, which can be common during contractions. Using a tennis ball to apply steady pressure to the lower back can help relieve this discomfort.
C. "Your partner will apply pressure to the top of your uterus during contractions" is not counterpressure but rather fundal pressure, which is used to assess fetal position and aid in descent during the second stage of labor.
D. "Your partner will apply continuous, firm pressure between your thumb and index finger" does not relate to counterpressure during labor and is not a recognized technique for labor support.
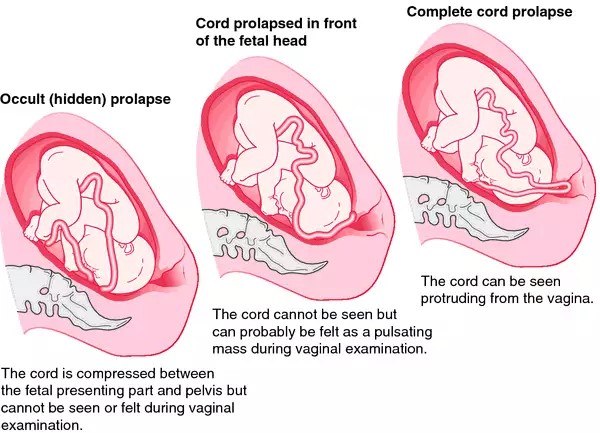
A nurse is caring for a client who reports spontaneous rupture of membranes. The nurse observes fetal bradycardia on the FHR tracing and notices that the umbilical cord is protruding. After calling for assistance and notifying the provider, which of the following actions should the nurse take next?
Explanation
A. Covering the exposed umbilical cord with a sterile, warm, saline-soaked towel helps prevent compression and drying of the cord. This can temporarily relieve pressure on the cord until more definitive interventions, such as a cesarean section, can be performed.
B. Administering oxygen via a nonrebreather mask is important but is not the first action to take. It should be done after covering the cord and ensuring adequate oxygenation for both the mother and the fetus.
C. Initiating an IV infusion is also important but not the first priority when there is a prolapsed cord. The priority is to relieve cord compression and restore fetal oxygenation.
D. Performing a vaginal examination by applying upward pressure on the presenting part can be harmful in this situation as it may push the presenting part further down and worsen cord compression. It should not be performed until the cord is covered and the situation is stabilized.
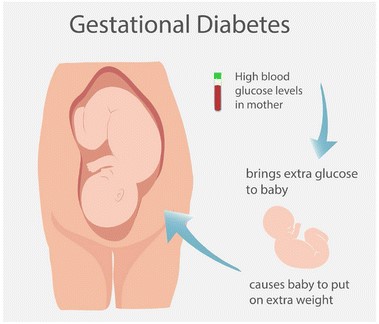
A nurse is caring for a client who is at 32 weeks of gestation and has gestational diabetes mellitus. Which of the following findings should the nurse report to the provider?
Explanation
A. The client has a fundal height of 38 cm.
A fundal height measurement significantly greater than the gestational age could indicate excessive fetal growth, which is a concern in gestational diabetes mellitus (GDM). It may suggest macrosomia (large baby) and requires further evaluation and management.
B. Nonpitting pedal edema is often seen in pregnancy and is typically not a concerning finding unless it's associated with other symptoms like hypertension.
C. A fasting blood glucose level of 90 mg/dL is within the target range for a client with GDM, and it indicates good blood sugar control.
D. Reporting 12 fetal movements in 1 hour is a positive finding, as it indicates fetal well-being and is a reassuring sign.
A nurse is caring for a client following a vaginal delivery of a term fetal demise. Which of the following statements should the nurse make?
Explanation
A. "You can bathe and dress your baby if you'd like to."
This statement gives the client the option to spend time with their baby if they wish to do so. It respects the client's autonomy and choice in how they want to handle this difficult situation.
B. Telling the client to name the baby may put unnecessary pressure on them during a challenging time.
C. Assuring the client that they can have another baby in the future might not be comforting at this moment, as they are grieving the loss of their current pregnancy.
D. Pressuring the client to hold the baby may not be appropriate, as everyone's grief process is different, and the client should be allowed to make their own choices regarding physical contact with the baby.
A nurse is assessing a full-term newborn upon admission to the nursery. Which of the following clinical findings should the nurse report to the provider?
Explanation
A. Transient circumoral cyanosis: This is a common finding in newborns and typically resolves without treatment.
B. The nurse should report the finding of "Single palmar creases" to the provider. Single palmar creases, also known as a single transverse palmar crease or simian crease, are associated with certain genetic syndromes like Down syndrome. It can be a significant clinical finding that warrants further evaluation and potential genetic testing to rule out any underlying conditions.
C. Rust-stained urine: This can occur due to the breakdown of red blood cells in the newborn's body during the first few days of life. It's usually benign and resolves on its own.
D. Subconjunctival hemorrhage: This is a common finding caused by pressure during childbirth and is typically benign, resolving without intervention.

A nurse is assisting the provider to administer a dinoprostone insert to induce labor for a client. Which of the following actions should the nurse take?
Explanation
A. Placing the client in a semi-Fowler's position for 1 hr after administration: While positioning can be important for some procedures, it is not a standard requirement for the administration of dinoprostone.
B. The nurse should verify that informed consent is obtained prior to the administration of any medication, including dinoprostone for labor induction. Informed consent is a legal and ethical requirement to ensure that the client understands the risks and benefits of the procedure or medication and gives their voluntary agreement.
C. Allowing the medication to reach room temperature prior to administration: The temperature of the medication is not typically a consideration for dinoprostone administration.
D. Instructing the client to avoid urinary elimination until after administration: This is not a standard requirement for dinoprostone administration, and it is important to encourage normal urinary elimination to prevent complications like urinary tract infections.
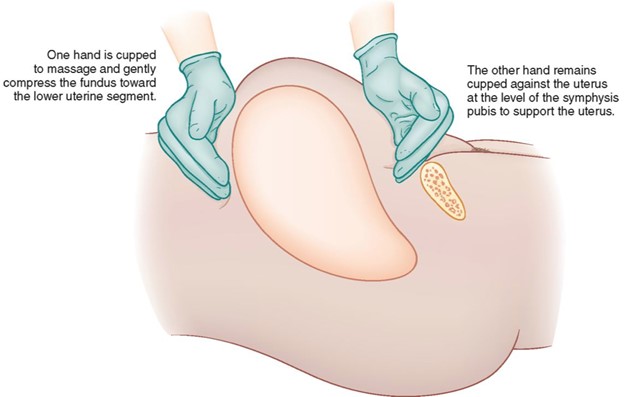
A nurse is preparing to perform a fundal massage for a postpartum client who is experiencing uterine atony. In which order should the nurse plan to perform the following actions? (Move the steps into the box on the right, placing them in the order of performance. Use all the steps.)
Explanation
Performing fundal massage for a postpartum client with uterine atony should be done in the following order:
Ask the client to lie on her back and with her knees flexed.
- Placing the client in the supine position with knees flexed helps relax the abdominal muscles and facilitates access to the uterus.
Position one hand around the top of the client's fundus and one hand just above the client's symphysis pubis.
- This step involves proper hand placement to locate and assess the position of the uterus.
Rotate the upper hand to massage the client's uterus while using slight downward pressure to compress the fundus.
- After proper hand placement, you can start the fundal massage with a rotating motion using slight downward pressure. This helps stimulate uterine contractions and control bleeding.
Observe the client's perineum for the passage of clots and the amount of bleeding.
- While massaging the uterus, it's essential to monitor the client's perineum for any signs of excessive bleeding or clot passage.
So, the correct order is: Ask the client to lie on her back and with her knees flexed > Position one hand around the top of the client's fundus and one hand just above the client's symphysis pubis > Rotate the upper hand to massage the client's uterus while using slight downward pressure to compress the fundus > Observe the client's perineum for the passage of clots and the amount of bleeding.
Sign Up or Login to view all the 13 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

