RN Maternal Newborn 2023
Total Questions : 63
Showing 25 questions, Sign in for moreA nurse is caring for a newborn Immediately following birth.
Exhibit 1
The nurse is assessing the newborn 24 hr later. How should the nurse interpret the findings?
For each finding, click to specify whether the finding is unrelated to the diagnosis, an indication that the client's condition is Improving, or an Indication that the client's condition is worsening.
Explanation
For the findings 24 hours later, the nurse should interpret them as follows:
Muscle tone: flaccid
Interpretation: Sign of potential improvement
Explanation: Flaccid muscle tone is normal in a newborn 24 hours after birth. This finding is indicative of the transitional period as the newborn adjusts to the extrauterine environment.
Respiration effort: good cry
Interpretation: Sign of potential improvement
Explanation: A good cry is a positive sign of effective respiratory effort, indicating that the newborn is adapting well to the postnatal environment. It suggests normal lung function.
Reflex irritability: cry
Interpretation: Sign of potential improvement
Explanation: Reflex irritability, demonstrated by crying, is a positive sign of neurological function. It indicates that the newborn is neurologically intact and responding appropriately.
Color: Consistent with genetic background
Interpretation: Unrelated to diagnosis
Explanation: The color being consistent with the genetic background is a normal finding and unrelated to the diagnosis. Newborns often exhibit variations in skin color that are genetically determined.
Heart rate: 140/min
Interpretation: Sign of potential improvement
Explanation: A heart rate of 140/min is within the normal range for a newborn. It is a positive finding, indicating that the cardiovascular system is functioning well.
Axillary temperature: 36.3°C (97.4°F)
Interpretation: Sign of potential improvement
Explanation: A normal axillary temperature is a positive finding, indicating that the newborn's thermoregulation is appropriate. It suggests that the newborn is maintaining a stable body temperature.
A nurse is caring for a client who is at 12 weeks of gestation and has hyperemesis gravidarum.
The nurse is assessing the client 24 hr later. How should the nurse interpret the findings?
For each finding click to specify whether the finding is unrelated to the diagnosis, a sign of potential improvement, or a sign of potential worsening condition.
Explanation
For the findings 24 hours later, the nurse should interpret them as follows:
Urinary output: 40 ml/hr
Interpretation: Sign of potential worsening condition
Explanation: A urinary output of 40 ml/hr is concerning and indicates potential dehydration. It is a sign of potential worsening of the client's condition, as it suggests inadequate fluid intake or ongoing fluid losses.
3+ ketones
Interpretation: Sign of potential worsening condition
Explanation: The presence of 3+ ketones in the urine suggests ongoing ketosis, which can occur in hyperemesis gravidarum due to starvation and the breakdown of fats for energy. It is a sign of potential worsening of the client's nutritional status.
Heart rate: 100/min
Interpretation: Sign of potential improvement
Explanation: A heart rate of 100/min is within the normal range. It can be interpreted as a sign of potential improvement, indicating that the client's cardiovascular system is maintaining an appropriate heart rate.
WBC count: 10,000/mm3
Interpretation: Unrelated to diagnosis
Explanation: The WBC count within the normal range (10,000/mm3) is unrelated to the diagnosis of hyperemesis gravidarum. It does not provide specific information about the client's condition in this context.
Urine specific gravity: 1.050
Interpretation: Sign of potential worsening condition
Explanation: A urine specific gravity of 1.050 is elevated and indicates concentrated urine. This finding is a sign of potential worsening of the client's dehydration status.
Urine pH: 5
Interpretation: Unrelated to diagnosis
Explanation: The urine pH of 5 is within the normal range and is unrelated to the diagnosis of hyperemesis gravidarum. It does not provide specific information about the client's condition in this context.
A nurse is caring for a newborn who was born at 39 weeks of gestation and is 36hr old.
Which of the following findings should the nurse report to the provider?
Select all that apply
Explanation
In the context of the newborn's information, the nurse should report the following findings to the provider:
A. Coombs test result:
Explanation: The Coombs test checks for the presence of antibodies that can destroy red blood cells. In the absence of information about any specific concern or risk factors, a Coombs test result may not be immediately necessary for a term newborn. The nurse should report this finding to the provider for clarification on why the test was performed.
D. Intake and output:
Explanation: The newborn has voided only once since birth. Infrequent voiding can be a concern, and the nurse should report this to the provider for further evaluation, as adequate urine output is important to assess renal function and hydration status.
G. Mucous membrane assessment:
Explanation: Mucous membrane color and moisture are important indicators of hydration. If there are abnormalities, such as pale or dry mucous membranes, the nurse should report this to the provider for further assessment.
H. Sclera color:
Explanation: The color of the sclera can indicate jaundice in a newborn. If the sclera color appears yellow or jaundiced, the nurse should report this finding to the provider for further evaluation.
The following findings are not typically of immediate concern in the given context:
B. Glucose level:
Explanation: While glucose levels are important in certain situations, there is no information suggesting a need for immediate concern about glucose levels in this case. The nurse can monitor blood glucose levels as part of routine care but does not need to report it without specific concerns.
C. Head assessment finding:
Explanation: The information does not provide details about any abnormal head assessment findings. If there are no specific concerns mentioned, the nurse may not need to report this finding unless there are abnormalities observed during routine assessments.
E. Respiratory rate:
Explanation: The respiratory rate is not highlighted as a concern in the given information. If there are no specific abnormalities or signs of respiratory distress, the nurse may not need to report this finding without additional information.
F. Heart rate:
Explanation: The heart rate is not highlighted as a concern, and a normal Apgar score was noted at 5 minutes. If there are no specific concerns or abnormal findings related to the heart rate, the nurse may not need to report this finding without additional information.
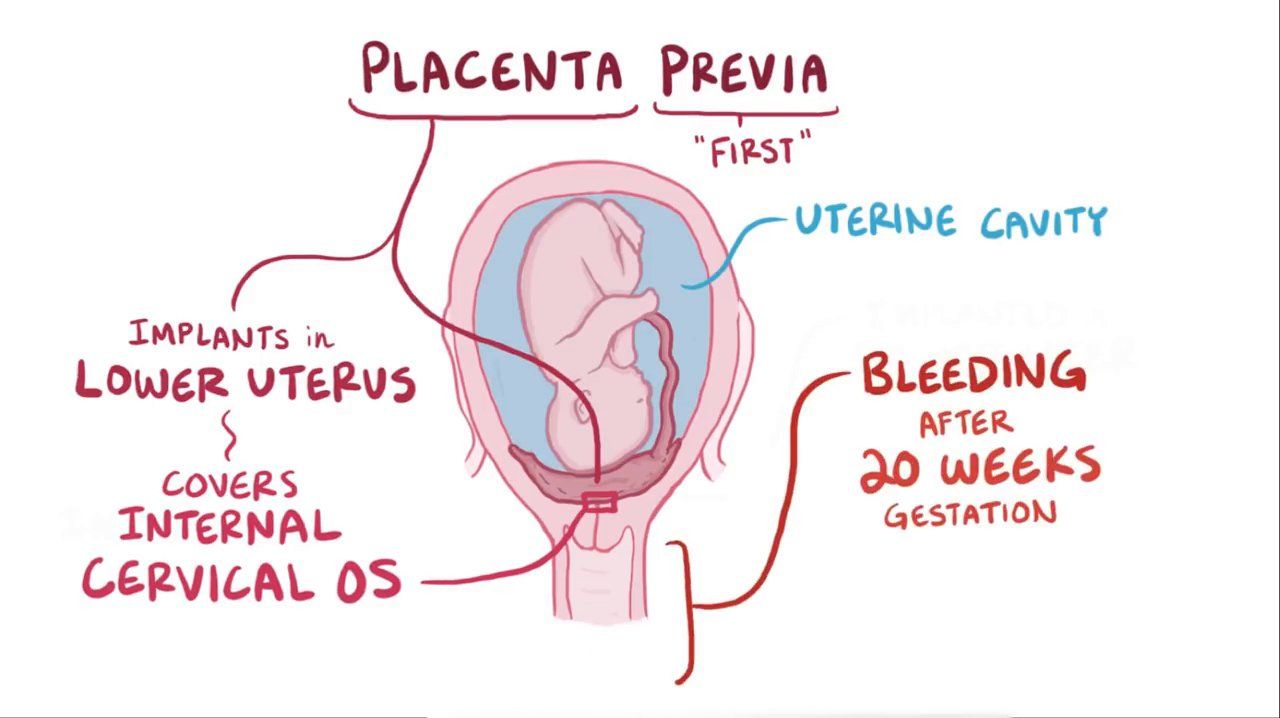
A nurse is caring for a client who is at 32 weeks of gestation and has complete placenta previa
Which of the following assessment findings requires immediate follow-up)
Select all that apply
Explanation
In the context of a client at 32 weeks of gestation with complete placenta previa, the following assessment findings require immediate follow-up:
A. Fetal heart rate:
Explanation: An elevated fetal heart rate (174/min) may be indicative of fetal distress. This finding requires immediate follow-up to assess the well-being of the fetus.
F. Vaginal bleeding:
Explanation: A moderate amount of bright red vaginal bleeding is a concerning sign, especially in the context of complete placenta previa. It indicates active bleeding, and immediate follow-up is necessary to assess the severity of the situation and the well-being of both the mother and the fetus.
C & D. Hemoglobin (Hgb) and Hematocrit (Hct):
Explanation: Hemoglobin and hematocrit levels are important indicators of blood loss. Given the vaginal bleeding, these values need immediate follow-up to assess the extent of maternal blood loss and the potential need for blood transfusion.
The following assessment findings do not require immediate follow-up in the given context:
B. Fundal height:
Explanation: Fundal height (33cm) is typically measured to assess fetal growth. While it's important to monitor, it may not be an immediate concern unless there are other signs of fetal distress.
E. Platelet count:
Explanation: While platelet count is important, it may not require immediate follow-up unless there is evidence of severe bleeding and a potential risk of disseminated intravascular coagulation (DIC). In this scenario, attention to Hgb and Hct is more urgent.
G & H. White Blood Cell (WBC) count and Red Blood Cell (RBC) count:
Explanation: WBC count and RBC count may be monitored but do not require immediate follow-up unless there are signs of infection or other complications not evident in the given information.
A nurse is caring for a term newborn who is 48 hr old
The nurse assessing the newborn 24 hr later. How should the nurse interpret the findings?
For each finding, click to specify whether the finding is unrelated to the diagnosis, a sign of potential improvement, or a sign of potential worsening condition.
Explanation
Transient strabismus:
Interpretation: Unrelated to diagnosis
Explanation: Transient strabismus (crossed eyes) is not necessarily related to the maternal history of opioid use or precipitous birth. It is a common finding in newborns and often resolves on its own without intervention.
Respiratory rate 70/min:
Interpretation: Sign of potential improvement
Explanation: A respiratory rate of 70/min is within the normal range for a newborn. This finding is a sign of potential improvement as it indicates that the newborn's respiratory function is within an expected range.
Continuous high-pitched cry:
Interpretation: Sign of potential worsening condition
Explanation: A continuous high-pitched cry can be a sign of potential distress or discomfort in a newborn. It may be associated with various conditions, including withdrawal symptoms related to maternal opioid use during pregnancy. This finding warrants further assessment.
Regurgitation:
Interpretation: Unrelated to diagnosis
Explanation: Regurgitation (spitting up) is a common occurrence in newborns and is not necessarily related to the maternal history of opioid use. It is often a normal physiological process in infants.
Loose stools:
Interpretation: Unrelated to diagnosis
Explanation: Loose stools can be a normal finding in newborns and may not be directly related to the maternal history of opioid use. It is not necessarily indicative of a worsening condition in this context.
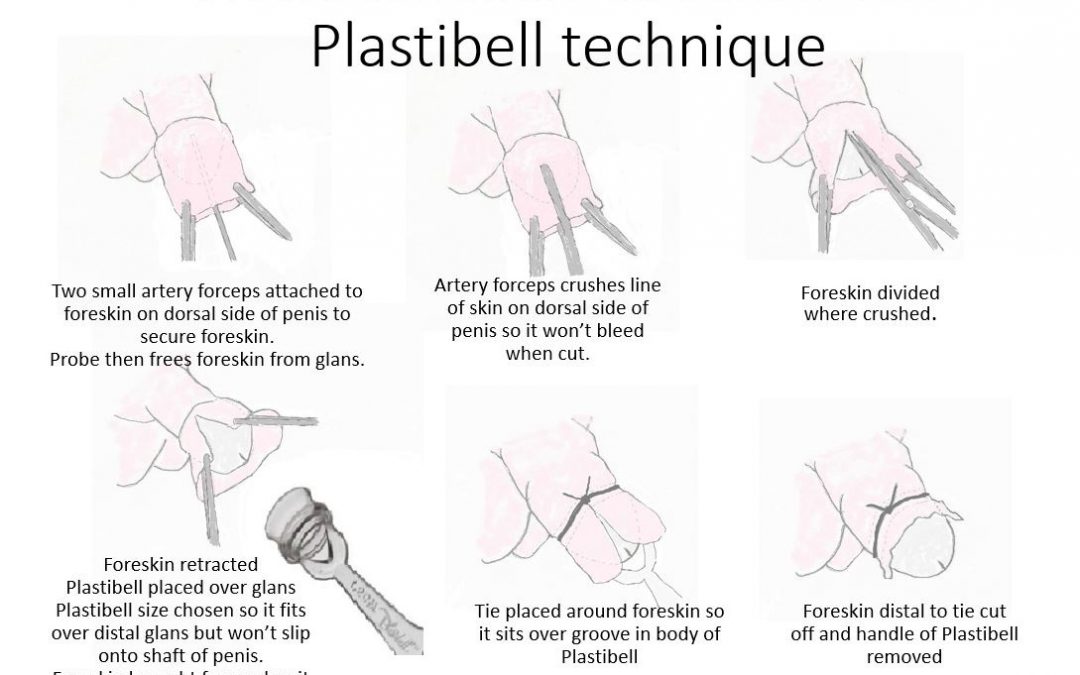
A nurse is providing teaching to the parents of a newborn about the Plastibell circumcision technique. Which of the following information should the nurse include?
Explanation
A. Yellow exudate will form at the surgical site in 24 hours: While some discharge or exudate is expected after the procedure, specifying a timeframe of 24 hours is not accurate. Parents should be informed that some exudate is normal, but they should follow specific instructions given by the healthcare provider.
B. The Plastibell will be removed 4 hours after the procedure: The Plastibell is not typically removed as quickly as 4 hours after the procedure. The timing of removal can vary and is usually determined by the healthcare provider based on the individual circumstances and healing progress.
C. Make sure the newborn’s diaper is snug: While keeping the diaper snug is generally recommended for comfort, it's not specific to the Plastibell circumcision technique. Parents should follow general diapering instructions and ensure they do not disrupt the Plastibell or cause any unnecessary pressure on the circumcision site.
D. Notify the provider if the end of your baby’s penis appears dark red
The Plastibell circumcision technique involves placing a plastic ring over the glans of the penis, leading to the separation of the foreskin. It's important for parents to be aware of signs of complications or issues. Notifying the provider if the end of the baby's penis appears dark red is crucial, as this may indicate a potential problem, such as excessive bleeding or infection.
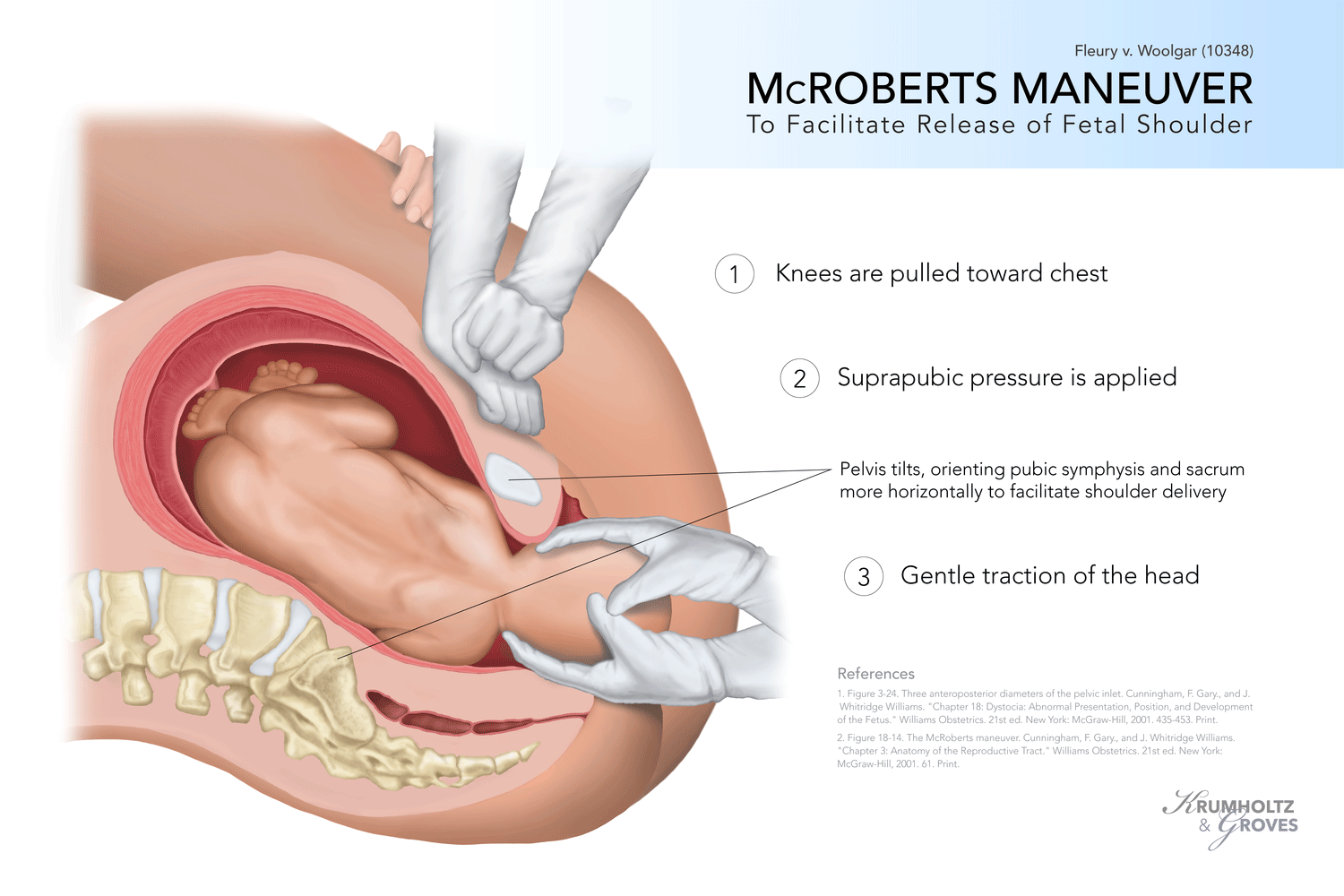
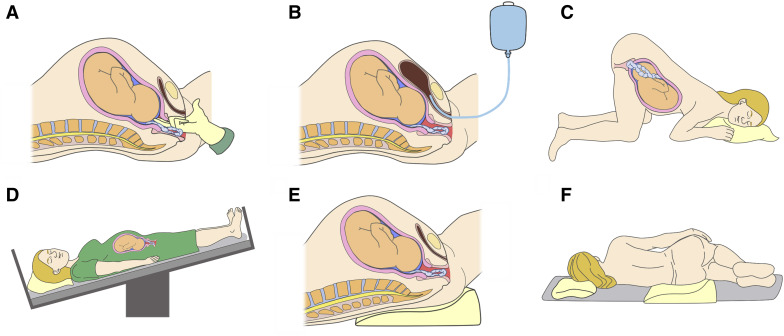
A nurse is caring for a client who is in the second stage of labor and is experiencing a shoulder dystocia. The provider instructs the nurse to perform the McRoberts maneuver. Which of the following actions should the nurse take?
Explanation
A. Move the client onto their hands and knees: This position is often used for the Gaskin maneuver, which involves positioning the mother on all fours to help resolve shoulder dystocia. However, the McRoberts maneuver specifically requires hyperflexing the legs toward the abdomen.
B. Press firmly on the client’s suprapubic area: This action is not part of the McRoberts maneuver. It is not the recommended technique for resolving shoulder dystocia.
C. Assist the client in pulling their knees toward their abdomen
The McRoberts maneuver involves hyperflexing the mother's legs toward her abdomen to widen the pelvic outlet. This repositions the pelvis, which can assist in dislodging the impacted shoulder of the baby during a shoulder dystocia.
D. Apply pressure to the client’s fundus: Applying pressure to the fundus can sometimes be used in other obstetric emergencies but is not part of the McRoberts maneuver for shoulder dystocia.
A nurse is providing teaching about the expected effects of magnesium sulfate to a client who is at 28 weeks of gestation and has preeclampsia. Which of the following responses by the nurse is appropriate?
Explanation
A. This medication increases cardiac output: Magnesium sulfate does not typically increase cardiac output. Its primary role in the context of preeclampsia is to prevent seizures and manage hypertension.
B. This medication stabilizes the fetal heart rate: While magnesium sulfate can have a relaxing effect on the uterus, which might indirectly influence fetal heart rate, its primary purpose in preeclampsia is seizure prevention rather than fetal heart rate stabilization.
C. The medication improves tissue perfusion: Magnesium sulfate primarily functions as an anticonvulsant and tocolytic (relaxes the uterus). While its effects on vasodilation can contribute to improved blood flow, the primary indication in preeclampsia is seizure prevention.
D. The medication prevents seizures
Magnesium sulfate is commonly used in the management of preeclampsia to prevent seizures (eclampsia), a serious complication of the condition. It has anticonvulsant properties and is the primary medication for seizure prophylaxis in pregnant individuals with preeclampsia.
A nurse is caring for a client who delivered by cesarean birth 6 hr ago. The nurse notes a steady trickle of vaginal bleeding that does not stop with fundal message. Which of the following actions should the nurse take?
Explanation
A. Administer 500 ml lactated Ringer's IV bolus:
This choice may be relevant in the context of postpartum hemorrhage, but the first step should be to assess the client's status, including urinary output. Administering fluids without a clear assessment may not address the underlying cause.
B. Replace the surgical dressing:
Vaginal bleeding after a cesarean birth is unlikely to be addressed by replacing the surgical dressing. This action may not address the root cause of the bleeding, which needs further assessment.
C. Apply an ice pack to the incision site:
Using an ice pack is not the appropriate intervention for postpartum bleeding. Ice is typically used for pain and swelling, not for controlling bleeding.
D. Evaluate urinary output:
This is the correct choice. Evaluating urinary output is crucial to assess the client's overall fluid status and kidney perfusion. In the context of postpartum bleeding, it helps determine if there is hypovolemia or other issues contributing to the bleeding. Adequate urinary output is a positive sign of organ perfusion.
A nurse is providing teaching to a postpartum client who has a prescription for a rubella immunization. Which of the following client statements indicates understanding of the teaching?
Explanation
A. I will receive a series of three immunizations, and each one will be a month apart: This statement is not accurate for rubella immunization. The MMR vaccine is usually administered as a single injection.
B. I should avoid becoming pregnant for at least 1 month following the immunization
Rubella immunization is typically administered as the measles, mumps, and rubella (MMR) vaccine. The statement indicating understanding reflects awareness of the importance of avoiding pregnancy for a certain period after receiving the rubella immunization due to potential risks to the developing fetus.
C. I should avoid breastfeeding for 2 weeks following the immunization: Breastfeeding is not a contraindication after receiving the rubella immunization. In fact, breastfeeding is generally not affected, and mothers can continue to breastfeed.
D. I will report joint pain that develops after the immunization to my provider immediately: Joint pain is a potential side effect of the rubella vaccine. Reporting joint pain to the provider is essential for monitoring and addressing any adverse reactions.
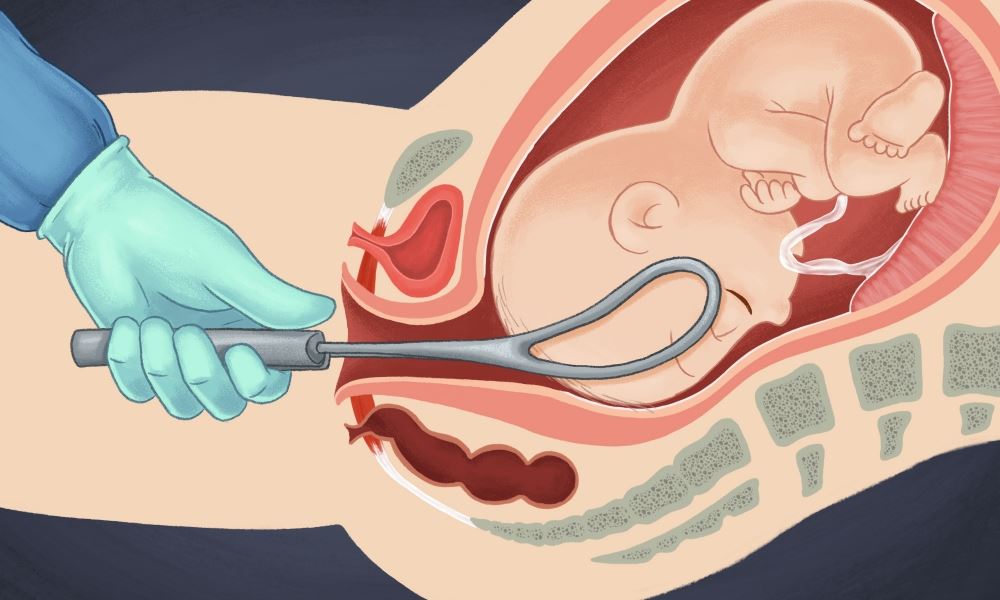
A nurse is assessing a newborn who was born via a forceps-assisted birth. Which of the following findings should the nurse identify as an injury caused by the forceps?
Explanation
A. Epicanthal folds: Epicanthal folds are the skin folds of the upper eyelid covering the inner corner of the eye. These folds are a normal anatomical variation and are not typically related to forceps-assisted births.
B. Depressed anterior fontanel: A depressed fontanel (the soft spot on a baby's head) might indicate dehydration or a potential concern but is not directly associated with forceps use during birth.
C. Facial asymmetry
Forceps-assisted births involve the use of forceps to aid in the delivery of the baby's head. Facial asymmetry can occur as a result of the pressure applied by the forceps during the birth process. This pressure might cause temporary facial bruising or swelling, leading to an asymmetrical appearance, particularly in the immediate post-birth assessment.
D. Uneven gluteal skinfolds: Uneven gluteal skinfolds, which refer to asymmetry in the skinfolds of the buttocks, are not typically linked to forceps use during delivery. This finding might be a normal variation or could indicate other unrelated conditions.
A nurse is providing teaching to a client about the purpose of her upcoming indirect Coombs' test. Which of the following statements should the nurse include in the teaching?
Explanation
A. This test determines if your baby is at risk for developing hypoglycemia after birth: The indirect Coombs' test is not related to assessing the risk of hypoglycemia in the baby. It specifically focuses on Rh sensitization.
B. The test will determine the amount of amniotic fluid around the fetus: The indirect Coombs' test does not assess the amount of amniotic fluid around the fetus. It is specifically aimed at detecting antibodies in the maternal blood.
C. The test studies blood flow in the fetus and placenta using ultrasound waves: This description is more indicative of a Doppler ultrasound or other tests that assess blood flow. The indirect Coombs' test is a blood test and does not involve ultrasound waves.
D. This test will detect the presence of Rh-positive antibodies in your blood
The indirect Coombs' test is performed during pregnancy to detect the presence of Rh antibodies in the maternal bloodstream. Rh antibodies can develop if an Rh-negative mother is carrying an Rh-positive baby, and there is a risk of hemolytic disease of the newborn (HDN) in subsequent pregnancies. The test helps identify if the mother has developed antibodies against Rh-positive blood, which could potentially affect the fetus.
A nurse is caring for a client who has a placenta previa. Which of the following findings should the nurse expect?
Explanation
A. Firm rigid abdomen: A firm and rigid abdomen is more indicative of uterine hypertonicity or uterine hyperstimulation, which is not typically associated with placenta previa. It may be seen in conditions such as uterine rupture.
B. Painless vaginal bleeding: Placenta previa is a condition where the placenta partially or completely covers the cervix, leading to painless vaginal bleeding. This bleeding occurs because as the cervix begins to dilate and efface in preparation for labor, blood vessels in the placenta may rupture, causing bleeding. Importantly, this bleeding is typically painless and can be sudden and profuse.
C. Uterine hypertonicity: Uterine hypertonicity refers to excessive, uncoordinated uterine contractions. Placenta previa is not generally associated with uterine hypertonicity; instead, it is more commonly linked with uterine relaxation and potential bleeding during contractions.
D. Persistent headache: A persistent headache is not a typical finding in placenta previa. However, it could be associated with conditions like preeclampsia, which might coexist with placenta previa but is a separate concern.
A nurse is caring for a client who has preeclampsia. Which of the following actions is the nurse's priority when implementing seizure precautions?
Explanation
A. Ensure the call button is within the client's reach: While having the call button within reach is important for the client to summon assistance quickly, the immediate priority is to prevent injury during a seizure. Padding the side rails takes precedence.
B. Place the suction equipment at the client’s bedside: While suction equipment may be necessary in certain situations, it is not the priority when implementing seizure precautions for a client with preeclampsia. The primary focus is on preventing injury during a seizure.
C. Pad the side rails of the client's bed : Seizure precautions aim to create a safe environment for a patient at risk of seizures. In the context of preeclampsia, the potential complication is eclampsia, which involves the occurrence of seizures. Padding the side rails of the bed is a priority because it helps prevent injury to the client during a seizure. In the event of a seizure, the client may move uncontrollably, and padding the side rails reduces the risk of injury if the client strikes the rails.
D. Dim the lights in the client’s room: Dimming the lights is not the priority when implementing seizure precautions. The focus should be on creating a safe environment to prevent injury during a seizure.
A nurse is providing instructions to a client who has chosen a diaphragm for birth control. Which of the following instructions should the nurse include?
No explanation
A nurse is caring for a postpartum client who recently had an indwelling urinary catheter removed. Which of the following findings indicates that the client is able to void effectively?
Explanation
A. The client urinates 30 ml/hr
Effective voiding after the removal of a urinary catheter involves the ability to produce an adequate amount of urine. A urine output of 30 ml per hour is within the normal range, indicating that the client is passing urine consistently, which is a positive sign of bladder function.
B. The uterine fundus is 2 cm above the umbilicus: The position of the uterine fundus is related to postpartum uterine involution and is not a direct indicator of effective voiding. It is more relevant to assessing the progress of the uterus returning to its pre-pregnancy state.
C. The bladder is distended upon palpation: A distended bladder is a sign of urinary retention, not effective voiding. If the bladder is distended, it indicates that the client may not be emptying the bladder properly.
D. The client does not feel the urge to urinate: Lack of urge to urinate could be a sign of urinary retention or impaired bladder function. A normal and healthy bladder function includes the sensation of the urge to void when the bladder is filling.
A nurse is providing teaching to a new parent about findings that require notification of the newborn's provider. Which of the following newborn clinical manifestations should the nurse include in the teaching?
Explanation
A. Yellowed sclera : Yellowed sclera (the white part of the eyes) can indicate jaundice in a newborn. Jaundice is caused by elevated levels of bilirubin and may signify various underlying conditions, including an excessive breakdown of red blood cells, liver immaturity, or other issues. Prompt notification of the healthcare provider is necessary to evaluate and manage jaundice appropriately.
B. Stooling after each breastfeeding: Stooling after each breastfeeding session is a common and expected occurrence in newborns. Breastfed babies often pass stools frequently, and this is generally not a cause for concern unless there are other associated symptoms.
C. Intermittent crossing of eyes: Occasional intermittent crossing of eyes can be normal in newborns. However, if persistent or accompanied by other concerning signs, it might require evaluation, but it's not typically an immediate concern.
D. Voids eight to ten times per day: A healthy newborn typically voids frequently throughout the day. Eight to ten times per day is within the expected range for a newborn's urinary output and might not be a cause for immediate concern.
A nurse on a labor and delivery unit is providing teaching to a client who plans to use hypnosis to control labor pain. Which of the following should the nurse include?
Explanation
A. Hypnosis can be beneficial if you practiced it during the prenatal period
Hypnosis techniques for pain management during labor can indeed be effective if practiced and learned before the onset of labor. Practicing hypnosis techniques during the prenatal period allows the individual to become more familiar with the process, enhancing their ability to use hypnosis as a pain management tool during labor.
B. Hypnosis does not work for controlling pain associated with labor: This statement is inaccurate. While hypnosis might not be effective for everyone, it can be a beneficial technique for managing labor pain in some individuals. It's important not to dismiss its potential efficacy for pain control in labor.
C. Synchronized breathing will be required during hypnosis: While breathing techniques are often incorporated into various pain management strategies during labor, such as in childbirth education classes or relaxation techniques, the requirement for synchronized breathing specifically during hypnosis is not universally accurate. Hypnosis techniques can vary, and they might or might not involve synchronized breathing.
D. Focusing on controlling body functions will be helpful during hypnosis: Hypnosis typically involves relaxation and focus but not necessarily the conscious control of body functions. The emphasis in hypnosis is often on relaxation, mental imagery, and suggestion rather than active control of physiological functions.
A nurse is caring for a client who is at 28 weeks of gestation and received no immunizations during childhood. Which of the following vaccines should the nurse plan to administer?
Explanation
A. Human papillomavirus (HPV): The HPV vaccine is generally not administered during pregnancy. It is recommended for routine vaccination before sexual activity begins to provide protection against certain types of HPV that can lead to cervical cancer and genital warts.
B. Varicella (chickenpox): The varicella vaccine is also typically not administered during pregnancy. If a woman is not immune to varicella and is planning pregnancy, vaccination is recommended before conception.
C. Rubella : The rubella vaccine is crucial for individuals who have not been immunized against rubella during childhood, especially in the context of pregnancy. Rubella (German measles) is a viral infection that can cause serious congenital abnormalities, known as congenital rubella syndrome, if a pregnant woman becomes infected. Administering the rubella vaccine during pregnancy is not appropriate, but vaccination before conception or in the postpartum period is recommended to prevent future rubella infections.
A nurse is caring for a client who is in labor and has spontaneous rupture of membranes. The nurse notes that the umbilical cord is protruding from the client's vagina. After calling for help, which of the following actions should the nurse take first?
Explanation
A. Use fingers to exert upward pressure on the presenting part
The priority in the case of a prolapsed umbilical cord is to relieve pressure on the cord to maintain blood flow to the fetus. The nurse should use sterile-gloved fingers to lift the presenting part of the fetus off the prolapsed cord. This action helps prevent compression of the umbilical cord, which could lead to fetal hypoxia and distress.
B. Administer a tocolytic medication: Tocolytic medications are used to inhibit uterine contractions. While tocolytics might be used in certain situations, the immediate concern with a prolapsed cord is to relieve pressure on it to maintain fetal blood flow.
C. Wrap the cord in a sterile towel and moisten with warm sterile normal saline: While covering the cord with a sterile towel and moistening it can help prevent drying and protect the cord, it is not the first priority. The primary concern is relieving pressure on the cord to prevent fetal compromise.
D. Apply oxygen via facemask to the client: Oxygen administration is important in managing fetal distress, but it is not the first action to take in the case of a prolapsed umbilical cord. The priority is to relieve pressure on the cord to maintain fetal oxygenation.
A nurse is reviewing the history of a client who is pregnant. Which of the following clinical data indicates the client is at risk for preterm delivery?
Explanation
A. Previous cervical cerclage
Cervical cerclage is a surgical procedure in which a stitch is placed in the cervix to reinforce it and reduce the risk of preterm birth. The fact that the client has had a previous cervical cerclage suggests a history of cervical insufficiency or a shortened cervix, which increases the risk of preterm delivery in subsequent pregnancies.
B. Previous delivery at 37 weeks gestation: A delivery at 37 weeks gestation is considered term. While it is on the earlier side of term, it does not inherently indicate an increased risk for preterm delivery.
C. Previous delivery of a newborn weighing 2.5 kg (5.5 lb): While low birth weight can be associated with preterm birth, the weight alone does not necessarily indicate a history of preterm delivery. Birth weight can be influenced by various factors.
D. Previous reactive non-stress test: A reactive non-stress test is a reassuring result, indicating that the fetus is responsive and generally doing well. It does not suggest a history or risk of preterm delivery.
A nurse is assessing the results of a nonstress test for an antepartal client at 35 weeks of gestation. Which of the following findings should indicate to the nurse the need for further diagnostic testing?
Explanation
A. Three fetal movements perceived by the client in a 20-min testing period: Perceiving fetal movements during the testing period is a positive finding and indicative of fetal well-being.
B. An increase in fetal heart rate to 150/min above the baseline of 140/min lasting 10 seconds in response to fetal movement within a 40-min testing period: This is considered a reassuring result in an NST, showing an appropriate acceleration in the fetal heart rate in response to fetal movement, which is a normal and positive finding.
C. Irregular contractions of 10 to 20 seconds in duration that are not felt by the client
During a nonstress test (NST), the presence of uterine contractions can sometimes interfere with the interpretation of fetal heart rate (FHR) patterns. If contractions occur but are not felt by the client, it can affect the accuracy of the test. Therefore, irregular contractions that are not felt by the client may prompt the need for further evaluation or testing to ensure accurate assessment of fetal well-being.
D. No late decelerations in the fetal heart rate noted with three uterine contractions of 60 seconds in duration within a 10-min testing period: Absence of late decelerations during uterine contractions is also a reassuring finding, indicating that the baby is tolerating the stress of contractions well.
A nurse is assessing a newborn who is 2 hr old. Which of the following findings is an indication of hypoglycemia? (Select all that apply.)
Explanation
A. Abdominal distention:
Explanation: Abdominal distention is more commonly associated with issues such as gas or gastrointestinal discomfort. It is not a typical sign of hypoglycemia.
B. Acrocyanosis:
Explanation: Acrocyanosis, a bluish discoloration of the extremities, is a common finding in newborns and is often unrelated to hypoglycemia. It is generally considered a normal response in the early hours or days of life.
C. Hypotonia:
Explanation: Hypotonia, or decreased muscle tone, can be associated with hypoglycemia. It may present as limpness or weakness in the newborn.
D. Jitteriness:
Explanation: Jitteriness, which is tremors or shakiness, can be a sign of hypoglycemia in a newborn. It is a result of the central nervous system responding to low blood glucose levels.
E. Temperature instability:
Explanation: Temperature instability, such as difficulty maintaining a stable body temperature, can be indicative of hypoglycemia. The newborn's ability to regulate temperature may be affected.
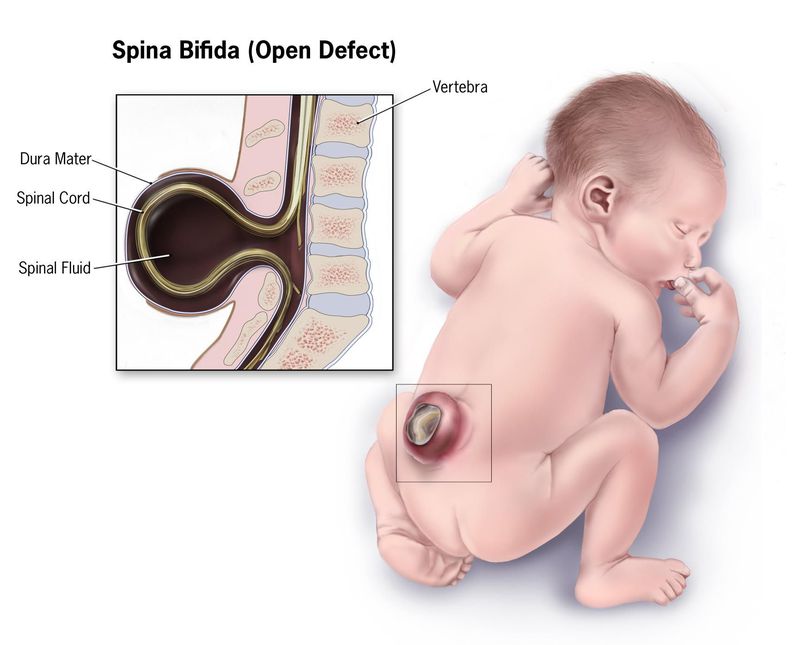
A nurse in planning care immediately following birth for a newborn who has a myelomeningocele that is leaking cerebrospinal fluid. Which of the following actions should the nurse include in the plan of care?
Explanation
A. Monitor the rectal temperature every 4 hours: While monitoring temperature is important, it is not the primary concern in a newborn with a myelomeningocele. The priority is to prevent infection and protect the exposed neural tissue.
B. Administer broad-spectrum antibiotics: Prophylactic antibiotics may be considered, but they are not the primary intervention. The definitive treatment is surgical closure to prevent infection and further damage to the exposed spinal cord.
C. Prepare for surgical closure after 72 hours
For a newborn with a myelomeningocele, the primary goal is to protect the exposed neural tissue and prevent infection. The plan of care typically involves surgical closure of the myelomeningocele within the first few days of life. The 72-hour timeframe is a common guideline, but the exact timing may vary based on the infant's overall health and clinical condition.
D. Cleanse the site with povidone-iodine: While maintaining cleanliness is important, cleansing the site with povidone-iodine is not the primary intervention. The main goal is to protect the exposed neural tissue and prevent infection through surgical closure.
A nurse in a clinic is caring for an adolescent client who requests a prescription for birth control. Which of the following questions should the nurse ask?
Explanation
A. Is your partner pressuring you to have sex?: While addressing issues of coercion or pressure in a relationship is important, this question may be more suited for a broader discussion about the client's overall well-being and relationships. It might be premature if the client is specifically seeking information about contraception.
B. What do you know about contraception?
This question aims to assess the adolescent's knowledge about contraception. Understanding the client's knowledge level is crucial for providing appropriate education and guidance on birth control options. It allows the nurse to tailor the information to the client's needs, address any misconceptions, and ensure informed decision-making regarding contraceptive choices
C. Why are you requesting a prescription for birth control?: This question may come across as judgmental or intrusive. It's important to approach the discussion in a non-judgmental and supportive manner. Focusing on the client's knowledge level allows for a more educational and collaborative conversation.
D. Are you sure your partner loves you?: This question delves into the emotional aspects of the client's relationship, which, while important, may not be directly relevant to the request for contraception. It's crucial to maintain a respectful and non-judgmental approach to avoid making the client feel uncomfortable.
Sign Up or Login to view all the 63 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

