RN Medical Surgical HESI
Total Questions : 44
Showing 25 questions, Sign in for moreA client with acute renal injury (AKI) weighs 110.3 pounds (50 kg) and has a potassium level of 6.7 mEq/L (6.7 mmol/L) is admitted to the hospital. Which prescribed medication should the nurse administer first?
Reference Range:
Potassium [3.5 to 5 mEq/L (3.5 to 5 mmol/L)]
Explanation
Choice A reason: Sodium polystyrene sulfonate is a medication that binds to excess potassium in the gastrointestinal tract and removes it from the body through feces. It is used to treat hyperkalemia, which is a high level of potassium in the blood. Hyperkalemia can cause cardiac arrhythmias and muscle weakness, and it is a common complication of AKI. Therefore, this medication should be administered first to lower the potassium level and prevent life-threatening complications.
Choice B reason: Sevelamer is a medication that binds to phosphorus in the gastrointestinal tract and removes it from the body through feces. It is used to treat hyperphosphatemia, which is a high level of phosphorus in the blood. Hyperphosphatemia can cause bone loss and soft tissue calcification, and it is a common complication of chronic kidney disease (CKD). However, it is not an urgent issue in AKI, and it does not affect the potassium level.
Choice C reason: Calcium acetate is a medication that also binds to phosphorus in the gastrointestinal tract and removes it from the body through feces. It has the same effect and indication as sevelamer, but it also provides calcium supplementation. However, it is not an urgent issue in AKI, and it does not affect the potassium level.
Choice D reason: Epoetin alfa, recombinant is a medication that stimulates the production of red blood cells in the bone marrow. It is used to treat anemia, which is a low level of hemoglobin or red blood cells in the blood. Anemia can cause fatigue, weakness, and shortness of breath, and it is a common complication of CKD and AKI. However, it is not an urgent issue in AKI, and it does not affect the potassium level.
The nurse is preparing an older client for a magnetic resonance imaging (MRI) with contrast. Which laboratory value should the nurse report to the healthcare provider before the scan is performed?
Reference Range:
Glycosylated hemoglobin (A1C) [4% to 5.9%]
Creatinine [0.5 to 1.1 mg/dL (44 to 97 umol/L)]
Glucose [74 to 106 mg/dL (4.1 to 5.9 mmol/L)]
Blood Urea Nitrogen (BUN) [10 to 20 mg/dL (3.6 to 7.1 mmol/L)]
Explanation
Choice A reason: Fasting blood sugar of 200 mg/dL (11.1 mmol/L) indicates hyperglycemia, which is a high level of glucose in the blood. It can be caused by diabetes mellitus, stress, infection, or medication. Hyperglycemia can cause symptoms such as thirst, hunger, frequent urination, fatigue, and blurred vision. However, it does not affect the safety or accuracy of MRI with contrast.
Choice B reason: Glycosylated hemoglobin A1c of 8% indicates poor glycemic control over the past three months. It can be caused by diabetes mellitus, chronic kidney disease, or hemoglobinopathy. Glycosylated hemoglobin A1c reflects the average blood glucose level over the lifespan of red blood cells, which is about 120 days. However, it does not affect the safety or accuracy of MRI with contrast.
Choice C reason: Blood urea nitrogen of 22 mg/dL (7.9 mmol/L) indicates mild azotemia, which is a high level of nitrogenous waste products in the blood. It can be caused by dehydration, high protein intake, gastrointestinal bleeding, or kidney impairment. Azotemia can cause symptoms such as nausea, vomiting, confusion, and lethargy. However, it does not affect the safety or accuracy of MRI with contrast.
Choice D reason: Serum creatinine of 1.9 mg/dL (169 umol/L) indicates moderate renal insufficiency, which is a reduced ability of the kidneys to filter and excrete waste products and fluids from the body. It can be caused by diabetes mellitus, hypertension, glomerulonephritis, or nephrotoxic drugs. Renal insufficiency can cause symptoms such as edema, anemia, electrolyte imbalance, and acidosis. It can also increase the risk of contrast-induced nephropathy, which is a sudden deterioration of kidney function after exposure to contrast media used for imaging studies such as MRI. Contrast-induced nephropathy can lead to acute kidney injury, dialysis requirement, or even death. Therefore, serum creatinine should be reported to the healthcare provider before MRI with contrast to assess the risk and benefit of the procedure and to take preventive measures such as hydration, medication adjustment, or alternative imaging modalities.
Explanation
Choice A reason: An abdominal catheter is used for peritoneal dialysis, not hemodialysis. Hemodialysis requires access to a large blood vessel, usually in the arm or leg.
Choice B reason: Routine medications may need to be adjusted or avoided before or after hemodialysis, depending on their effects on blood pressure, fluid balance, and electrolytes.
Choice C reason: Insulin dosage may need to be reduced during hemodialysis because insulin is removed by the dialyzer and blood glucose levels may drop. This is the correct statement to include in client education.
Choice D reason: Potassium-rich foods should be limited in the diet of clients with chronic kidney disease and hemodialysis, because potassium can build up in the blood and cause cardiac arrhythmias.
A patient is admitted to the hospital with symptoms consistent with a right hemisphere stroke. Which neurovascular assessment requires immediate intervention by the nurse?
Explanation
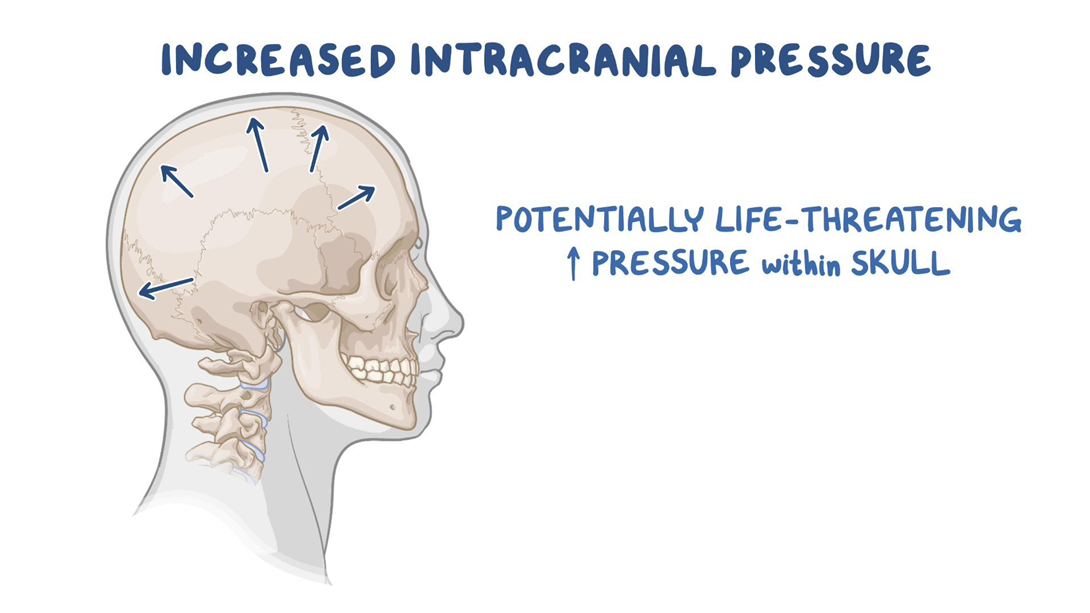
Choice A reason: Pupillary changes to ipsilateral dilation indicate increased intracranial pressure, which is a life-threatening complication of stroke. The nurse should notify the physician and prepare for emergency measures.
Choice B reason: Left-sided facial drooping and dysphagia are common signs of right hemisphere stroke, but they do not require immediate intervention by the nurse. The nurse should monitor the patient's swallowing ability and provide oral care.
Choice C reason: Orientation to person and place only is a sign of impaired cognition, which is also common in right hemisphere stroke. The nurse should assess the patient's memory, judgment, and attention span.
Choice D reason: Unequal bilateral hand grip strengths are a sign of hemiparesis, which is a weakness on one side of the body. The nurse should assist the patient with mobility and prevent contractures.
Explanation
Choice A reason: A referral for social services at home is not necessary for a client with Addison's disease who has stable vital signs, adequate hydration, and good self-care knowledge.
Choice B reason: Limiting daily fluid intake to 500 mL is not appropriate for a client with Addison's disease, who is at risk of dehydration and hypotension. The client should drink fluids according to thirst and urine output.
Choice C reason: Preparing the client for discharge home is the best action for the nurse to implement, as the client has no signs of complications or deterioration from Addison's disease. The client should be able to manage the condition at home with regular follow-up and medication adherence.
Choice D reason: Strict intake and output monitoring is not required for a client with Addison's disease who has normal blood pressure, moist mucous membranes, and strong peripheral pulses. These indicate adequate fluid balance and renal function.
A client who had a biliopancreatic diversion procedure (BPD) 3 months ago is admitted with severe dehydration. Which assessment finding warrants immediate intervention by the nurse?
Explanation
Choice A reason: Gastroccult positive emesis indicates the presence of blood in the vomit, which is a sign of a serious complication such as anastomotic leak, ulcer, or bleeding. The nurse should notify the physician and monitor the client's vital signs and hemoglobin level.
Choice B reason: Strong foul smelling flatus is a common side effect of BPD, which involves bypassing a large portion of the small intestine and creating a connection between the stomach and the colon. This results in malabsorption and bacterial overgrowth, which produce gas and odor.
Choice C reason: Complaint of poor night vision is a sign of vitamin A deficiency, which can occur after BPD due to reduced absorption of fat-soluble vitamins. The nurse should advise the client to take vitamin supplements and eat foods rich in vitamin A, such as carrots, sweet potatoes, and spinach.
Choice D reason: Loose bowel movements are another common side effect of BPD, which causes diarrhea and steatorrhea (fatty stools). The nurse should encourage the client to drink fluids with electrolytes and avoid foods that worsen diarrhea, such as greasy, spicy, or sugary foods.
Explanation
Choice A reason: Weight gain of 2 pounds (0.91 kg) in one day is a sign of fluid retention, which occurs in SIADH due to excessive secretion of antidiuretic hormone (ADH). ADH causes the kidneys to reabsorb water and reduce urine output, leading to hyponatremia and hypervolemia.
Choice B reason: Fremitus over the chest wall is a sign of increased vibration or air movement in the lungs, which can indicate pneumonia, bronchitis, or pleural effusion. These are not related to SIADH, but may be complications of head injury or fluid overload.
Choice C reason: Serum sodium of 150 mEq/L (150 mmol/L) is a sign of hypernatremia, which is a high level of sodium in the blood. This is the opposite of what happens in SIADH, where sodium levels are low due to dilution by excess water.
Choice D reason: Urine specific gravity of 1.004 is a sign of diluted urine, which indicates low concentration of solutes in the urine. This is also the opposite of what happens in SIADH, where urine is concentrated and has a high specific gravity.
Following a motor vehicle accident, a client with chest trauma receives a chest tube to relieve a hemothorax. Two hours following the chest tube insertion, the nurse observes the water level in the water-seal chamber is rising during inspiration and falling during expiration. Which action should the nurse implement?
Explanation
Choice A reason: Lifting and clearing drainage from the chest tube is not necessary, as the water level fluctuations indicate that the chest tube is functioning properly and allowing air and fluid to escape from the pleural space.
Choice B reason: Inspecting the tube insertion site for leaking is not indicated, as there is no evidence of air leak in the water-seal chamber. An air leak would cause continuous or intermittent bubbling in the water-seal chamber.
Choice C reason: Continuing to monitor the drainage system is the best action for the nurse to implement, as the water level fluctuations are normal and expected in a water-seal drainage system. The water level should rise during inspiration and fall during expiration, reflecting the changes in intrathoracic pressure.
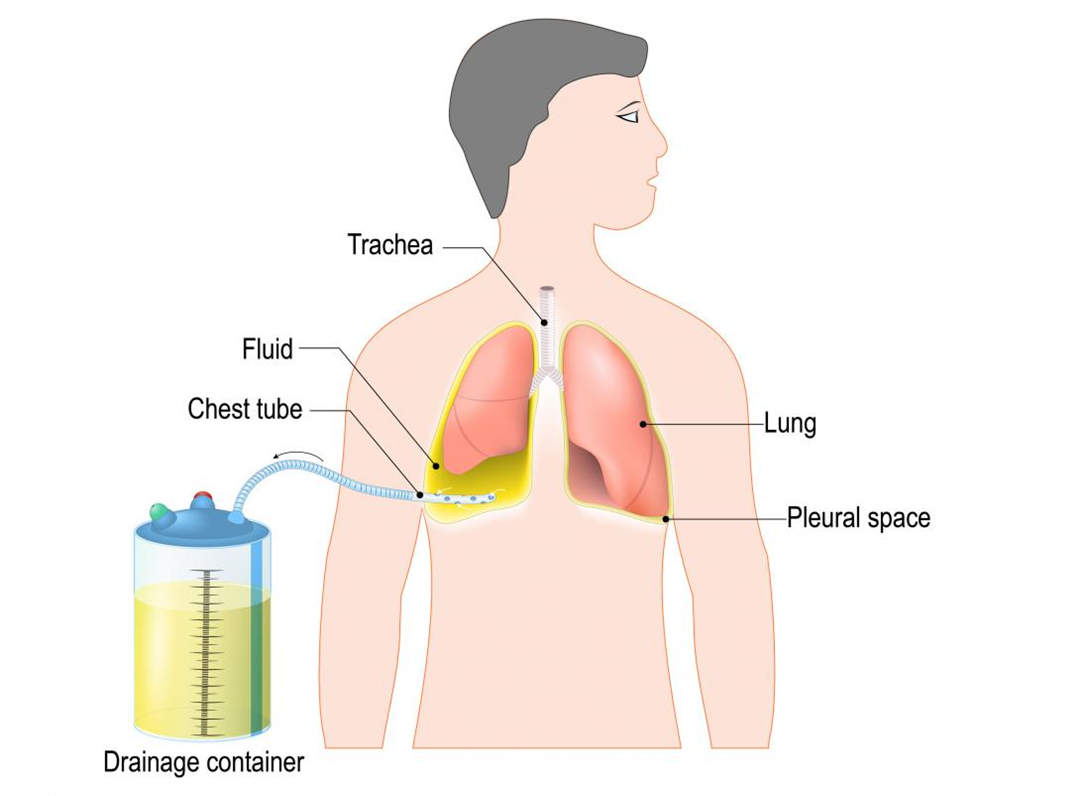
Choice D reason: Auscultating lungs for unequal breath sounds is not relevant, as it does not address the question of what to do with the water level fluctuations. Unequal breath sounds may indicate a pneumothorax or atelectasis, which are complications of chest trauma or chest tube insertion.
Explanation
Choice A reason: Redness and edema noted at the incision site are signs of inflammation, which are normal in the early stages of wound healing. The nurse should monitor the site for signs of infection, such as purulent drainage, increased pain, or fever.
Choice B reason: Apical heart rate of 100 to 110 beats/minute is a sign of tachycardia, which may be caused by pain, anxiety, dehydration, or blood loss. The nurse should assess the client's vital signs, fluid status, and hemoglobin level, and administer pain medication as prescribed.
Choice C reason: High-pitched sound heard upon inspiration is a sign of stridor, which is a life-threatening emergency that indicates airway obstruction. The nurse should call for help, administer oxygen, and prepare for intubation or tracheostomy.
Choice D reason: Pain rating of 8 on a scale of 0 to 10 is a sign of severe pain, which may impair the client's recovery and increase the risk of complications. The nurse should administer pain medication as prescribed and use non-pharmacological methods to relieve pain, such as positioning, distraction, or relaxation techniques.
A client who received 6 units of packed red blood cells 3 days ago for a lower gastrointestinal (GI) bleed is now displaying signs of shortness of breath with occasional stridor and is reporting muscle cramping.
Reference Range:
Potassium [3.5 to 5 mEq/L (3.5 to 5 mmol/L)]
Magnesium [Adult: 1.3 to 2.1 mEq/L (0.65 to 1.05 mmol/L)]
Calcium [9 to 10.5 mg/dL (2.3 to 2.6 mmol/L)]
Sodium (136 to 145 mEq/L (136 to 145 mmol/L)]
Which serum laboratory value should the nurse immediately report to the healthcare provider?
Explanation
Choice A reason: Potassium 4.7 mEq/L (4.70 mmol/L) is within the normal reference range of 3.5 to 5 mEq/L (3.5 to 5 mmol/L). Potassium is an electrolyte that helps regulate the balance of fluids and acids in the body, as well as the function of nerves and muscles. A high potassium level (hyperkalemia) can cause muscle weakness, irregular heartbeat, and cardiac arrest. A low potassium level (hypokalemia) can cause muscle cramps, fatigue, and arrhythmias.
Choice B reason: Magnesium 2.1 mEq/L (0.86 mmol/L) is within the normal reference range of 1.3 to 2.1 mEq/L (0.65 to 1.05 mmol/L). Magnesium is an electrolyte that helps regulate the activity of enzymes, muscles, and nerves, as well as the balance of calcium and potassium in the body. A high magnesium level (hypermagnesemia) can cause nausea, vomiting, flushing, muscle weakness, and respiratory depression. A low magnesium level (hypomagnesemia) can cause muscle twitching, tremors, seizures, and cardiac arrhythmias.
Choice C reason: Calcium 6.5 mg/dL (1.63 mmol/L) is below the normal reference range of 9 to 10.5 mg/dL (2.3 to 2.6 mmol/L). Calcium is an electrolyte that helps regulate the function of muscles, nerves, bones, and blood clotting. A high calcium level (hypercalcemia) can cause nausea, vomiting, constipation, confusion, kidney stones, and bone pain. A low calcium level (hypocalcemia) can cause muscle spasms, cramps, tingling, numbness, and stridor (a high-pitched sound when breathing). **This is a critical value that should be immediately reported to the healthcare provider**, as it can indicate a serious condition such as acute pancreatitis, sepsis, or massive blood transfusion.
Choice D reason: Sodium 135 mEq/L (135 mmol/L) is slightly below the normal reference range of 136 to 145 mEq/L (136 to 145 mmol/L). Sodium is an electrolyte that helps regulate the balance of fluids and acids in the body, as well as the function of nerves and muscles. A high sodium level (hypernatremia) can cause thirst, dry mouth, confusion, seizures, and coma. A low sodium level (hyponatremia) can cause headache, nausea, vomiting, fatigue, muscle weakness, and confusion.
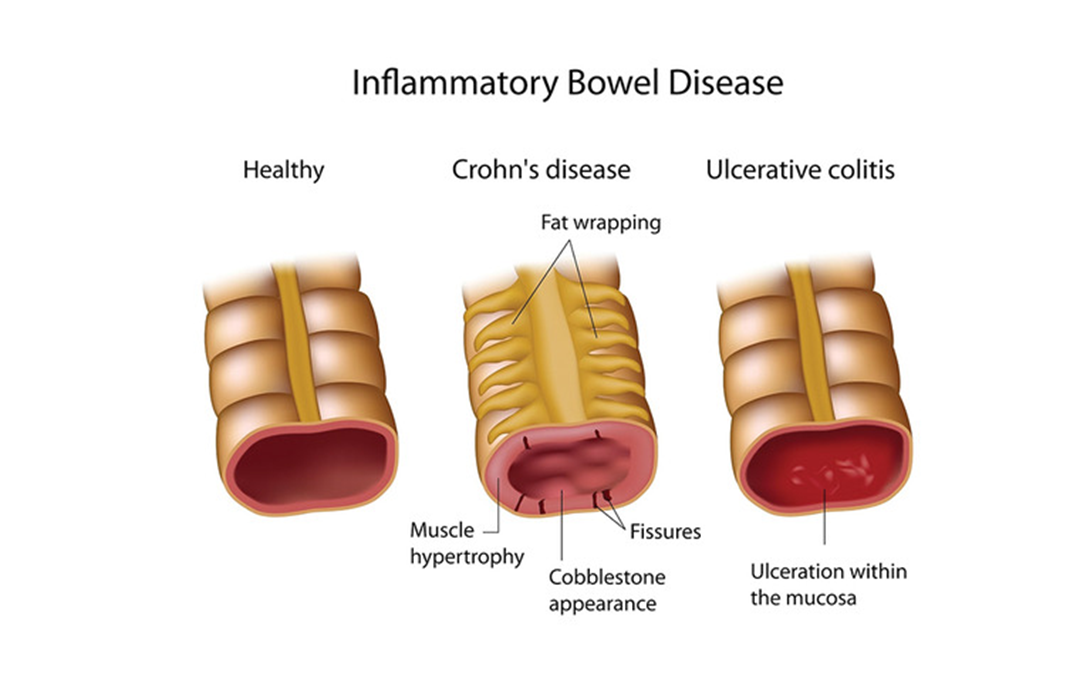
A client is hospitalized with an inflammatory bowel disease (IBD) exacerbation and is being treated with a corticosteroid. The client develops a rigid abdomen with rebound tenderness. Which action should the nurse take?
Explanation
Choice A reason: Measuring capillary glucose level is not a priority action for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Corticosteroids can increase blood glucose levels, but this is not an urgent concern in this situation.
Choice B reason: Encouraging ambulation in the room is not appropriate for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Ambulation can worsen the pain and inflammation, and increase the risk of bowel perforation.
Choice C reason: Monitoring for bloody diarrheal stools is important for a client with IBD, but not a priority action for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Bloody stools can be a sign of ulceration or bleeding in the bowel, but they are not specific to peritonitis.
Choice D reason: Obtaining vital sign measurements is the priority action for a client with a rigid abdomen and rebound tenderness. These signs indicate peritonitis, which is a serious complication of IBD that requires immediate attention. Vital signs can reveal signs of infection, inflammation, shock, and organ failure, which can guide the appropriate interventions and treatments.
Explanation
Choice A reason: Presenting a calm, supportive demeanor is an appropriate intervention for a client who is experiencing anxiety and hallucinations. The nurse should use a soothing tone of voice, maintain eye contact, and avoid arguing or challenging the client's perceptions. This can help reduce the client's agitation and promote trust.
Choice B reason: Reorienting to day and time frequently is an appropriate intervention for a client who is experiencing anxiety and hallucinations. The nurse should provide reality-based information and reminders about the client's situation, such as the reason for hospitalization, the name of the nurse, and the expected plan of care. This can help the client regain a sense of orientation and control.
Choice C reason: Administering an as needed (PRN) dose of lorazepam is an appropriate intervention for a client who is experiencing anxiety and hallucinations. Lorazepam is a benzodiazepine that can reduce anxiety, agitation, and psychotic symptoms by enhancing the effects of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter in the brain. The nurse should monitor the client's vital signs, level of sedation, and risk of falls after giving the medication.
Choice D reason: Turning the television on for distraction is not an appropriate intervention for a client who is experiencing anxiety and hallucinations. The television can increase the sensory stimulation and confusion for the client, and may worsen the hallucinations or delusions. The nurse should provide a quiet and safe environment for the client.
Choice E reason: Applying soft wrist restraints bilaterally is not an appropriate intervention for a client who is experiencing anxiety and hallucinations. Restraints can increase the anxiety and agitation for the client, and may cause physical or psychological harm. The nurse should use restraints only as a last resort when other less restrictive measures have failed to protect the client or others from harm.
An older adult client with symptoms of osteoarthritis asks the nurse which form of exercise would be most beneficial. Which is the best response by the nurse?
Explanation
Choice A reason: Jogging or running are not excellent aerobic exercises for an older adult client with osteoarthritis. These activities can put a lot of stress and impact on the joints, especially the knees, hips, and ankles, which can worsen the pain and inflammation of osteoarthritis. The nurse should advise the client to avoid high-impact exercises that can damage the cartilage and bones.
Choice B reason: Tennis or racquetball are not ideal exercises for an older adult client with osteoarthritis. These activities involve sudden movements, twists, and turns that can strain the joints, especially the elbows, wrists, and shoulders, which can aggravate the symptoms of osteoarthritis. The nurse should advise the client to avoid exercises that can cause joint instability and injury.
Choice C reason: Limiting the exercise to just the daily activities is not a good advice for an older adult client with osteoarthritis. Exercise is important for maintaining joint health, mobility, and function, as well as preventing muscle loss, obesity, and cardiovascular diseases. The nurse should encourage the client to engage in regular moderate exercise that can improve the quality of life and reduce the complications of osteoarthritis.
Choice D reason: Swimming is an excellent exercise for an older adult client with osteoarthritis. Swimming is a low-impact aerobic exercise that can strengthen the muscles, improve the cardiovascular fitness, and enhance the flexibility of the joints without putting too much pressure or stress on them. Swimming can also reduce the pain and stiffness of osteoarthritis by providing a soothing and relaxing effect on the body. The nurse should recommend swimming as a safe and effective exercise for the client.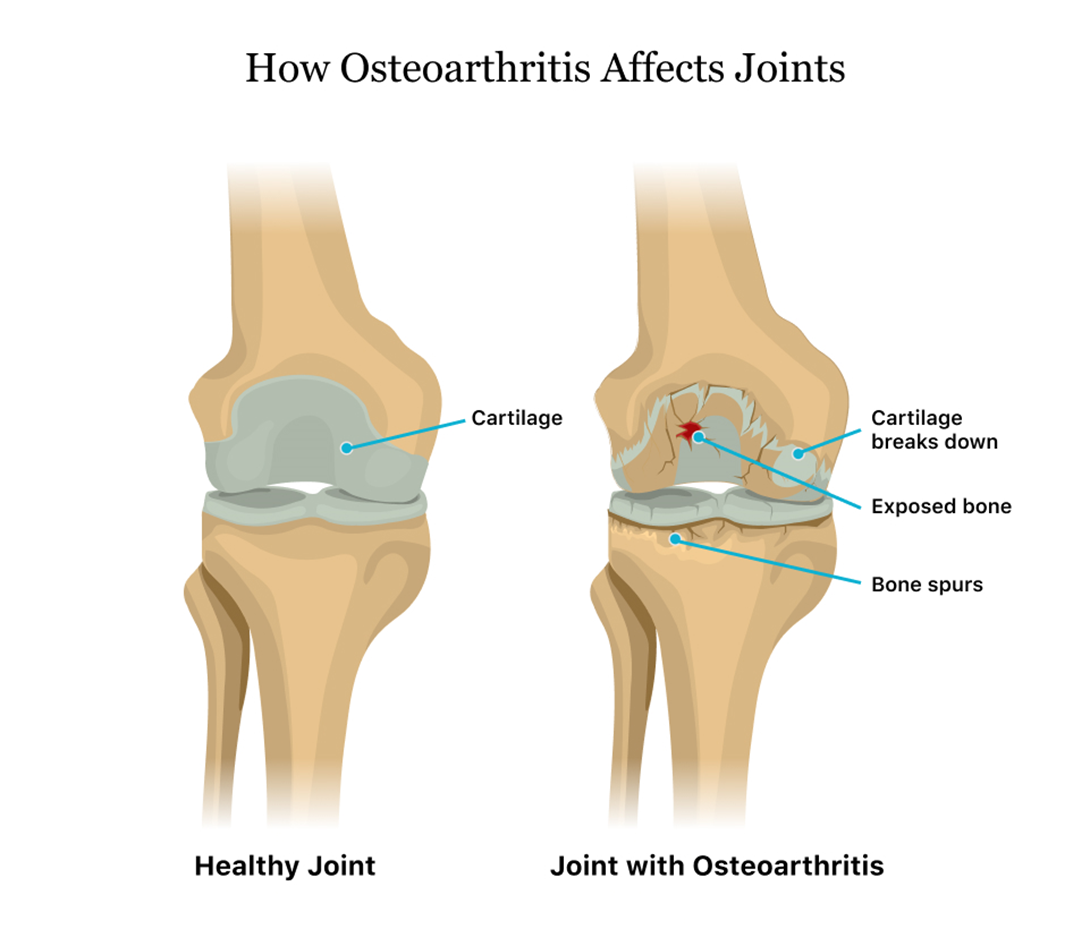
Explanation
Choice A reason: Returning for periodic liver function studies is an important instruction for a client with gouty arthritis who is taking colchicine and indomethacin. These medications can cause liver toxicity, which can manifest as jaundice, abdominal pain, nausea, vomiting, and dark urine. The nurse should advise the client to monitor for these signs and symptoms, and to have regular blood tests to check the liver enzymes and function.
Choice B reason: Massaging joints to relax muscles and decrease pain is not a recommended instruction for a client with gouty arthritis who has acute inflammation of the right ankle and great toe. Massage can increase the blood flow and pressure to the affected joints, which can worsen the pain and swelling. The nurse should advise the client to avoid touching or moving the inflamed joints, and to apply ice packs or cold compresses to reduce the inflammation.
Choice C reason: Limiting use of mobility equipment to avoid muscle atrophy is not a necessary instruction for a client with gouty arthritis who has acute inflammation of the right ankle and great toe. Mobility equipment such as crutches, walkers, or canes can help the client to ambulate safely and comfortably, and to prevent further injury or damage to the affected joints. The nurse should encourage the client to use mobility equipment as needed, and to perform gentle range of motion exercises when the inflammation subsides.
Choice D reason: Substituting natural fruit juices for carbonated drinks is not a helpful instruction for a client with gouty arthritis who is taking colchicine and indomethacin. Fruit juices can contain high amounts of fructose, which can increase the uric acid levels in the blood and trigger gout attacks. Carbonated drinks are not a major risk factor for gout, unless they contain high-fructose corn syrup or alcohol. The nurse should advise the client to drink plenty of water, and to avoid foods and beverages that are high in purines, such as organ meats, seafood, beer, and wine.
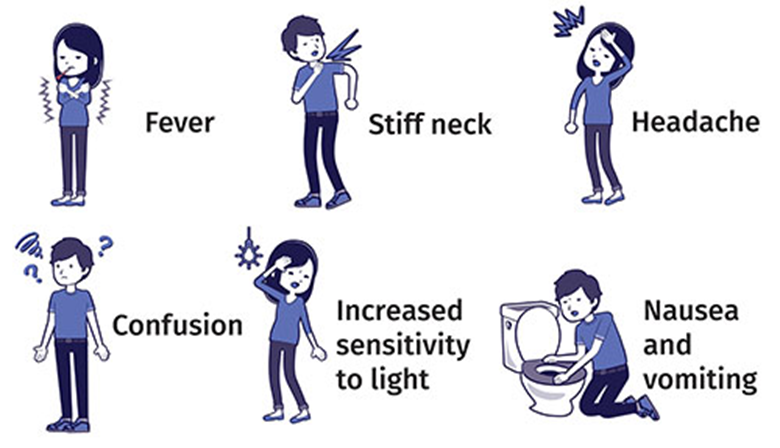
A client presents with the onset of a severe headache, fever, nuchal rigidity, and a petechial rash on arms and legs. The nurse recognizes the client is exhibiting symptoms of which condition?
Explanation
Choice A reason: Rocky Mountain spotted fever is not the most likely condition for the client who has a severe headache, fever, nuchal rigidity, and a petechial rash on arms and legs. Rocky Mountain spotted fever is a bacterial infection transmitted by ticks that causes a distinctive rash that usually begins on the wrists and ankles and spreads to the rest of the body. The rash is not limited to the arms and legs, and the client may also have other symptoms such as nausea, vomiting, abdominal pain, and muscle aches.
Choice B reason: Intracerebral hemorrhage is not the most likely condition for the client who has a severe headache, fever, nuchal rigidity, and a petechial rash on arms and legs. Intracerebral hemorrhage is a type of stroke that occurs when a blood vessel bursts inside the brain, causing bleeding and swelling. The rash is not a typical sign of intracerebral hemorrhage, and the client may also have other symptoms such as weakness, numbness, vision loss, confusion, and loss of consciousness.
Choice C reason: Cerebrovascular accident (CVA) is not the most likely condition for the client who has a severe headache, fever, nuchal rigidity, and a petechial rash on arms and legs. CVA is another term for stroke, which occurs when the blood supply to a part of the brain is interrupted, causing brain tissue damage. The rash is not a common sign of CVA, and the client may also have other symptoms such as facial drooping, slurred speech, difficulty swallowing, paralysis, and cognitive impairment.
Choice D reason: Meningococcal meningitis is the most likely condition for the client who has a severe headache, fever, nuchal rigidity, and a petechial rash on arms and legs. Meningococcal meningitis is a bacterial infection that causes inflammation of the membranes that cover the brain and spinal cord. The rash is a characteristic sign of meningococcal meningitis, which can appear as small red or purple spots that do not fade when pressed. The client may also have other symptoms such as nausea, vomiting, sensitivity to light, confusion, and seizures.
Explanation
Choice A reason: Obtaining a soft diet for the client is not the best initial nursing action for a client with chemotherapy-induced mucositis who is describing soreness of the tongue and oral issues. A soft diet can help reduce the irritation and discomfort of the oral mucosa, but it does not address the underlying cause of the inflammation and infection. The nurse should first assess the client's oral hygiene and provide appropriate interventions to prevent further complications.
Choice B reason: Encouraging frequent mouth care is the best initial nursing action for a client with chemotherapy-induced mucositis who is describing soreness of the tongue and oral issues. Frequent mouth care can help prevent or reduce the severity of mucositis by removing plaque, bacteria, and debris from the oral cavity, and by moisturizing and soothing the oral tissues. The nurse should instruct the client to use a soft toothbrush, a mild toothpaste, and a saline or bicarbonate rinse at least four times a day, and to avoid alcohol, tobacco, spicy, acidic, or hot foods and beverages.
Choice C reason: Cleansing the tongue and mouth with swabs is not the best initial nursing action for a client with chemotherapy-induced mucositis who is describing soreness of the tongue and oral issues. Swabs can be abrasive and damaging to the oral mucosa, especially if they are dry or contain alcohol or hydrogen peroxide. Swabs can also increase the risk of bleeding, infection, and ulceration of the oral tissues. The nurse should use a soft toothbrush or a gentle sponge to clean the tongue and mouth.
Choice D reason: Administering a topical analgesic per protocol is not the best initial nursing action for a client with chemotherapy-induced mucositis who is describing soreness of the tongue and oral issues. A topical analgesic can provide temporary relief of pain and discomfort, but it does not address the underlying cause of the inflammation and infection. The nurse should first assess the client's oral hygiene and provide appropriate interventions to prevent further complications. The nurse should also monitor the client's response to the analgesic and report any adverse effects or inadequate pain control.
A patient experiences residual effects following an acute attack of Ménière's disease and receives a new prescription for an antihistamine. Which assessment finding indicates that the medication is effective?
Explanation
Choice A: A headache rated at 0 on 0 to 10 scale is not a specific indicator of the effectiveness of an antihistamine. A headache may be caused by other factors, such as dehydration, stress, or sinus congestion.
Choice B: Oxygen saturation level of 99% is a normal finding and does not reflect the effect of an antihistamine. Oxygen saturation measures the amount of oxygen in the blood and can be affected by respiratory conditions, altitude, or smoking.
Choice C: Ambulating easily without vertigo is a sign that the antihistamine is effective. Vertigo is a common symptom of Ménière's disease, which is a disorder of the inner ear that causes episodes of spinning sensation, hearing loss, and tinnitus. Antihistamines can help reduce the fluid buildup in the inner ear and relieve vertigo.
Choice D: Blood pressure of 120/80 mm Hg is a normal finding and does not indicate the effect of an antihistamine. Blood pressure measures the force of blood against the walls of the arteries and can be influenced by factors such as heart rate, cardiac output, blood volume, and vascular resistance.

A client with acquired immune deficiency syndrome (AIDS) and Pneumocystis jiroveci pneumonia has a CD4+ T cell count of 200 cells/mm³ (20%). The client asks the nurse why they have these recurring massive infections. Which pathophysiologic mechanism should the nurse describe in response to this client's question?
Reference Range:
T-helper CD4 cells [600 to 1500 cells/mm³ (60 to 75%)]
Explanation
Choice A reason: This is incorrect because the humoral immune response involves B cells that produce antibodies against specific antigens. However, AIDS affects the cellular immune response, which involves T cells that activate other immune cells and directly kill infected cells.
Choice B reason: This is correct because AIDS is caused by human immunodeficiency virus (HIV), which infects and destroys CD4+ T cells, also known as helper T cells. These cells are essential for initiating and regulating both humoral and cellular immunity. Without enough CD4+ T cells, the body cannot mount an effective response against pathogens, especially opportunistic infections that take advantage of a weakened immune system.
Choice C reason: This is incorrect because bone marrow suppression of white blood cells is not a direct consequence of AIDS. However, some drugs used to treat AIDS, such as zidovudine, may cause bone marrow suppression as a side effect.
Choice D reason: This is incorrect because exposure to multiple environmental infectious agents does not cause AIDS. However, people with AIDS are more susceptible to infections from various sources due to their impaired immune system.
Explanation
Choice A reason: This is incorrect because teaching the client to wear a mask, hand wash, and social distance is not the most important action for the nurse to take. These are preventive measures that should be followed by everyone, regardless of their COVID-19 status.
Choice B reason: This is correct because isolating the client from other clients, family, and healthcare workers not wearing proper PPE is the most important action for the nurse to take. This is to prevent transmission of COVID-19 to others who may be at risk of severe complications or death.
Choice C reason: This is incorrect because reporting the COVID-19 result to the local health department according to CDC guidelines is not the most important action for the nurse to take. This is a legal and ethical obligation that should be done after confirming the diagnosis, but it does not have an immediate impact on the client's health or safety.
Choice D reason: This is incorrect because explaining to the client to inform others that they may have been potentially exposed in the last 14 days is not the most important action for the nurse to take. This is a moral and social responsibility that should be done as soon as possible, but it does not address the urgent need of isolating the client from potential sources of infection.
While completing a health assessment for a young adult female with acute appendicitis, the client informs the nurse that there is a chance that she may be pregnant. The operating team is preparing to take the client to surgery. Which intervention should the nurse implement immediately?
Explanation
Choice A reason: This is correct because performing a bedside pregnancy test is the intervention that should be implemented immediately by the nurse. This is to confirm or rule out pregnancy and inform the surgical team of any possible risks or complications that may affect the client or the fetus.
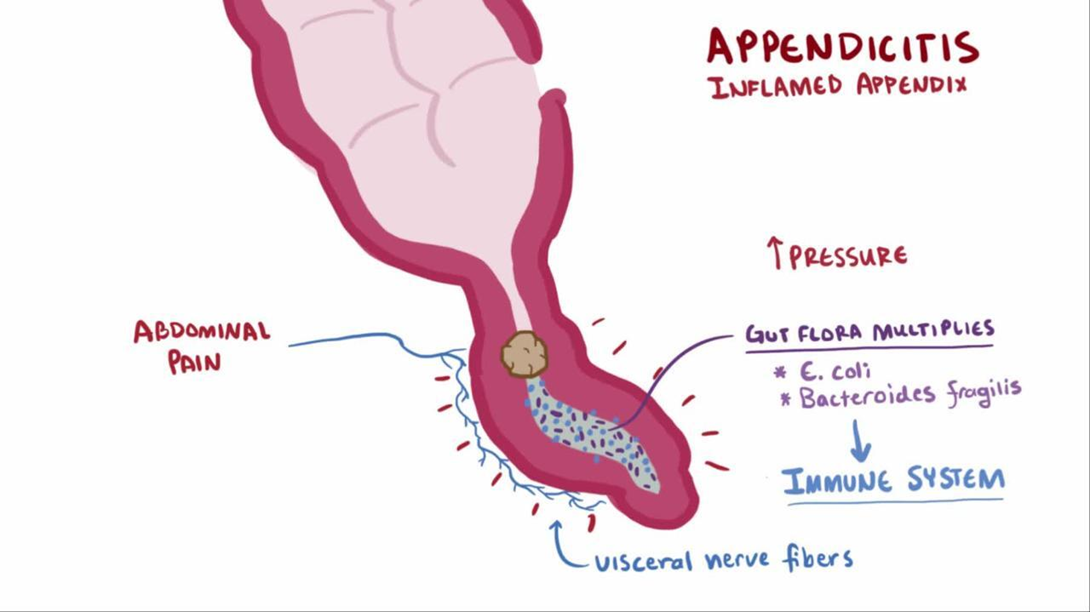
Choice B reason: This is incorrect because continuing with surgery as scheduled is not an appropriate intervention without verifying the pregnancy status of the client. Surgery may pose serious threats to both maternal and fetal health, such as bleeding, infection, anesthesia complications, or miscarriage.
Choice C reason: This is incorrect because calculating gestation from last menstrual cycle is not an accurate or reliable method of determining pregnancy. The menstrual cycle can vary widely among women and may be affected by various factors such as stress, illness, or medication.
Choice D reason: This is incorrect because notifying the surgical team to cancel the surgery is not a necessary intervention unless pregnancy is confirmed. Appendicitis is a medical emergency that requires prompt surgical treatment to prevent rupture, peritonitis, or sepsis.
A client has an absolute neutrophil count (ANC) of 500/mm³ (0.5 x 10⁹/L) after completing chemotherapy. Which intervention is most important for the nurse to implement?
Reference Range:
Neutrophils (ANC) [2500 to 5800/mm³ (2.5 to 5.8 x 10⁹/L)]
Explanation
Choice A reason: This is incorrect because reviewing the need for pneumococcal vaccine is not the most important intervention for the nurse to implement. Pneumococcal vaccine is recommended for people who are at high risk of pneumococcal infections, such as those with chronic diseases or immunosuppression. However, it is not a priority action for a client with neutropenia, which is a low number of neutrophils that increases the risk of bacterial and fungal infections.
Choice B reason: This is incorrect because implementing bleeding precautions is not the most important intervention for the nurse to implement. Bleeding precautions are indicated for clients who have thrombocytopenia, which is a low number of platelets that impairs blood clotting. However, this is not the case for a client with neutropenia, which affects the white blood cells that fight infections.
Choice C reason: This is incorrect because assessing vital signs every 4 hours is not the most important intervention for the nurse to implement. Vital signs are important indicators of the client's health status and may reveal signs of infection, such as fever, tachycardia, or hypotension. However, this is not a sufficient measure to prevent or treat infections in a client with neutropenia, who needs more aggressive and proactive interventions.
Choice D reason: This is correct because placing the client in protective isolation is the most important intervention for the nurse to implement. Protective isolation, also known as reverse isolation or neutropenic precautions, is a set of measures that aim to protect the client from exposure to pathogens that may cause infections. These include wearing gloves, masks, gowns, and eye protection; using sterile equipment and techniques; avoiding contact with people who are sick or have infections; and restricting visitors and fresh flowers or fruits.
The nurse is caring for a client who had a cholecystectomy two days ago. The client is febrile, reporting upper abdominal pain radiating to the back and has had three episodes of vomiting in the last 8 hours. The nurse reviews the client's serum amylase and lipase level results which are twice the normal value. Based on these findings, the nurse should recognize the client is exhibiting symptoms of which condition?
Explanation
Choice A reason: This is incorrect because hepatorenal failure is a condition that involves both liver and kidney dysfunction, usually as a complication of cirrhosis or portal hypertension. The symptoms of hepatorenal failure may include jaundice, ascites, edema, oliguria, or encephalopathy. However, these are not consistent with the client's presentation of fever, abdominal pain, vomiting, and elevated amylase and lipase levels.
Choice B reason: This is correct because acute pancreatitis is an inflammation of the pancreas that can be caused by gallstones, alcohol abuse, trauma, infection, or drugs. The symptoms of acute pancreatitis may include fever, upper abdominal pain that radiates to the back, nausea, vomiting, and elevated amylase and lipase levels. These are consistent with the client's presentation and suggest that the cholecystectomy may have triggered an attack of acute pancreatitis.
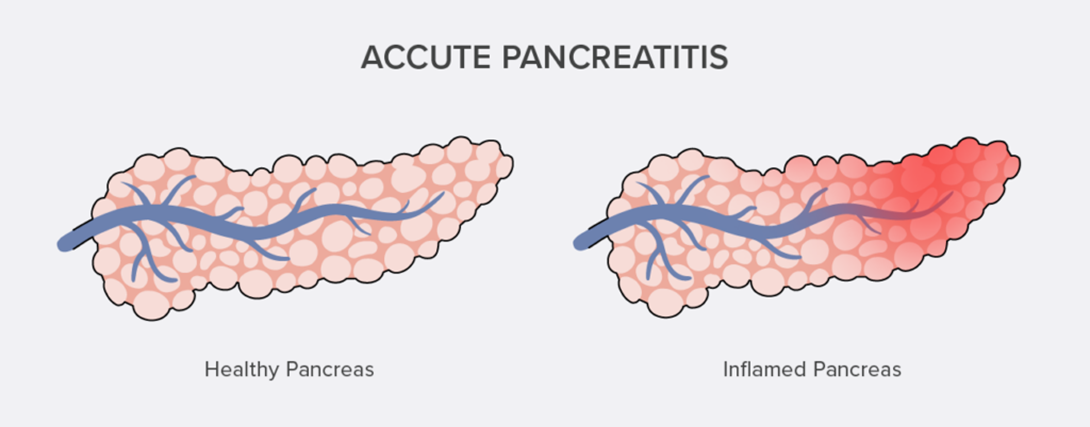
Choice C reason: This is incorrect because surgical site infection is an infection that occurs at or near the incision site after surgery. The symptoms of surgical site infection may include redness, swelling, warmth, pus drainage, or pain at the wound site. However, these are not consistent with the client's presentation of fever, abdominal pain radiating to the back, vomiting, and elevated amylase and lipase levels.
Choice D reason: This is incorrect because biliary duct obstruction is a blockage of the bile ducts that carry bile from the liver and gallbladder to the intestine. The causes of biliary duct obstruction may include gallstones, tumors, inflammation, or scarring. The symptoms of biliary duct obstruction may include jaundice, dark urine, pale stools, itching, or abdominal pain. However, these are not consistent with the client's presentation of fever, abdominal pain radiating to the back, vomiting, and elevated amylase and lipase levels.
Explanation
Choice A reason: This is incorrect because consuming a high protein diet is not a recommended strategy to reduce risk factors for BPH. In fact, some studies have suggested that a high protein intake may increase the risk of BPH by stimulating the production of insulin-like growth factor-1 (IGF-1), which may promote prostate growth.
Choice B reason: This is incorrect because obtaining a prostate-specific antigen blood level test is not a preventive measure for BPH, but rather a diagnostic tool to detect prostate cancer or monitor its treatment. Prostate-specific antigen (PSA) is a protein produced by the prostate gland that can be elevated in both BPH and prostate cancer. However, PSA levels alone cannot distinguish between these two conditions and need to be interpreted along with other factors, such as age, race, family history, and digital rectal examination.
Choice C reason: This is incorrect because taking vitamin supplements is not a proven method to reduce risk factors for BPH. While some vitamins, such as vitamin D and vitamin E, may have some beneficial effects on prostate health, there is not enough evidence to support their use as preventive agents for BPH. Moreover, some vitamins, such as vitamin A and vitamin B6, may have adverse effects on prostate health and increase the risk of BPH or prostate cancer.
Choice D reason: This is correct because increasing physical activity is a helpful way to reduce risk factors for BPH. Physical activity can help maintain a healthy weight, lower blood pressure, improve blood circulation, reduce inflammation, and regulate hormone levels. All of these factors can contribute to preventing or delaying the development of BPH.
Explanation
Choice A reason: This is incorrect because performing a complete mental status exam is not a relevant or appropriate action for the nurse to implement. A mental status exam is used to evaluate the client's cognitive, emotional, and behavioral functioning, but it does not address the client's physical pain or its underlying cause.
Choice B reason: This is incorrect because determining if the client has had a shingles vaccination is not a priority or helpful action for the nurse to implement. A shingles vaccination is recommended for people who are 50 years or older to prevent or reduce the severity of shingles, but it does not affect the occurrence or treatment of postherpetic neuralgia, which is a chronic pain condition that can develop after shingles.
Choice C reason: This is incorrect because teaching the client about phantom pain symptoms is not an accurate or useful action for the nurse to implement. Phantom pain is a type of neuropathic pain that occurs when a person feels pain in a body part that has been amputated or removed. However, this is not the case for the client who has pain in the area where the shingles rash occurred.
Choice D reason: This is correct because completing an assessment of the client's pain is the most important action for the nurse to implement. Pain assessment involves collecting information about the location, intensity, quality, duration, frequency, and aggravating or relieving factors of the pain, as well as its impact on the client's daily activities and quality of life. This can help the nurse identify the cause and severity of the pain, as well as plan and evaluate appropriate interventions.
Explanation
Choice A reason: This is correct because abdominal obesity, also known as central obesity or visceral fat, is one of the criteria for diagnosing metabolic syndrome and a major risk factor for diabetes mellitus and vascular disease. Abdominal obesity is defined as having a waist circumference of more than 40 inches (102 cm) for men or 35 inches (88 cm) for women. Abdominal obesity can increase insulin resistance, inflammation, and blood pressure, which can lead to impaired glucose metabolism and cardiovascular complications.
Choice B reason: This is correct because blood pressure of 150/96 mm Hg is another criterion for diagnosing metabolic syndrome and a significant risk factor for diabetes mellitus and vascular disease. Blood pressure is defined as the force exerted by blood against the walls of blood vessels. Normal blood pressure is less than 120/80 mm Hg, while high blood pressure (hypertension) is 140/90 mm Hg or higher. High blood pressure can damage the blood vessels and organs, such as the heart, kidneys, eyes, and brain, and increase the risk of heart attack, stroke, kidney failure, and vision loss.
Choice C reason: This is incorrect because elevated high density lipoproteins (HDL), also known as good cholesterol, are not a criterion for diagnosing metabolic syndrome or a risk factor for diabetes mellitus and vascular disease. In fact, HDL are beneficial for cardiovascular health because they help remove excess cholesterol from the blood and prevent plaque buildup in the arteries. Normal HDL levels are 40 mg/dL (1.0 mmol/L) or higher for men and 50 mg/dL (1.3 mmol/L) or higher for women.
Choice D reason: This is correct because increased triglyceride levels are another criterion for diagnosing metabolic syndrome and a risk factor for diabetes mellitus and vascular disease. Triglycerides are a type of fat that circulates in the blood and provides energy to cells. Normal triglyceride levels are less than 150 mg/dL (1.7 mmol/L), while high triglyceride levels are 200 mg/dL (2.3 mmol/L) or higher. High triglyceride levels can increase insulin resistance, inflammation, and blood clotting, which can impair glucose metabolism and increase the risk of heart attack and stroke.
Choice E reason: This is correct because hyperglycemia, also known as high blood sugar, is another criterion for diagnosing metabolic syndrome and a hallmark of diabetes mellitus. Hyperglycemia occurs when the body cannot produce enough insulin or use it properly to regulate the amount of glucose in the blood. Normal blood glucose levels are 70 to 99 mg/dL (3.9 to 5.5 mmol/L) before meals and less than 140 mg/dL (7.8 mmol/L) two hours after meals, while hyperglycemia is 126 mg/dL (7.0 mmol/L) or higher before meals or 200 mg/dL (11.1 mmol/L) or higher two hours after meals. Hyperglycemia can damage the blood vessels and organs, such as the eyes, kidneys, nerves, and feet, and increase the risk of infections, ulcers, amputations, and diabetic ketoacidosis.
Choice F reason: This is incorrect because hypothyroidism, also known as underactive thyroid, is not a criterion for diagnosing metabolic syndrome or a direct risk factor for diabetes mellitus and vascular disease. Hypothyroidism occurs when the thyroid gland does not produce enough thyroid hormones, which regulate the body's metabolism, growth, and development. Hypothyroidism can cause symptoms such as fatigue, weight gain, cold intolerance, dry skin, hair loss, constipation, and depression. However, hypothyroidism does not affect the blood glucose or lipid levels directly, but rather indirectly through its effects on weight and appetite.
Sign Up or Login to view all the 44 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

