RN Pharmacology 2019 Exam 5
Total Questions : 53
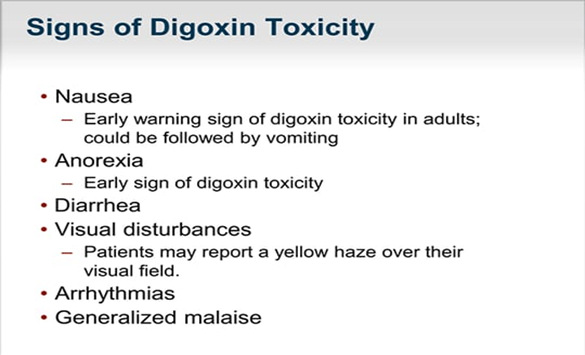
Showing 25 questions, Sign in for moreA nurse is assessing a client who has heart failure and is taking digoxin. Which of the following findings should the nurse identify as an early indication of medication toxicity?
Explanation
Choice A Reason:
Visual disturbances is the correct findings. In individuals taking digoxin, visual disturbances such as blurred or yellow-tinted vision can indicate early signs of medication toxicity. This symptom often requires prompt medical attention, as it can precede more severe complications.
Choice B Reason:
Sudden weight gain is not correct. While weight gain can be a symptom of worsening heart failure, it's not typically associated specifically with digoxin toxicity. It's more commonly related to fluid retention in heart failure.
Choice C Reason:
Potassium 4.4 mEq/L is not correct. This potassium level is within the normal range. Digoxin toxicity can be exacerbated by low potassium levels, but a normal potassium level doesn't directly indicate digoxin toxicity.
Choice D Reason:
Insomnia is not a typical early sign of digoxin toxicity. It's more commonly associated with issues like difficulty sleeping rather than being a direct symptom of digoxin toxicity.
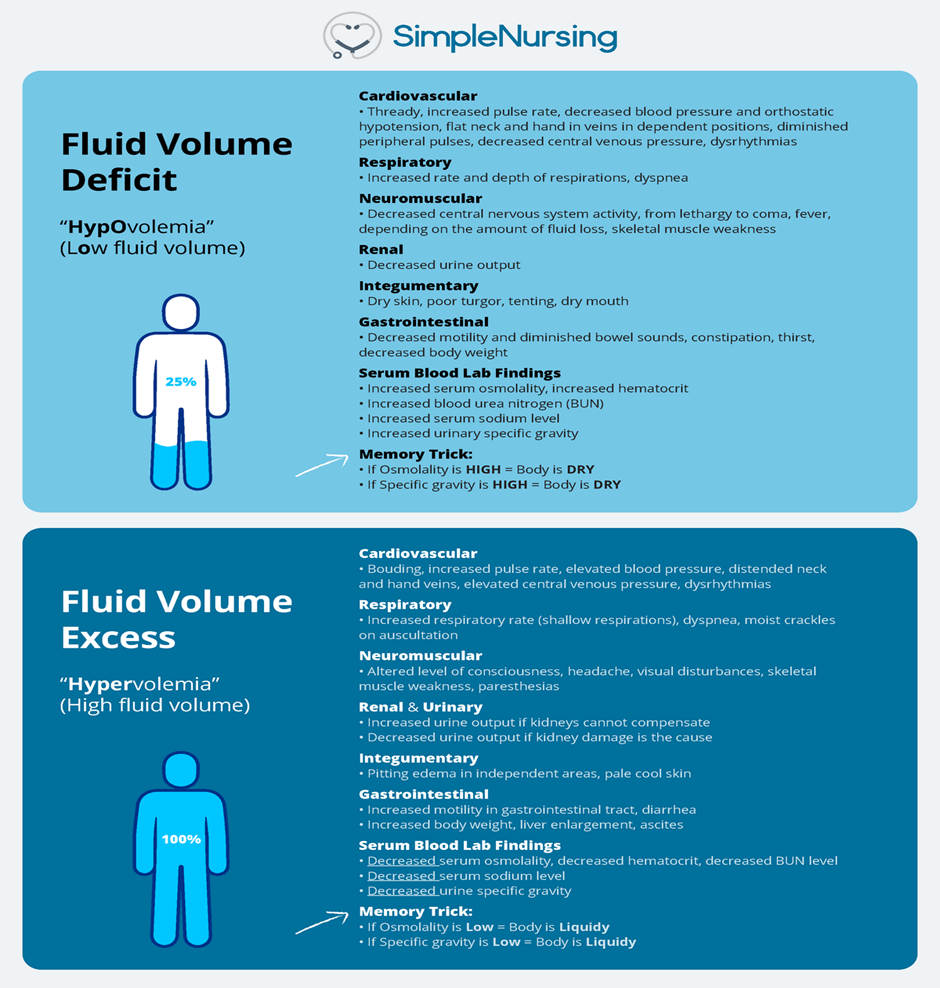
A nurse is teaching a class about administering IV fluids to treat dehydration. The nurse should include in the teaching that which of the following laboratory values indicates effective treatment of dehydration?
Explanation
Choice A Reason:
Serum osmolarity 310 mOsm/L is incorrect. Serum osmolarity measures the concentration of particles in the blood. While an elevated serum osmolarity might indicate dehydration, it's not a direct indicator of the effectiveness of treatment. It signifies the concentration of solutes in the blood rather than reflecting hydration improvement after treatment.
Choice B Reason:
Serum hematocrit 55%m is incorrect. Elevated hematocrit levels can occur in dehydration because of hemoconcentration (an increase in the concentration of red blood cells due to reduced fluid volume). However, similar to serum osmolarity, while it can indicate dehydration, it doesn't specifically reflect the effectiveness of treatment.
To determine effective treatment of dehydration, the nurse should consider the laboratory values that reflect hydration status:
Choice C Reason:
Urine specific gravity 1.020 is correct. Urine specific gravity measures the concentration of solutes in the urine, indicating the kidneys' ability to concentrate urine. A higher specific gravity (typically above 1.020) suggests more concentrated urine, which can indicate dehydration. As hydration improves, the urine becomes less concentrated, so a decrease in urine specific gravity toward the normal range (around 1.010-1.020) indicates effective rehydration and improved kidney function in retaining fluids.
Choice D Reason:
BUN 28 mg/dL is incorrect. Blood urea nitrogen (BUN) levels can also rise in dehydration due to reduced kidney perfusion. However, like serum osmolarity and hematocrit, while it can indicate dehydration, it doesn't directly show the effectiveness of treatment or the improvement in hydration status after treatment.
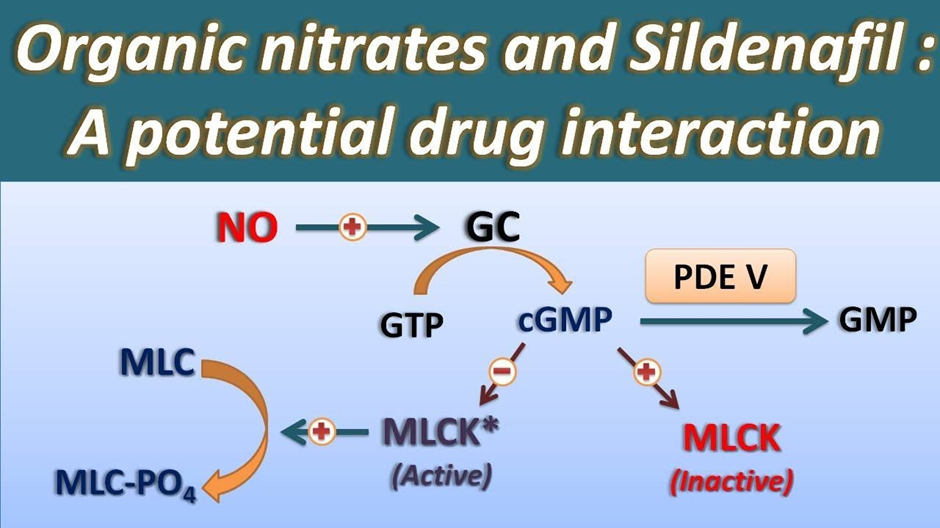
A nurse is reviewing the medication list of a client who has erectile dysfunction and is requesting a prescription for sildenafil. The nurse should identify that which of the following medications is a contraindication for receiving this medication?
Explanation
Choice A Reason:
Furosemide is not correct. Furosemide is a diuretic used to treat conditions like heart failure and edema by increasing urine output. It is not a contraindication for sildenafil. However, it's essential to monitor blood pressure when these medications are used together, as both can potentially lower blood pressure.
Choice B Reason:
Albuterol is not correct. Albuterol is a bronchodilator commonly used to treat asthma and other respiratory conditions. It doesn't have direct contraindications with sildenafil for erectile dysfunction. Although both medications can cause some cardiovascular effects, they are not typically considered contraindications for each other.
Choice C Reason:
Indomethacin is not correct. Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) used to reduce inflammation and pain. While it can have effects on blood pressure and the cardiovascular system, it is not a direct contraindication for sildenafil specifically for erectile dysfunction.
Choice D Reason:
Nitroglycerin is correct. Nitroglycerin is a contraindication for sildenafil. Both medications can cause a significant drop in blood pressure. When taken together, they can potentiate each other's effects, leading to a severe decrease in blood pressure, which can be dangerous and potentially life-threatening. Therefore, individuals using nitroglycerin or any nitrate medications should not take sildenafil or other medications for erectile dysfunction due to the risk of hypotension (dangerously low blood pressure).
A nurse realizes that they failed to administer a medication that was due 4 hr ago to a client. Which of the following actions should the nurse take first?
Explanation
Choice A Reason:
Determine factors that led to the omission. Understanding why the dosage was missed is crucial. Was there a specific reason such as an interruption, conflicting priorities, or confusion in the medication schedule? Identifying these factors can help prevent future omissions and improve the medication administration process.
Choice B Reason:
File an incident report. If the missed dosage poses any potential risk or deviation from the prescribed treatment plan, it's important to document the incident through an incident report. This ensures transparency and allows the healthcare team to address and learn from the situation.
Choice C Reason:
Report the missed dosage to the client's provider. Informing the client's healthcare provider about the missed dosage is crucial. The provider can assess the situation and provide guidance on whether any adjustments or additional steps are necessary to ensure the client's well-being.
Choice D Reason:
Assess the client for adverse reactions. Monitoring the client for any adverse reactions or changes in their condition is essential after a missed dosage. This observation helps detect any potential effects of the missed medication and allows for prompt intervention if needed.
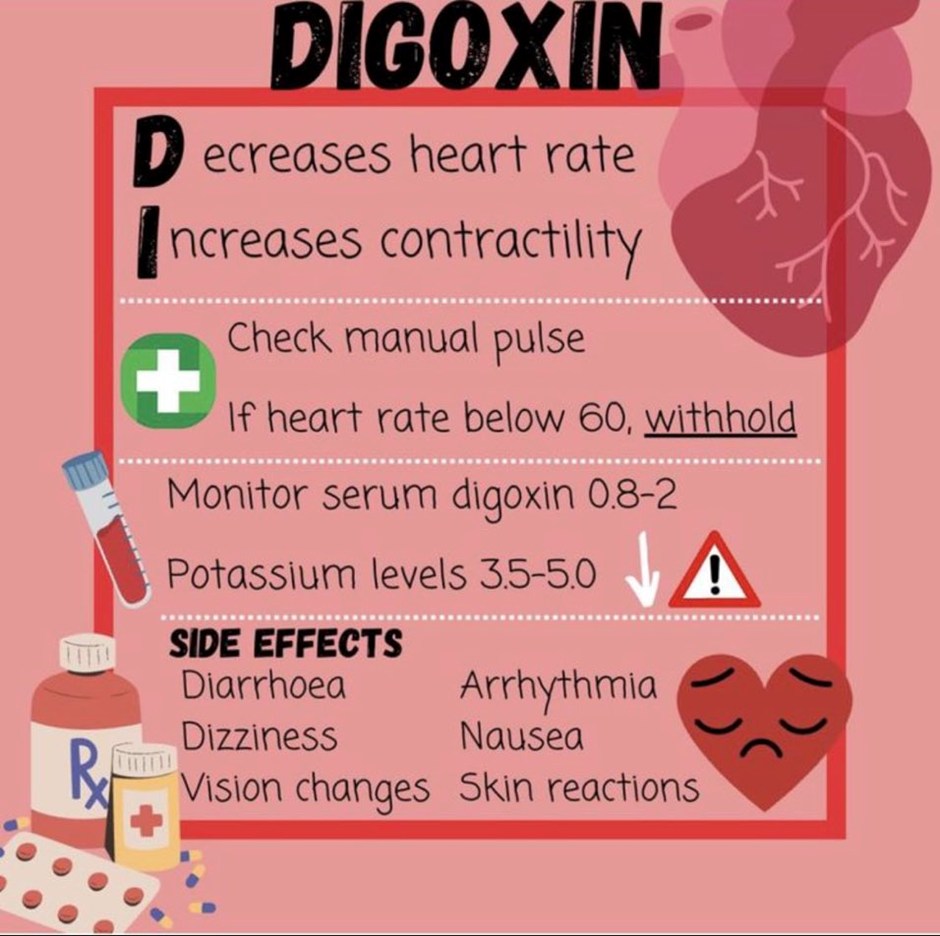
A nurse is preparing to administer digoxin to a client who has heart failure. The nurse should withhold the medication for which of the following findings?
Explanation
Choice A Reason:
Weight gain of 0.7 kg (1.5 lb) in 24 hours is not recommendable. While sudden weight gain can indicate fluid retention, it is not a direct contraindication for administering digoxin. However, it might indicate worsening heart failure, which needs attention, but it doesn't specifically necessitate withholding digoxin.
Choice B Reason:
Urinary output 30 mL/hr is not recommendable. A low urinary output might indicate decreased kidney perfusion or renal issues. While monitoring urinary output is important, it is not a direct reason to withhold digoxin unless it's coupled with severe renal impairment or an acute kidney injury.
For a client receiving digoxin, certain findings would warrant withholding the medication due to potential complications. Among the options provided:
Choice C Reason:
Pulse rate 56/min is the correct recommendation. A low pulse rate (bradycardia), especially below 60 beats per minute, is a reason to withhold digoxin. Digoxin can further decrease the heart rate, potentially leading to excessive bradycardia or heart block. The nurse should hold the medication and consult with the healthcare provider to determine the appropriate action.
Choice D Reason:
BP 160/90 mm Hg is not recommendable. Elevated blood pressure alone is not a direct contraindication for administering digoxin to a patient with heart failure. Digoxin is not primarily used for controlling blood pressure; its use is more focused on managing heart rate and contractility in heart failure patients.
A nurse is reviewing the plan of care with a client who has a new prescription for lovastatin. Which of the following statements by the client should indicate to the nurse a need for further assessment?
Explanation
Choice A Reason:
"I should avoid drinking grapefruit juice." This statement is actually accurate. Grapefruit juice can interfere with the metabolism of certain statin medications, including lovastatin, leading to increased levels of the drug in the body. Advising against grapefruit juice consumption is a recommended precaution when taking lovastatin, so this statement shows the client's understanding of this interaction.
Choice B Reason:
"I am trying to decrease my dietary fat intake." This statement reflects a positive lifestyle change. Lowering dietary fat intake is often recommended for individuals on statin medications to help manage cholesterol levels. This statement demonstrates the client's commitment to making healthy dietary adjustments, which aligns with the treatment plan.
Choice B Reason:
"I was just diagnosed with hepatitis B. "Hepatitis B can affect liver function, and statin medications like lovastatin can potentially impact liver enzymes. Therefore, in someone with a history of hepatitis B, it's crucial to assess liver function before starting a statin and to monitor the liver during treatment. This statement raises concerns about potential liver complications or interactions that require further evaluation before initiating lovastatin.
Choice D Reason:
"I take metformin for my diabetes." Metformin, a medication for diabetes, does not directly interact with lovastatin. While it's relevant to know the client's other medications, this statement doesn't indicate a need for immediate further assessment regarding the use of lovastatin.
A nurse is assessing a client who is receiving intravenous therapy. The nurse should identify which of the following findings as a manifestation of fluid volume excess?
Explanation
Choice A Reason:
Bilateral muscle weakness is not typically associated specifically with fluid volume excess. Muscle weakness can result from various causes, such as electrolyte imbalances or certain medical conditions, but it's not a primary manifestation of fluid volume excess.
Choice B Reason:
Thready pulse is not correct. A thready pulse refers to a weak and barely palpable pulse. This is more commonly associated with conditions like shock or reduced cardiac output rather than fluid volume excess.
Choice C Reason:
Decreased bowel sounds is not correct. Reduced or absent bowel sounds may indicate gastrointestinal issues, but they are not a direct manifestation of fluid volume excess. Increased bowel sounds might be more associated with certain types of gastrointestinal disturbances or fluid imbalances, but decreased sounds are not a typical sign of fluid volume excess.
Choice D Reason:
Distended neck veins is correct. In a client experiencing fluid volume excess, distended neck veins can often be observed due to increased venous pressure. This occurs as a result of the body retaining more fluid than it can handle, leading to an increase in blood volume and pressure within the vascular system. This can cause the jugular veins in the neck to appear distended or prominent.
A nurse is teaching a client who has pernicious anemia to self-administer nasal cyanocobalamin. Which of the following information should the nurse include in the teaching?
Explanation
Choice A Reason:
There's no requirement to lie down for an hour after administering nasal cyanocobalamin.
Choice B Reason:
The duration of treatment might vary depending on the healthcare provider's instructions and the client's response, so stating a specific duration of 6 months may not be accurate.
Choice C Reason:
"Administer the medication into one nostril once per week. “Nasal cyanocobalamin is typically used weekly for the treatment of pernicious anemia. It's administered into one nostril as directed by a healthcare provider. This method allows for the absorption of vitamin B12 through the nasal mucosa.
Choice D Reason:
Using a nasal decongestant before administering the medication is not typically part of the recommended administration protocol for nasal cyanocobalamin.

A nurse is caring for a client who has diabetes insipidus and is receiving desmopressin by intermittent IV bolus. Which of the following manifestations should indicate to the nurse a therapeutic response to the medication?
Explanation
Choice A Reason:
Increase in serum glucose is incorrect. Desmopressin, which is a synthetic form of vasopressin, primarily affects water reabsorption in the kidneys and doesn't directly impact glucose levels. Therefore, an increase in serum glucose wouldn't be an expected therapeutic response to desmopressin for diabetes insipidus.
Choice B Reason:
Decrease in blood pressure is incorrect. Desmopressin is primarily used for its antidiuretic effect, concentrating urine by increasing water reabsorption in the kidneys. It typically doesn't have a significant impact on blood pressure. Therefore, a decrease in blood pressure wouldn't typically be an anticipated therapeutic response to desmopressin in this context.
Choice C Reason:
Decrease in urine output is correct. Desmopressin is a synthetic form of vasopressin (antidiuretic hormone) used to treat diabetes insipidus, a condition characterized by excessive urination and extreme thirst due to the inability to concentrate urine. The primary goal of desmopressin is to reduce urine output by increasing water reabsorption in the kidneys, thereby decreasing excessive urination. Therefore, a decrease in urine output would indicate a therapeutic response to the medication in this context.
Choice D Reason:
Increase in WBC count is incorrect. Desmopressin's action is centered on affecting kidney function by regulating water reabsorption and does not involve changes in white blood cell count. Consequently, an increase in WBC count wouldn't be an expected therapeutic response to desmopressin for diabetes insipidus.
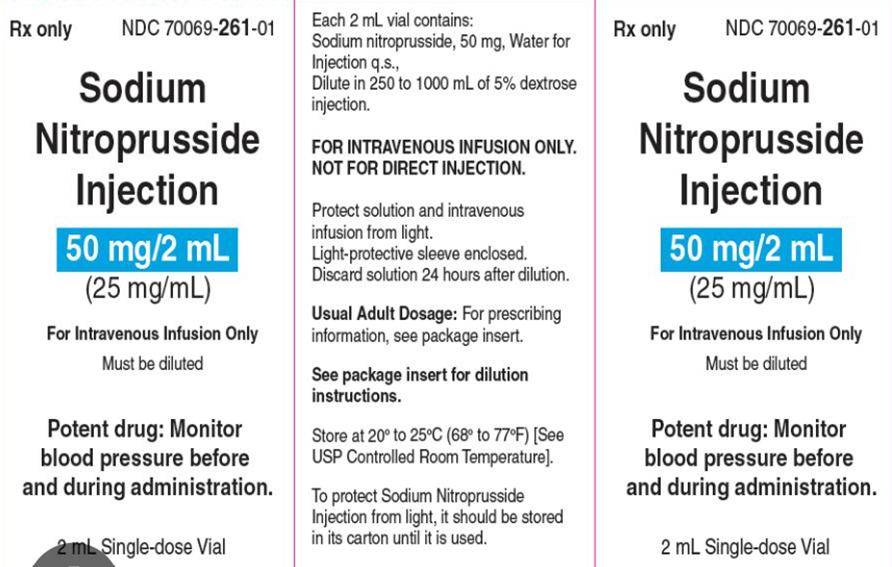
A nurse is preparing to titrate a continuous nitroprusside infusion for a client. The nurse should plan to titrate the infusion according to which of the following assessments?
Explanation
Choice A Reason:
Blood pressure is correct. Nitroprusside is a medication used to lower blood pressure in conditions such as hypertensive emergencies. It's titrated based on blood pressure readings, with the goal of achieving the desired target blood pressure range as directed by the healthcare provider. The nurse would monitor the client's blood pressure closely and adjust the infusion rate accordingly to achieve the prescribed blood pressure parameters.
Choice B Reason:
Stroke volume is incorrect. While stroke volume (the amount of blood ejected by the heart with each contraction) is important in assessing heart function, it's not directly used to titrate a nitroprusside infusion. Nitroprusside primarily acts as a vasodilator to reduce blood pressure, rather than affecting stroke volume.
Choice C Reason:
Cardiac output is incorrect. Cardiac output (the volume of blood pumped by the heart per minute) is also a crucial measure of heart function, but adjusting a nitroprusside infusion based on cardiac output is not a common practice. Nitroprusside's primary action is to dilate blood vessels, impacting blood pressure regulation more directly than cardiac output.
Choice D Reason:
Urine output is incorrect. While urine output is an important indicator of renal function and overall fluid balance, it is not typically used as the main parameter for titrating nitroprusside. Nitroprusside's primary effect is on vasodilation and blood pressure control rather than directly impacting urine output.
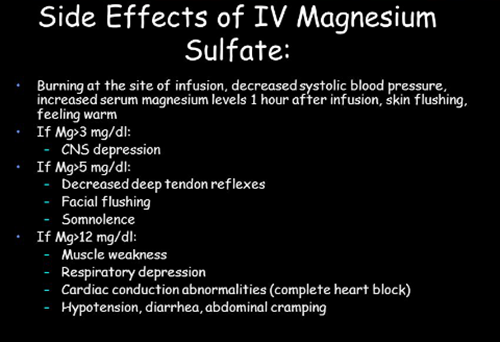
A nurse is caring for a client who is receiving a continuous IV infusion of magnesium sulfate for preterm labor. The nurse should discontinue the infusion and prepare to administer calcium gluconate if the client demonstrates which of the following findings? (Select all that apply.)
Explanation
Choice A Reason:
Absence of deep-tendon reflexes is correct. The absence or decrease in deep-tendon reflexes can be a sign of magnesium toxicity. Magnesium sulfate, when given in excessive amounts or in the case of accumulation due to impaired renal function, can lead to muscle weakness, hyporeflexia, and in severe cases, loss of deep-tendon reflexes. Discontinuation of magnesium sulfate and administration of calcium gluconate is warranted in severe cases of magnesium toxicity to counteract its effects.
Choice B Reason:
Report of chills is incorrect. Chills are non-specific symptoms and are not typically associated specifically with magnesium toxicity. They are less indicative of a need for calcium gluconate administration in the context of magnesium sulfate infusion.
Choice C Reason:
Decreased level of consciousness is correct. Severe magnesium toxicity can affect the central nervous system, leading to symptoms like confusion, drowsiness, and eventually decreased level of consciousness. In these cases, discontinuation of magnesium sulfate and administration of calcium gluconate is crucial to counteract the effects of excessive magnesium.
Choice D Reason:
Systolic blood pressure of 130 mm Hg is incorrect. A systolic blood pressure of 130 mm Hg, by itself, is not an indicator of magnesium toxicity that necessitates the administration of calcium gluconate. Blood pressure within this range is not typically a cause for concern related to magnesium sulfate administration.
Choice EReason:
Urine output of 80 mL in 4 hours is incorrect. While decreased urine output might indicate potential renal issues or compromised kidney function, it's not a specific indication for the administration of calcium gluconate in the context of magnesium sulfate infusion. It can signal the need for further assessment but is not a direct sign of magnesium toxicity requiring calcium gluconate administration.
A nurse is preparing to administer nitroglycerin topical ointment to a client. Which of the following actions should the nurse plan to take?
Explanation
Choice A Reason:
Using the applicator paper is appropriate for measuring the dosage accurately, but simply measuring the dosage is not the only step; the medication needs to be spread over the specified area of the skin.
Choice B Reason:
Spread the medication over a 12.7 cm (5 in) area of the client's skin. Nitroglycerin ointment is typically measured using a specific paper or measuring tape provided with the medication to ensure accurate dosing. The ointment is spread thinly and evenly over a specific measured area of the skin, usually about 12.7 cm (5 inches) in length, to maintain consistent dosing.
Choice C Reason:
Covering the medication with a sterile gauze pad is not typically done with nitroglycerin ointment. The ointment is meant to be absorbed through the skin, and covering it may interfere with its absorption.
Choice D Reason:
Nitroglycerin ointment is often applied to different sites to prevent skin irritation and tolerance from developing at one site. It's usually rotated to different clean areas of the skin to prevent skin irritation and tolerance buildup. Applying it to the same site for three consecutive days is not standard practice.
A nurse is transcribing a new prescription for a client which states, "Diphenhydramine 50 mg NOW." Which of the following actions should the nurse take?
Explanation
Choice A Reason:
Contact the provider to clarify the prescription is not appropriate. Contacting the provider might not be necessary in this case. The prescription specifies "NOW," indicating an urgent administration, which is a clear directive to administer the medication promptly without further clarification.
Choice B Reason:
Administer the medication within 90 minutes is appropriate. "NOW" typically implies an urgent need for administration, and within a hospital setting, "NOW" often indicates a timeframe of around 90 minutes for prompt administration of the medication.
Choice C Reason:
Notify the pharmacy to send the medication immediately is inappropriate. With the prescription stating "NOW," the need for immediate administration usually requires using the hospital's available stock of the medication rather than waiting for delivery from the pharmacy. This action might cause a delay in administration.
Choice D Reason:
Inform the client there is a prescription available if needed is inappropriate. This option is not suitable in this scenario. "NOW" in the prescription implies the immediate need for administration, so informing the client about the availability of the prescription doesn't align with the urgency implied by the directive "NOW."
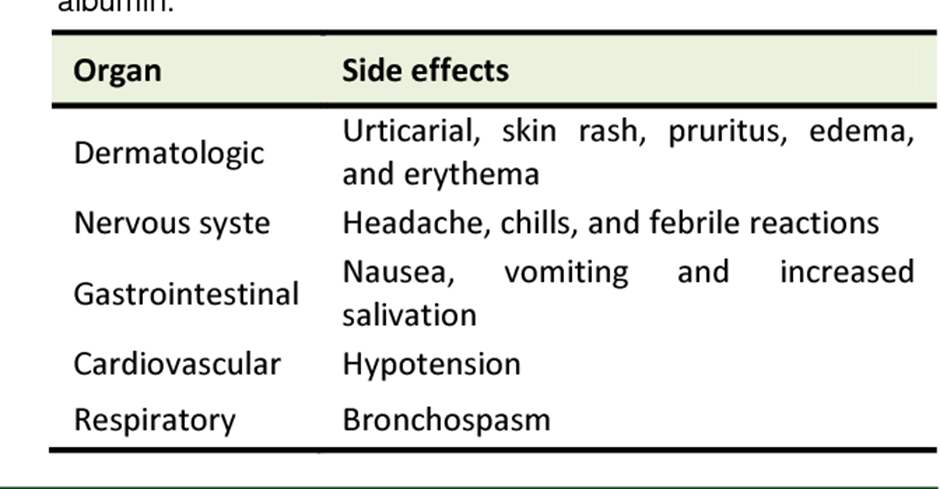
A nurse is caring for a client who is in shock and is receiving an infusion of albumin. Which of the following findings should the nurse expect?
Explanation
Choice A Reason:
Oxygen saturation within this range is generally considered adequate and might not directly correlate with the administration of albumin.
Choice B Reason:
Decrease in protein is incorrect. Albumin infusions are meant to supplement protein levels in the blood, so a decrease in protein wouldn't be an expected finding.
Choice C Reason:
Increase in blood pressure is correct. Albumin infusions can potentially help increase blood volume, leading to an increase in blood pressure. In shock, where there's a significant decrease in blood pressure due to reduced circulating volume, administering albumin or other intravenous fluids can help restore blood volume and consequently raise blood pressure towards a more stable range.
Choice D Reason:
PaCO2 of 30 mm Hg is incorrect. PaCO2 levels are related to respiratory function and the amount of carbon dioxide in the blood. While shock can impact various physiological parameters, a PaCO2 level of 30 mm Hg alone might not be directly tied to the administration of albumin in shock.
A nurse is caring for a client who has major depression and a new prescription for citalopram. Which of the following adverse effects is the priority for the nurse to report to the provider?
Explanation
Choice A Reason:
Weight loss is incorrect. While weight loss can be a side effect of citalopram, it's not typically considered a severe or urgent adverse effect that requires immediate reporting to the provider. It's more often observed in some individuals as a common side effect of this medication.
Choice B Reason:
Confusion can indicate a severe or uncommon adverse reaction to citalopram, especially in the context of treating major depression. It could potentially signify a serious condition that requires immediate attention. Reporting confusion promptly allows the healthcare provider to assess the situation and make appropriate adjustments to the medication regimen or provide additional interventions if necessary.
Choice C Reason:
Insomnia is incorrect. Insomnia is another potential side effect of citalopram. While it can affect the individual's quality of life, it's not typically an adverse effect that would be considered an urgent concern requiring immediate reporting to the provider.
Choice D Reason:
Bruxism is incorrect. Bruxism, or teeth grinding, is a less common side effect of citalopram. While it can cause discomfort or dental issues, it's not typically considered a priority adverse effect that necessitates immediate reporting to the provider compared to confusion, which might indicate a more serious or severe reaction.
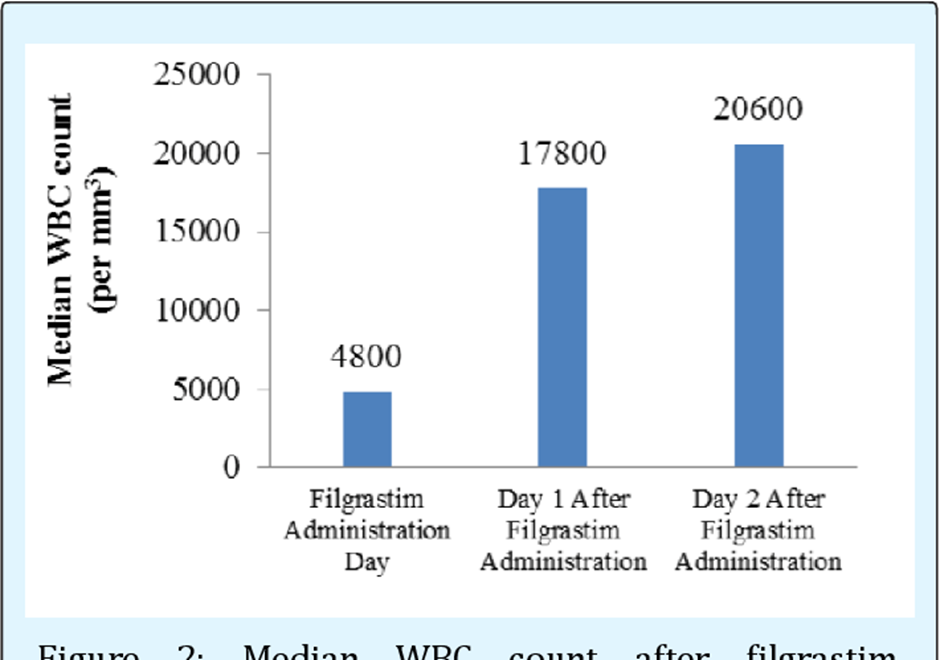
A nurse is reviewing the laboratory data of a client who is receiving filgrastim. Which of the following laboratory values should the nurse monitor to evaluate the effectiveness of the treatment?
Explanation
Choice A Reason:
INR (International Normalized Ratio) is incorrect. INR is a measurement used to monitor the effects of anticoagulants like warfarin. It assesses the blood's ability to clot. Filgrastim does not directly affect INR levels, so monitoring INR would not provide information about the effectiveness of filgrastim in stimulating white blood cell production.
Choice B Reason:
BUN (Blood Urea Nitrogen) is incorrect. BUN levels primarily indicate kidney function and hydration status. They are not directly influenced by filgrastim treatment. Monitoring BUN is essential for assessing kidney function but does not reflect the effectiveness of filgrastim therapy in increasing white blood cell counts.
Choice C Reason:
WBC count is correct. Filgrastim is a medication that stimulates the production of white blood cells (WBCs), particularly neutrophils. Therefore, the key laboratory value to monitor for assessing the effectiveness of filgrastim therapy is the WBC count. An increase in the WBC count, particularly in the neutrophil count, signifies the intended therapeutic effect of filgrastim in boosting the immune system's response by increasing the production of these infection-fighting cells.
Choice D Reason:
Potassium level is incorrect. Potassium levels are crucial for heart and muscle function. While certain medications might affect potassium levels, filgrastim's primary action is on stimulating white blood cell production and does not directly impact potassium levels. Monitoring potassium levels is essential for overall health but does not specifically indicate the effectiveness of filgrastim treatment.
A nurse is assessing a client who is receiving heparin via continuous IV. The client has an aPTT of 90 seconds. The nurse should monitor the client for which of the following changes in their vital signs?
Explanation
Choice A Reason:
Decreased respiratory rate is incorrect. Heparin administration and an elevated aPTT typically do not directly cause a decrease in respiratory rate. Respiratory rate changes might occur due to other factors such as respiratory conditions, pain, or medications affecting the respiratory center, but they are not commonly linked to heparin therapy.
Choice B Reason:
Increased blood pressure is incorrect. Heparin therapy and an elevated aPTT do not typically result in increased blood pressure. Heparin's primary effect is on preventing blood clotting, and while it can indirectly affect blood pressure by preventing clot formation, it doesn't typically cause a significant increase in blood pressure.
Choice C Reason:
Decreased temperature is incorrect. Heparin therapy and an elevated aPTT do not generally cause a decrease in body temperature. Changes in body temperature might occur due to various reasons such as infection, environmental factors, or certain medications, but they are not directly linked to heparin administration.
Choice D Reason:
Increased pulse rate is correct. An increased pulse rate can be an early indicator of bleeding or a potential side effect of heparin administration. Heparin's anticoagulant effect might predispose individuals to bleeding, so an increased pulse rate could indicate a response to potential bleeding complications rather than a direct effect of heparin itself.
A nurse is preparing to administer clindamycin to a client who states she forgot to report to the provider that she is allergic to penicillin. Which of the following actions should the nurse take?
Explanation
Choice A Reason:
Giving the prescribed dose of clindamycin is not appropriate due to the reported penicillin allergy, which increases the risk of an allergic reaction.
Choice B Reason:
Obtain a prescription for an alternative antibiotic is correct. Given the client's reported allergy to penicillin, which is in the same antibiotic class as clindamycin (both are antibiotics that belong to the beta-lactam group), there is a higher risk of cross-reactivity and potential allergic reaction. Therefore, it's important to avoid administering clindamycin in such cases and seek an alternative antibiotic that does not have a similar chemical structure to penicillin to prevent an allergic reaction.
Choice C Reason:
Premeditating the client with epinephrine before administering the antibiotic is not a standard practice in this context. Epinephrine is used to treat severe allergic reactions but is not used as a preventive measure before administering antibiotics.
Choice D Reason:
Administering the clindamycin using a desensitization schedule might be an option in certain situations under the guidance of an allergist or immunologist, but it's not typically performed by nurses and requires a specific protocol and expertise in managing drug allergies. Obtaining an alternative antibiotic is a more appropriate and immediate action to avoid the risk of an allergic reaction in this scenario.
A nurse is teaching a client who has a prescription for ferrous gluconate. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
Choice A Reason:
"I should notify my provider if my stools turn black." This is the appropriate statement. Ferrous gluconate is an iron supplement commonly prescribed to treat or prevent iron deficiency anemia. When taking iron supplements, it's common for stools to become darker or even black in color. This change in stool color is due to the iron and is generally harmless. However, it's essential to inform the healthcare provider about this change because it can also indicate bleeding in the gastrointestinal tract, which requires evaluation.
Choice B Reason:
Taking an antacid with iron supplements can interfere with iron absorption. Antacids may decrease the absorption of iron in the stomach, so it's not recommended to take them together.
Choice C Reason:
While staying upright after taking certain medications can help prevent esophageal irritation or reflux, it's not specifically required with ferrous gluconate.
Choice D Reason:
Taking iron supplements with milk is also not recommended as milk and calcium-containing products can inhibit the absorption of iron. It's generally best to take iron supplements on an empty stomach or with vitamin C to enhance absorption, unless otherwise instructed by the healthcare provider.
A nurse is caring for a client who is taking lithium and reports starting a new exercise program. The nurse should assess the client for which of the following electrolyte imbalances?
Explanation
Choice A Reason:
Hypomagnesemia is incorrect. Lithium therapy itself is not a direct cause of hypomagnesemia. While exercise can affect magnesium levels to some extent, it's not a primary electrolyte imbalance that is typically associated with lithium use or considered a significant concern specifically due to lithium.
Choice B Reason:
Hypocalcemia is incorrect. Similarly, lithium therapy is not a direct cause of hypocalcemia. Exercise can affect calcium metabolism, but it's not a primary electrolyte imbalance typically associated with lithium use or considered a significant concern specifically due to lithium.
When a client taking lithium begins a new exercise program, the nurse should primarily assess for the risk of:
Choice C Reason:
Hyponatremia is correct. Lithium can affect the body's regulation of sodium, and excessive sweating due to increased exercise can lead to sodium loss. This combination can potentially contribute to the development of hyponatremia (low sodium levels). Therefore, when a client on lithium starts a new exercise regimen that may induce sweating, monitoring for signs of hyponatremia becomes crucial. Symptoms of hyponatremia can include confusion, headaches, nausea, and in severe cases, seizures or coma.
Choice D Reason:
Hypokalemia is incorrect. Lithium itself does not commonly cause hypokalemia. Exercise can lead to potassium loss through sweating, but hypokalemia is not the primary electrolyte imbalance typically associated with lithium use or considered a significant concern specifically due to lithium.
A nurse is mixing regular insulin and NPH insulin in the same syringe prior to administering it to a client who has diabetes mellitus. Which of the following actions should the nurse take first?
Explanation
Choice A Reason:
Withdrawing the NPH insulin from the vial should come after injecting air into the NPH vial.
Choice B Reason:
Injecting air into the regular insulin vial should occur after withdrawing the NPH insulin from its vial.
Choice C Reason:
Inject air into the NPH vial is correct. The sequence for mixing regular insulin (clear) and NPH insulin (cloudy) in the same syringe typically involves injecting air into the NPH (cloudy) insulin vial first. This step prevents excess pressure buildup when withdrawing the solution, making it easier to draw the correct amount of NPH insulin into the syringe.
Choice D Reason:
Withdrawing the regular insulin from the vial should occur after withdrawing the correct amount of NPH insulin into the syringe.
A nurse is reviewing the medication administration record for a client who has cancer and is receiving morphine via a PCA pump. Which of the following prescriptions should the nurse clarify with the provider?
Explanation
Choice A Reason:
Ondansetron is incorrect. Ondansetron is an anti-nausea medication commonly used in cancer patients to manage nausea and vomiting, often caused by chemotherapy. It's not typically contraindicated or known to interact significantly with morphine administered via a PCA pump. This combination is often used to manage both pain and associated symptoms in cancer patients.
Choice B Reason:
Acetaminophen is incorrect. Acetaminophen is a pain reliever and fever reducer that doesn't typically interact significantly with morphine administered via a PCA pump. It's often used concurrently with other pain medications to manage discomfort in cancer patients. There isn't a known significant interaction between acetaminophen and morphine when used appropriately.
Choice C Reason:
Nalbuphine is correct. Nalbuphine is an opioid analgesic, similar to morphine, and administering it concurrently with morphine could potentially lead to opioid overdose or increased risk of opioid-related side effects such as respiratory depression. Thus, it's crucial to clarify with the provider whether there might be a potential interaction or if both medications are indeed necessary in this specific clinical scenario.
Choice D Reason:
Insulin glargine is incorrect. Insulin glargine is a long-acting insulin used to manage blood sugar levels in individuals with diabetes. While its interaction with morphine isn't typically a concern, it's essential to monitor blood sugar levels closely in individuals receiving opioids like morphine, as opioids can affect glucose metabolism and may necessitate adjustments in insulin dosage.
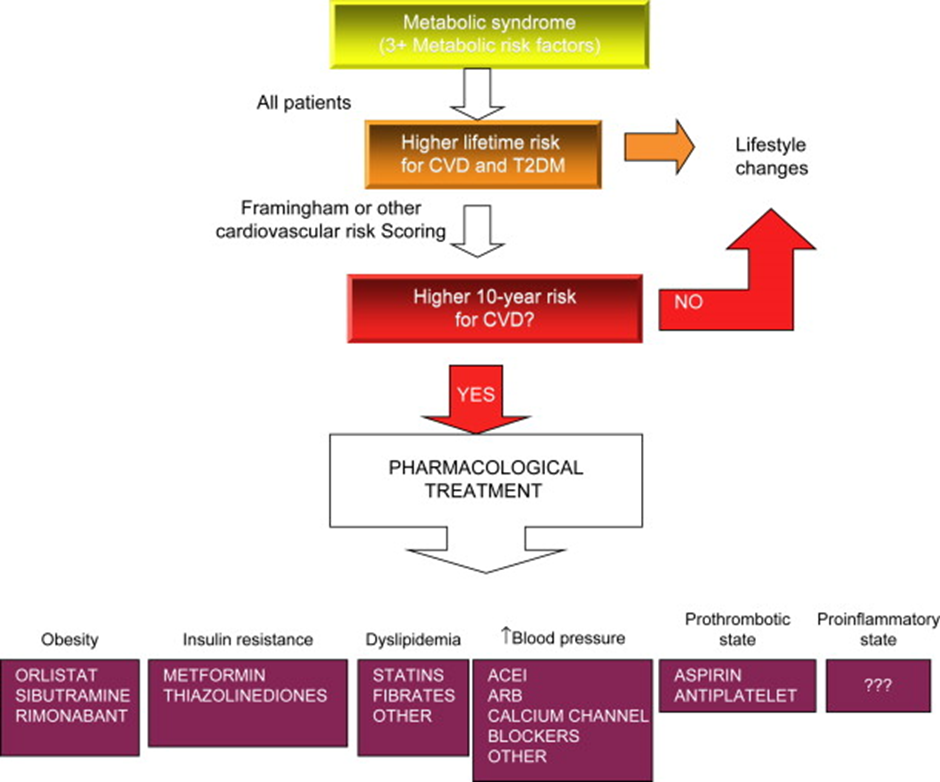
A nurse in a provider's office is preparing to teach a middle adult client who has a new diagnosis of metabolic syndrome and an HbA1c of 6.5%. Which of the following medications should the nurse plan to teach the client about first?
Explanation
Choice A Reason:
Regular insulin is incorrect. Regular insulin is a short-acting insulin used for managing diabetes, particularly for controlling blood sugar levels during meals. However, it's not typically the initial medication introduced in the management of metabolic syndrome with an HbA1c of 6.5%. Insulin therapy is generally considered when other medications or lifestyle changes aren't effective in controlling blood sugar levels.
Choice B Reason:
Exenatide is incorrect. Exenatide is a GLP-1 receptor agonist, used to manage type 2 diabetes. While it's effective in controlling blood sugar levels, it's often considered after initial treatments like metformin, especially in newly diagnosed cases or those with moderately elevated HbA1c levels.
Choice C Reason:
Insulin glargine is incorrect. Insulin glargine is a long-acting insulin used in diabetes management, providing a steady level of insulin throughout the day. Like regular insulin, insulin glargine is typically considered later in the treatment plan and is not usually the first medication introduced in cases of new metabolic syndrome diagnoses with moderately elevated HbA1c levels.
Choice D Reason:
Considering the client's new diagnosis and moderately elevated HbA1c level, educating about metformin aligns with the typical first-line approach in managing blood sugar levels and metabolic syndrome in this scenario.
A nurse is caring for a group of clients. For which of the following situations should the nurse complete an incident report?
No explanation
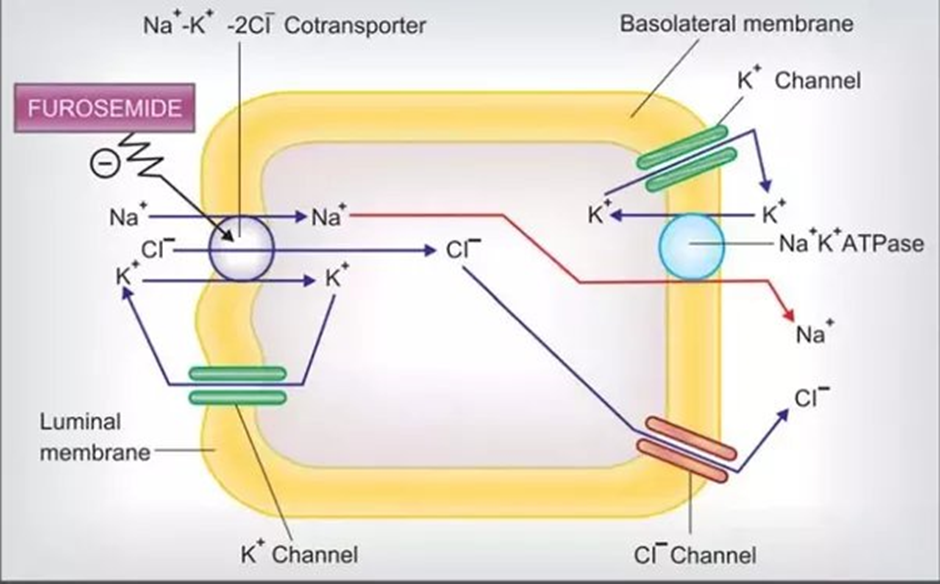
A nurse is reviewing a client's laboratory results before administering furosemide 40 mg IV bolus. For which of the following values should the nurse withhold the medication and contact the provider?
Explanation
Choice A Reason:
Sodium 141 mEq/L is incorrect. This value is within the normal range (usually around 135-145 mEq/L).
Choice B Reason:
Potassium 2.5 mEq/ is correct. Furosemide, a loop diuretic, can lead to potassium loss through increased urine output. If a client already has a low potassium level (hypokalemia), administering furosemide can further decrease potassium levels, potentially causing or worsening hypokalemia. Hypokalemia can lead to various complications, including cardiac arrhythmias.
Choice C Reason:
WBC count 8,000/mm3 is incorrect. This value falls within the normal range for white blood cell count.
Choice D Reason:
INR 1.0: An INR of 1.0 is within the normal range for a person not on anticoagulation therapy.
Sign Up or Login to view all the 53 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

