RN VATI Pharmacology S 2019
Total Questions : 41
Showing 25 questions, Sign in for moreA nurse is caring for a client who is receiving meperidine. Which of the following is the nurse's priority assessment before administering the medication?
Explanation
A. Urinary retention: While urinary retention can be a side effect of meperidine and other opioids, it is not the priority assessment before administering the medication. Urinary retention is a concern but is not immediately life-threatening compared to other potential side effects of opioids, such as respiratory depression. Assessing urinary retention is important, but it is not the primary concern in this situation.
B. Vomiting: Vomiting can also be a side effect of opioids, including meperidine. While it is essential to assess for vomiting and its potential impact on the client's overall condition, it is not the priority assessment before administering the medication. Vomiting can be managed, and the nurse should address it as needed. However, the priority assessment is one that can affect the client's immediate safety and well-being, such as respiratory rate and potential respiratory depression.
C. Respiratory rate: This is the correct answer. The priority assessment before administering meperidine is the client's respiratory rate. Opioids can cause respiratory depression, leading to reduced breathing and inadequate ventilation. Monitoring the respiratory rate allows the nurse to detect any signs of respiratory distress or inadequate breathing, enabling them to intervene promptly to prevent serious complications.
D. Level of consciousness: While assessing the client's level of consciousness is essential for overall assessment and monitoring, it is not the priority assessment before administering meperidine. Respiratory depression due to opioid use can occur even when the client is conscious. However, if respiratory depression occurs, it can lead to a decrease in consciousness and potentially unconsciousness, making the assessment of respiratory rate more critical to prevent such complications.

A nurse is caring for a client who has a new prescription for metformin. Which of the following laboratory results should the nurse evaluate prior to administering the first dose?
Explanation
Before administering the first dose of metformin, the nurse should evaluate the client's creatinine level. Metformin is primarily excreted by the kidneys, and its clearance from the body depends on the renal function. If the client has impaired kidney function, metformin can accumulate in the body and lead to potential adverse effects, particularly lactic acidosis.
Monitoring the creatinine level helps assess the client's kidney function and determines whether it is safe to administer metformin. If the creatinine level is elevated, indicating reduced kidney function, the nurse should consult with the healthcare provider to determine the appropriate dose adjustment or consider an alternative treatment option.
Let's go through the other options and explain why they are not the priority laboratory results to evaluate before administering metformin:
A. Potassium level: While monitoring potassium levels is important in some situations, it is not a primary concern before administering metformin. Metformin does not have a significant effect on potassium levels, and it is not a medication known for causing hypokalemia (low potassium levels).
C. Platelet count: Metformin does not have a direct impact on platelet count, and evaluating platelet count is not typically required before starting metformin therapy. Platelet count monitoring may be relevant for certain other medications or medical conditions, but it is not specific to metformin administration.
D. Liver enzymes: While it is essential to monitor liver function in clients on long-term metformin therapy, evaluating liver enzymes before the first dose of metformin is not the priority. Metformin is primarily cleared by the kidneys, and liver enzymes are not directly affected by its initial administration. However, ongoing monitoring of liver function may be necessary during long-term
A nurse is providing teaching for a client who has a new prescription for rifampin. Which of the following statements should the nurse include?
Explanation
The nurse should include the statement that rifampin can cause the client's urine to turn orange. Rifampin is an antibiotic commonly used to treat tuberculosis and other bacterial infections. One of its common side effects is discoloration of bodily fluids, including urine, saliva, sweat, and tears. This discoloration is harmless and is not a cause for concern. Informing the client about this side effect helps prevent unnecessary worry or alarm.
"You should take this medication with food" (B) is not specifically related to rifampin. However, taking rifampin with food can help reduce gastrointestinal side effects such as stomach upset or nausea.
"This medication can cause insomnia" (C) is not a common side effect of rifampin. Insomnia is more commonly associated with certain other medications or medical conditions.
"You should take a stool softener with this medication" (D) is not necessary for rifampin. Stool softeners are typically used to alleviate constipation, but rifampin does not commonly cause constipation as a side effect.
Therefore, the nurse should primarily include the statement that rifampin can cause the client's urine to turn orange.
A nurse accidently removes celecoxib from an automated medication dispensing system (AMDS) instead of citalopram and almost administers the wrong medication to a client. Which of the following actions should the nurse take?
Explanation
When a medication error occurs, the nurse should report the incident to the nurse manager or appropriate supervisor. It is essential to follow the facility's policies and procedures for reporting and managing medication errors. Prompt reporting allows for appropriate investigation, documentation, and implementation of necessary measures to prevent future errors.
Documenting that the pharmacy sent the incorrect medication (B) is not appropriate in this situation, as it does not address the nurse's role and responsibility in the error. Reporting the incident is the primary action required.
Contacting the provider to change the client's prescription (C) is not necessary in this case, as the error was related to the medication selection during administration, not an issue with the prescription itself.
Placing the unwrapped celecoxib back into the AMDS (D) is not appropriate. Once a medication has been removed from its packaging or container, it should not be returned to the dispensing system. Additionally, since it was the wrong medication for the client, it should not be administered.
Therefore, the nurse should primarily report the incident to the nurse manager or appropriate supervisor to ensure appropriate handling of the medication error.
A nurse discovers that a client has been administered a higher dose of oxybutynin than the prescription indicates. The nurse should assess the client for which of the following adverse effects?
Explanation
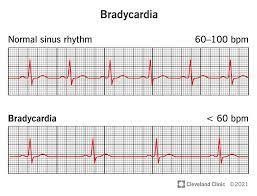
Oxybutynin is an anticholinergic medication commonly used to treat urinary incontinence. One of the adverse effects of anticholinergic medications is the potential for bradycardia, which refers to a slower than normal heart rate. Anticholinergic medications can inhibit the effects of acetylcholine, a neurotransmitter responsible for regulating various bodily functions, including heart rate. Therefore, it is important to assess the client for signs of bradycardia after an unintended higher dose of oxybutynin.
Increased salivation (A) is not an expected adverse effect of oxybutynin. In fact, anticholinergic medications like oxybutynin often have the opposite effect, causing dry mouth and reduced salivation.
Hyperthermia (B) is not a typical adverse effect of oxybutynin. It is more commonly associated with other conditions or medications.
Urinary incontinence (C) is the condition that oxybutynin is intended to treat. It is not an adverse effect but rather the therapeutic effect of the medication.
A nurse is reviewing the medical record of a client who has a new prescription for verapamil. Which of the following findings in the client's medical record should the nurse identify as a contraindication for the administration of verapamil?
Explanation
The nurse should identify a history of asthma as a contraindication for the administration of verapamil. Verapamil is a calcium channel blocker commonly used to treat high blood pressure, angina, and certain heart rhythm disorders. However, it can cause bronchospasm and worsen symptoms in individuals with asthma or other reactive airway diseases. Therefore, verapamil should be avoided in clients with a history of asthma.
History of heart failure (B) is not a contraindication for verapamil use. In fact, verapamil is sometimes prescribed for certain types of heart failure. However, caution is required and careful monitoring is necessary in clients with heart failure.
Systolic blood pressure of 110 mm Hg (C) is not a contraindication for verapamil. Verapamil is often prescribed to lower blood pressure. However, it may require dose adjustments based on the client's blood pressure response.
Blood creatinine level of 1.0 mg/dL (D) is within the normal range and does not pose a contraindication for verapamil use.
A nurse is assessing a client who has ovarian cancer and is receiving paclitaxel. Which of the following findings is the priority for the nurse to report to the provider?
Explanation
A. Alopecia: Alopecia, or hair loss, is a common side effect of many chemotherapy drugs, including paclitaxel. While it can be distressing for the client, alopecia is not a life-threatening side effect and does not require immediate intervention. It is essential for the nurse to provide emotional support to the client experiencing hair loss and educate them about potential ways to cope with it.
B. Muscle pain: Muscle pain, also known as myalgia, is another common side effect of paclitaxel and many other chemotherapy agents. While it can cause discomfort for the client, myalgia is generally managed with pain medications and supportive care. It is not a priority finding that requires immediate reporting to the provider unless it becomes severe or debilitating.
C. Nausea: Nausea is a well-known side effect of chemotherapy, including paclitaxel. It is often managed with antiemetic medications and other supportive measures. While severe or persistent nausea can lead to dehydration and other complications, it is not an immediate life-threatening concern in most cases.
D. Bradycardia: This is the correct answer. Bradycardia (slow heart rate) is a less common but more concerning side effect of paclitaxel. It may indicate potential cardiac toxicity, which is a serious and potentially life-threatening complication. The healthcare provider should be notified promptly so that appropriate evaluation and intervention can be initiated to manage any cardiac issues and prevent further complications.
A nurse is assessing a client who is receiving IV ciprofloxacin to treat a urinary tract infection. Which of the following findings should the nurse identify as the priority to report to the provider?
Explanation
When assessing a client receiving ciprofloxacin, the nurse should prioritize reporting tendon pain when walking to the provider. Ciprofloxacin is a fluoroquinolone antibiotic that can rarely cause tendonitis or tendon rupture, particularly in the Achilles tendon. Tendon pain, especially when associated with difficulty walking, can be indicative of a serious adverse effect and requires immediate attention and evaluation by the provider.
Nausea and vomiting (A) are common side effects of ciprofloxacin but are typically not considered urgent or life-threatening. They can often be managed with supportive care measures and may not require immediate intervention.
Daytime drowsiness (B) is not typically associated with ciprofloxacin and may be unrelated to the medication. It should be assessed and reported if it persists or is severe, but it is not a priority finding specifically related to ciprofloxacin administration.
Photosensitivity (D) is a known side effect of ciprofloxacin, but it is not typically considered a priority finding unless it is severe or causing significant discomfort. Adequate sun protection measures can help manage photosensitivity.
A nurse is providing teaching for a client who has a prescription for gentamicin. Which of the following should the nurse include as an adverse effect of this medication?
Explanation
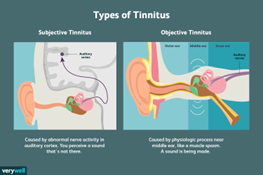
The nurse should include tinnitus (ringing in the ears) as an adverse effect of gentamicin in the client's teaching. Gentamicin is an aminoglycoside antibiotic commonly used to treat bacterial infections. One of the potential side effects of gentamicin is damage to the inner ear, which can lead to tinnitus.
Tinnitus is a concerning symptom as it may indicate ototoxicity, which is damage to the structures of the inner ear responsible for hearing and balance. If the client experiences tinnitus while taking gentamicin, it is essential to notify the healthcare provider immediately to assess the severity of the issue and consider appropriate interventions.
Let's go through the other options and explain why they are not adverse effects of gentamicin:
A. Urinary frequency: Urinary frequency is not a common adverse effect of gentamicin. Gentamicin primarily affects the kidneys, and its main concern is related to potential nephrotoxicity (kidney damage) rather than causing urinary frequency.
B. Constipation: Constipation is not an adverse effect typically associated with gentamicin. Gentamicin is not known to affect the gastrointestinal system or cause constipation.
C. Hypertension: Hypertension (high blood pressure) is not a known adverse effect of gentamicin. Gentamicin primarily affects the kidneys and the inner ear, as mentioned earlier, but it does not significantly impact blood pressure.
A nurse is caring for a client who has fluid volume excess and received furosemide 40 mg via intermittent IV bolus 1 hr ago. Which of the following findings indicates that the medication has been effective?
Explanation
Furosemide is a loop diuretic commonly used to treat fluid volume excess by promoting diuresis. One of the expected outcomes of furosemide administration is an increased urinary output as excess fluid is eliminated from the body. Therefore, if the medication has been effective, the nurse would expect to see an increased urinary output as a result of the diuretic effect.
Increased respiratory rate (B) is not an expected outcome of furosemide administration. It may occur in some cases due to increased fluid elimination and potential electrolyte imbalances, but it is not the primary indicator of the medication's effectiveness.
Decreased blood pressure (C) is a possible outcome of furosemide administration due to the diuretic effect and subsequent reduction in fluid volume. However, it is not the most specific indicator of the medication's effectiveness in this case.
Increased pulse (D) is not a typical finding associated with the effectiveness of furosemide. In fact, furosemide can sometimes cause a decrease in heart rate due to its impact on fluid and electrolyte balance.
A nurse who is caring for a preschooler should question a prescription for which of the following antibiotics?
Explanation
A nurse who is caring for a preschooler should question a prescription for tetracycline. Tetracycline is contraindicated in children under 8 years of age due to its potential to cause permanent discoloration and damage to developing teeth and bones. This adverse effect is known as tooth staining or dental hypoplasia.
Let's go through the other options:
A. Azithromycin: Azithromycin is an appropriate antibiotic for use in preschool-age children and is commonly prescribed for various bacterial infections. It does not pose the same risk of tooth staining as tetracycline, making it a safe option for this age group.
C. Cefuroxime: Cefuroxime is another antibiotic that is safe for use in preschoolers. It belongs to the cephalosporin class of antibiotics and is commonly prescribed for respiratory tract infections, skin infections, and other bacterial infections.
D. Gentamicin: While gentamicin is an effective antibiotic, its use in preschool-age children should be carefully monitored. Gentamicin can have potential ototoxic and nephrotoxic effects (damage to the inner ear and kidneys, respectively). However, its use is not strictly contraindicated in this age group, and it can be prescribed when necessary with appropriate monitoring.
A nurse is caring for a client who is receiving diazepam as sedation for an endoscopy, Which of the following antidotes should the nurse have on hand during the procedure?
Explanation
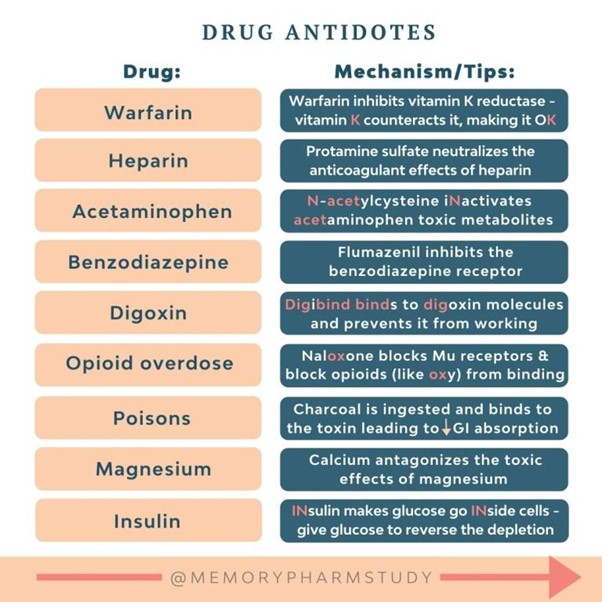
Flumazenil is the antidote for diazepam, which is a benzodiazepine. Flumazenil is a selective antagonist that can reverse the sedative effects of benzodiazepines and is commonly used in cases of benzodiazepine overdose or to reverse sedation after procedures.
Naloxone (A) is the antidote for opioid overdose and would not be appropriate for reversing the effects of diazepam.
Atropine (B) is an anticholinergic medication used to increase heart rate and is not specific to the reversal of diazepam sedation.
Neostigmine (D) is a cholinesterase inhibitor used to reverse the effects of non-depolarizing neuromuscular blocking agents and is not indicated for reversing the effects of diazepam.
A nurse in the PACU is caring for a client who received isoflurane. Which of the following assessments is the nurse's priority?
Explanation
A. Intake and output: Monitoring intake and output is essential in the postoperative care of a client to assess fluid balance and kidney function. However, it is not the priority assessment when the client has received isoflurane in the PACU. The priority assessment in this situation is related to the potential cardiovascular side effect of isoflurane, which is hypotension. Hypotension can have immediate and significant implications for the client's perfusion and overall well-being, requiring prompt attention and intervention.
B. Non-verbal pain cues: Assessing for pain is important in the postoperative period to ensure adequate pain management and comfort for the client. However, it is not the priority assessment when the client has received isoflurane in the PACU. The priority assessment at this time is related to the potential cardiovascular impact of the anesthesia, which is blood pressure. Addressing hypotension takes precedence over pain assessment as it poses a more immediate threat to the client's well-being.
C. Bowel sounds: Assessing bowel sounds is part of a comprehensive postoperative assessment to monitor the return of bowel function after surgery. While it is important, it is not the priority assessment when the client has received isoflurane in the PACU. The priority assessment in this situation is related to the potential cardiovascular side effect of the anesthesia, which is blood pressure. Monitoring and managing hypotension is of greater concern in the immediate postoperative period.
D. Blood pressure: This is the correct answer. The priority assessment for a client who received isoflurane in the PACU is the blood pressure. Isoflurane is an inhalation anesthetic that can cause hypotension (low blood pressure). Monitoring the client's blood pressure is crucial to promptly identify and address any hypotension, as it can lead to inadequate tissue perfusion and oxygenation. Addressing blood pressure deviations is essential for the client's cardiovascular stability and overall recovery in the PACU.
A nurse is caring for a client who is receiving long-term treatment with oral doses of prednisone. For which of the following adverse effects should the nurse monitor?
Explanation
The nurse should monitor the client receiving long-term treatment with oral doses of prednisone for the development of osteoporosis. Prednisone is a corticosteroid medication that can lead to decreased bone density and increase the risk of fractures. Prolonged use of prednisone can interfere with calcium absorption and increase bone resorption, leading to osteoporosis.
Hypoglycemia (A) is not a common adverse effect of prednisone. In fact, prednisone can cause hyperglycemia and increase the risk of developing diabetes.
Hyperreflexia (B) is not typically associated with prednisone use. Hyperreflexia is an exaggerated reflex response and is not a common adverse effect of corticosteroid therapy.
Inflammatory bowel disease (D) is not an adverse effect of prednisone. In fact, prednisone is often used as a treatment for inflammatory bowel disease to reduce inflammation and symptoms.
Therefore, the nurse should primarily monitor the client for the development of osteoporosis when receiving long-term treatment with oral doses of prednisone.
A nurse is caring for a client who is receiving diazepam as conscious sedation for an endoscopy, Which of the following antidotes should the nurse have on hand during the procedure?
Explanation
Flumazenil is the antidote for diazepam, which is a benzodiazepine. Flumazenil is a selective antagonist that can reverse the sedative effects of benzodiazepines and is commonly used in cases of benzodiazepine overdose or to reverse sedation after procedures.
Naloxone (A) is the antidote for opioid overdose and would not be appropriate for reversing the effects of diazepam.
Atropine (B) is an anticholinergic medication used to increase heart rate and is not specific to the reversal of diazepam sedation.

Neostigmine (D) is a cholinesterase inhibitor used to reverse the effects of non-depolarizing neuromuscular blocking agents and is not indicated for reversing the effects of diazepam.
A nurse is assessing a client who is receiving total parenteral nutrition (TPN). Which of the following findings should the nurse identify as an adverse effect of TPN
Explanation
TPN is a form of nutrition given intravenously to provide essential nutrients when a client is unable to consume an adequate oral diet. One of the potential adverse effects of TPN is fluid overload, which can manifest as peripheral edema. The presence of 2+ peripheral pitting edema indicates the accumulation of excess fluid in the tissues. It is important for the nurse to monitor the client's fluid balance closely and assess for signs of fluid overload, such as edema, to prevent complications.
A nurse is caring for a client who is starting to take aspirin 81 mg daily. Which of the following findings should the nurse identify as a risk factor for the client's development of an aspirin-induced ulcer?
Explanation
Smoking is a known risk factor for the development of aspirin-induced ulcers. It can increase the risk of gastrointestinal bleeding and compromise the integrity of the gastric mucosa. Smoking can also impair the healing process and increase the risk of complications associated with ulcers.
While the other factors mentioned in the options may have their own health implications, smoking is specifically associated with an increased risk of aspirin-induced ulcers. Therefore, the nurse should identify the client's smoking habit as a risk factor for the development of an aspirin-induced ulcer.
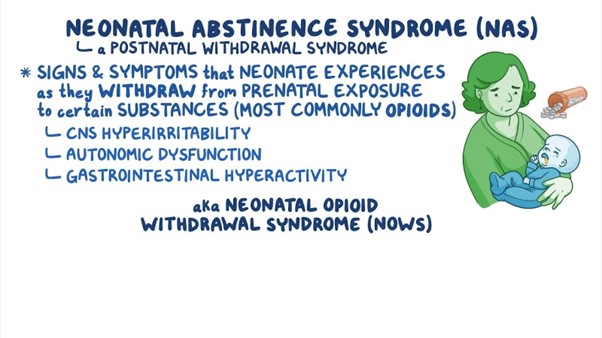
A nurse is assessing a neonate who was exposed to heroin in utero. Which of me following findings should the nurse identify as an indication that the neonate is experiencing neonatal abstinence syndrome?
Explanation
Neonatal abstinence syndrome (NAS) is a group of withdrawal symptoms that occur in newborns who were exposed to drugs, including heroin, in utero. Hyporeflexia, which refers to reduced or diminished reflexes, is one of the key findings in neonates experiencing NAS.
During pregnancy, when the mother uses opioids like heroin, the baby becomes dependent on the drug. After birth, when the drug is no longer available, the baby experiences withdrawal symptoms as the body adjusts to the absence of the drug. Hyporeflexia is a common manifestation of NAS and is observed due to the central nervous system's response to the withdrawal.
Let's go through the other options:
B. Frequent yawning: While yawning can be seen in neonates with NAS, it is not as specific to the condition as hyporeflexia. Yawning can occur for various reasons and may not always be indicative of NAS.
C. Respiratory depression: Respiratory depression can be a severe complication of opioid exposure in utero and can result in life-threatening situations for the neonate. However, it is not specific to NAS. Respiratory depression is more closely associated with opioid overdose in the newborn, which can be a separate concern from NAS.
D. Constipation: Constipation is a possible symptom in neonates experiencing NAS, but it is not as specific as hyporeflexia. Constipation can occur due to various factors and is not unique to NAS.
A nurse is providing discharge teaching to a client who has a prescription for enoxaparin. Which of the following instructions should the nurse include in the teaching?
Explanation
When providing discharge teaching to a client with a prescription for enoxaparin, the nurse should include the instruction to expel the air bubble prior to injecting the medication. Enoxaparin is a type of anticoagulant medication that is administered as a subcutaneous injection.
Here's why the other options are incorrect:
A. Insert the needle at a 45 angle: Enoxaparin is typically administered as a subcutaneous injection, where the needle is inserted at a 90-degree angle (straight into the skin). A 45-degree angle is used for intramuscular injections, but it is not appropriate for enoxaparin administration.
B. Inject the medication into a muscle: Enoxaparin is not intended to be injected into a muscle. It is a low-molecular-weight heparin designed for subcutaneous administration, meaning it is injected just below the skin into the fatty tissue.
C. Rub the injection site following administration: Rubbing the injection site after administering enoxaparin or any other subcutaneous medication is not recommended. Rubbing the site can cause irritation and bruising. Instead, the nurse should apply gentle pressure with a cotton ball or gauze pad for a few seconds after the injection to help minimize bleeding.
A nurse is assessing a client who is experiencing an anaphylactic reaction to an antibiotic. Which of the following manifestations of anaphylaxis should the nurse expect?
Explanation
The nurse should expect angioedema as one of the manifestations of anaphylaxis in a client experiencing an allergic reaction to an antibiotic. Angioedema is a severe swelling that occurs beneath the skin, typically affecting the face, lips, tongue, throat, or other body parts. It is a result of the release of histamine and other inflammatory mediators in response to the allergen.
Anaphylaxis is a life-threatening allergic reaction that can occur rapidly and affect multiple body systems. In addition to angioedema, other common manifestations of anaphylaxis include:
-
Difficulty breathing or wheezing due to bronchospasm
-
Hives or urticaria, which are itchy raised skin rashes
-
Severe itching or tingling sensation
-
Rapid and weak pulse
-
Low blood pressure leading to hypotension
-
Nausea, vomiting, or diarrhea
-
Feeling of impending doom or anxiety
Let's go through the other options:
A. Hypertonic reflexes: This is not a manifestation of anaphylaxis. "Hypertonic reflexes" are not typically associated with allergic reactions or anaphylaxis. Hypertonic reflexes refer to increased muscle tone, but they are not part of the usual presentation of anaphylaxis.
B. Increase in systolic blood pressure: Anaphylaxis usually leads to a decrease in blood pressure rather than an increase. The decrease in blood pressure can be severe and result in shock, which is a life-threatening condition.
D. Urinary retention: Urinary retention is not a common manifestation of anaphylaxis. Anaphylaxis primarily affects the respiratory and circulatory systems, leading to airway constriction, difficulty breathing, and cardiovascular collapse. Urinary retention is not directly related to the pathophysiology of anaphylaxis.

A nurse is reviewing the laboratory results of a client who has been taking warfarin for 3 months. Which of the following laboratory results Indicates that the medication has been effective?
Explanation
A. Hemoglobin level: The hemoglobin level measures the amount of hemoglobin, the oxygen-carrying protein in red blood cells, in the blood. Warfarin is not directly responsible for increasing or decreasing the hemoglobin level. While warfarin can lead to bleeding complications in some cases, it does not specifically target the hemoglobin level, so it is not a direct indicator of the medication's effectiveness.
B. Platelet count: The platelet count measures the number of platelets in the blood, which are essential for blood clotting. Warfarin does not directly affect platelet production or count. It works by inhibiting the production of certain clotting factors, not by affecting platelets. Monitoring the platelet count is important, but it is not an indicator of warfarin's effectiveness in preventing excessive clotting.
C. Prothrombin time (PT) or activated partial thromboplastin time (aPTT): Prothrombin time (PT) and activated partial thromboplastin time (aPTT) are coagulation tests used to assess different types of anticoagulant medications, such as heparin. Warfarin's effect is measured using the International Normalized Ratio (INR). PT and aPTT are not specific to warfarin therapy and are not used to monitor its effectiveness. The INR is the appropriate laboratory test for assessing the efficacy of warfarin therapy.
D. International Normalized Ratio (INR): This is the correct answer. The International Normalized Ratio (INR) is the laboratory test used to monitor the effectiveness of warfarin therapy. The INR measures the time it takes for the blood to clot and reflects the anticoagulant effect of warfarin. A therapeutic INR within the target range (e.g., INR = 2.0 to 3.0 for most indications) indicates that warfarin has been effective in preventing excessive clotting and reducing the risk of complications associated with blood clots.
A nurse is providing teaching to a client who has chronic rheumatoid arthritis and a new prescription for hydroxychloroquine. The nurse should instruct the client to obtain which of the following diagnostic studies routinely?
Explanation
When providing teaching to a client with chronic rheumatoid arthritis who is starting a new prescription for hydroxychloroquine, the nurse should instruct the client to obtain routine eye examinations. Hydroxychloroquine is an antimalarial and immunosuppressive medication commonly used to treat rheumatoid arthritis and other autoimmune conditions.
One of the potential side effects of hydroxychloroquine is ocular toxicity, particularly affecting the retina. Retinal toxicity can lead to vision changes or, in severe cases, irreversible damage to the eyes. Therefore, regular eye examinations are necessary to monitor for any signs of retinal toxicity and detect any visual changes early to prevent further complications.
The American Academy of Ophthalmology recommends that patients taking hydroxychloroquine undergo a baseline eye examination before starting the medication and annual eye examinations thereafter, especially after five years of continuous use.
Let's go through the other options:
B. Chest x-ray: A chest x-ray is not routinely required for monitoring clients taking hydroxychloroquine for rheumatoid arthritis. Hydroxychloroquine is not known to cause significant respiratory or pulmonary side effects.
C. Pancreatic enzyme levels: Monitoring pancreatic enzyme levels is not specifically related to hydroxychloroquine therapy. Pancreatic enzyme level testing is typically used to assess the function of the pancreas in conditions like pancreatitis or pancreatic insufficiency.
D. Urinalysis screening: While regular monitoring of kidney function is important for clients on long-term medication therapy, routine urinalysis screening is not specifically related to hydroxychloroquine use in clients with rheumatoid arthritis. Regular eye examinations are of higher priority due to the potential ocular toxicity associated with this medication.
A nurse is caring for a client who has a magnesium level of 3.2 mEq/L. Which of the following medications should the nurse expect to administer?
Explanation
A client with a magnesium level of 3.2 mEq/L has a higher-than-normal magnesium level, indicating hypermagnesemia. The nurse should expect to administer calcium gluconate.
Calcium gluconate is the antidote for hypermagnesemia, as it works to antagonize the effects of magnesium on the body. By administering calcium gluconate, the nurse can help counteract the effects of excess magnesium and normalize the client's magnesium levels.
Let's go through the other options:
B. Calcitonin: Calcitonin is not used to treat hypermagnesemia. Calcitonin is a hormone that regulates calcium and phosphorus levels in the body. It is used in certain conditions, such as hypercalcemia (high calcium levels), but it is not indicated for hypermagnesemia.
C. Magnesium oxide: Magnesium oxide is a form of magnesium supplement, and it is not appropriate for a client with hypermagnesemia, as it would further increase the magnesium level, exacerbating the condition.
D. Magnesium sulphate: Magnesium sulfate is also not appropriate for a client with hypermagnesemia, as it would further elevate the magnesium levels in the body. Magnesium sulfate is often used to treat magnesium deficiency or as a tocolytic agent to prevent premature labor.
A nurse is caring for a client who has congestive heart failure and is taking captopril. Which of the following laboratory values should the nurse report to the provider as a potential adverse effect of captopril?
Explanation
The nurse should report a creatinine level of 2 mg/dl to the provider as a potential adverse effect of captopril. Captopril is an angiotensin-converting enzyme (ACE) inhibitor commonly used to treat congestive heart failure and hypertension. One of the side effects of ACE inhibitors, including captopril, is the potential to cause kidney problems, leading to an increase in serum creatinine levels.
An increase in serum creatinine may indicate impaired kidney function, and it is essential to monitor kidney function regularly in clients taking ACE inhibitors. Elevated creatinine levels can suggest reduced glomerular filtration rate (GFR) and impaired kidney function, which may require adjustments in medication dosage or further evaluation and management.
Let's go through the other options:
A. Absolute neutrophil count (ANC) 4.000/ mm^3: An absolute neutrophil count of 4.000/ mm^3 is within the normal range, so it is not an adverse effect of captopril that requires immediate reporting.
B. Brain natriuretic peptide (BNP) 90 ng/L: A brain natriuretic peptide (BNP) level of 90 ng/L is used to assess heart failure severity. While BNP levels can be helpful in managing congestive heart failure, a BNP level of 90 ng/L is not an adverse effect of captopril that requires immediate reporting.
C. Sodium 140 mEq/l: A sodium level of 140 mEq/L is within the normal range, so it is not an adverse effect of captopril that requires immediate reporting.
A nurse is preparing to administer exenatide for a client who has type 2 diabetes mellitus. Which of the following routes of administration should nurse plan to use?
Explanation
Exenatide is a medication used to treat type 2 diabetes mellitus. The nurse should plan to administer exenatide via the subcutaneous route.
Subcutaneous administration involves injecting the medication into the fatty tissue just below the skin. Exenatide is available as a subcutaneous injection and is typically given in the abdomen, thigh, or upper arm.
Let's go through the other options:
A. Oral: Exenatide is not available in an oral form. It is a peptide-based medication that would be destroyed by stomach acid and digestive enzymes if taken orally. Therefore, it must be administered via injection to be effective.
B. Intramuscular: Exenatide is not administered intramuscularly. Intramuscular injections are given deep into the muscle tissue, and exenatide is not formulated or intended for this route of administration.
D. Intravenous: Exenatide is not administered intravenously. Intravenous injections are given directly into the bloodstream, and exenatide is not suitable for this route of administration.
Sign Up or Login to view all the 41 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

