SIMMONS U BSN PEDIATRICS
Total Questions : 35
Showing 25 questions, Sign in for moreA nurse is assessing a child who is postoperative following a tonsillectomy. Which of the following findings is a manifestation of hemorrhage?
Explanation
Drooling is a manifestation of hemorrhage after a tonsillectomy. Hemorrhage can result in the pooling of blood in the throat, leading to excessive drooling. This is an important sign to watch for in postoperative tonsillectomy patients, as it can indicate a potential complication that requires immediate medical attention. Other signs of hemorrhage may include increased heart rate, pallor, restlessness, and vomiting blood. If a child who has undergone a tonsillectomy exhibits any signs of hemorrhage, the nurse should notify the healthcare provider promptly.
A. Increased pain: Increased pain is a common and expected finding after a tonsillectomy. The surgical removal of tonsils creates wounds in the throat, which can cause discomfort and pain during the healing process. However, increased pain alone is not a specific manifestation of hemorrhage. Hemorrhage would be indicated by other signs, such as drooling, frequent swallowing, or vomiting blood.
B. Frequent swallowing: Frequent swallowing is also expected after a tonsillectomy due to postoperative throat irritation and saliva production. The throat may be sore and sensitive after the surgery, leading the child to swallow more frequently to manage the discomfort. While swallowing can increase after a tonsillectomy, it is not a specific manifestation of hemorrhage. Hemorrhage would be characterized by other signs, such as drooling, severe pain, or vomiting blood.
C. Poor fluid intake: Poor fluid intake is a common concern after a tonsillectomy due to postoperative pain and discomfort in the throat. The child may be reluctant to drink or eat initially because of their sore throat. However, poor fluid intake alone is not an indicative sign of hemorrhage. Hemorrhage would present with other symptoms, such as drooling, frequent swallowing, or vomiting blood.
D. Drooling: Drooling is a critical manifestation of hemorrhage after a tonsillectomy. If the child experiences bleeding at the surgical site, they may swallow the blood, leading to nausea and vomiting. The child may have difficulty swallowing the blood effectively, leading to drooling. In this context, drooling is a concerning sign that indicates active bleeding and requires immediate medical attention to prevent further complications.
A nurse is assessing an adolescent who experienced blunt trauma to the abdomen. Which of the following findings is the nurse's priority?
Explanation
The nurse's priority assessment finding in an adolescent who experienced blunt trauma to the abdomen is low blood pressure (hypotension). Hypotension could indicate significant internal bleeding or hemorrhage, which is a life-threatening condition and requires immediate attention. The decreased blood pressure may be a sign of shock, and prompt intervention is needed to stabilize the client's condition and prevent further deterioration.
While all the other findings (respiratory rate, abdominal pain, and heart rate) are important and should be assessed and monitored, blood pressure is the most critical in this situation due to its potential association with severe internal injuries and the risk of hypovolemic shock.
A nurse is teaching the mother of a 5-year-old child who has cystic fibrosis about pancreatic enzymes. The nurse should understand that further teaching is necessary when the mother states which of the following?
Explanation
In cystic fibrosis, the pancreas does not secrete enough digestive enzymes, leading to malabsorption of nutrients, especially fats. To help with digestion, pancreatic enzymes are prescribed to be taken with meals and snacks. These enzymes should be given just before or with each meal or snack to aid in the breakdown and absorption of nutrients.
A nurse is providing discharge teaching about nutrition to the parents of a child who has cystic fibrosis (CF). Which of the following responses by the parents indicates an understanding of the teaching?
Explanation
Cystic fibrosis (CF) is a genetic disorder that affects the production and function of certain glands, particularly those that produce mucus and sweat. One of the key aspects of CF management is addressing the pancreatic insufficiency that occurs in many individuals with CF. Due to the impairment of the pancreas, children with CF may have difficulty digesting food properly, especially fats. This can lead to malabsorption of nutrients, poor weight gain, and other nutritional deficiencies.
Pancreatic enzyme replacement therapy is a crucial part of CF management. Pancreatic enzymes are prescribed to help the child digest and absorb essential nutrients, especially fats. The enzymes are typically given with each meal and snack to aid in the breakdown and absorption of nutrients.
The other options are not correct:
A. "We will restrict the amount of salt in our child's food."
Sodium restriction is generally not a focus in CF management unless there are specific indications for it. CF patients may have increased salt losses in sweat, but dietary sodium restriction is not a primary aspect of their care.
B. "I will limit my child's fluid intake."
Fluid intake is important for children with CF to maintain hydration and prevent dehydration. There is no specific need to limit fluid intake unless there are individualized medical reasons for doing so.
C. "I will prepare low-fat meals with limited protein for my child."
Children with CF often require a high-calorie, high-protein diet to maintain adequate nutrition and growth. Restricting fat and protein intake is not typically recommended, as these nutrients are essential for a child's development and well-being. Instead, pancreatic enzymes are used to aid in the digestion and absorption of fats and other nutrients.
A nurse is caring for a child who has a sickle cell crisis and is hospitalized. Nursing interventions to prevent infection include administering:
Explanation
In a child with a sickle cell crisis who is hospitalized, preventing infections is crucial due to the increased risk of infections in this condition. Administering immunizations that the patient is scheduled for can help prevent certain infections.
Children with sickle cell disease are at a higher risk of bacterial infections, especially from encapsulated organisms like Streptococcus pneumoniae and Haemophilus influenzae. Vaccines can help protect against these pathogens and reduce the risk of serious infections.
Some of the recommended immunizations for children with sickle cell disease include:
Pneumococcal vaccine: This helps protect against infections caused by Streptococcus pneumoniae, which can cause severe respiratory and bloodstream infections.
Haemophilus influenzae type B (Hib) vaccine: This protects against infections caused by Haemophilus influenzae type B, which can lead to serious illnesses like pneumonia and meningitis.
Meningococcal vaccine: This protects against Neisseria meningitidis, which can cause meningitis and bloodstream infections.
Influenza vaccine: This annual vaccine helps protect against seasonal flu, which can be severe in children with sickle cell disease.
Administering these vaccines according to the recommended schedule helps provide protection against certain infections and can improve outcomes for children with sickle cell disease during hospitalization and beyond. The other options, Factor X, steroids, and PCA morphine, are not specific measures for preventing infections in a child with sickle cell crisis.
A nurse is caring for a child who has acute gastroenteritis but is able to tolerate oral fluids. The nurse should anticipate providing which of the following types of fluid?
Explanation
A. Broth: While broth can be a source of fluids, it does not contain the appropriate balance of electrolytes needed to rehydrate the body effectively. Gastroenteritis can cause significant fluid and electrolyte loss, so an oral rehydration solution (ORS) with the right proportions of salts and sugars is essential to replace these losses adequately.
B. Diluted apple juice: Diluted apple juice may not provide the proper electrolyte balance needed for rehydration in cases of gastroenteritis. In fact, apple juice is not recommended during episodes of acute gastroenteritis, as it can worsen diarrhea due to its high sugar content. This can lead to further dehydration and discomfort.
C. Oral rehydration solution (ORS): This is the correct answer. Oral rehydration solution is specifically designed to replace lost fluids and electrolytes in cases of gastroenteritis. It contains the right balance of salts and sugars to facilitate effective absorption in the intestines and help rehydrate the body. ORS is the recommended fluid for managing dehydration caused by gastroenteritis in children.
D. Water: While water is essential for hydration, it is not enough to effectively treat dehydration caused by gastroenteritis. Plain water does not contain the necessary electrolytes like sodium, potassium, and chloride, which are lost during episodes of diarrhea and vomiting. Giving water alone may not adequately rehydrate the child and could potentially worsen the dehydration.
A nurse is caring for a 6-month-old infant who has a prescription for clear liquids by mouth after a repair of an intussusception. Which of the following fluids should the nurse select for the infant?
Explanation
For a 6-month-old infant who has undergone the repair of an intussusception, the nurse should select an oral electrolyte solution. This solution is specifically designed to replace lost fluids and electrolytes due to vomiting or diarrhea, which is crucial in preventing dehydration in infants.
Options A, B, and C are not suitable choices for an infant in this situation:
A. Half-strength orange juice: Citrus juices, including orange juice, are not recommended for infants under 12 months old. They are acidic and may cause stomach upset or diarrhea.
B. Sterile water: Sterile water does not contain the necessary electrolytes, and offering plain water to an infant after surgery or during an illness can lead to electrolyte imbalances and further dehydration.
C. Half-strength infant formula: Diluting infant formula can lead to inadequate nutrition for the infant. The baby requires appropriate nutrition to support recovery after surgery, and diluting formula can be harmful.
D. An oral electrolyte solution is the best choice as it helps maintain proper hydration and electrolyte balance in the infant's body during the recovery period. If the infant tolerates the oral electrolyte solution well and is not at risk for aspiration, the healthcare provider may gradually advance the diet to include other clear liquids and then slowly reintroduce regular infant formula or breast milk as appropriate. The healthcare provider's instructions should be followed carefully to support the infant's recovery and ensure adequate nutrition.
A nurse is providing discharge instructions to the parent of a 10-year-old child following a cardiac catheterization. Which of the following instructions should the nurse include?
Explanation
Following a cardiac catheterization, the nurse should provide the parent with appropriate discharge instructions to ensure the child's proper recovery. The correct instruction to include is option B: "Give the child acetaminophen for discomfort."
Explanation:
Option A: Offering the child clear liquids for the first 24 hours is not a typical instruction following a cardiac catheterization. After the procedure, the child may be allowed to resume a regular diet, as tolerated, based on the healthcare provider's orders.
Option B: This is the correct instruction. After cardiac catheterization, the child may experience some discomfort at the insertion site or the area where the catheter was threaded through the blood vessels. Acetaminophen can be used to manage mild pain or discomfort.
Option C: Taking a tub bath for the first 3 days is not typically mentioned in discharge instructions after a cardiac catheterization. The nurse might advise the parent to avoid submerging the catheter insertion site in water for a specific period and instead use sponge baths until permitted by the healthcare provider.
Option D: Keeping the child home for 1 week is not a standard recommendation for a cardiac catheterization. The recovery period after a cardiac catheterization is usually shorter, and the child can often resume normal activities within a day or two, depending on the specific circumstances of the procedure and the child's condition.
The nurse should thoroughly review the specific discharge instructions provided by the healthcare provider and ensure the parent understands the care required at home, including any restrictions on activities or signs of potential complications that require immediate attention.
A child with severe anemia requires a unit of red blood cells (RBCs). The nurse explains to the child that the transfusion is necessary to:
Explanation
Severe anemia is a condition characterized by a significant decrease in the number of red blood cells or hemoglobin in the blood, leading to reduced oxygen-carrying capacity. This can result in fatigue, weakness, and shortness of breath in the affected individual.
A red blood cell transfusion is given to a child with severe anemia to increase the number of red blood cells and, consequently, the hemoglobin level in the blood. This helps improve oxygen delivery to tissues and organs, which can lead to increased energy levels and reduced fatigue.
Option A is incorrect because red blood cell transfusion is not given to help the body stop bleeding by forming a clot. Platelets are responsible for clot formation, not red blood cells.
Option B is incorrect because a red blood cell transfusion is not used to fight infections. White blood cells and the immune system are responsible for fighting infections.
Option D is incorrect because a red blood cell transfusion is not given to allow her parents to come to visit her. Transfusions are medical treatments to address specific medical conditions and are not related to visitation rights.
A parent tells a nurse that her toddler drinks a quart of milk a day and has a poor appetite for solid foods. The nurse should explain that the toddler is at risk for which of the following disorders?
Explanation
Consuming a large amount of milk, such as a quart a day, can lead to iron deficiency anemia in toddlers. Milk is a poor source of iron, and excessive milk intake can displace other iron-rich foods from the toddler's diet.
Iron deficiency anemia occurs when the body lacks sufficient iron to produce enough hemoglobin, which is essential for oxygen transport in the blood. Toddlers are particularly vulnerable to iron deficiency anemia because they have increased iron needs for growth and development.
Option A (Obesity) and option B (Diabetes mellitus) are not directly related to the toddler's milk consumption. Obesity may be a concern if the child consumes excessive calories overall, but it is not specifically associated with milk intake. Similarly, diabetes mellitus is not directly related to milk consumption.
Option D (Rickets) is caused by a deficiency of vitamin D, not iron. Rickets results in weakened and deformed bones, and it is usually associated with inadequate sunlight exposure and insufficient dietary vitamin D. While milk is often fortified with vitamin D, excessive milk intake can displace other vitamin D sources in the diet and contribute to an increased risk of rickets, but the primary concern with excessive milk intake is iron deficiency anemia.
A nurse is preparing to administer acetaminophen 10 mg/kg/dose to a child who weighs 28 lb. The amount available is acetaminophen 120 mg/5 mL. How many mL should the nurse administer? (Round the answer to the nearest tenth. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
To calculate the dose of acetaminophen for a child, the nurse needs to convert the child's weight from pounds to kilograms and then multiply it by the prescribed dose per kilogram. The formula is:
Weight in kg = Weight in lb / 2.2
Dose in mg = Weight in kg x Dose per kg
Dose in mL = Dose in mg / Concentration in mg/mL
Using the given information, the nurse can plug in the values and solve for the dose in mL:
Weight in kg = 28 / 2.2 = 12.73
Dose in mg = 12.73 x 10 = 127.3
Dose in mL = 127.3 / 120 x 5 = 5.3
Therefore, the nurse should administer 5.3 mL of acetaminophen to the child.
A nurse is admitting an infant who has severe dehydration from acute gastroenteritis. Which of the following findings should the nurse expect?
Explanation
Severe dehydration from acute gastroenteritis can lead to decreased blood volume and reduced tissue perfusion, which affects the capillary refill time. Capillary refill time is the time it takes for color to return to the nail bed after pressure is applied and then released. In a well-hydrated individual, the normal capillary refill time is less than 2 seconds. However, in severe dehydration, the capillary refill time can be prolonged, and it may take more than 2 seconds for color to return to the nail bed after pressure is released. A capillary refill time of 3 seconds or more is considered abnormal and indicates inadequate tissue perfusion.
The other options are not typical findings associated with severe dehydration from acute gastroenteritis:
A. A 13% weight loss is not a specific finding for severe dehydration and is a very high percentage for an infant.
B. A bulging anterior fontanel may be a sign of increased intracranial pressure, but it is not directly related to severe dehydration.
C. Bradypnea (slow breathing) is not a typical finding in severe dehydration; in fact, tachypnea (rapid breathing) is more commonly seen as the body tries to compensate for fluid loss.
A nurse is caring for an infant who has gastroesophageal reflux. The nurse should place the infant in which of the following positions following feedings?
Explanation
Infants with gastroesophageal reflux should be placed in an infant seat or an upright position after feedings to help prevent regurgitation and aspiration of stomach contents into the airway. Placing the infant in an upright position facilitates gravity-assisted movement of stomach contents down and away from the esophagus, reducing the likelihood of reflux. It is essential to ensure that the infant seat is appropriate for the child's age and size and that the infant is safely secured within it.
The other options are not recommended for infants with gastroesophageal reflux:
When caring for an infant with gastroesophageal reflux (GER), the nurse should place the infant in an infant seat or an upright position following feedings. Placing the infant in an upright position helps to reduce the risk of reflux and regurgitation. Gravity can assist in keeping the stomach contents from flowing back into the esophagus, reducing the potential for discomfort and reflux symptoms.
The other options are not recommended for an infant with GER:
A. Placing the infant in a prone position (lying on the stomach) after feedings can increase the risk of choking and aspiration. It is essential to avoid this position, especially after feeding, to reduce the risk of reflux and its complications.
B. Placing the infant on his left side is not the preferred position for GER management. While the left side is often recommended for sleeping to reduce the risk of sudden infant death syndrome (SIDS), it is not specifically indicated for GER management after feedings.
D. Placing the infant on his right side is also not the preferred position for GER management after feedings. The right side does not provide the benefits of an upright position in reducing the risk of reflux and regurgitation.
A nurse is caring for a child who has Kawasaki disease. Which of the following systems should the nurse monitor in response to this diagnosis?
Explanation
A. Gastrointestinal:
Kawasaki disease primarily affects blood vessels, and the gastrointestinal system is not the main target of this condition. While gastrointestinal symptoms can occur as part of the overall inflammatory response, such as abdominal pain, vomiting, or diarrhea, they are not the primary focus of concern in Kawasaki disease. The most critical system to monitor in Kawasaki disease is the cardiovascular system, specifically the coronary arteries.
B. Respiratory:
The respiratory system is not the primary system affected by Kawasaki disease. While respiratory symptoms can occur as part of the overall inflammatory response and fever associated with the disease, such as coughing or runny nose, they are not the main concern in Kawasaki disease. The primary system to monitor in this condition is the cardiovascular system, especially the coronary arteries.
C. Cardiovascular:
This is the correct answer. Kawasaki disease is primarily a vasculitis (inflammation of blood vessels) that affects various blood vessels, including the coronary arteries. The inflammation of the coronary arteries can lead to coronary artery aneurysms and other cardiac complications. Monitoring the cardiovascular system is essential to detect any signs of coronary artery involvement and ensure timely intervention to prevent potential long-term cardiac problems.
D. Integumentary:
The integumentary system (skin) is not the primary focus of Kawasaki disease. While some skin changes can occur during the acute phase of the disease, such as a rash or peeling skin on the hands and feet, these are not the primary concerns. Monitoring the cardiovascular system is critical in Kawasaki disease due to the risk of coronary artery inflammation and potential complications.
A nurse is obtaining vital signs from a 2-month-old infant. The infant's heart rate is 190/min and his temperature is 40° C (104° F). The father asks the nurse why the infant's heart is beating so fast. Which of the following responses by the nurse is appropriate?
Explanation
In this scenario, the infant has a heart rate of 190/min and a fever of 40°C (104°F). Fever in infants can cause an increase in heart rate, which is a normal physiological response to elevated body temperature. Fever is the body's way of responding to an infection or illness, and it triggers various physiological changes, including an increase in heart rate. This helps the body to circulate blood and deliver immune cells to fight off the infection.
The other options are not accurate or relevant to the infant's current condition:
A. "This is within the expected range for your baby." - A heart rate of 190/min is above the normal expected range for a 2-month-old infant, which is typically between 120 to 160 beats per minute. This response would not address the elevated heart rate and fever.
C. "As your baby begins to fall asleep, his heart rate will decrease." - While heart rate may decrease during sleep, it does not explain the elevated heart rate and fever observed in this situation.
D. "Your baby's heart is beating fast in an attempt to cool down his body." - While tachycardia (fast heart rate) can be associated with increased metabolic demands during fever, the main reason for the increased heart rate in this case is the fever itself, not the body's attempt to cool down. Fever is a response to infection or illness and can cause an increase in heart rate as part of the body's normal immune response.
A nurse is providing teaching to the parent of an infant who has gastroesophageal reflux. Which of the following statements by the parent indicates an understanding of the teaching?
Explanation
A. "I will keep my baby in an upright position after feedings."
Gastroesophageal reflux (GER) is a condition where the stomach contents flow back into the esophagus, which can cause spitting up or regurgitation in infants. Keeping the baby in an upright position after feedings can help reduce the likelihood of reflux episodes. By holding the baby in an upright position for about 30 minutes after feeding, gravity can aid in keeping the stomach contents from flowing back into the esophagus.
The other statements are incorrect or do not address the management of gastroesophageal reflux:
B. "My baby's formula can be thickened with oatmeal." - Thickening formula with oatmeal is not a standard recommendation for managing GER in infants. In some cases, thickening formulas may be recommended, but it should be done under the guidance of a healthcare provider.
C. "I should position my baby side-lying during sleep." A side-lying position is not recommended for sleep in infants, as it increases the risk of sudden infant death syndrome (SIDS). The safe sleep position for infants is on their back.
D. "I will have to feed my baby formula rather than breast milk." - The type of feeding (formula or breast milk) does not directly impact the occurrence of gastroesophageal reflux. Both breast milk and formula can cause reflux in some infants. It is essential to discuss feeding options with a healthcare provider to determine the best approach for the individual infant's needs.
A nurse is caring for a 2-month-old infant who is postoperative following surgical repair of a cleft lip. Which of the following actions should the nurse take?
Explanation
D. Offer the infant a pacifier.
After surgical repair of a cleft lip, the infant may experience discomfort and agitation. Offering a pacifier can be beneficial for soothing the infant and providing non-nutritive sucking, which can help promote comfort and reduce the need for oral feeding during the immediate postoperative period. However, the pacifier should be offered carefully to avoid putting pressure on the surgical site.
The other options are not appropriate for an infant postoperative following cleft lip repair:
A. Encourage the parents to rock the infant: Rocking can be soothing, but it might not be sufficient for managing the infant's pain and postoperative needs.
B. Administer ibuprofen as needed for pain: Pain management in infants, especially after surgery, requires careful consideration and proper dosing based on the infant's weight and age. Medication administration should be done according to the healthcare provider's prescription and guidelines.
C. Position the infant on her abdomen: After cleft lip repair surgery, it is generally recommended to position the infant on her back to prevent any pressure on the surgical site and to minimize the risk of infection. Placing the infant on her abdomen may interfere with the healing process and increase the risk of complications.
A nurse is teaching the mother of a child who has cystic fibrosis and has a prescription for pancreatic enzymes three times per day. Which of the following statements indicates that the mother understands the teaching?
Explanation
D. "My child will take the enzymes to help digest the fat in foods."
Cystic fibrosis (CF) affects the exocrine glands, leading to thick and sticky mucus production, which can block the pancreatic ducts. As a result, children with CF have difficulty digesting fats and absorbing fat-soluble vitamins. Pancreatic enzyme replacement therapy (PERT) is prescribed to help improve fat digestion and nutrient absorption. These enzymes are taken with meals and snacks to aid in the breakdown of fats.
The other options are incorrect:
A. "My child will take the enzymes following meals." - This is the correct timing for taking pancreatic enzymes. The enzymes should be taken with meals and snacks, not following meals.
B. "My child will take the enzymes to improve her metabolism." - The purpose of taking pancreatic enzymes is not related to improving metabolism but to assist in fat digestion and nutrient absorption.
C. "My child will take the enzymes 2 hours before meals." - Taking pancreatic enzymes 2 hours before meals is not the recommended timing. They should be taken with meals and snacks to aid in fat digestion while eating.
A nurse is caring for a group of adolescents. Which of the following findings should be reported to the provider immediately?
Explanation
D. A client's blood pressure changes from 112/60 mm Hg to 90/54 mm Hg when standing.
A significant drop in blood pressure when changing positions from lying to standing may indicate orthostatic hypotension, which can be a sign of dehydration, blood loss, or other underlying medical issues. This can be a cause for concern, especially if the client is an adolescent, as it may lead to decreased perfusion of vital organs and may require immediate medical attention.
The other options are as follows:
A. A client who has a burn injury to an estimated 5% of his leg and is crying - While it's essential to assess and address the client's pain and comfort, this finding does not indicate an immediate need for medical attention. Pain management and wound care can be addressed based on the severity of the burn and the client's pain level.
B. A client who has an ankle fracture reports a pain level increase from 3 to 5 after initial ambulation - This finding is concerning, and the nurse should notify the provider to reassess pain management and evaluate for potential complications related to the fracture. However, it may not require immediate medical attention unless there are signs of severe pain or complications.
C. A client who is 1 day postoperative and has a temperature of 37.5° C (99.5° F) - A slight increase in temperature in the immediate postoperative period may not be unusual and can be attributed to the normal inflammatory response after surgery. The nurse should continue monitoring the client's temperature and report any further changes or additional signs of infection or complications to the provider.
Overall, while all findings should be addressed and managed appropriately, the significant drop in blood pressure (option D) should be reported immediately due to the potential implications for the client's overall health and well-being.
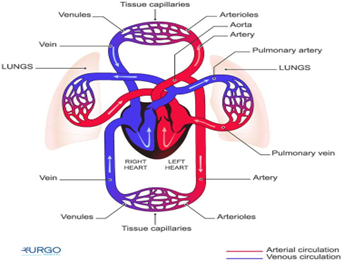
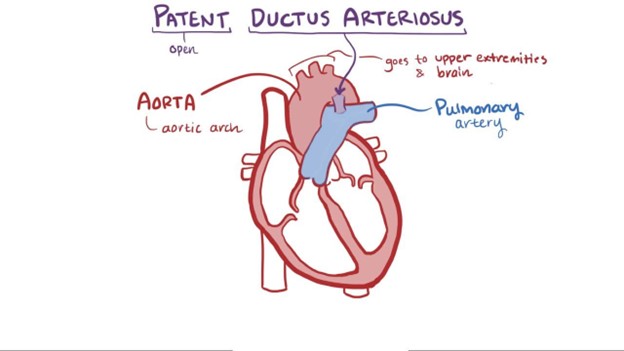
A nurse is caring for an infant who has a congenital heart defect. Which of the following defects is associated with increased pulmonary blood flow?
Explanation
A patent ductus arteriosus (PDA) is a congenital heart defect associated with increased pulmonary blood flow. In normal fetal circulation, the ductus arteriosus allows blood to bypass the lungs since the baby receives oxygen from the mother's placenta. After birth, the ductus arteriosus should close, redirecting blood flow to the lungs for oxygenation. However, in some infants with PDA, the ductus arteriosus remains open, causing an abnormal connection between the aorta and the pulmonary artery. As a result, oxygenated blood from the aorta flows back into the pulmonary artery, increasing the workload on the lungs.
The other options are as follows:
A. Coarctation of the aorta - Coarctation of the aorta is a narrowing of the aorta, which obstructs blood flow and leads to increased blood pressure in the upper body and reduced blood flow to the lower body.
C. Tetralogy of Fallot - Tetralogy of Fallot is a combination of four heart defects that results in decreased pulmonary blood flow due to a ventricular septal defect (VSD), overriding aorta, pulmonary stenosis, and right ventricular hypertrophy.
D. Tricuspid atresia - Tricuspid atresia is a congenital heart defect where the tricuspid valve does not develop correctly, resulting in an absent or abnormal tricuspid valve. This defect prevents blood flow from the right atrium to the right ventricle and, therefore, reduces pulmonary blood flow.
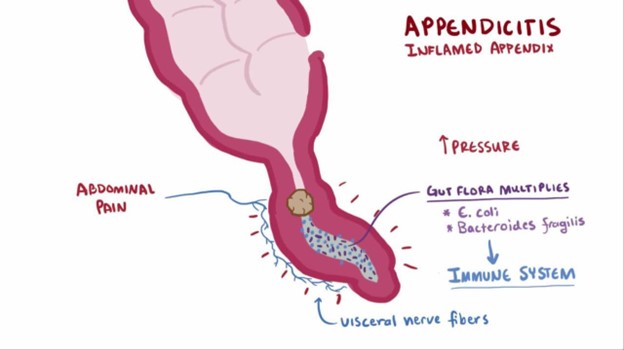
A nurse is caring for a child who has suspected appendicitis. Which of the following provider prescriptions should the nurse clarify?
Explanation
The nurse should clarify the prescription to administer sodium biphosphate/sodium phosphate because it is a laxative and is contraindicated in a child with suspected appendicitis. The use of laxatives or enemas can potentially worsen the condition by increasing the risk of perforation or rupture of the inflamed appendix.
A. Monitoring oral temperature every 4 hours is important to assess for signs of infection or worsening condition.
C. Maintaining NPO status is essential to avoid stimulating the digestive system and to prepare for possible surgery.
D. Medicating the client for pain every 4 hours as needed is appropriate to manage pain and provide comfort while the child awaits further evaluation or treatment.
Remember, it's crucial to avoid the use of laxatives, enemas, or any other interventions that can potentially aggravate the inflamed appendix in a child with suspected appendicitis.
A nurse in an emergency department is assessing an infant who is dehydrated. Which of the following findings should the nurse expect?
Explanation
The nurse should expect to find irritability in an infant who is dehydrated. Dehydration in infants can lead to changes in behavior and irritability due to the imbalance in fluid and electrolytes. Other common signs of dehydration in infants may include:
Poor skin turgor (skin tenting)
Sunken fontanelles (soft spots on the baby's head)
Dry mucous membranes (dry mouth and tongue)
Decreased urine output or concentrated urine
Rapid heart rate (tachycardia)
Increased respiratory rate
Sunken eyes
Decreased tears when crying
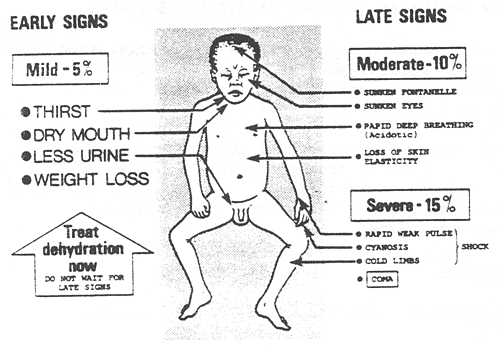
B. Tetany is a condition characterized by involuntary muscle contractions and is more commonly associated with hypocalcemia (low calcium levels) rather than dehydration.
C. A slow, bounding pulse is not typically associated with dehydration. Dehydration often leads to a rapid heart rate (tachycardia) as the body attempts to compensate for the loss of fluid.
D. Decreased temperature is not a typical finding in dehydration. Dehydration can lead to fever in some cases due to an underlying infection, but it does not cause a decrease in body temperature on its own.
A nurse in an emergency department is caring for an infant who has a 2-day history of vomiting and an elevated temperature. Which of the following should the nurse recognize as the most reliable indicator of fluid loss?
Explanation
In an infant with a history of vomiting and fever, body weight is the most reliable indicator of fluid loss. Monitoring the infant's weight over time can help assess the degree of dehydration and guide the appropriate fluid replacement therapy. A significant decrease in body weight suggests significant fluid loss.
Option A: Skin integrity is important to assess for signs of dehydration, but it is not as reliable as body weight in determining the extent of fluid loss.
Option B: Respiratory rate can be affected by various factors and is not a direct indicator of fluid loss.
Option D: Blood pressure is not the most reliable indicator of fluid loss in an infant with dehydration. In severe cases of dehydration, blood pressure can drop, but it is not as sensitive as body weight in assessing the extent of fluid loss.
A nurse is assessing a child who is in a sickle cell crisis. Which of the following findings should the nurse expect?
Explanation
During a sickle cell crisis, the child experiences severe pain due to the sickled red blood cells blocking blood flow in the vessels, leading to tissue ischemia and infarction. Pain is the hallmark symptom of sickle cell crisis and can occur in various parts of the body, such as the abdomen, chest, back, joints, and extremities.
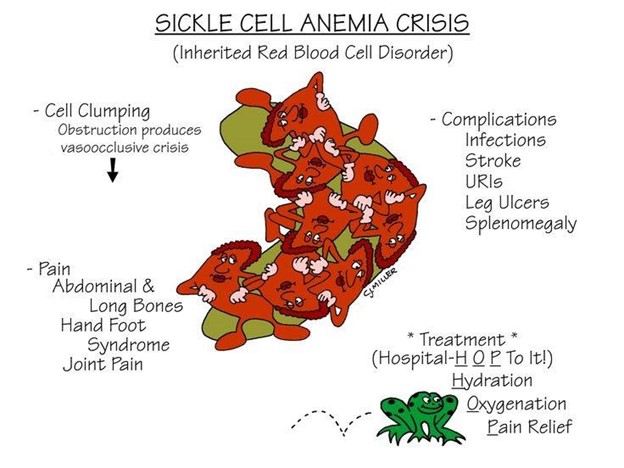
A. Constipation is not a common symptom of sickle cell crisis. It may be associated with other conditions but is not directly related to sickle cell crisis.
C. High fever is not a typical finding in sickle cell crisis. Fever may occur due to infections, which individuals with sickle cell disease are at increased risk of developing, but it is not a direct symptom of the crisis itself.
D. Bradycardia (slow heart rate) is not commonly associated with sickle cell crisis. Tachycardia (rapid heart rate) may occur in response to pain, but bradycardia is not a typical finding.
A nurse receives a call from a parent of a child who has von Willebrand disease and has had a nosebleed. Which of the following instructions should the nurse give to the parent?
Explanation
For a child with von Willebrand disease experiencing a nosebleed, the nurse should instruct the parent to have the child sit with their head tilted forward slightly (not backward) to prevent blood from flowing down the throat. Applying direct pressure to the nostrils with fingers or using a clean cloth for about 10 minutes will help stop the bleeding.
Option B (applying ice at the base of the nose) is not recommended because ice can cause vasoconstriction, potentially prolonging bleeding in individuals with bleeding disorders.
Option C (placing the child in a supine position with a pillow under the back) is also not recommended, as this can lead to blood flowing down the throat, increasing the risk of aspiration.
Option D (placing the child in a sitting position with her head tilted back) should be avoided as it can lead to blood flowing into the throat and potentially being swallowed or aspirated. This position is generally discouraged for nosebleeds.
Sign Up or Login to view all the 35 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

