South Tampa University, Pharmocology exam 2
Total Questions : 34
Showing 25 questions, Sign in for moreA client has the feeling of having “chest tightness” while experiencing “cold-like” symptoms. Her cough is nonproductive. Her physician prescribed guaifenesin (Mucinex) to help with secretions.
When teaching about this medication, what should the nurse instruct? (Select all that apply)
Explanation
A. “Drink extra water while taking this medication.”
This is correct. Guaifenesin is an expectorant that works by thinning and loosening mucus in the airways. Drinking extra water helps to enhance its effectiveness by keeping the patient well-hydrated.
B. “Monitor urine output closely.”
Monitoring urine output is not typically necessary with guaifenesin. It does not have a diuretic effect, and excessive monitoring of urine output may not be relevant in this context.
C. “Take it with an oral antihistamine for better effectiveness.”
Guaifenesin is often used in combination with other medications, but taking it with an oral antihistamine is not a standard recommendation. The combination should be based on the specific guidance of the healthcare provider.
D. “Avoid driving or using heavy machinery while on this medication.”
Guaifenesin does not typically cause sedation or impairment, so there is generally no need to avoid driving or using heavy machinery. This instruction may not be necessary for this medication.
A client is receiving Dextromethorphan (Robitussin). The nurse knows the drug is exerting its therapeutic effects with which client report?
Explanation
. Decreased coughing:
Dextromethorphan is primarily used as an antitussive, meaning it helps reduce coughing. It acts on the cough center in the brain to suppress the urge to cough.
B. Relief of nasal congestion:
Dextromethorphan is not typically used for relieving nasal congestion. Decongestants, such as pseudoephedrine, are more commonly used for this purpose.
C. Thinning of secretions:
Dextromethorphan does not have a direct effect on thinning secretions. Expectorants, like guaifenesin, are often used for this purpose.
D. Bronchodilation:
Dextromethorphan is not known for its bronchodilator effects. Bronchodilators, such as albuterol, are used for widening the airways in conditions like asthma or chronic obstructive pulmonary disease (COPD).
A patient being treated for cancer is receiving medication for palliation. The nurse understands that palliative therapy is used to
Explanation
A. Decrease viral load:
This is a goal typically associated with antiviral medications, which aim to reduce the amount of virus in the body, commonly seen in the treatment of viral infections like HIV.
B. Kill tumor cells:
This is the goal of many cancer treatments, such as chemotherapy or radiation therapy. These treatments aim to destroy or inhibit the growth of cancer cells.
C. Increase body defenses:
This is a goal often associated with immunotherapy, which aims to enhance the body's immune system to better recognize and attack cancer cells or other pathogens.
D. Relieve symptoms:
This is the primary goal of palliative therapy, which focuses on managing and alleviating symptoms, improving the patient's comfort and quality of life, especially in the context of serious or life-limiting illnesses like cancer.
The oncology RN knows that the most important reason that patients who are undergoing chemotherapy have either intravenous ports, central lines, or peripherally inserted central line is:
Explanation
. because many chemotherapy patients require blood transfusions:
While some chemotherapy patients may require blood transfusions, this is not the primary reason for using intravenous ports, central lines, or peripherally inserted central lines.
B. because many chemotherapy patients need long-term intravenous access:
Long-term intravenous access may be needed for some chemotherapy patients, but the critical consideration is the vesicant nature of many chemotherapy drugs.
C. because chemotherapy patients have frequent blood draws orders:
Frequent blood draws may be necessary for monitoring purposes, but the primary reason for using specialized lines in chemotherapy patients is to administer the drugs safely.
D. because many chemotherapeutic drugs are vesicants:
The primary reason for using intravenous ports, central lines, or peripherally inserted central lines in chemotherapy patients is to administer chemotherapy drugs directly into large veins. Many chemotherapeutic drugs are vesicants, meaning they can cause severe damage to tissues if they leak into the surrounding areas. These specialized lines allow for the safe and controlled administration of chemotherapy drugs, reducing the risk of extravasation (leakage into surrounding tissues).
A client is being discharged after receiving IV chemotherapy for cancer. Which statement indicates a need for additional teaching?
Explanation
A. “I will not need to know how to check my body temperature.”:
This statement is incorrect. Monitoring body temperature is important for patients receiving chemotherapy because a compromised immune system increases the risk of infection. Fever can be an early sign of infection, and patients are often instructed to monitor their temperature regularly.
B. “Chemotherapy is excreted in my bodily fluids.”:
This statement is correct. Chemotherapy drugs can be excreted in various bodily fluids, such as urine, sweat, and saliva. Patients are advised to take precautions to avoid exposing others to these bodily fluids during and shortly after chemotherapy.
C. “My spouse will wear gloves when emptying my urinal.”:
This statement is correct. To reduce the risk of exposure to chemotherapy drugs in urine, it is advisable for caregivers, such as spouses, to wear gloves when handling bodily fluids.
D. “The chemotherapy will remain in my body for 2-3 days.”:
This statement is correct. The duration during which chemotherapy remains in the body can vary depending on the specific drugs administered. Patients are typically provided with guidelines on how long they need to take precautions to minimize exposure to others.
A client is scheduled to receive chemotherapy drugs that will cause myelosuppression. Which action by the nurse will be most important?
Explanation
A. Evaluate gastrointestinal function:
While gastrointestinal function is important to assess for side effects of chemotherapy, such as nausea and vomiting, monitoring for potential infection (fever) takes precedence in the context of myelosuppressive chemotherapy.
B. Assess for evidence of cardiac compromise:
Myelosuppression primarily affects the hematopoietic system, and assessing for cardiac compromise is not the priority in this situation.
C. Question about changes in taste or smell:
Changes in taste or smell are common side effects of chemotherapy, but they are not as critical as monitoring for signs of infection, especially fever.
D. Monitor for temperature changes:
Myelosuppression refers to the suppression of the bone marrow's ability to produce blood cells, including white blood cells. Neutropenia, a common side effect of myelosuppressive chemotherapy, increases the risk of infection. Fever may be the only early sign of infection in immunocompromised patients, and it can progress rapidly. Therefore, monitoring for temperature changes is crucial to identify and address potential infections promptly.
Mrs. Miller is a 34 year-old who just successfully completed chemotherapy for breast cancer. Which of the following should the RN include in her plan of care?
Explanation
A. Avoid elevated altitudes of greater than 2,000 feet (if possible) and air travel for 2-4 weeks (depending on the oncologist’s advice):
Altitude and air travel restrictions are not common recommendations after completing chemotherapy.
B. Avoid foods high in purine for 30-90 days (depending on the oncologist’s advice):
Restrictions on foods high in purine are not typically associated with post-chemotherapy care.
C. Avoid sun exposure for 60-90 days following chemotherapy (depending on oncologist’s advice):
Chemotherapy can make the skin more sensitive to sunlight. Advising the patient to avoid sun exposure or take precautions such as using sunscreen can help prevent skin damage during this period.
D. Have a solid plan for contraception for 3 months to 2 years (depending on the oncologist’s advice):
Contraception considerations may be important, but the timeframe mentioned is not a standard recommendation following chemotherapy completion. The need for contraception may vary depending on the patient's overall health, reproductive goals, and specific chemotherapy drugs received. This decision is usually discussed with the healthcare provider on an individual basis.
Ms. Samuels is scheduled to receive chemotherapy this afternoon at 1400. Her prescribed chemotherapy treatment causes nausea and vomiting as a side effect. How should the RN approach treating this patient for this side effect?
Explanation
Explanation:
A. Administer phenergan (Promethazine) 12.5 mg IVP at the first complaint of nausea.
This option suggests waiting until the patient complains of nausea before administering the antiemetic. It is not a proactive approach and may not effectively prevent nausea associated with chemotherapy.
B. Administer ondansetron (Zofran) 4mg IV Push after Ms. Samuels complains of nausea.
Similar to option A, this choice involves waiting for the patient to experience nausea before administering the medication. Again, it is not a proactive strategy for preventing chemotherapy-induced nausea and vomiting.
C. Administer ondansetron (Zofran) 4mg IV push sometime between 1300-1330.
This option is the most appropriate among the given choices. It suggests administering the antiemetic (ondansetron) before the scheduled chemotherapy session. Ondansetron is commonly used as a prophylactic measure to prevent nausea and vomiting associated with chemotherapy.
D. Administer phenergan (Promethazine) 25 mg PO at 1345.
This choice involves administering the antiemetic (phenergan) orally just 15 minutes before the scheduled chemotherapy session. While it is better than waiting for symptoms to appear, oral medications may take some time to be absorbed, and it might not provide as rapid relief as an intravenous (IV) medication.
Ms. Williams is a 72 year-old female who is scheduled to begin chemotherapy within the next two weeks. The chemotherapeutic agent that he oncologist has prescribed causes alopecia in almost 100% of all cases. Ms. Williams has always been very particular about her hair and is concerned about this side effect. Which statement by the oncology clinic RN, as it relates to this side effect, is most appropriate?
Explanation
A. “Do you think you and your daughter may have time to go shopping for a wig between now and the time you begin treatment?”
This option recognizes the patient's concern about hair loss and offers a practical suggestion for preparing for it. It shows empathy and support by involving a family member in the process of coping with potential hair loss.
B. “Most patients just wear a hat or turban and just let their hair grow back following treatment.”
This statement provides an alternative approach to dealing with hair loss by suggesting the use of head coverings like hats or turbans. It emphasizes the temporary nature of the hair loss during treatment.
C. “I would be less concerned about cosmetic changes that you may experience and be more concerned about treating the cancer.”
This option encourages the patient to prioritize the cancer treatment over cosmetic concerns, emphasizing the importance of addressing the underlying health issue. It offers a supportive and empathetic perspective.
D. “Just pray about it.”
This option suggests relying on prayer as a sole coping mechanism, which may not address the patient's emotional concerns effectively. While spirituality and prayer can be important for some individuals, it's essential to provide practical and emotional support as well.
E. “Keep a positive attitude. Just wait until your treatment begins to before you become concerned
about losing your hair, after all, you may not experience hair loss.”
This statement encourages a positive attitude and suggests delaying concerns about hair loss until after treatment has begun. While maintaining a positive outlook is beneficial, it's also important to acknowledge and address the patient's current concerns and provide information about potential side effects.
Mr. Johnson is a 56 year-old male who is being treated for cancer of the bladder. He is receiving chemotherapy and the RN noticed that the oncologist has instructed the patient to drink 2-3 liters of water per day. In addition to staying hydrated, what is another rationale for encouraging fluid intake for this client?
Explanation
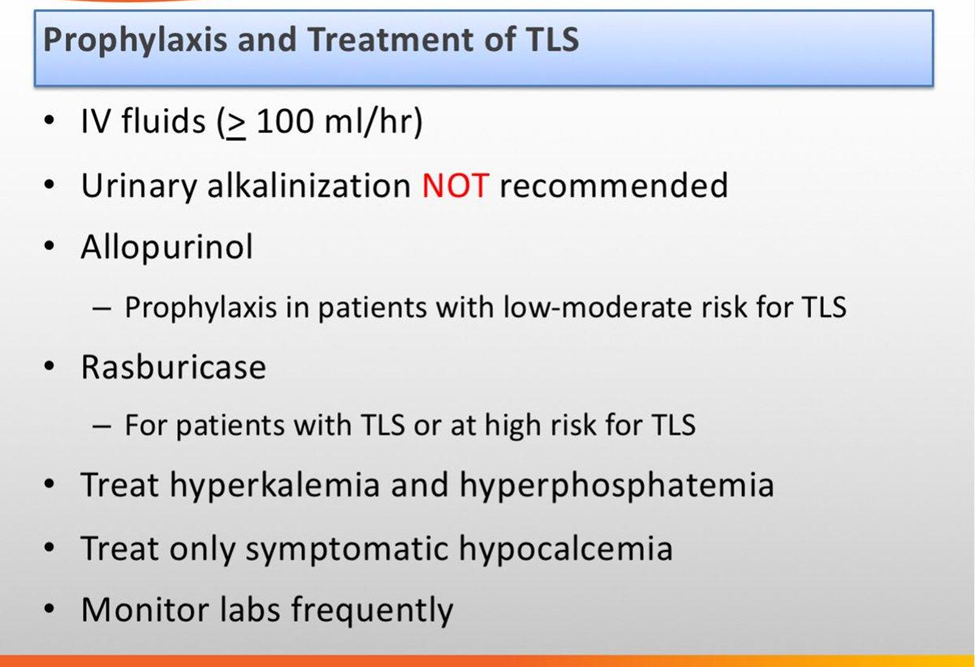
A. To help prevent Tumor Lysis Syndrome.
Encouraging fluid intake is crucial for patients undergoing chemotherapy, especially when there's a risk of Tumor Lysis Syndrome (TLS). TLS is a potentially serious complication that can occur when cancer cells release their contents into the bloodstream, leading to metabolic imbalances. Adequate hydration helps prevent the concentration of these released substances and reduces the risk of TLS.
B. Staying hydrated decreases oral dryness that the patient may exhibit as a result of chemotherapy.
While hydration is generally important for overall well-being, oral dryness is not typically a direct consequence of bladder cancer chemotherapy. It might be a side effect of certain medications, but the primary concern in this case is likely related to preventing TLS.
C. To help prevent new onset diabetes mellitus.
The rationale for fluid intake in the context of bladder cancer chemotherapy is not typically related to preventing new onset diabetes mellitus. The primary focus is usually on managing potential side effects of chemotherapy and promoting overall health.
D. Because it is better to encourage water Vs. carbonated beverages.
While encouraging water over carbonated beverages is generally a healthy choice, the primary rationale for increased fluid intake in the context of bladder cancer chemotherapy is more specific and related to preventing Tumor Lysis Syndrome.
Ms. Smith, a 48 year-old female, is being treated for cancer with chemotherapy with medications that routinely cause myelosuppression. Which lab values would the RN need to especially monitor?
Explanation
A. Cardiac Enzymes
Cardiac enzymes are markers used to assess heart health and are not directly related to myelosuppression caused by chemotherapy. Monitoring cardiac enzymes is important for assessing heart function but is not the primary concern in the context of myelosuppression.
B. Complete Blood Count with differential
This is the correct choice. The complete blood count (CBC) with differential provides information about the levels of red blood cells, white blood cells, and platelets. Since myelosuppression affects blood cell production, monitoring the CBC with differential is crucial to detect and manage any abnormalities in these cell counts.
C. Chemistry Profile
A chemistry profile typically includes measurements of electrolytes, kidney function, and other metabolic parameters. While monitoring overall health is important, the specific concern with myelosuppression and chemotherapy is related to blood cell counts. Therefore, a complete blood count (CBC) is more directly relevant in this context than a chemistry profile.
D. Liver Function Tests
Liver function tests assess the health of the liver and are not directly related to myelosuppression caused by chemotherapy. These tests are important in certain situations, but they do not provide information about blood cell counts, which are the primary concern when dealing with myelosuppression.
Many patients who are undergoing chemotherapy treatment require both invasive and noninvasive tests to be conducted to rule out, or monitor, organ toxicities. Please select which routine tests are considered noninvasive: (Select all that apply)
Explanation
A. Chest X-rays
Chest X-rays are imaging tests that provide detailed pictures of the inside of the chest, including the heart, lungs, and other structures. They are noninvasive as they do not involve any penetration or insertion into the body.
B. Echocardiogram
An echocardiogram is a noninvasive test that uses sound waves to create images of the heart. It provides information about the structure and function of the heart without the need for invasive procedures.
C. Pulmonary function tests
Pulmonary function tests (PFTs) are noninvasive tests that assess the function of the lungs. They include various breathing exercises and measurements to evaluate lung capacity and respiratory function.
D. Cardiac catheterization
Cardiac catheterization is an invasive procedure that involves the insertion of a catheter into the heart. It is not considered noninvasive.

Many patients who are undergoing chemotherapy treatment require both invasive and noninvasive tests to be conducted to rule out, or monitor, organ toxicities. Please select which routine tests are considered noninvasive: (Select all that apply)
Explanation
A. Remove the intravenous catheter.
While removing the intravenous catheter is an important step, the immediate priority in cases of extravasation is to stop the infusion to prevent further leakage into the surrounding tissues. After stopping the infusion, the catheter can be carefully removed.
B. Pack the intravenous site with ice.
Cold compresses or ice packs are sometimes used in the management of certain types of extravasation to help reduce local swelling and vasoconstriction. However, the immediate priority is to stop the infusion (Choice C). After that, specific interventions, such as warm or cold compresses, may be employed based on the specific chemotherapy agent involved.
C. Stop the intravenous infusion.
This is the correct answer. Stopping the infusion is the first and most immediate action to prevent further leakage of the chemotherapy drug into the surrounding tissues, reducing the risk of tissue damage and adverse effects.
D. Attempt to aspirate residual medication from the patient’s vein.
While aspirating residual medication may be part of the overall management of extravasation, it is not the first action. The priority is to stop the infusion to prevent further damage. After stopping the infusion, the nurse may assess the situation and determine whether aspirating residual medication is appropriate.
Which antitumor drug has a dual role of being an antibiotic?
Explanation
Choice A rationale: Incorrect. Methotrexate is a chemotherapy drug and an immunosuppressant but not an antibiotic. It inhibits the metabolism of folic acid, which is necessary for cell replication, but it does not have antibiotic properties.
Choice B rationale: Incorrect. Antiestrogens are a class of drugs used to treat hormone-sensitive cancers like breast cancer by blocking the effects of estrogen. They are not antibiotics and do not have antimicrobial properties.
Choice C rationale: Incorrect. Corticosteroids are used in cancer treatment primarily to reduce inflammation and manage side effects of chemotherapy, such as nausea and allergic reactions. They have immunosuppressive properties but are not antibiotics.
Choice D rationale: Correct. Doxorubicin (Doxil) is an antitumor drug that also has antibiotic properties. It belongs to the anthracycline class of chemotherapy drugs and works by intercalating DNA, disrupting the replication and transcription processes, leading to cell death. Doxorubicin was originally derived from the bacterium Streptomyces peucetius, which imparts its antibiotic properties.
The nurse evaluates a nursing student’s understanding of chemotherapy. When the nurse asks, “Which factor would be a major obstacle to successful chemotherapy?” What is the student’s best response?
Explanation
A. "The client’s degree of nausea."
The client's degree of nausea is a side effect of chemotherapy, but it is not a major obstacle to successful chemotherapy in the broader sense. Nausea can often be managed with antiemetic medications, and it is generally considered a manageable aspect of chemotherapy care.
B. "The patient’s reluctance about the doses administered."
Patient compliance and acceptance of the prescribed treatment are important factors in the success of chemotherapy. However, while patient reluctance can be a challenge, it is not considered a major obstacle to chemotherapy as there are strategies and interventions to address issues related to patient understanding, fears, or concerns.
C. "The toxicity of anticancer drugs to normal tissues."
This is the correct answer. The toxicity of anticancer drugs to normal tissues is a major obstacle in chemotherapy. While the drugs aim to kill rapidly dividing cancer cells, they can also affect healthy cells, leading to side effects and complications. Striking a balance between effective cancer treatment and minimizing harm to normal tissues is a key challenge in chemotherapy.
D. "The difficulty of maintaining venous access."
Maintaining venous access can be a logistical challenge in chemotherapy, but it is not considered a major obstacle to successful treatment. While it is important for delivering chemotherapy drugs, there are various methods and technologies to address issues related to venous access, such as the use of central venous catheters or ports.
Which medication is considered a “rescue inhaler”?
Explanation
A. Glucocorticoid
Glucocorticoids are anti-inflammatory medications commonly used as long-term control medications in asthma management. They are not typically considered rescue inhalers. They work gradually over time to reduce inflammation and are not suitable for immediate relief during an acute asthma attack.
B. Mast cell stabilizer
Mast cell stabilizers are anti-inflammatory medications that work by preventing the release of inflammatory substances from mast cells. They are used as maintenance therapy to prevent asthma symptoms but are not rescue inhalers. They do not provide quick relief during acute episodes.
C. Mucolytic agent
Mucolytic agents are medications that help thin and loosen mucus in the airways. While they may be used to improve respiratory symptoms, they are not considered rescue inhalers. They do not provide rapid bronchodilation and are typically used for different purposes, such as addressing mucus production and clearance.
D. Short-acting beta 2 agonist
This is the correct answer. Short-acting beta 2 agonists (SABAs) are bronchodilators that provide quick relief during acute bronchoconstriction. They act by relaxing the smooth muscles in the airways, allowing for rapid dilation and improved airflow. SABAs are commonly used as rescue inhalers to alleviate symptoms during asthma attacks or sudden exacerbations.
A home care nurse is visiting a client with asthma who suddenly experiences an acute asthma attack. Which drug should the nurse prepare to administer?
Explanation
A. Tiotropium bromide (Spiriva)
Tiotropium bromide is a long-acting anticholinergic bronchodilator used for maintenance therapy in conditions like chronic obstructive pulmonary disease (COPD). It is not indicated for the immediate relief of acute asthma symptoms.
B. Montelukast (Singulair)
Montelukast is a leukotriene receptor antagonist used for maintenance therapy in asthma. It is not a rescue medication and does not provide immediate relief during an acute asthma attack.
C. Albuterol (Proventil)
In the case of an acute asthma attack, the nurse should prepare to administer a short-acting bronchodilator. Albuterol (Proventil) is a short-acting beta-agonist bronchodilator that provides rapid relief of bronchoconstriction and acute symptoms during an asthma attack.
D. Acetylcysteine (Mucomyst)
Acetylcysteine is a mucolytic agent used to help loosen and thin mucus in the airways. It is not indicated for the immediate relief of bronchoconstriction during an acute asthma attack.
A client will be using an albuterol (Proventil) metered-dose inhaler to treat asthma symptoms. The client asks the nurse about the difference between the effect of inhaled albuterol (Proventil) versus an oral form of albuterol.
How should the nurse best explain the difference between inhaled and oral albuterol?
Explanation
A. The inhaled form may cause more side effects than the oral form.
The route of administration does not necessarily determine the likelihood of side effects. Both inhaled and oral forms of albuterol can cause side effects, but they may vary in nature.
B. The inhaled form requires an increased dose.
The dose of albuterol may differ between inhaled and oral forms, but it is not accurate to say that the inhaled form always requires an increased dose. The choice of dosage depends on factors such as the severity of symptoms and the patient's response to treatment.
C. The inhaled form will not lead to increased doses.
The need for increased doses depends on the individual patient's response and the severity of symptoms. In some cases, increased doses may be necessary, especially during acute exacerbations.
D. The inhaled form has a more immediate onset of action.
Inhaled albuterol has a quicker onset of action compared to the oral form. When inhaled, the medication reaches the airways directly, leading to rapid bronchodilation and relief of symptoms. This is especially important during acute bronchoconstriction or asthma exacerbations when prompt relief is needed.
The nurse is caring for a patient diagnosed with COPD who has been prescribed tiotropium (Spiriva). Which statement will the nurse include in the education?
Explanation
A. Tiotropium (Spiriva) works by relaxing and dilating the bronchioles
Tiotropium is an anticholinergic bronchodilator used in the management of chronic obstructive pulmonary disease (COPD). It works by blocking the action of acetylcholine, a neurotransmitter, leading to relaxation and dilation of the bronchioles, which helps improve airflow in the lungs.
B. If you experience dry mouth, stop taking the medication immediately
Dry mouth is a common side effect of tiotropium but is not a reason to stop taking the medication. The nurse may advise the patient to manage dry mouth with measures such as increased water intake or using sugar-free gum.
C. Use tiotropium (Spiriva) as needed for sudden breathing problems
Tiotropium is typically used as a maintenance medication for long-term control of COPD symptoms, not as a rescue medication for sudden breathing problems. Short-acting bronchodilators are often prescribed for acute symptom relief.
D. Remove the capsules from the packaging and place in your 7-day med box
Tiotropium is available in a dry powder inhalation capsule, and it should be used with the inhalation device provided. Removing the capsules from the packaging and placing them in a weekly medication box is not the correct method for administration.
Which statement is accurate regarding methylxanthine (Theophylline)?
Explanation
A. Is a first-line drug currently to treat COPD
Methylxanthines are not considered first-line drugs for the treatment of COPD. They are often reserved for use when other bronchodilators (such as beta-agonists and anticholinergics) are not effective or well-tolerated.
B. Is considered toxic if theophylline levels are between 5-15 mcg/mL
The therapeutic range for theophylline levels is generally considered to be lower, typically 5-15 mcg/mL. However, toxicity can occur at levels above the therapeutic range, and symptoms can vary between individuals.
C. Has fewer major side effects than beta-agonists and glucocorticoids
Methylxanthines can have side effects, and their use is associated with a risk of toxicity. Beta-agonists and glucocorticoids are often preferred as first-line treatments due to their efficacy and a more favorable side effect profile.
D. Has the potential to cause central nervous system side effects, especially if levels are elevated
Methylxanthines, such as theophylline, are bronchodilators that can be used in the treatment of respiratory conditions like asthma and chronic obstructive pulmonary disease (COPD). However, they have a narrow therapeutic window, and elevated levels can lead to toxicity. Central nervous system side effects, such as restlessness, insomnia, and seizures, can occur with elevated theophylline levels.
The nurse knows that montelukast (Singulair) is given for what purpose?
Explanation
A. Seasonal allergy only
Montelukast may be used for the treatment of allergic rhinitis associated with seasonal allergies, but its primary use is for asthma prevention.
B. Severe asthmatic attacks
Montelukast is not typically used for the treatment of severe asthmatic attacks. Short-acting bronchodilators and systemic corticosteroids are more commonly used in this scenario.
C. Acute bronchospasm
While montelukast has a role in the prevention of bronchospasm, it is not typically used for the acute treatment of bronchospasm. Short-acting bronchodilators are more appropriate for immediate relief of bronchospasm.
D. Maintenance and prevention of asthma
Montelukast (Singulair) is used for the maintenance and prevention of asthma. It is a leukotriene receptor antagonist that works by blocking the action of leukotrienes, which are inflammatory mediators involved in the pathophysiology of asthma. By inhibiting leukotrienes, montelukast helps to reduce airway inflammation and bronchoconstriction, thereby preventing asthma symptoms.
In which of the following scenarios would the RN anticipate glucocorticoids (steroids) to be prescribed?
Explanation
A. Maintenance therapy of controlled chronic asthma
Glucocorticoids are commonly used as maintenance therapy for controlled chronic asthma to prevent exacerbations and maintain long-term control.
B. Severe asthmatic attack
While bronchodilators are often the first-line treatment for a severe asthmatic attack, glucocorticoids may be added to reduce inflammation and improve overall outcomes.
C. Asthma that is unresponsive to bronchodilator therapy
In cases where asthma is unresponsive to bronchodilator therapy or there is an exacerbation of asthma symptoms, glucocorticoids (steroids) are often prescribed. These medications have anti-inflammatory effects and can help reduce airway inflammation, improving symptoms and preventing further exacerbation.
D. Acute allergic reaction
Glucocorticoids may be used in the management of acute allergic reactions, but they are not the first-line treatment. Antihistamines and other medications are typically used initially, and glucocorticoids may be added in certain cases.
The prescriber has written a new order for a glucocorticoid inhaler for a client being discharged to home. What information should be included in the teaching plan regarding the use of this medication?
Explanation
A. “This medication is a leading cause of bronchospasm.”
Glucocorticoid inhalers are not a leading cause of bronchospasm. In fact, they are often prescribed to reduce inflammation and prevent bronchospasm in conditions like asthma and chronic obstructive pulmonary disease (COPD).
B. “This medication will cause you to become fatigued.”
Fatigue is not a common side effect of inhaled glucocorticoids. Systemic effects are more likely with oral or intravenous administration, whereas inhaled forms are designed to have localized effects.
C. “You must gargle and rinse your mouth immediately after each use of this medication.”
Inhaled glucocorticoids can sometimes lead to local side effects, such as oral candidiasis (thrush) or hoarseness. Gargling and rinsing the mouth after using the inhaler can help minimize these side effects by reducing the risk of fungal overgrowth in the mouth and throat.
D. “This medication may cause you to feel anxious.”
Anxiety is not a common side effect of inhaled glucocorticoids. Again, systemic effects are more associated with other routes of administration. The use of inhaled glucocorticoids is generally well-tolerated when used as directed.
A patient will begin using ipratropium bromide (Atrovent), albuterol (Proventil), and an inhaled glucocorticoid medication (steroid) to treat chronic bronchitis.
When teaching this patient about disease and medication management, the nurse will instruct the patient to administer these medications in which order?
Explanation
The correct order for administering ipratropium bromide (Atrovent), albuterol (Proventil), and an inhaled glucocorticoid (steroid) to treat chronic bronchitis is:
C. Ipratropium bromide (Atrovent), albuterol (Proventil), glucocorticoid (steroid)
Here's the rationale for this order:
Ipratropium bromide (Atrovent): Ipratropium is an anticholinergic bronchodilator that helps to relax the muscles around the airways, allowing for increased airflow. It is typically recommended to use ipratropium before other bronchodilators to maximize their effectiveness.
Albuterol (Proventil): Albuterol is a short-acting beta-agonist bronchodilator. It works by relaxing the muscles in the airways, leading to improved airflow. Using it after ipratropium further promotes bronchodilation.
Glucocorticoid (steroid): Inhaled glucocorticoids have anti-inflammatory effects and help to reduce airway inflammation. Using the glucocorticoid last allows it to reach the airways and exert its anti-inflammatory effects.
A patient is receiving a glucocorticoid medication to treat an exacerbation of COPD and the provider has ordered a slow taper in order to discontinue this medication. The nurse explains to the patient that this is done to prevent which condition?
Explanation
A. Adrenocortical insufficiency
Tapering glucocorticoid medications is done to prevent adrenocortical insufficiency, also known as adrenal insufficiency or adrenal suppression. Prolonged use of glucocorticoids can suppress the natural production of cortisol by the adrenal glands. Abrupt discontinuation of glucocorticoids can lead to adrenal insufficiency, characterized by symptoms such as fatigue, weakness, weight loss, and potentially life-threatening complications.
B. Thyroid storm
Thyroid storm is a severe and life-threatening condition related to overactivity of the thyroid gland. It is not a consequence of tapering glucocorticoids.
C. Acromegaly
Acromegaly is a disorder characterized by the excessive production of growth hormone, often caused by a pituitary tumor. It is not related to glucocorticoid tapering.
D. Hypertensive crisis
Hypertensive crisis refers to a severe and abrupt increase in blood pressure. It is not a known consequence of tapering glucocorticoid medications.
Sign Up or Login to view all the 34 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

