Summary
Total Questions : 20
Showing 20 questions, Sign in for moreA nurse is assessing a client who is in labor and notes that the fetal head is visible at the vaginal opening but does not advance with pushing.
The nurse should identify this finding as which of the following?
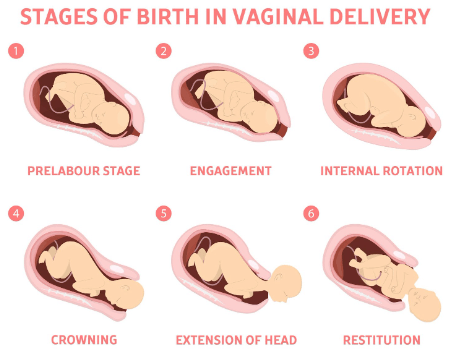
Explanation
Crowning is when the fetal head is visible at the vaginal opening and does not slip back in with each contraction.This indicates that the baby is ready to be born and the mother should stop pushing to avoid tearing or the need for an episiotomy.
A nurse is caring for a client who has prolonged labor and is at risk for infection.
Which of the following actions should the nurse take to reduce this risk? (Select all that apply.)
Explanation
These actions can help reduce the risk of infection for the client who has prolonged labor.
• ChoiceBis correct because changing perineal pads every 2 hours can prevent bacterial growth and contamination of the genital tract.
• ChoiceCis correct because encouraging oral fluid intake can help maintain hydration and blood volume, which can improve uterine perfusion and prevent maternal and fetal acidosis.
• ChoiceDis correct because administering IV antibiotics as prescribed can prevent or treat maternal peripartum infections, which are among the leading causes of maternal mortality worldwide.
• ChoiceEis correct because using sterile gloves when providing perineal care can prevent introducing pathogens into the genital tract.
A nurse is preparing to assist with an emergency cesarean delivery for a client who has a ruptured uterus.
Which of the following equipment should the nurse have readily available? (Select all that apply.)
Explanation
Oxygen mask and tubing and blood products and IV fluids should be readily available for a client who has a ruptured uterus.This is because a ruptured uterus can cause severe hemorrhage, hypovolemia, and fetal distress.The client and the fetus may need oxygen therapy and blood transfusion to prevent hypoxia and shock.
A nurse is evaluating a client who has prolonged labor and suspects uterine rupture.
Which of the following findings should alert the nurse to this complication?
Explanation
Uterine rupture can cause fetal distress and hypoxia, which can slow down the fetal heart rate.
Fetal bradycardia is a sign of a serious complication that requires immediate intervention.
A nurse is caring for a client who has prolonged and obstructed labor and develops a vesicovaginal fistula.
Which of the following interventions should the nurse include in the plan of care?
Explanation
a vesicovaginal fistula is an abnormal opening that forms between the bladder and the wall of the vagina, causing urine to leak out of the vagina.Zinc oxide cream can help protect the skin from irritation and infection.
Normal ranges for fluid intake are about 2 to 3 liters per day for healthy adults, depending on age, activity level, and climate.Normal ranges for pelvic floor muscle strength are 10 to 12 contractions of 6 to 8 seconds each, with a rest period of 4 to 6 seconds between each contraction.
A nurse is counseling a client who has a small pelvis and wants to have a vaginal delivery.
Which of the following factors should the nurse consider when discussing the possibility of vaginal birth after cesarean (VBAC)?
Explanation
All of the above factors should be considered when discussing the possibility of vaginal birth after cesarean (VBAC).
Here’s why:
• The type of uterine incision used in the previous cesarean delivery affects the risk of uterine rupture during VBAC.A low transverse incision is associated with the lowest risk, while a high vertical incision is associated with the highest risk.
• The gestational age of the current pregnancy affects the success rate of VBAC.The optimal time for VBAC is between 39 and 40 weeks of gestation.Attempting VBAC before 37 weeks or after 41 weeks may increase the risk of complications.
• The presentation and position of the fetus affects the feasibility and safety of VBAC.A breech presentation, a transverse lie, or a posterior position may make vaginal delivery difficult or impossible.A cephalic presentation and an anterior position are more favorable for VBAC.
A nurse is providing discharge teaching to a client who had a ruptured uterus and a hysterectomy during labor.
Which of the following instructions should the nurse include in the teaching? (Select all that apply.)
Explanation
The nurse should include these instructions in the teaching because:
• Choice B: Using sanitary pads rather than tampons for vaginal bleeding can prevent infection and irritation of the surgical site.
• Choice D: Drinking plenty of fluids and eating foods high in fiber can help prevent constipation, which can strain the abdominal muscles and cause pain.
• Choice E: Reporting any foul-smelling vaginal discharge or fever to the provider can help detect signs of infection, which can be a complication of hysterectomy.
A nurse is reviewing the risk factors for uterine rupture with a group of nursing students.
Which of the following risk factors should the nurse include? (Select all that apply.)
Explanation
Intrauterine infection is a risk factor for uterine rupture because it can weaken the uterine wall and make it more prone to tearing.
The most common risk factor for uterine rupture is having a previous cesarean delivery or other uterine surgery that leaves a scar on the uterus.Other risk factors include uterine trauma, congenital uterine anomalies, having multiples or too much amniotic fluid, having a breech baby that requires manual turning, and prolonged labor.
A nurse is monitoring a client who had a vaginal birth after cesarean (VBAC) delivery.
The nurse notes that the client has a boggy uterus, heavy vaginal bleeding, and signs of hypovolemic shock.
The nurse suspects that the client has a concealed uterine rupture.
What is an appropriate nursing action for this client?
Explanation
This is because the client has signs of concealed uterine rupture, which is a rare but serious complication of VBAC delivery.Concealed uterine rupture occurs when the uterus tears through the endometrium and myometrium, but the peritoneum remains intact.This can cause heavy vaginal bleeding, hypovolemic shock, and fetal distress.The priority nursing action is to restore the client’s blood volume and prepare for emergency surgery to deliver the fetus and repair the uterus.
A nurse is caring for a client who is in active labor and experiencing shoulder dystocia.
Which of the following actions should the nurse take? (Select all that apply.).
Explanation
Applying suprapubic pressure and assisting the provider with McRoberts maneuver are two nursing interventions that can help dislodge the impacted shoulder and facilitate the delivery of the baby.
Normal ranges for fetal heart rate are 110 to 160 beats per minute, and for maternal blood pressure are 110/70 to 140/90 mm Hg.
A nurse is assessing a client who is in labor and has been pushing for 3 hours with no progress.
The nurse should identify that this client is at risk for which of the following complications? (Select all that apply.).
Explanation
A client who is in labor and has been pushing for 3 hours with no progress is at risk for postpartum hemorrhage and maternal exhaustion.This is because a prolonged second stage of labor can cause uterine atony, which is a failure of the uterus to contract and stop bleeding after delivery.It can also cause fatigue, dehydration, and electrolyte imbalance in the mother.
A nurse is reviewing the medical record of a client who is in labor and has cephalopelvic disproportion (CPD).
Which of the following findings should the nurse expect to see in the record?
Explanation
A macrosomic fetus is a fetus that is larger than average, usually weighing more than 4 kg or 8.8 lb at birth.A large fetus can cause cephalopelvic disproportion (CPD), which is a condition where the baby’s head does not fit through the mother’s pelvis during labor.CPD can lead to prolonged or obstructed labor, which can endanger both the mother and the baby.
A gush of blood is noted with the rupture of membranes.
On palpation, the uterus is soft (i.e., relaxed) and the patient is not reporting any pain.
An FHR deceleration down to 90 bpm is noted.
What does the nurse suspect has happened?
Explanation
This is a condition where fetal blood vessels that run through the membranes rupture and bleed.
The bleeding is from the fetus, not the mother, and can cause fetal hypoxia and death.
The FHR deceleration indicates fetal distress.
The uterus is soft because there is no uterine bleeding or contraction.
Normal ranges for FHR are 110 to 160 beats per minute.
Normal ranges for uterine contraction frequency are 2 to 5 contractions in 10 minutes.
Normal ranges for uterine contraction duration are 45 to 80 seconds.
Normal ranges for uterine contraction intensity are mild to moderate to palpation
Women with previous uterine scars are prone to uterine rupture, especially if oxytocin or forceps are used.
If a woman complains of a sharp pain accompanied by the abrupt cessation of contractions, suspect uterine rupture, a medical emergency.
Immediate surgical delivery is indicated to save the fetus and mother.
Based on this information, which of the following nursing actions is most appropriate?
Explanation
This is because uterine rupture is a life-threatening complication that requires immediate surgical intervention to save the mother and the fetus.
Delaying the delivery can result in hemorrhage, shock, infection, and fetal death.
A nurse is reviewing the partograph of a client in labor.
The nurse notes that the cervical dilation curve is above the alert line and below the action line.
What does this indicate?
Explanation
This is because the cervical dilation curve is above the alert line and below the action line, which means that the dilation is less than 1 cm per hour.This indicates a possible delay in labor progress and a risk of complications such as fetal distress, infection, or postpartum hemorrhage.
A nurse is assisting a client who has prolonged and obstructed labor to deliver by vacuum extraction.
Which of the following complications should the nurse monitor for in the newborn?
Explanation
Caput succedaneum is a swelling of the scalp that can occur after vacuum extraction delivery.It is caused by the pressure of the suction cup on the baby’s head and usually resolves within a few days.
A nurse is evaluating a client who has prolonged and obstructed labor for signs of postpartum hemorrhage.
Which of the following findings is an early indicator of postpartum hemorrhage?
Explanation
A boggy uterus that does not respond to massage is an early indicator of postpartum hemorrhage.
A boggy uterus means that the uterus is not contracting properly after delivery, which can lead to excessive bleeding from the site where the placenta was attached.This condition is called uterine atony and it is the most common cause of postpartum hemorrhage.
Massage can help stimulate the uterus to contract and stop the bleeding, but if it does not work, other interventions are needed.
A nurse is assessing a client who had a prolonged labor and is at risk for uterine atony.
Which of the following findings should indicate to the nurse that the client has this condition? Select all that apply.
Explanation
A boggy uterus is a sign of uterine atony, which is the failure of the uterus to contract sufficiently after childbirth.
This can lead to excessive bleeding and postpartum hemorrhage.
A firm fundus at the umbilicus is a normal finding after delivery and indicates that the uterus is contracting well.
Excessive lochia rubra is also a sign of uterine atony and postpartum hemorrhage.Lochia rubra is the vaginal discharge composed of blood, mucus, and tissue from the placenta and the uterus lining that occurs after childbirth.
It is normal for the first 3 to 4 days, but it should gradually decrease in amount and change in color.
Clots larger than a quarter are abnormal and indicate excessive bleeding.
A pulse rate of 110/min is a sign of tachycardia, which can be caused by blood loss, infection, or pain.
A normal pulse rate for an adult is between 60 and 100 beats per minute.
A nurse is caring for a client who had a vacuum-assisted delivery due to prolonged labor and is at risk for developing a hematoma in the perineal area.
Which of the following manifestations should alert the nurse to this complication?
Explanation
Severe perineal pain is a manifestation of a hematoma in the perineal area, which can result from vacuum-assisted delivery.A hematoma is a collection of blood under the skin or in the tissues that can cause pressure and pain.
Normal ranges for hemoglobin are 12 to 16 g/dL for women and 14 to 18 g/dL for men.Normal ranges for white blood cell count are 4,000 to 11,000 cells per microliter of blood.
A nurse is providing emotional support to a client who had a prolonged labor and delivered a stillborn baby by cesarean section.
Which of the following actions should the nurse take?
Explanation
Grief is a normal and natural response to the loss of a baby, and the nurse should provide emotional support and acknowledge the client’s pain.The nurse should also respect the client’s personal, cultural, or religious needs and preferences regarding the care of the baby.
Sign Up or Login to view all the 20 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

