Chemotherapy Agents and Oncology Pharmacology > Pharmacology
Exam Review
Targeted Therapy and Immunotherapy in Oncology
Total Questions : 5
Showing 5 questions, Sign in for moreA nurse is caring for a client who is receiving rituximab, a monoclonal antibody, as part of targeted therapy for nonHodgkin's lymphoma. The nurse should monitor the client for which of the following adverse effects of this drug?
Explanation
Choice A reason:
Infusion reactions and allergic reactions are common and potentially serious adverse effects of rituximab, a monoclonal antibody that binds to the CD20 antigen on the surface of B lymphocytes and causes their destruction. Rituximab is used to treat nonHodgkin's lymphoma, a type of cancer that affects the lymphatic system. Infusion reactions can occur during or shortly after the administration of rituximab and may include fever, chills, rigors, hypotension, dyspnea, bronchospasm, angioedema, and anaphylaxis. Allergic reactions can occur within hours or days after the infusion and may include rash, urticaria, pruritus, and serum sickness. The nurse should monitor the client's vital signs, oxygen saturation, and symptoms during and after the infusion and administer premedications, such as antihistamines, corticosteroids, and acetaminophen, as prescribed.
Choice B reason:
Gastrointestinal toxicity and hepatotoxicity are not common adverse effects of rituximab, a monoclonal antibody that is used to treat nonHodgkin's lymphoma. Gastrointestinal toxicity and hepatotoxicity may be caused by other drugs, such as methotrexate and cyclophosphamide, which are often used in combination with rituximab. The nurse should monitor the client's liver function tests, such as serum bilirubin, alkaline phosphatase, and transaminases, and report any abnormalities to the provider.
Choice C reason:
Hypertension and bleeding are not common adverse effects of rituximab, a monoclonal antibody that is used to treat nonHodgkin's lymphoma. Hypertension and bleeding may be caused by other factors, such as renal impairment, coagulation disorders, or anticoagulant therapy. The nurse should monitor the client's blood pressure, urine output, creatinine clearance, coagulation studies, platelet count, and signs of bleeding.
Choice D reason:
Flulike symptoms and bone marrow suppression are not common adverse effects of rituximab, a monoclonal antibody that is used to treat nonHodgkin's lymphoma. Flulike symptoms and bone marrow suppression may be caused by other drugs, such as interferon alfa and vinblastine, which are also used to treat nonHodgkin's lymphoma. The nurse should monitor the client's temperature, white blood cell count, hemoglobin level, and symptoms of infection or anemia.
A nurse is administering erlotinib, a tyrosine kinase inhibitor, to a client who has lung cancer. The nurse should instruct the client to report which of the following adverse effects of this drug? (Select all that apply.)
Explanation
Choice A reason:
Diarrhea and abdominal pain are common and potentially serious adverse effects of erlotinib, a tyrosine kinase inhibitor that blocks the epidermal growth factor receptor (EGFR) and inhibits the growth and survival of cancer cells. Erlotinib is used to treat lung cancer, a type of cancer that affects the respiratory system. Diarrhea and abdominal pain can indicate gastrointestinal toxicity, which can lead to dehydration, electrolyte imbalance, and perforation. The client should report these symptoms to the provider and receive appropriate treatment, such as fluids, electrolytes, and antidiarrheal drugs.
Choice B reason:
Jaundice and dark urine are rare but serious adverse effects of erlotinib, a tyrosine kinase inhibitor that is used to treat lung cancer. Jaundice and dark urine can indicate liver damage, which can impair the liver's function and cause complications, such as bleeding, infection, and encephalopathy. The client should report these symptoms to the provider and have their liver function tests, such as serum bilirubin, alkaline phosphatase, and transaminases, monitored regularly.
Choice C reason:
Skin rash and dry skin are common and usually mild adverse effects of erlotinib, a tyrosine kinase inhibitor that is used to treat lung cancer. Skin rash and dry skin can occur because erlotinib affects the EGFR in the skin cells as well as the cancer cells. The client should report these symptoms to the provider and use moisturizers, sunscreen, and mild soap to prevent skin irritation and infection.
Choice D reason:
Chest pain and dyspnea are not common adverse effects of erlotinib, a tyrosine kinase inhibitor that is used to treat lung cancer. Chest pain and dyspnea may be caused by other factors, such as cardiac or pulmonary problems. The client should report these symptoms to the provider and have their cardiac and pulmonary function assessed.
Choice E reason:
Fever and chills are not common adverse effects of erlotinib, a tyrosine kinase inhibitor that is used to treat lung cancer. Fever and chills may indicate infection, which is a risk factor for clients receiving chemotherapy. Chemotherapy drugs can suppress the immune system and make the client more susceptible to infections. The client should report these symptoms to the provider and have their temperature, white blood cell count, and cultures monitored.
A nurse is educating a client who has colorectal cancer and is receiving bevacizumab, an angiogenesis inhibitor, as part of targeted therapy. The nurse should explain to the client that bevacizumab works by:
Explanation
Choice A reason:
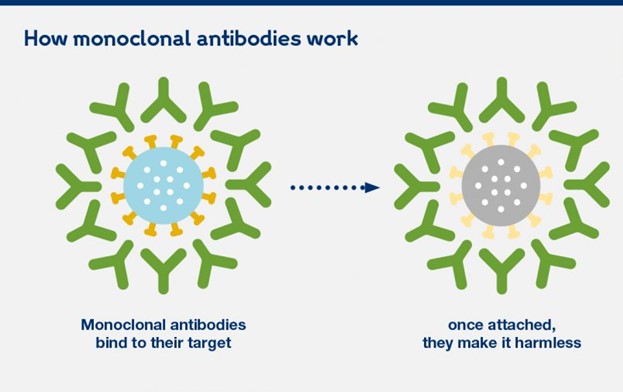
Binding to specific antigens on cancer cells and triggering their destruction is the mechanism of action of monoclonal antibodies, such as rituximab and trastuzumab, that are used to treat some types of cancer, such as nonHodgkin's lymphoma and breast cancer. Monoclonal antibodies are proteins that recognize and attach to specific antigens on the surface of cancer cells and activate the immune system to destroy them.
Choice B reason:
Inhibiting the activity of enzymes that mediate cell growth and survival signals is the mechanism of action of tyrosine kinase inhibitors, such as erlotinib and imatinib, that are used to treat some types of cancer, such as lung cancer and chronic myeloid leukemia. Tyrosine kinase inhibitors are drugs that block the activity of enzymes called tyrosine kinases, which are involved in transmitting signals from growth factors and hormones to the cell nucleus.
Choice C reason:
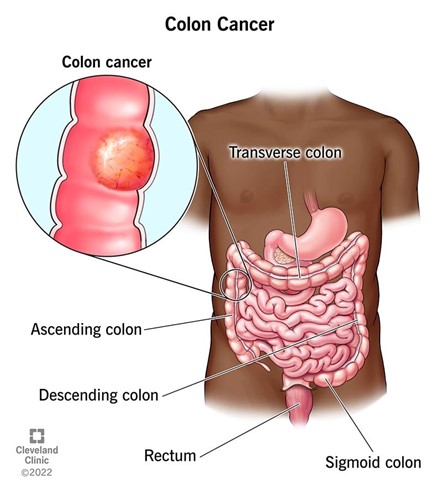
Preventing the formation of new blood vessels that supply oxygen and nutrients to tumors is the mechanism of action of angiogenesis inhibitors, such as bevacizumab and sorafenib, that are used to treat some types of cancer, such as colorectal cancer and renal cell carcinoma. Angiogenesis inhibitors are drugs that interfere with the process of angiogenesis, which is the formation of new blood vessels from existing ones. Angiogenesis is essential for tumor growth and metastasis, as tumors need a constant supply of oxygen and nutrients to survive and spread.
Choice D reason:
Enhancing the immune system's ability to recognize and eliminate cancer cells is the mechanism of action of immunotherapy, such as interferon alfa and interleukin2, that are used to treat some types of cancer, such as melanoma and renal cell carcinoma. Immunotherapy is a type of treatment that uses substances produced by the body or made in a laboratory to boost or restore the immune system's function. Immunotherapy can stimulate the immune system to attack cancer cells or make them more visible to the immune system.
A nurse is caring for a client who has melanoma and is receiving interferon alfa2b, an immunomodulator, as part of immunotherapy. The client tells the nurse that he feels tired, achy, and feverish after each injection. The nurse should respond by saying:
Explanation
Choice A reason:
These are not normal side effects of interferon alfa2b, but symptoms of flulike syndrome, which is a common and potentially serious adverse effect of interferon alfa2b, an immunomodulator that enhances the immune system's ability to recognize and eliminate cancer cells. Interferon alfa2b is used to treat melanoma, a type of skin cancer that develops from melanocytes. Flulike syndrome can cause fever, chills, fatigue, myalgia, headache, and malaise. These symptoms may not go away after a few days, but may persist or worsen during the course of treatment.
Choice B reason:
These are not signs of an allergic reaction to interferon alfa2b, but symptoms of flulike syndrome caused by interferon alfa2b. An allergic reaction to interferon alfa2b would manifest as rash, urticaria, pruritus, angioedema, or anaphylaxis. The client should not stop taking interferon alfa2b without consulting the provider, as this may compromise the effectiveness of the treatment.
Choice C reason:
These are symptoms of flulike syndrome caused by interferon alfa2b. The nurse should explain to the client that flulike syndrome is a common adverse effect of interferon alfa2b and provide education on how to manage it. The nurse should advise the client to take acetaminophen as prescribed to reduce fever and pain, drink plenty of fluids to prevent dehydration, rest as needed to conserve energy, and report any severe or persistent symptoms to the provider.
Choice D reason:
These are not indications of bone marrow suppression caused by interferon alfa2b, but symptoms of flulike syndrome caused by interferon alfa2b. Bone marrow suppression is another possible adverse effect of interferon alfa2b, which can result in leukopenia, anemia, and thrombocytopenia. Bone marrow suppression can cause symptoms such as infection, bleeding, or pallor. The client should have their blood counts monitored regularly and receive supportive care as needed.
A nurse is administering nivolumab, a checkpoint inhibitor, to a client who has renal cell carcinoma. The nurse should identify that nivolumab can cause which of the following adverse effects?
Explanation
Choice A reason:
Cardiotoxicity and extravasation injury are not common adverse effects of nivolumab, a checkpoint inhibitor that blocks the programmed cell death1 (PD1) receptor and enhances the immune system's ability to recognize and eliminate cancer cells. Nivolumab is used to treat renal cell carcinoma, a type of kidney cancer that originates from the renal tubules. Cardiotoxicity and extravasation injury may be caused by other drugs, such as anthracyclines and vinca alkaloids, which are used to treat other types of cancer.
Choice B reason:
Peripheral neuropathy and pulmonary fibrosis are not common adverse effects of nivolumab, a checkpoint inhibitor that is used to treat renal cell carcinoma. Peripheral neuropathy and pulmonary fibrosis may be caused by other drugs, such as natural products and antineoplastic antibiotics, which are used to treat other types of cancer.
Choice C reason:
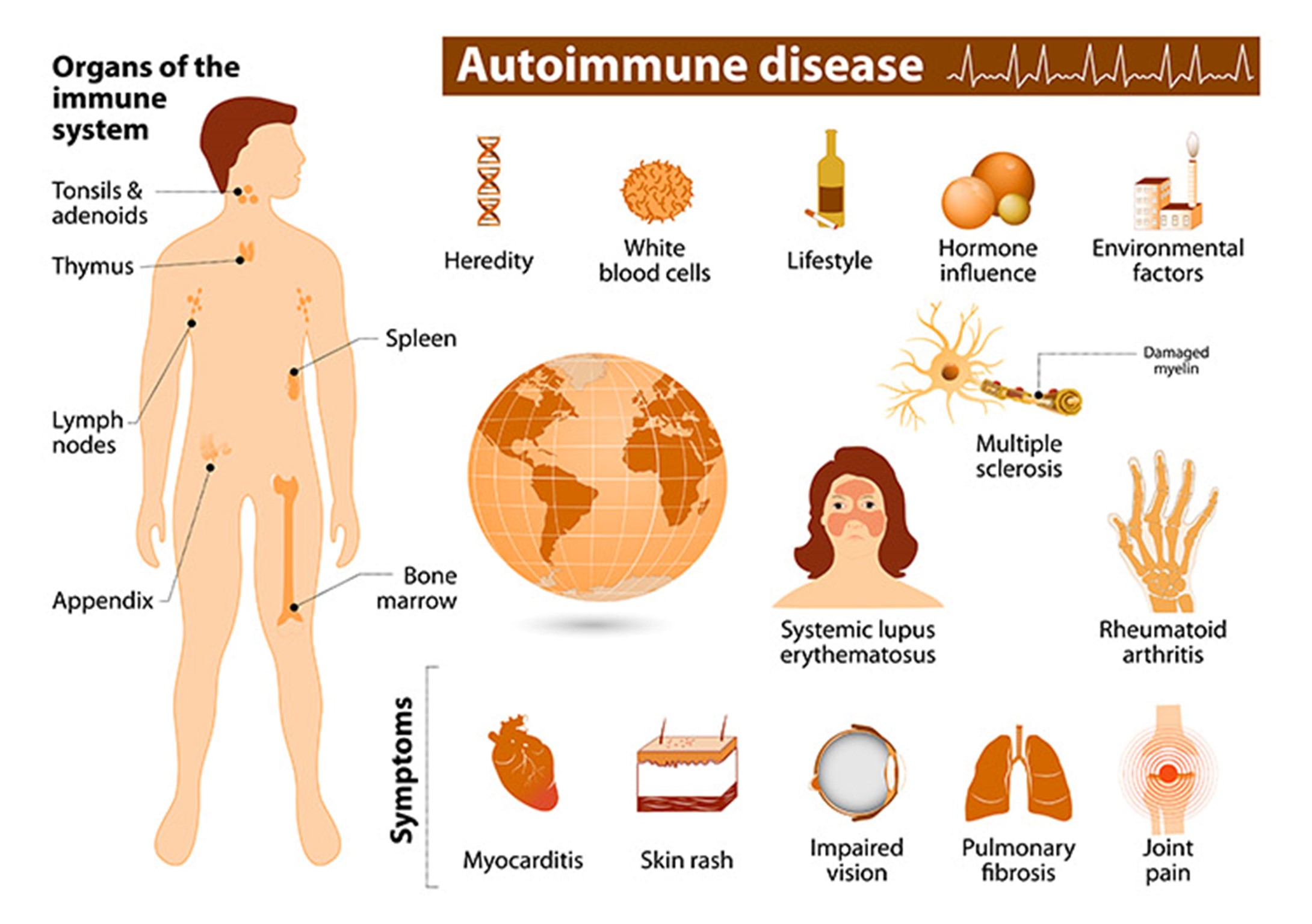
Autoimmune disorders and organ dysfunction are common and potentially serious adverse effects of nivolumab, a checkpoint inhibitor that is used to treat renal cell carcinoma. Autoimmune disorders and organ dysfunction can occur because nivolumab affects the PD1 receptor in the immune cells as well as the cancer cells. The PD1 receptor normally acts as a brake on the immune system and prevents it from attacking healthy tissues. By blocking the PD1 receptor, nivolumab can unleash the immune system and cause it to attack various organs, such as the skin, lungs, liver, kidneys, thyroid, pituitary gland, colon, and pancreas. The client should be monitored for signs and symptoms of autoimmune disorders and organ dysfunction, such as rash, pruritus, dyspnea, cough, jaundice, dark urine, fatigue, weight loss or gain, diarrhea, abdominal pain, and hypotension or hypertension. The client should receive corticosteroids or immunosuppressive drugs as prescribed to suppress the immune system and prevent further damage.
Choice D reason:
Thrombosis and teratogenicity are not common adverse effects of nivolumab, a checkpoint inhibitor that is used to treat renal cell carcinoma. Thrombosis and teratogenicity may be caused by other factors, such as coagulation disorders, genetic mutations, or pregnancy. The client should have their coagulation studies monitored regularly and receive anticoagulant therapy as prescribed to prevent thrombosis. The client should also avoid pregnancy while receiving nivolumab and use effective contraception methods.
Sign Up or Login to view all the 5 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

