WGU Dosage Calculations
Total Questions : 53
Showing 25 questions, Sign in for moreA client is receiving intravenous (1V) vancomycin and the nurse plans to draw blood for a peak a. trough to determine the serum level of the drug. Which collection times provide the best determination of these levels?
Explanation
A. Thirty minutes into the administration of the IV dose and 30 minutes before the next administration of the medication:
This timing doesn't align with the standard practice of drawing peak levels immediately after the IV dose is completed.
The trough level should be taken just before the next dose, not 30 minutes before.
B. Two hours after completion of the IV dose and 1 hour before the next administration of the medication:
Waiting for two hours after the dose to draw the peak level is too long. Peak levels are typically drawn immediately after completion.
Drawing the trough level one hour before the next dose doesn't provide an accurate assessment of the lowest drug concentration just before the next administration.
C. One hour after completion of the IV dose and one hour before the next administration of the medication:
Similar to choice B, waiting one hour after the dose to draw the peak level is not in line with standard practice.
Drawing the trough level one hour before the next dose is administered is too early to accurately represent the lowest concentration.
The best collection times for determining the peak and trough levels of intravenous (IV) vancomycin are:
D. Immediately after completion of the IV dose and 30 minutes before the next administration of the medication.
Explanation:
Peak Level: Peak levels of vancomycin are drawn immediately after the completion of the IV dose. This is done to assess the highest concentration of the drug in the bloodstream, which is important for ensuring its therapeutic efficacy and monitoring for potential toxicity.
Trough Level: Trough levels are drawn just before the next dose is administered. A trough level represents the lowest concentration of the drug in the bloodstream, ensuring that the drug is still present at a therapeutic level before the next dose is given. Taking the trough level 30 minutes before the next administration is appropriate, as it allows time for the drug to reach its lowest concentration before receiving the next dose.
Which nursing action has the highest priority when administering a dose of codeine with acetaminophen to a client?
Explanation
While administering a stool softener or laxative can be important to prevent constipation associated with opioids, it is not the highest priority action at the time of medication administration. Ensuring the client's safety during ambulation takes precedence.
The nursing action with the highest priority when administering a dose of codeine with acetaminophen to a client is:
B. Instruct the client to request assistance when ambulating to the bathroom.
Explanation: Codeine is an opioid medication that can cause drowsiness, sedation, and impaired coordination. It can also have constipating effects. Therefore, the highest priority is ensuring the client's safety while ambulating to the bathroom to prevent falls or other accidents. Instructing the client to request assistance when ambulating is essential to prevent potential injuries.
C. Tell the client to notify the nurse if the pain is not relieved:
This is an important instruction, but it is not the highest priority when the client is about to ambulate. Safety during ambulation is the immediate concern.
D. Advise the client that the medication should start to work in about 30 minutes:
Providing information about when the medication is expected to take effect is helpful but not the highest priority at this moment. Safety during ambulation is the primary concern before the client receives the medication.
The nurse is planning care for a client with major depression who is receiving a new prescription for duloxetine. Which information is most important for the nurse to obtain?
Explanation
A. Weight change in the last month:
While monitoring weight changes is important in clients with depression, it is not the most critical piece of information to obtain before initiating duloxetine. Weight changes are one of many possible side effects of the medication.
B. Recent use of other antidepressants:
Knowing about the client's previous antidepressant use is relevant, but it is not the most critical information to obtain before starting duloxetine. The choice of medication should be based on the client's current clinical condition and needs.
The most important information for the nurse to obtain when planning care for a client with major depression receiving a new prescription for duloxetine is:
C. Liver function laboratory results.
Explanation: Duloxetine is an antidepressant medication that can affect liver function. It is important to assess the client's liver function through laboratory results before starting the medication to ensure that the client's liver can metabolize the drug safely. Monitoring liver function during treatment is also essential to identify any potential adverse effects on the liver.
D. Family history of mental illness:
While family history can provide valuable information about a client's risk factors for mental illness, it is not the most crucial information to obtain before starting duloxetine. Assessing the client's current medical status and the potential impact of the medication on their liver function takes precedence.
The nurse admits a client with a diagnosis of stage 4 cancer. The client has a prescription to wear a subcutaneous morphine sulfate patch for pain. The client is short of breath and difficult to arouse. While performing a head to toe assessment, the nurse discovers four patches on the client's body. Which action should the nurse take first?
Explanation
A. Administer a narcotic reversal drug:
While administering a narcotic reversal drug (such as naloxone) can be necessary if the client's respiratory depression persists or worsens, it is not the first action. The first step is to remove the source of the potential overdose, which is the excess morphine patches.
The first action the nurse should take in this situation is:
B. Remove the morphine patches.
Explanation: If the client is experiencing difficulty breathing and is difficult to arouse, it is possible that they have received an excessive dose of morphine, which could lead to respiratory depression. Removing the morphine patches is a critical step in reducing the risk of further respiratory depression and overdose. It is important to address the immediate cause of the symptoms.
C. Monitor blood pressure:
Monitoring blood pressure is important for assessing the client's overall condition, but it is not the first action in this scenario where respiratory distress and possible narcotic overdose are the primary concerns.
D. Apply oxygen face mask:
Providing oxygen can help improve oxygenation, but it does not address the potential overdose caused by the excessive use of morphine patches. The priority is to remove the source of the overdose first.
In summary, the initial action should be to remove the excessive morphine patches to reduce the risk of further respiratory depression, and then further interventions, such as administering a narcotic reversal drug, can be considered as needed based on the client's response.
A male client with a history of heart failure (HF) complains of heartburn when he lies down after dinner. The home health nurse should encourage the client to talk to the healthcare provider about using which over-the-counter medication to relieve this problem?
Explanation
The over-the-counter medication that the home health nurse should encourage the client with a history of heart failure (HF) to discuss with the healthcare provider to relieve heartburn when lying down after dinner is:
A. Low sodium antacid.
Explanation: Heartburn is a common symptom of gastroesophageal reflux disease (GERD), and it can exacerbate symptoms in individuals with heart failure due to the discomfort and potential fluid retention associated with excessive sodium intake. Low sodium antacids can help relieve heartburn without exacerbating fluid retention, making them a better choice for individuals with heart failure.
B. Diphenhydramine:
Diphenhydramine is an antihistamine commonly used to relieve allergies and may cause drowsiness. It is not indicated for heartburn or GERD symptoms.
C. Acetaminophen:
Acetaminophen is a pain reliever and fever reducer. It is not used to address heartburn or GERD symptoms.
D. Low dose aspirin:
Aspirin is typically used to prevent cardiovascular events in individuals at risk for heart disease but is not used to treat heartburn or GERD symptoms. In fact, aspirin can irritate the stomach lining and potentially worsen heartburn symptoms.
While assessing a client who takes acetaminophen for chronic pain, the nurse observes that the client's skin looks yellow in color. Which action should the nurse take in response to this finding?
Explanation
A. Use a pulse oximeter to assess oxygen saturation:
Oxygen saturation assessment is unrelated to the observation of jaundice. Jaundice primarily indicates a potential liver issue, not an oxygenation problem.
When a nurse observes that a client taking acetaminophen for chronic pain has yellowish skin (jaundice), the appropriate action is:
B. Report the finding to the healthcare provider.
Explanation: Yellowing of the skin (jaundice) can indicate a potential liver problem, and acetaminophen is metabolized by the liver. It's crucial to report this finding to the healthcare provider promptly so that they can assess the client's liver function and determine whether the jaundice is related to the medication or another underlying condition. Monitoring and addressing liver function is essential when using medications metabolized by the liver like acetaminophen.
C. Advise the client to reduce the medication dose:
In cases of jaundice, reducing the medication dose may not be sufficient. A healthcare provider needs to evaluate the client's liver function and determine the appropriate course of action.
D. Check the client's capillary glucose level:
Assessing the capillary glucose level is not relevant to the observation of jaundice. Jaundice is related to liver function and bilirubin metabolism, while glucose levels are related to diabetes management or other glucose-related issues.
The nurse administers risedronate to a client with osteoporosis at 0700. The client asks for a glass of milk to drink with the medication. Which action should the nurse take?
Explanation
A. Consulting with a pharmacist about scheduling the dose one hour after the client eats:
While it is important to take risedronate on an empty stomach, waiting one hour after eating is insufficient. The recommendation is to take it first thing in the morning, at least 30 minutes before any other food or drink, including milk.
B. Withholding the medication until the client's breakfast tray is available on the unit:
Delaying the administration of risedronate until breakfast may not align with the recommended dosing instructions, which specify taking it in the morning on an empty stomach. Delaying the medication could affect its effectiveness.
C. Assigning unlicensed assistive personnel (UAP) to bring the client a glass of low-fat milk:
Providing milk or other beverages with risedronate is not appropriate, as it can interfere with the medication's absorption. Instructing the client to take it with water alone is the correct approach.
The correct action for the nurse to take when the client with osteoporosis asks for a glass of milk to drink with risedronate is:
D. Instruct the client that it is necessary to take nothing but water with the medication.
Explanation: Risedronate is a bisphosphonate medication used to treat osteoporosis. It is essential that it be taken with plain water (typically at least 6-8 ounces) on an empty stomach, preferably in the morning before any food, beverages, or other medications. Consuming other liquids, especially milk or calcium-containing beverages, can interfere with the absorption of the medication. Therefore, instructing the client to take risedronate with water alone is the correct action to ensure its effectiveness.
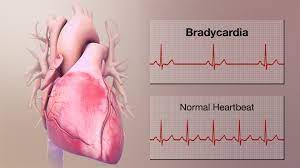
The nurse prepares to administer a scheduled dose of labetalol by mouth to a client with hypertension. The client's vital signs are temperature 99° F (37.2° C), heart rate 48 beats/minute, respirations 16 breaths/minute, and blood pressure (B/P) 150/90 mm Hg. Which action should the nurse take?
Explanation
A. Apply a telemetry monitor before administering the dose:
While monitoring the client's heart rate is important, applying a telemetry monitor may not be necessary at this stage. The primary concern is addressing the bradycardia and elevated blood pressure by notifying the healthcare provider.
B. Administer the dose and monitor the client's BP regularly:
Administering the dose without addressing the low heart rate and inadequate blood pressure control may not be safe. The healthcare provider should be consulted before proceeding.
The action the nurse should take when preparing to administer a scheduled dose of labetalol to a client with hypertension, with vital signs including a heart rate of 48 beats/minute and a blood pressure of 150/90 mm Hg, is:
C. Withhold the scheduled dose and notify the healthcare provider.
Explanation: Labetalol is a beta-blocker used to treat hypertension. A heart rate of 48 beats/minute indicates bradycardia, which is a potential side effect of labetalol. Additionally, the client's blood pressure remains elevated (150/90 mm Hg), which suggests that the medication may not be effectively controlling blood pressure at this time. Before administering the dose, it is important to withhold it and notify the healthcare provider to discuss the client's low heart rate and inadequate blood pressure control. The healthcare provider can assess whether a dose adjustment or alternative treatment is necessary.
D. Assess for orthostatic hypotension before administering the dose:
While orthostatic hypotension assessment is important when starting antihypertensive medications, it does not address the immediate concerns of bradycardia and elevated blood pressure. The healthcare provider should be notified before administering the medication.
The nurse is caring for a client who has been taking ibuprofen. Which finding is most important for the nurse report to the healthcare provider?
Explanation
A. Dizziness:
While dizziness can be a side effect of ibuprofen, it is generally less serious than vomiting blood. Dizziness should still be reported, but it is not as urgently concerning as hematemesis.
B. Nausea:
Nausea is a common side effect of ibuprofen and can occur due to its effects on the stomach lining. While it should be reported, it is not as immediately concerning as vomiting blood.
C. Insomnia:
Insomnia is not typically associated with ibuprofen use and is generally less concerning in this context. It should be addressed but is not a sign of a potentially life-threatening condition.
In summary, the presence of hematemesis is a critical finding that suggests significant gastrointestinal bleeding and requires immediate medical attention when a client is taking ibuprofen.
The finding that is most important for the nurse to report to the healthcare provider when caring for a client who has been taking ibuprofen is:
D. Hematemesis.
Explanation: Hematemesis refers to vomiting blood, which is a serious and potentially life-threatening symptom. Ibuprofen, a nonsteroidal anti-inflammatory drug (NSAID), can cause gastrointestinal irritation, ulcers, and bleeding as side effects. The presence of hematemesis indicates a significant gastrointestinal problem, likely related to the use of ibuprofen, and requires immediate medical attention.
When administering medications to a group of clients, which client should the nurse closely monitor for development of acute kidney injury (AKI)?
Explanation
A. Lorazepam:
Lorazepam is a benzodiazepine used for its anxiolytic and sedative effects. It is not known to cause AKI. Monitoring for sedation and respiratory depression may be necessary, but this is unrelated to kidney function.
The client the nurse should closely monitor for the development of acute kidney injury (AKI) when administering medications is:
B. Vancomycin.
Explanation: Vancomycin, an antibiotic commonly used to treat bacterial infections, has the potential to cause nephrotoxicity (kidney damage), especially when given in high doses or over a prolonged period. Therefore, clients receiving vancomycin should be closely monitored for signs of AKI, including changes in urine output, serum creatinine levels, and other renal function indicators.
C. Sucralfate:
Sucralfate is a medication used to treat and prevent gastrointestinal ulcers. It is not typically associated with AKI. Monitoring for gastrointestinal side effects is more relevant when administering sucralfate.
D. Digoxin:
Digoxin is a medication used to treat heart conditions. While it can affect renal function, it is not a primary cause of AKI. Monitoring serum digoxin levels and assessing for signs of digoxin toxicity are important when administering digoxin, but it is not the primary concern for AKI.
A client with heart failure (HF) develops hyperaldosteronism and spironolactone is prescribed. Which instruction should the nurse include in this client's plan of care?
Explanation
When a client with heart failure (HF) develops hyperaldosteronism and is prescribed spironolactone, the nurse should include the following instruction in the client's plan of care:
A. Limit intake of high-potassium foods.
Explanation: Spironolactone is a potassium-sparing diuretic, and one of its actions is to promote the retention of potassium by the body. Therefore, it's important to instruct the client to limit the intake of high-potassium foods to avoid hyperkalemia (high potassium levels), which can be a potential side effect of this medication. High-potassium foods include bananas, oranges, potatoes, tomatoes, and many others.
Why the other choices are not appropriate:
B. Cover your skin before going outside:
This instruction is not directly related to spironolactone or hyperaldosteronism. It may be relevant for clients taking photosensitizing medications but is not specific to this situation.
C. Monitor skin for excessive bruising:
This instruction is also not directly related to spironolactone or hyperaldosteronism. It may be relevant in other clinical contexts, but it does not address the potential side effects or management of spironolactone.
D. Replace salt with a salt substitute:
While reducing sodium intake is often recommended for clients with heart failure, replacing salt with a salt substitute containing potassium is not advisable for clients taking spironolactone. This would increase the risk of hyperkalemia.
The nurse is administering sodium polystyrene sulfonate to a client in acute kidney injury (AKI). Which laboratory finding indicates that the medication has been effective?
Glucose [Reference Range: 74 to 106 mg/dL (4.1 to 5.9 mmol/L)] Hemoglobin (Hgb) [Reference Range:12-16 g/dL (120-160 g/L)] Potassium (K+) [Reference Range: 3.5 to 5.0 mEq/L (3.5 to 5.0 mmol/L)] Ammonia [Reference Range: Adult: 10 to 80 Mcg/dL (6 to 47 Mcmol/dL)]
Explanation
A. Serum glucose level of 120 mg/dL (6.7 mmol/L):
This glucose level is within the reference range and is not directly related to the effectiveness of sodium polystyrene sulfonate in treating hyperkalemia.
B. Serum ammonia level of 30 Mcg/dL (17.62 Mamal /dL):
Serum ammonia levels are not typically affected by sodium polystyrene sulfonate, and this value is within the reference range.
When administering sodium polystyrene sulfonate to a client with acute kidney injury (AKI), the medication is used to help lower elevated potassium levels (hyperkalemia). Therefore, the laboratory finding that indicates the medication has been effective is:
C. Serum potassium level of 3.8 mEq/L (3.8 mmol/L).
Explanation: Sodium polystyrene sulfonate is a medication used to treat hyperkalemia by exchanging sodium ions for potassium ions in the intestines, leading to the removal of excess potassium from the body through the stool. A reduction in the serum potassium level within the reference range (3.5 to 5.0 mEq/L) indicates that the medication has been effective in lowering the elevated potassium level associated with AKI.
D. Hemoglobin level of 13.5 g/dl (135 g/L):
Hemoglobin levels are unrelated to the effectiveness of sodium polystyrene sulfonate in treating hyperkalemia. This hemoglobin level is within the reference range.
A client taking atorvastatin develops an increased serum creatine phosphokinase (CK) level. The nurse should assess the client for the onset of which problem?
Explanation
A. Muscle tenderness.
Explanation: An increased serum creatine phosphokinase (CK) level can indicate muscle damage, which is a potential side effect of statin medications like atorvastatin. The most common symptom associated with this muscle damage is muscle tenderness, often accompanied by muscle pain or weakness. It's important to assess the client for any signs of muscle problems, as this can be a serious side effect that requires medical attention, and the medication may need to be adjusted or discontinued.
Why the other choices are less relevant:
B. Peripheral edema:
Peripheral edema (swelling of the extremities) is not a typical symptom of muscle damage associated with statin use. It is more commonly associated with other cardiovascular or renal conditions.
C. Excessive bruising:
Excessive bruising is not a typical symptom of muscle damage related to statin use. It is more commonly associated with bleeding disorders or certain medications, such as anticoagulants.
D. Nausea and vomiting:
Nausea and vomiting are not typical symptoms of muscle damage associated with statin use. They are more commonly associated with gastrointestinal side effects or other unrelated issues.
The nurse is providing instructions about a client's new medications. How should the nurse explain the purpose of probenecid, a uricosuric drug?
Explanation
A. Increases the strength of the urine stream:
This is not the purpose of probenecid. Probenecid primarily affects uric acid metabolism in the body, not the strength of the urine stream.
The nurse should explain the purpose of probenecid, a uricosuric drug, as:
B. Promotes excretion of uric acid in the urine.
Explanation: Probenecid is a uricosuric medication that increases the excretion of uric acid in the urine. It works by inhibiting the reabsorption of uric acid in the kidneys, which helps lower blood uric acid levels. This is beneficial in the management of conditions like gout and hyperuricemia, as it can reduce the risk of uric acid crystal formation in joints and tissues.
C. Prevents the formation of kidney stones:
While probenecid may indirectly reduce the risk of certain types of kidney stones associated with high uric acid levels, its primary purpose is not to prevent kidney stone formation. It is used to manage conditions like gout and hyperuricemia.
D. Decreases pain and burning during urination:
Probenecid does not have a direct effect on pain and burning during urination. These symptoms are typically associated with urinary tract infections or other urinary conditions, not gout or hyperuricemia managed with probenecid.
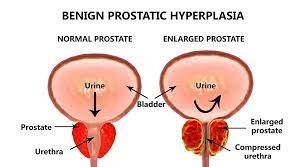
A client with benign prostatic hyperplasia receives a new prescription of tamsulosin. Which intervention should the nurse perform to monitor for an adverse reaction?
Explanation
A. Obtain daily weights:
Daily weights are more relevant for monitoring fluid balance and assessing for edema, which is not a common adverse reaction to tamsulosin.
B. Perform a bladder scan:
Bladder scans may be used to assess for urinary retention or post-void residual urine, but this is not a primary intervention to monitor for adverse reactions to tamsulosin.
C. Assess urine output:
Monitoring urine output is important to assess for urinary retention or changes in urinary function, but it is not the primary intervention for monitoring adverse reactions to tamsulosin.
When a client with benign prostatic hyperplasia (BPH) receives a new prescription for tamsulosin, the nurse should perform the following intervention to monitor for an adverse reaction:
D. Monitor blood pressure.
Explanation: Tamsulosin is an alpha-blocker medication used to relax the smooth muscle in the prostate and bladder neck, thereby improving urinary flow in clients with BPH. However, a potential side effect of alpha-blockers, including tamsulosin, is orthostatic hypotension, which can lead to a sudden drop in blood pressure upon standing. Therefore, monitoring the client's blood pressure is essential to assess for any significant decreases that could result from this medication. Clients should be advised to rise slowly from a sitting or lying position to minimize the risk of orthostatic hypotension.
Prior to administering oral doses of calcitriol and calcium carbonate to a client with hypoparathyroidism, the nurse notes that the client's total calcium level is 14 mg/dL. (3.5 mmol/L). Which action should the nurse implement?
Reference Range
Total Calcium [Reference Range: Adult 9 to 10.5 mg/dl or 2.25 to 2.62 mmol/L]
Explanation
A. Hold the calcitriol but administer the calcium carbonate as scheduled:
Both medications should be held in the presence of significant hypercalcemia. Administering calcium in this situation can exacerbate the elevated calcium levels.
When the nurse notes that a client with hypoparathyroidism has a total calcium level of 14 mg/dL (3.5 mmol/L), which is above the reference range (normal range for adults: 9 to 10.5 mg/dL or 2.25 to 2.62 mmol/L), the appropriate action is:
B. Hold both medications until contacting the healthcare provider.
Explanation: A total calcium level significantly above the reference range can indicate hypercalcemia, which can be a concern, especially for a client with hypoparathyroidism who may be receiving calcium supplementation and calcitriol (active vitamin D) to manage their condition. In cases of hypercalcemia, it is important to withhold calcium and vitamin D supplements and consult the healthcare provider for further evaluation and guidance. The client's calcium levels need to be rechecked, and the treatment plan may need to be adjusted.
C. Hold the calcium carbonate, but administer the calcitriol as scheduled:
Holding only one of the medications is not appropriate when the client has hypercalcemia. Both medications should be withheld pending further evaluation by the healthcare provider.
D. Administer both prescribed medications as scheduled:
Administering both medications when the client has hypercalcemia can worsen the condition and is not appropriate. Hypercalcemia requires intervention and close monitoring.

The nurse initiates an infusion of piperacillin-tazobactam for a client with an urinary tract infection. Five minutes into the infusion, the client reports not feeling well. Which client manifestation should the nurse identify as a reason to stop the infusion?
Explanation
A. Hypertension:
Hypertension (high blood pressure) is not typically associated with piperacillin-tazobactam. While monitoring blood pressure is important during infusions, it is not a reason to stop the infusion on its own.
B. Pupillary constriction:
Pupillary constriction (miosis) is not a common adverse reaction to piperacillin-tazobactam. It is not a primary reason to stop the infusion.
When a client receiving an infusion of piperacillin-tazobactam for a urinary tract infection reports not feeling well, the manifestation that the nurse should identify as a reason to stop the infusion is:
C. Bradycardia.
Explanation: Bradycardia (a slow heart rate) can be an adverse reaction to piperacillin-tazobactam. While it is important to monitor vital signs during the administration of antibiotics, particularly for signs of an allergic reaction or anaphylaxis, bradycardia is a specific manifestation that can be associated with this medication. Stopping the infusion and assessing the client's condition further is appropriate if bradycardia occurs.
D. Scratchy throat:
A scratchy throat could be a sign of an allergic reaction but is not specific to piperacillin-tazobactam. Other signs of an allergic reaction, such as rash, itching, swelling, or difficulty breathing, would be more concerning. In such cases, the infusion should be stopped and appropriate interventions initiated.
A client with pneumonia who has an emergent episode of respiratory distress is intubated and transferred to the intensive care unit. The client's chest x-ray shows consolidation in the left lobe, and physical assessment reveals diminished lung sounds. The nurse administers acetylcysteine as prescribed per nebulization via endotracheal tube. Which therapeutic response of this medication should the nurse expect?
Explanation
A. Unpleasant smell when using the medication:
While acetylcysteine has a distinctive odor, this is not the primary therapeutic response to expect. The odor is often described as unpleasant or sulfur-like.
B. Bronchodilation and wheezing:
Acetylcysteine is not primarily used for bronchodilation. It is used to thin mucus and facilitate its removal. Wheezing is not a common response to acetylcysteine.
When administering acetylcysteine via nebulization through an endotracheal tube to a client with pneumonia, the nurse should expect the following therapeutic response:
C. Increased sputum, requiring suctioning.
Explanation: Acetylcysteine is a mucolytic agent used to help thin and loosen mucus in the airways, making it easier to clear secretions. When administered via nebulization, it can stimulate increased mucus production, which may result in the client needing suctioning to remove the loosened secretions. This is a desired therapeutic effect because it helps clear the airways and improve lung function in clients with conditions like pneumonia.
D. Hypotension:
Hypotension is not a common or expected therapeutic response to acetylcysteine. It is important to monitor blood pressure during administration, but hypotension is not the primary effect of this medication.
The nurse is planning to administer the antiulcer gastrointestinal (GI) agent sucralfate to a client with peptic ulcer disease. Which action should the nurse include in this client's plan of care?
Explanation
The correct answer is A.
When planning to administer the antiulcer gastrointestinal (GI) agent sucralfate to a client with peptic ulcer disease, the nurse should include the following action in the client's plan of care:
A. Give sucralfate on an empty stomach.
Explanation: Sucralfate works by forming a protective coating over the ulcerated area in the stomach and duodenum, providing a physical barrier that helps protect the mucosa from further injury. To maximize its effectiveness, sucralfate should be given on an empty stomach, preferably 1 hour before meals and at bedtime. This allows the medication to adhere to the ulcerated areas without being diluted by food or other medications.
Why the other choices are not appropriate:
B. Monitor for electrolyte imbalance:
Sucralfate is not typically associated with causing electrolyte imbalances. Monitoring for electrolyte imbalances may be relevant for other medications or conditions, but it is not a primary consideration for sucralfate.
C. Administer sucralfate once a day, preferably at bedtime:
The typical dosing regimen for sucralfate involves multiple daily doses, not once a day. The timing of the doses is important, but once-daily dosing is not recommended.
D. Assess for secondary Candida infection:
Sucralfate is not associated with an increased risk of secondary Candida (fungal) infections. Candida infections are more commonly associated with the use of antibiotics or immunosuppressive medications.
A young adult female client who is planning to become pregnant asks the nurse if she can continue taking isotretinoin for cystic acne. Which information is most important for the nurse to provide this client?
Explanation
A. Breastfeeding is not recommended while taking this medication:
While it's important to avoid breastfeeding while taking isotretinoin due to potential risks to the infant, the priority in this scenario is preventing exposure to the medication during pregnancy.
The most important information for the nurse to provide to a young adult female client planning to become pregnant while taking isotretinoin for cystic acne is:
B. Discontinue this medication one month before attempting to conceive.
Explanation: Isotretinoin (commonly known as Accutane) is a teratogenic medication, which means it can cause severe birth defects if taken during pregnancy. Therefore, it is crucial for the client to discontinue this medication well before attempting to conceive. The recommended time frame to wait after stopping isotretinoin before attempting conception varies but is generally at least one month. The specific duration should be discussed with the healthcare provider.
C. Do not take multiple vitamins that contain vitamin A while taking this drug:
Avoiding excessive vitamin A intake is important to prevent vitamin A toxicity, but it is not the most critical piece of information for a client planning to become pregnant while on isotretinoin.
D. Baseline liver function results must be obtained during therapy:
Monitoring liver function is important during isotretinoin therapy, but the priority in this scenario is preventing fetal exposure to the medication by discontinuing it before attempting pregnancy.
A client has a new prescription for zolpidem, a hypnotic. The client tells the home health nurse that he plans to take a dose of the medication during the day because he is exhausted and needs to take a short afternoon nap prior to an evening activity in his home. Which action should the nurse take?
Explanation
A. Remind the client to drink plenty of fluids when taking the medication:
Drinking fluids with zolpidem is not a primary concern in this situation. The main issue is the timing of the medication.
When a client with a new prescription for zolpidem, a hypnotic, plans to take a dose of the medication during the day for a short afternoon nap, the nurse should take the following action:
B. Encourage the client to wait until bedtime to take the medication.
Explanation: Zolpidem is a medication primarily prescribed to help individuals with insomnia fall asleep more easily when taken at bedtime. Taking it during the day, especially if the client plans to engage in activities afterward, can lead to drowsiness, impaired coordination, and reduced alertness. It is not intended for daytime use or for short naps during the day. The nurse should encourage the client to take the medication as prescribed, at bedtime, to ensure safe and effective use.
C. Advise the client to take the medication with the noon meal:
Zolpidem is not typically taken with meals. Again, the primary concern is the timing of the medication.
D. Explain that the client needs to allow for sleep time of at least two hours:
While it's important to allow for sufficient sleep time after taking zolpidem to minimize the risk of impaired alertness and coordination, the client should be encouraged to take the medication at bedtime rather than during the day to ensure it works as intended.
. A client has a new prescription for zolpidem, a hypnotic. The client tells the home health nurse that he plans to take a dose of the medication during the day because he is exhausted and needs to take a short afternoon nap prior to an evening activity in his home. Which action should the nurse take?
Explanation
A. Remind the client to drink plenty of fluids when taking the medication:
Drinking fluids with zolpidem is not a primary concern in this situation. The main issue is the timing of the medication.
When a client with a new prescription for zolpidem, a hypnotic, plans to take a dose of the medication during the day for a short afternoon nap, the nurse should take the following action:
B. Encourage the client to wait until bedtime to take the medication.
Explanation: Zolpidem is a medication primarily prescribed to help individuals with insomnia fall asleep more easily when taken at bedtime. Taking it during the day, especially for a short nap, can lead to drowsiness, impaired coordination, and reduced alertness during activities. It is not intended for daytime use or for short naps during the day. The nurse should encourage the client to take the medication as prescribed, at bedtime, to ensure safe and effective use.
C. Advise the client to take the medication with the noon meal:
Zolpidem is not typically taken with meals. Again, the primary concern is the timing of the medication.
D. Explain that the client needs to allow for sleep time of at least two hours:
While it's important to allow for sufficient sleep time after taking zolpidem to minimize the risk of impaired alertness and coordination, the client should be encouraged to take the medication at bedtime rather than during the day to ensure it works as intended.
The healthcare provider prescribes the antibiotic tetracycline HCI for an adult client that arrived at an outpatient clinic. Which instruction should the nurse include in the teaching plan for this client?
Explanation
A. Take with milk or antacids to prevent gastrointestinal (GI) irritation:
Tetracycline should not be taken with milk or antacids because these can bind to the medication and reduce its absorption. It is generally recommended to take tetracycline with a full glass of water on an empty stomach, unless otherwise instructed by the healthcare provider.
When providing instructions to a client prescribed tetracycline HCl, the nurse should include the following instruction:
B. Protect the skin from sunlight while taking the drug.
Explanation: Tetracycline antibiotics can make the skin more sensitive to sunlight (photosensitivity). Exposure to sunlight or ultraviolet (UV) rays can lead to severe sunburn reactions. Therefore, it is important for clients taking tetracycline to avoid prolonged exposure to direct sunlight and to use sunblock, protective clothing, and sunglasses when outdoors. This precaution helps prevent skin irritation and sunburn.
C. Return to the clinic weekly to obtain serum drug levels:
Routine monitoring of serum drug levels is not typically required for clients taking tetracycline. Monitoring may be necessary for other medications, but it is not a standard practice for tetracycline.
D. Take with orange juice to enhance GI absorption:
Like milk and antacids, taking tetracycline with orange juice can interfere with its absorption. It is generally recommended to take tetracycline with a full glass of water on an empty stomach for optimal absorption.
After receiving five doses of filgrastim, the nurse notes that the client's white blood cell count has increased from 2,500/mm³ (2.5x 10L) to 5,000/mm³ (5 x 10"/L) Which action should the nurse implement?
White Blood Cell (WBC) [Reference Range: 5000 to 10,000/mm3 (5 to 10 x 109/L)]
Explanation
When the nurse notes that the client's white blood cell count has increased from 2,500/mm³ to 5,000/mm³ after receiving five doses of filgrastim, the appropriate action to implement is:
A. Inform the client that the medication has been effective.
Explanation: Filgrastim is a medication that stimulates the production of white blood cells, specifically neutrophils. An increase in the white blood cell count, especially in neutrophils, is a positive response to filgrastim therapy, indicating that the medication has been effective in stimulating the production of white blood cells to combat neutropenia. Therefore, the nurse should inform the client that the medication has been successful in achieving the desired response.
Why the other choices are not appropriate:
B. Assess the client's vital signs:
While monitoring vital signs is important in the overall care of the client, the increase in the white blood cell count alone does not warrant immediate vital signs assessment. Vital signs would be assessed as part of routine nursing care, but they are not the primary concern in this scenario.
C. Implement neutropenic precautions:
Neutropenic precautions are typically implemented when the client has a low white blood cell count (neutropenia), not when the white blood cell count is increasing in response to treatment. In this case, the increase in white blood cells is a desired therapeutic effect.
D. Review the client's culture and sensitivity reports:
Reviewing culture and sensitivity reports is important in cases of infection, but it is not the immediate action to take in response to the increased white blood cell count. The increase in white blood cells indicates a positive response to treatment, but it does not provide information about the presence or type of infection.
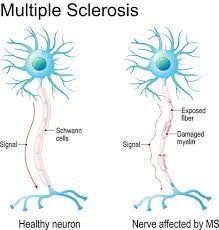
The nurse is administering the muscle relaxant baclofen by mouth (PO) to a client diagnosed with multiple sclerosis. Which intervention should the nurse implement?
Explanation
A. Evaluate muscle strength every 4 hours:
While monitoring muscle strength is essential in assessing the client's response to treatment and potential side effects, checking it every 4 hours may not be necessary and can disrupt the client's rest. Assessing muscle strength as part of the overall neurological assessment at regular intervals is appropriate.
B. Monitor intake and output every 8 hours:
Monitoring intake and output is essential for assessing hydration status, but it is not directly related to the administration of baclofen. It is a routine nursing assessment and should not be tied specifically to this medication.
When administering the muscle relaxant baclofen by mouth (PO) to a client diagnosed with multiple sclerosis, the nurse should implement the following intervention:
C. Advise the client to move slowly and cautiously when rising and walking.
Explanation: Baclofen is a muscle relaxant that can cause drowsiness, dizziness, and muscle weakness as side effects. Therefore, clients taking baclofen should be advised to move slowly and cautiously when rising from a sitting or lying position and when walking. This helps prevent falls and injuries due to the medication's potential effects on coordination and muscle function.
D. Ensure the client knows to stop baclofen before using other antispasmodics:
It is essential for the client to be aware of their medications and potential interactions, but stopping baclofen or any medication should be done under the guidance of a healthcare provider. The nurse should educate the client about the importance of discussing all medications and potential interactions with their healthcare provider but should not instruct them to stop any medication without medical advice.
Sign Up or Login to view all the 53 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

