Wgu rn hesi pharmocology
Total Questions : 39
Showing 25 questions, Sign in for moreThe healthcare provider prescribes the antibiotic tetracycline HCl for an adult client that arrived at an outpatient clinic. Which instruction should the nurse include in the teaching plan for this client?
Explanation
Choice A reason: Tetracycline HCl can make the skin more sensitive to sunlight and increase the risk of sunburn. Therefore, the client should avoid exposure to direct sunlight and use sunscreen or protective clothing while taking the drug.
Choice B reason: Orange juice is acidic and can decrease the absorption of tetracycline HCl in the GI tract. Therefore, the client should not take the drug with orange juice or other acidic beverages.
Choice C reason: Serum drug levels are not routinely monitored for tetracycline HCl, as there is no established therapeutic range or toxicity level for this drug. Therefore, the client does not need to return to the clinic weekly to obtain serum drug levels.
Choice D reason: Milk and antacids can bind to tetracycline HCl and reduce its effectiveness. Therefore, the client should not take the drug with milk or antacids or within 2 hours of consuming them.
The nurse administers risedronate to a client with osteoporosis at 0700. The client asks for a glass of milk to drink with the medication. Which action should the nurse take?
Explanation
Choice A reason: Risedronate is a bisphosphonate that is used to treat osteoporosis by inhibiting bone resorption. It should be taken on an empty stomach with a full glass of water at least 30 minutes before any other food, beverage, or medication. This is because food, milk, and antacids can interfere with the absorption of risedronate and reduce its effectiveness.
Choice B reason: Milk contains calcium, which can bind to risedronate and prevent its absorption. Therefore, the client should not drink milk with or within 2 hours of taking risedronate.
Choice C reason: Withholding the medication until the client's breakfast tray is available is not appropriate, as it would delay the administration of risedronate and disrupt the dosing schedule. The client should take risedronate as soon as possible after waking up and before eating anything.
Choice D reason: Consulting with a pharmacist about scheduling the dose one hour after the client eats is not necessary, as risedronate should be taken at least 30 minutes before any food or beverage. Taking risedronate one hour after eating may not ensure adequate absorption of the drug.
The nurse is planning care for a client with major depression who is receiving a new prescription for duloxetine. Which information is most important for the nurse to obtain?
Explanation
Choice A reason: Recent use of other antidepressants is important to know, as duloxetine is a serotonin-norepinephrine reuptake inhibitor (SNRI) that can interact with other antidepressants, especially monoamine oxidase inhibitors (MAOIs) and selective serotonin reuptake inhibitors (SSRIs). However, this information is not as important as liver function laboratory results, as duloxetine can cause hepatotoxicity in some clients.
Choice B reason: Weight change in the last month is relevant to monitor, as duloxetine can cause weight loss or gain in some clients. However, this information is not as important as liver function laboratory results, as duloxetine can cause liver damage in some clients.
Choice C reason: Family history of mental illness is useful to assess, as duloxetine may be more effective or less effective in clients with certain genetic factors. However, this information is not as important as liver function laboratory results, as duloxetine can cause liver failure in some clients.
Choice D reason: Liver function laboratory results are most important to obtain, as duloxetine is metabolized by the liver and can cause hepatotoxicity in some clients. The nurse should monitor the client's liver enzymes and bilirubin levels before and during treatment with duloxetine and report any signs of liver impairment, such as jaundice, dark urine, abdominal pain, or fatigue.
While assessing a client who takes acetaminophen for chronic pain, the nurse observes that the client's skin looks yellow in color. Which action should the nurse take in response to this finding?
Explanation
Choice A reason: Checking the client's capillary glucose level is not relevant to this finding, as acetaminophen does not affect blood glucose levels. The yellow color of the skin may indicate jaundice, which is a sign of liver damage caused by acetaminophen overdose or toxicity.
Choice B reason: Advising the client to reduce the medication dose is not sufficient to address this finding, as acetaminophen can cause irreversible liver damage if taken in excess or for prolonged periods. The client may need immediate medical attention and treatment with an antidote such as N-acetylcysteine.
Choice C reason: Reporting the finding to the healthcare provider is the appropriate action to take, as the yellow color of the skin may indicate jaundice, which is a sign of liver failure caused by acetaminophen overdose or toxicity. The healthcare provider can order further tests and interventions to assess and treat the client's condition.
Choice D reason: Using a pulse oximeter to assess oxygen saturation is not related to this finding, as acetaminophen does not affect oxygen levels. The yellow color of the skin may indicate jaundice, which is a sign of liver dysfunction caused by acetaminophen overdose or toxicity.
Prior to administering oral doses of calcitriol and calcium carbonate to a client with hypoparathyroidism, the nurse notes that the client's total calcium level is 14 mg/dL (3.5 mmol/L). Which action should the nurse implement?
Explanation
Choice A reason: Holding the calcitriol but administering the calcium carbonate as scheduled is not appropriate, as both drugs can increase the serum calcium level and worsen the condition of hypercalcemia. Calcitriol is a synthetic form of vitamin D that enhances the absorption of calcium from the GI tract and promotes bone mineralization. Calcium carbonate is a supplement that provides additional calcium to the body.
Choice B reason: Holding the calcium carbonate, but administering the calcitriol as scheduled is not appropriate, as calcitriol alone can also raise the serum calcium level and cause hypercalcemia. Calcitriol is a synthetic form of vitamin D that enhances the absorption of calcium from the GI tract and promotes bone mineralization.
Choice C reason: Holding both medications until contacting the healthcare provider is the appropriate action to take, as the client's total calcium level is above the normal range of 9 to 10.5 mg/dL or 2.25 to 2.62 mmol/L and indicates hypercalcemia. Hypercalcemia can cause symptoms such as nausea, vomiting, constipation, confusion, lethargy, muscle weakness, cardiac arrhythmias, and kidney stones. The healthcare provider can adjust the dose or frequency of the medications or prescribe other treatments to lower the serum calcium level.
Choice D reason: Administering both prescribed medications as scheduled is not appropriate, as both drugs can increase the serum calcium level and worsen the condition of hypercalcemia. Calcitriol is a synthetic form of vitamin D that enhances the absorption of calcium from the GI tract and promotes bone mineralization. Calcium carbonate is a supplement that provides additional calcium to the body.
On admission, the healthcare provider prescribes a broad spectrum antibiotic for a client with a gram-negative infection. Before administering the first dose, it is most important for the nurse to implement which prescription?
Explanation
Choice A reason: Monitoring for signs of sodium and fluid retention is not relevant to this situation, as broad spectrum antibiotics do not affect sodium or fluid balance. Sodium and fluid retention may be caused by other conditions such as heart failure, kidney disease, or liver disease.
Choice B reason: Obtaining wound and blood specimens for culture and sensitivity is most important before administering the first dose of a broad spectrum antibiotic, as this can help identify the specific type and strain of bacteria causing the infection and determine which antibiotic is most effective against it. Broad spectrum antibiotics are effective against a wide range of bacteria, but they may also kill beneficial bacteria and increase the risk of resistance or superinfection.
Choice C reason: Obtaining a complete blood count and serum electrolytes is not necessary before administering the first dose of a broad spectrum antibiotic, as these tests do not provide information about the type or severity of infection. A complete blood count may show an elevated white blood cell count or other changes in response to infection, but it does not identify the causative organism. Serum electrolytes may show abnormalities due to dehydration, vomiting, diarrhea, or other factors, but they do not indicate infection.
Choice D reason: Performing irrigation and topical antibiotic application to wound area is not sufficient before administering the first dose of a broad spectrum antibiotic, as this may not reach all sites of infection or eradicate all bacteria. Irrigation and topical antibiotic application may help clean and prevent further contamination of wound area, but they do not replace systemic antibiotic therapy.
A client with Parkinson's disease who is taking carbidopa/levodopa reports that urine appears to be darker in color. Which action should the nurse take?
Explanation
Choice A reason: Encouraging an increase in oral intake is not necessary in this situation, as dark urine is not a sign of dehydration or fluid imbalance. Dark urine may be caused by certain foods, medications, or medical conditions, but it does not indicate a need for more fluids.
Choice B reason: Measuring the client's urinary output is not relevant to this situation, as dark urine is not a sign of urinary retention or obstruction. Urinary output may vary depending on fluid intake, activity level, or other factors, but it does not reflect urine color.
Choice C reason: Explaining that color change is normal is the appropriate action to take, as dark urine is a common and harmless side effect of carbidopa/levodopa, which is a combination drug used to treat Parkinson's disease by increasing dopamine levels in the brain. Carbidopa/levodopa can cause urine to turn brown, black, or red, but this does not affect the function or health of the kidneys or bladder.
Choice D reason: Obtaining a specimen for a urine culture is not necessary in this situation, as dark urine is not a sign of infection or inflammation. A urine culture may be indicated if the client has symptoms such as fever, pain, burning, frequency, or urgency, but it does not diagnose urine color
A female client with multiple sclerosis reports having less fatigue and improved memory since she began using the herbal supplement, ginkgo biloba. Which information is most important for the nurse to include in the teaching plan for this client?
Explanation
Choice A reason: Nausea and diarrhea are possible side effects of ginkgo biloba, but they are not as serious or common as the risk of bleeding caused by the interaction with aspirin and non-steroidal anti-inflammatory drugs. Therefore, this information is not as important as choice c.
Choice B reason: Anxiety and headaches are not associated with the use of ginkgo biloba, but rather with the underlying condition of multiple sclerosis. Therefore, this information is not relevant or accurate for this client.
Choice C reason: Aspirin and non-steroidal anti-inflammatory drugs interact with ginkgo biloba, as both substances have antiplatelet effects that can increase the risk of bleeding. Therefore, this information is most important for the nurse to include in the teaching plan for this client, as the client should avoid taking these drugs while using ginkgo biloba or inform the healthcare provider if they are prescribed.
Choice D reason: Ginkgo biloba use should be limited and not taken during pregnancy, as there is insufficient evidence about its safety and efficacy for pregnant women. However, this information is not as important as choice c, as the client may not be pregnant or planning to become pregnant.
A client in the surgical recovery area asks the nurse to bring the largest possible dose of pain medication available. Which action should the nurse implement first?
Explanation
Choice A reason: Determining when the last dose was administered is important to ensure safe and effective pain management, but it is not the first action that the nurse should implement. The nurse should first assess the client's pain level and intensity before deciding on the appropriate dose and frequency of pain medication.
Choice B reason: Encouraging the client to use diversional thoughts to manage pain is a non-pharmacological intervention that can help reduce pain perception and anxiety, but it is not sufficient to address severe or acute pain. The nurse should first assess the client's pain level and intensity before suggesting any complementary or alternative therapies.
Choice C reason: Asking the client to rate the current level of pain using a pain scale is the first action that the nurse should implement, as it can help quantify and communicate the client's pain experience and guide the nurse's decision on pain medication. The nurse should use a valid and reliable pain scale that is appropriate for the client's age, cognitive ability, and language preference.
Choice D reason: Reviewing the history for a past use of recreational drugs is relevant to assess the client's risk of addiction or tolerance to pain medication, but it is not the first action that the nurse should implement. The nurse should first assess the client's pain level and intensity before considering any factors that may influence pain management.
Prior to administering the evening dose of carbamazepine, the nurse notes that the client's morning carbamazepine level was 8.4 mg/L (35.6 mcmol/L). Which action should the nurse take?
Explanation
Choice A reason: Notifying the healthcare provider of the carbamazepine level is not necessary, as 8.4 mg/L (35.6 mcmol/L) is within
the normal range of 4 to 12 mg/L (16.9 to 50.8 mcmol/L). The healthcare provider may adjust
the dose based on other factors such as clinical response, seizure frequency, or adverse effects,
but not based on this level alone.
Choice B reason: Administering the carbamazepine as prescribed is the appropriate action to take, as 8.4 mg/L (35.6 mcmol/L) is within
the normal range of 4 to 12 mg/L (16.9 to 50.8 mcmol/L). The nurse should follow the prescribed
dose and schedule of carbamazepine to maintain a therapeutic level and prevent seizures.
Choice C reason: Assessing the client for side effects of carbamazepine is important, as carbamazepine can cause adverse effects such as drowsiness, dizziness, nausea, rash, or blood dyscrasias. However, this action is not related to the carbamazepine level, as side effects can occur at any level and may not correlate with the serum concentration. The nurse should monitor the client for side effects regardless of the carbamazepine level.
Choice D reason: Withholding this dose of carbamazepine is not appropriate, as 8.4 mg/L (35.6 mcmol/L) is withinthe normal range of 4 to 12 mg/L (16.9 to 50.8 mcmol/L). Withholding the dose may cause a drop in the serum concentration and increase the risk of seizures. The nurse should administer the carbamazepine as prescribed unless instructed otherwise by the healthcare provider.
A client is receiving intravenous (IV) vancomycin and the nurse plans to draw blood for a peak and trough to determine the serum level of the drug. Which collection times provide the best determination of these levels?
Explanation
Choice A reason: This is the best option to measure the peak and trough levels of vancomycin, as it reflects the highest and lowest concentrations of the drug in the blood. The peak level indicates the efficacy and potential toxicity of vancomycin, while the trough level indicates the clearance and potential subtherapeutic effect of vancomycin. The peak level should be drawn immediately after completion of the IV dose, as it takes about 30 minutes for vancomycin to reach its maximum concentration in the blood. The trough level should be drawn 30 minutes before the next administration of the medication, as it represents the lowest concentration of vancomycin in the blood before it is replenished by another dose.
Choice B reason: This is not a good option to measure the peak and trough levels of vancomycin, as it may not capture the true highest and lowest concentrations of the drug in the blood. The peak level may be lower than expected, as it takes about 30 minutes for vancomycin to reach its maximum concentration in the blood. The trough level may be higher than expected, as it is drawn too close to the next administration of the medication.
Choice C reason: This is not a good option to measure the peak and trough levels of vancomycin, as it does not reflect the highest and lowest concentrations of the drug in the blood. The peak level is drawn too early, as vancomycin has not reached its maximum concentration in the blood yet. The trough level is drawn too late, as vancomycin has already started to decline in the blood.
Choice D reason: This is not a good option to measure the peak and trough levels of vancomycin, as it may miss the highest and lowest concentrations of the drug in the blood. The peak level is drawn too late, as vancomycin may have already started to decline in the blood. The trough level is drawn too early, as vancomycin may have not reached its minimum concentration in the blood yet.
A young adult female client who is planning to become pregnant asks the nurse if she can continue taking isotretinoin for cystic acne. Which information is most important for
Explanation
Choice A reason: Breast feeding is not recommended while taking this medication, as isotretinoin can pass into breast milk and harm
the nursing infant. However, this information is not as important as choice d, as the client may not be breast feeding or planning to breast feed.
Choice B reason: Baseline liver function results must be obtained during therapy, as isotretinoin can cause liver damage and increase liver enzymes. However, this information is not as important as choice d, as the client may not have liver problems or need liver function tests.
Choice C reason: Do not take multiple vitamins that contain vitamin A while taking this drug, as isotretinoin is a derivative of vitamin A and can cause vitamin A toxicity if taken in excess. However, this information is not as important as choice d, as the client may not take multiple vitamins or have vitamin A toxicity.
Choice D reason: Discontinue this medication one month before attempting to conceive, as isotretinoin can cause severe birth defects and miscarriages if taken during pregnancy. Therefore, this information is most important for the nurse to provide this client, as the client is planning to become pregnant and should avoid isotretinoin exposure.
The nurse is planning to administer the antiulcer gastrointestinal (GI) agent sucralfate to a client with peptic ulcer disease. Which action should the nurse include in this client's plan of care?
Explanation
Choice A reason: This is the correct action to include in the client's plan of care, as sucralfate should be given on an empty stomach, at least one hour before meals and at bedtime. Sucralfate is a mucosal protectant that forms a protective barrier over the ulcer and prevents further damage from acid and pepsin. It requires an acidic environment to work, so it should not be taken with food or antacids.
Choice B reason: This is not a relevant action to include in the client's plan of care, as sucralfate does not cause or increase the risk of secondary Candida infection. Candida infection is a fungal infection that can affect the mouth, throat, esophagus, or vagina. It is more common in clients who use antibiotics, corticosteroids, or immunosuppressants, but not sucralfate.
Choice C reason: This is not an accurate action to include in the client's plan of care, as sucralfate should be administered four times a day, not once a day. Sucralfate has a short duration of action, so it needs to be taken frequently to maintain its protective effect on the ulcer.
Choice D reason: This is not a necessary action to include in the client's plan of care, as sucralfate does not cause or affect electrolyte imbalance. Electrolyte imbalance is an abnormality in the levels of sodium, potassium, calcium, magnesium, or other minerals in the blood. It can be caused by dehydration, vomiting, diarrhea, kidney disease, or other conditions, but not sucralfate.
The nurse administers naloxone to a client with opioid-induced respiratory depression. One hour later, nursing assessment reveals that the client has a respiratory rate of 4 breaths/minute, oxygen saturation of 75%, and is unable to be aroused. Which action should the nurse implement?
Explanation
Choice A reason: Chest tube insertion is not indicated for respiratory depression caused by opioid overdose. It is a procedure used to treat pneumothorax, hemothorax, or pleural effusion.
Choice B reason: CPR is not the first-line intervention for respiratory depression. It is only indicated when the client has no pulse or signs of life.
Choice C reason: Glasgow Coma Scale score is a tool to assess the level of consciousness of a client. It is not an intervention that can reverse respiratory depression.
Choice D reason: Naloxone is an opioid antagonist that can reverse the effects of opioid overdose. It has a short half-life and may need to be repeated if the client's condition does not improve or worsens.
A client with benign prostatic hyperplasia receives a new prescription of tamsulosin. Which intervention should the nurse perform to monitor for an adverse reaction?
Explanation
Choice A reason: A bladder scan is used to measure the post-void residual urine volume, which can indicate urinary retention. It is not related to the adverse effects of tamsulosin.
Choice B reason: Assessing urine output is important for clients with urinary problems, but it is not specific to the adverse effects of tamsulosin.
Choice C reason: Tamsulosin is an alpha-blocker that relaxes the smooth muscles of the prostate and bladder neck, improving urine flow. However, it can also cause hypotension, dizziness, and fainting as adverse effects. Therefore, monitoring blood pressure is essential for clients taking tamsulosin.
Choice D reason: Obtaining daily weights is not relevant to the adverse effects of tamsulosin. It is more useful for clients with fluid retention or edema.
A client is receiving a secondary infusion of azithromycin 500 mg in 500 mL of normal saline (NS) to be infused over 2 hours. The intravenous (IV) administration set delivers 10 gtt/mL. How many gtt/min should the nurse regulate the infusion? (Enter numerical value only. If rounding is required, round to the nearest whole number.)
Explanation
The correct answer is 21 gtt/min.
To calculate the infusion rate, use the formula:
gtt/min = (volume in mL x drop factor in gtt/mL) / time in min
Plug in the given values:
gtt/min = (500 mL x 10 gtt/mL) / 120 min
gtt/min = 5000 gtt / 120 min
gtt/min = 41.67 gtt/min
Round to the nearest whole number:
gtt/min = 42 gtt/min
A client with chemotherapy-induced nausea receives a prescription for metoclopramide. Which adverse effect is most important for the nurse to report?
Explanation
Choice A reason: Diarrhea is a common side effect of metoclopramide, but it is not life-threatening or indicative of a serious reaction. The nurse should monitor the client's fluid and electrolyte status and provide supportive care.
Choice B reason: Involuntary movements, such as twitching, grimacing, or spasms, are signs of a rare but serious condition called tardive dyskinesia, which can be caused by metoclopramide. This condition can be irreversible and disabling, so the nurse should report it immediately and stop the medication.
Choice C reason: Nausea is the reason why the client is receiving metoclopramide, which is an antiemetic drug. If the client still experiences nausea, the nurse should assess the effectiveness of the medication and notify the prescriber if needed.
Choice D reason: Unusual irritability is not a common or serious side effect of metoclopramide. It may be related to other factors, such as stress, pain, or fatigue. The nurse should provide emotional support and reassurance to the client.
The nurse initiates an infusion of piperacillin-tazobactam for a client with a urinary tract infection. Five minutes into the infusion, the client reports not feeling well. Which client manifestation should the nurse identify as a reason to stop the infusion?
Explanation
Choice A reason: Hypertension is not a typical sign of an allergic reaction to piperacillin-tazobactam, which is an antibiotic. It may be caused by other factors, such as pain, anxiety, or renal impairment. The nurse should monitor the client's blood pressure and report any abnormal findings.
Choice B reason: Bradycardia is not a common or serious side effect of piperacillin-tazobactam. It may be related to other medications, such as beta-blockers, or underlying cardiac conditions. The nurse should check the client's pulse and rhythm and report any changes.
Choice C reason: Pupillary constriction is not associated with piperacillin-tazobactam or an allergic reaction. It may be caused by other drugs, such as opioids, or neurological disorders. The nurse should assess the client's level of consciousness and pupillary response.
Choice D reason: Scratchy throat is a possible sign of anaphylaxis, which is a severe and potentially fatal allergic reaction to piperacillin-tazobactam or any other drug. Other symptoms may include hives, swelling, wheezing, or hypotension. The nurse should stop the infusion immediately and call for help.
A female client who is a vegetarian has a new prescription for warfarin. The client states she eats leafy green vegetables every day. How should the nurse respond?
Explanation
Choice A reason: Replacing leafy vegetables with a protein source is not necessary or advisable for a vegetarian client who takes warfarin. Leafy vegetables are rich in vitamin K, which can interfere with warfarin's anticoagulant effect, but they also provide other nutrients and benefits for health. Protein sources such as nuts or beans may also contain vitamin K or other substances that can affect warfarin's action.
Choice B reason: Commending the client for her healthy lifestyle and encouraging her to continue her current diet habits is not appropriate or safe for a vegetarian client who takes warfarin. Leafy vegetables can alter warfarin's anticoagulant effect and increase the risk of bleeding or clotting complications if not monitored closely by the healthcare provider.
Choice C reason: Advising the client that the healthcare provider needs to be made aware of her current diet is the best response for a vegetarian client who takes warfarin. Leafy vegetables can affect warfarin's anticoagulant effect by increasing vitamin K levels in the body, which counteracts warfarin's action. The healthcare provider can adjust the warfarin dose accordingly and monitor the client's international normalized ratio (INR), which is a measure of blood clotting time.
Choice D reason: Confirming that her diet choices will help the medication be more effective in preventing blood clots is incorrect and misleading for a vegetarian client who takes warfarin. Leafy vegetables can decrease warfarin's anticoagulant effect by increasing vitamin K levels in the body, which enhances blood clotting. This can reduce the effectiveness of warfarin and increase the risk of thromboembolic events, such as stroke or pulmonary embolism.
The nurse is caring for a client who has been taking ibuprofen. Which finding is most important for the nurse to report to the healthcare provider?
Explanation
Choice A reason: Hematemesis is the vomiting of blood, which can indicate a serious gastrointestinal bleeding caused by ibuprofen. This is a life-threatening condition that requires immediate medical attention. Therefore, the nurse should report this finding to the healthcare provider as soon as possible.
Choice B reason: Insomnia is the difficulty in falling asleep or staying asleep. It can be a side effect of ibuprofen, but it is not as serious or urgent as hematemesis. The nurse can advise the client to take ibuprofen with food or milk, avoid caffeine and alcohol, and practice good sleep hygiene.
Choice C reason: Dizziness is the feeling of lightheadedness, faintness, or unsteadiness. It can also be a side effect of ibuprofen, but it is usually mild and transient. The nurse can instruct the client to rise slowly from a sitting or lying position, drink plenty of fluids, and avoid driving or operating machinery if dizzy.
Choice D reason: Nausea is the feeling of discomfort or unease in the stomach that may lead to vomiting. It can also be a side effect of ibuprofen, but it is usually manageable with simple measures. The nurse can suggest the client to take ibuprofen with food or milk, eat small and frequent meals, and avoid spicy or fatty foods.
An older adult with iron deficiency anemia is being discharged with a prescription for ferrous sulfate enteric-coated tablets. To promote best absorption of the medication, which information should the nurse include in the discharge instructions?
Explanation
Choice A reason: Ferrous sulfate is best absorbed on an empty stomach, so waiting 2 hours after meals to take the tablet will enhance its effectiveness. Food can interfere with iron absorption, especially dairy products, eggs, coffee, tea, and antacids.
Choice B reason: Bedtime is not the best time to take the tablet, because lying down after taking iron can cause gastrointestinal upset, such as nausea, vomiting, constipation, or diarrhea. The client should take the tablet with a full glass of water and remain upright for at least 30 minutes.
Choice C reason: Taking the tablet with a daily multivitamin is not recommended, because some vitamins and minerals can reduce iron absorption, such as calcium, zinc, copper, and vitamin E. The client should avoid taking iron with other supplements unless advised by the healthcare provider.
Choice D reason: Crushing the tablets and mixing with pudding is not advisable, because enteric-coated tablets are designed to dissolve slowly in the intestine and protect the stomach from irritation. Crushing them will destroy their coating and reduce their effectiveness. The client should swallow the tablets whole and not chew or crush them.
A client with pneumonia who has an emergent episode of respiratory distress is intubated and transferred to the intensive care unit. The client's chest x-ray shows consolidation in the left lobe, and physical assessment reveals diminished lung sounds. The nurse administers acetylcysteine as prescribed per nebulization via endotracheal tube. Which therapeutic response of this medication should the nurse expect?
Explanation
Choice C reason: Acetylcysteine is a mucolytic agent that breaks down mucus and makes it easier to cough up or suction out. This helps to clear the airways and improve oxygenation. The nurse should expect to see increased sputum production after administering acetylcysteine and provide frequent suctioning as needed.
Choice A reason: Bronchodilation and wheezing are not therapeutic responses of acetylcysteine, but rather possible adverse effects. Acetylcysteine can cause bronchospasm or bronchoconstriction in some clients, especially those with asthma or chronic obstructive pulmonary disease (COPD). The nurse should monitor the client's breath sounds and oxygen saturation and report any signs of respiratory distress.
Choice B reason: Unpleasant smell when using the medication is not a therapeutic response of acetylcysteine, but rather a common side effect. Acetylcysteine has a rotten egg odor that can be unpleasant for both the client and the nurse. The nurse can minimize this by using a mouthwash or a flavored lozenge before and after administering acetylcysteine.
Choice D reason: Hypotension is not a therapeutic response of acetylcysteine, but rather a rare but serious adverse effect. Acetylcysteine can cause vasodilation or hypovolemia in some clients, leading to low blood pressure and shock. The nurse should monitor the client's vital signs and report any signs of hypotension.
The nurse admits a client with a diagnosis of stage 4 cancer. The client has a prescription to wear a subcutaneous morphine sulfate patch for pain. The client is short of breath and difficult to arouse. While performing a head to toe assessment, the nurse discovers four patches on the client's body. Which action should the nurse take first?
Explanation
Choice B reason: Administering a narcotic reversal drug, such as naloxone, is the first action that the nurse should take in this situation. The client is showing signs of opioid overdose, such as respiratory depression, sedation, and confusion. Naloxone can reverse these effects by blocking the opioid receptors in the brain and restoring normal breathing and consciousness.
Choice A reason: Applying oxygen face mask is not the first action that the nurse should take in this situation, but rather a supportive measure that can be done after administering naloxone. Oxygen can help to improve the client's oxygenation and prevent hypoxia, but it will not reverse the opioid overdose.
Choice C reason: Removing the morphine patches is not the first action that the nurse should take in this situation, but rather a preventive measure that can be done after administering naloxone. Removing the patches can help to stop the absorption of more morphine into the bloodstream and prevent further toxicity, but it will not reverse the opioid overdose.
Choice D reason: Monitoring blood pressure is not the first action that the nurse should take in this situation, but rather an ongoing assessment that can be done after administering naloxone. Monitoring blood pressure can help to detect any changes in the client's hemodynamic status and guide further interventions, but it will not reverse the opioid overdose.
A client with heart failure (HF) develops hyperaldosteronism and spironolactone is prescribed. Which instruction should the nurse include in this client's plan of care?
Explanation
Choice B reason: Spironolactone is a potassium-sparing diuretic that blocks the action of aldosterone, a hormone that causes sodium and water retention and potassium loss. By reducing fluid overload and blood pressure, spironolactone can improve the symptoms and outcomes of HF. However, spironolactone can also cause bleeding problems, such as thrombocytopenia (low platelet count) and increased prothrombin time (PT). Therefore, the nurse should instruct the client to monitor skin for excessive bruising, petechiae, or bleeding gums, and report any signs of bleeding to the healthcare provider.
Choice A reason: Covering your skin before going outside is not an instruction that the nurse should include in this client's plan of care, but rather a general precaution that anyone should take to protect their skin from sun damage. Spironolactone does not increase the risk of sunburn or photosensitivity.
Choice C reason: Limiting intake of high-potassium foods is not an instruction that the nurse should include in this client's plan of care, but rather a contraindication for taking spironolactone. Spironolactone can cause hyperkalemia (high potassium level) by preventing potassium excretion in the urine. Therefore, the client should avoid foods that are high in potassium, such as bananas, oranges, potatoes, tomatoes, spinach, and salt substitutes.
Choice D reason: Replacing salt with a salt substitute is not an instruction that the nurse should include in this client's plan of care, but rather a dangerous practice that can lead to hyperkalemia. Salt substitutes are often made with potassium chloride, which can increase the potassium level in the blood. The client should use herbs or spices instead of salt or salt substitutes to flavor their food.
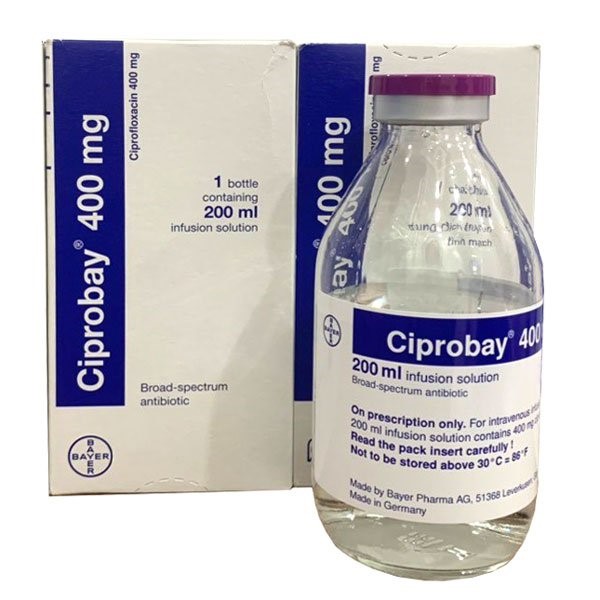
The nurse receives a prescription for ciprofloxacin 400 mg intravenously (IV) every 12 hours to be infused over an hour. The IV bag contains ciprofloxacin 400 mg in dextrose 5% in water (D5W) 200 mL. The nurse should program the infusion pump to deliver how many mL/hr? (Enter numerical value only.)
Explanation
The correct answer is 200 mL/hr.
Explanation: To calculate the infusion rate, the nurse should use the formula:
Infusion rate (mL/hr) = Volume (mL) / Time (hr)
In this case, the volume is 200 mL and the time is 1 hour. Therefore,
Infusion rate (mL/hr) = 200 mL / 1 hr
Infusion rate (mL/hr) = 200 mL/hr
Sign Up or Login to view all the 39 Questions on this Exam
Join over 100,000+ nursing students using Nursingprepexams’s science-backend flashcards, practice tests and expert solutions to improve their grades and reach their goals.
Sign Up Now

